Fibrinogen degradation product levels on arrival for trauma patients requiring a transfusion even without head injury
Youichi Yanagawa, Kouhei Ishikawa, Kei Jitsuiki, Toshihiko Yoshizawa, Yasumasa Oode, Kazuhiko Omori, Hiromichi Ohsaka
Department of Acute Critical Care Medicine, Shizuoka Hospital, Juntendo University, Nagaoka Izunokuni City Shizuoka, Japan
Fibrinogen degradation product levels on arrival for trauma patients requiring a transfusion even without head injury
Youichi Yanagawa, Kouhei Ishikawa, Kei Jitsuiki, Toshihiko Yoshizawa, Yasumasa Oode, Kazuhiko Omori, Hiromichi Ohsaka
Department of Acute Critical Care Medicine, Shizuoka Hospital, Juntendo University, Nagaoka Izunokuni City Shizuoka, Japan
BACKGROUND: There have been few reports on the clinical significance of the fibrinogen degradation product (FDP) level in trauma patients with and without head injury. We retrospectively analyzed trauma patients with or without head injury to investigate the clinical signif i cance of the FDP level.
METHODS: From April 2013 to June 2015, a medical chart review was retrospectively performed for all patients with trauma. The exclusion criteria included patients who did not receive a transfusion. The patients were divided into two groups: a FDP>100 group, which included patients who had an FDP level on arrival over 100 ng/mL, and a FDP≤100 group.
RESULTS: The ratio of open fractures and the prothrombin ratio in the FDP>100 group were significantly smaller than those observed in the FDP≤100 group. The average age, ratio of blunt injury, Injury Severity Score (ISS), volume of transfusion and mortality ratio in the FDP>100 group were signif i cantly greater than those in the FDP≤100 group. There was a weakly positive correlation between the FDP level and ISS (R=0.35, P=0.002), but it was not associated with the transfusion volume. The results of an analysis excluding patients with head injury showed a similar tendency.
CONCLUSION: The FDP levels may be a useful biochemical parameter for the initial evaluation of the severity of trauma and mortality even in blunt traumatized patients without head injury or with stable vital signs.
Fibrinogen degradation product; Injury Severity Score; Transfusion; Mortality
INTRODUCTION
Brain tissue contains a rich tissue plasminogen activator. When the brain tissue is damaged, elevated fibrinogen degradation product (FDP) levels are recognized as a result of fibrinolysis by the released tissue plasminogen activator. For head injured patients, the level of FDP on arrival has been reported to be a useful biochemical marker to predict the deterioration of a hematoma, severity and mortality.[1–3]However, few reports have investigated the clinical signif i cance of the FDP level for trauma patients without head injury. Zhang et al[4]reported that elevated plasma D-dimer levels, which have a strongly positive correlation with the FDP level, were common in orthopedic trauma cases, and the D-dimer level and the number of fractures in trauma patients were closely correlated. Accordingly, the authors concluded that the D-dimer level was not only an indicator for the diagnosis of deep vein thrombosis and pulmonary embolus, but also an indicator of the severity of trauma in acute orthopedic trauma patients. Other reports have also indicated that the level of FDP on arrival is a useful biochemical marker to predict the injury severity, volume of transfusion and mortality of trauma patients.[5–8]However, these reports includedpatients with head injury, so the existence of patients with head injury affected their results. Accordingly, we retrospectively analyzed trauma patients with or without head injury to investigate the clinical signif i cance of the FDP level.
METHODS
The protocol of this retrospective study was approved by the review board of Juntendo Shizuoka Hospital, and all examinations were conducted according to the standards of good clinical practice and the Helsinki Declaration.
The Department of Acute Critical Care Medicine, Juntendo Shizuoka Hospital, which is a hospital with 552 beds in the Izu Peninsula at Shizuoka Prefecture located near Tokyo, serves a population of approximately 270 000. The helicopter parks at our hospital, and the emergency medical system of physician-staffed emergency helicopters in Eastern Shizuoka Prefecture, primarily transports patients with severe conditions from Izu Peninsula to our hospital. Our department mainly treats patients with severe trauma, cardiopulmonary arrest, unconsciousness, convulsion, intoxication and unstable vital signs. When we treat these trauma patients, we typically perform a biochemical analysis which includes the FDP level.
The purpose of the present study was to evaluate the clinical signif i cance of FDP in an attempt to prevent mortality, assess the need for transfusion, evaluate the severity of injury among patients with moderate and severe trauma, and investigate the factors that inf l uence the FDP level. From April 2013 to June 2015, a medical chart review was retrospectively performed for all patients with trauma. Cases of trauma were recorded as "trauma" in our hospital database. The excluded patients were those who did not receive a transfusion, and those with moderate and severe trauma.[9–13]The results of a pre-review indicated that the minimum FDP levels of the mortality cases were over 100 ng/mL [except for patients with a cut wound (Figure 1)]. The patients were divided into two groups: an FDP>100 group, patients whose FDP level on arrival >100 ng/mL; and an FDP≤100 group, patients whose FDP level on arrival ≤100 ng/mL. At fi rst, data on patient's gender, age, systolic blood pressure, heart rate, Glasgow Coma Scale on arrival, type of injury (blunt versus penetrating), mechanism of injury (traffic accident, fall or others), Injury Severity Score (ISS), ratio of head injury, ratio of open fracture, level of FDP, hemoglobin, creatine phosphokinase (CPK), prothrombin ratio, volume of transfusion and mortality rate were analyzed between the two groups. Then, the same data excluding the ratio of head injury were analyzed between the two groups after the exclusion of patients with intracranial lesions, such as subarachnoid hemorrhage or cerebral contusion, conf i rmed by computed tomography. The correlation between the FDP level and ISS or transfusion volume was also analyzed.
Statistical analyses were performed using the non-paired Student's t test, the paired Student's t test, the Chi-square test or correlation as appropriate. A P value of <0.05 was considered to indicate a statistically significant difference. All data were presented as the mean±standard error.
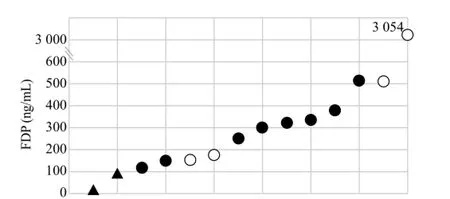
Figure 1. A scattergram of the FDP values among the mortality cases. Among the blunt trauma mortality cases (head injury, white circle; without head injury, back circle), the minimum FDP value was 104 ng/mL (with the exception of the penetrating wound cases [triangle]).
RESULTS
During the investigation, 2 041 patients were treated in the emergency room. Among these patients, 1 098 were trauma patients. In the 1 098 patients, 997 patients who did not receive a transfusion were excluded, and 101 were enrolled as study subjects. There were 57 patients in the FDP>100 group and 44 patients in the FDP≤100 group. Among the subjects, the minimum ISS was 4; thus mild trauma patients could be excluded because in all patients, the Abbreviated Injury Scale (AIS) was at least 2 (moderate injury).
The results of an analysis including all subjects are shown in Table 1. There were no signif i cant differences between the two groups in vital signs, ratio of head injury, level of hemoglobin and CPK. However, the ratio of open fractures and the prothrombin ratio in the FDP>100 group were significantly smaller than those in the FDP≤100 group. The average age, ratio of blunt injury, ISS, volume of transfusion and mortality ratio in the FDP>100 group were significantly greater thanthose in the FDP≤100 group. The ratio of females in the FDP>100 group was greater than that in the FDP≤100 group; however, this difference was not signif i cant.
The results of an analysis excluding patients with head injury are shown in Table 2. The results showed similar tendencies to the analysis of the overall cohort. A weakly positive correlation was observed between the FDP level and ISS (R=0.35, P=0.002); however, there was no positive correlation between the FDP level and the transfusion volume (R=0.17, P=0.9).
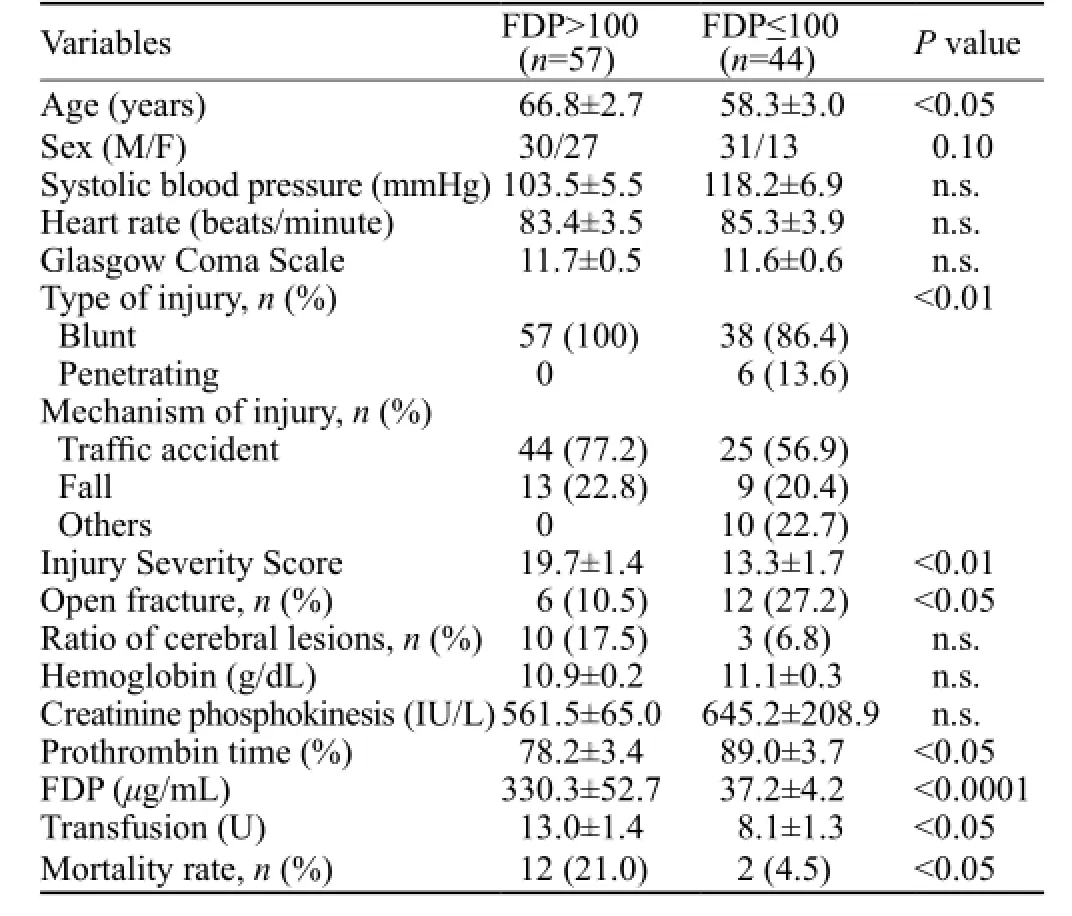
Table 1. The demographic and clinical characteristics according to the FDP level in all patients including those with head injuries
DISCUSSION
This is a study to demonstrate that among trauma patients who required a transfusion, patients with a level of FDP over 100 ng/mL on arrival tended to have a higher age, higher frequency of closed fractures, blunt injury, severe trauma, greater volume of transfusion and higher mortality in comparison with the FDP≤100 group. A similar tendency remained even after the exclusion of patients with head injury.
Previous reports have revealed that the FDP levels increase because of trauma and the levels of FDP correlated with the severity of the trauma.[4,14,15]The mechanism of the positive correlation between the FDP levels and the severity of the trauma might be a potential explanation for an increase in the release of tissue factor, which causes fibrinolysis or formation of a hematoma depending on the severity of the trauma.[16,17]However, drainage of the tissue factor or hematoma from the body through penetrating or open wounds may explain the finding that penetrating trauma patients or blunt trauma patients with open fractures tended to have low levels of FDP.
In the present study, more patients overall and more elderly patients were observed in the FDP>100 group than in the FDP≤100 group. Elderly or female patients tend to have soft tissue or osteoporotic bone fragility.[18,19]Accordingly, similar external energy might produce more severe injuries in elderly or female patients than in young or male patients. More severe injuries lead to higher levels of FDP. This might be an explanation why more patients overall and more elderly patients were observed in the FDP>100 group in our study. Since Japan is a super aging society and the number of elderly women in the general population is increasing, the results of our study may be affected.[20,21]
In our study, the mortality of the FDP>100 group was signif i cantly higher than that of the FDP≤100 group. However, average vital signs such as the systolic blood pressure, heart rate and GCS were not significantly different between the two groups. The level of FDP on arrival was positively correlated with the severity of the trauma, which indicated the severity of anatomical damage. Accordingly, the level of FDP in trauma patients might be a useful biochemical marker even in patients with stable vital signs.
There are some limitations in our study, including its retrospective design and the small number of cases. We also excluded patients who did not require a transfusion, who were thought to have mild trauma because most patients with mild injury did not receive blood test.Therefore, future prospective investigations with a greater accumulation of patients are needed to further study this issue.
CONCLUSION
The FDP levels may be a useful biochemical parameter for the initial evaluation of the severity of trauma and mortality even in blunt trauma patients without head injury or with stable vital signs.
Funding: None.
Ethical approval: The protocol of this retrospective study was approved by the review board of Juntendo Shizuoka Hospital, and all examinations were conducted according to the standards of good clinical practice and the Helsinki Declaration.
Conf l icts of interest: No any benef i ts have been received from a commercial party related directly or indirectly to the study.
Contributors: Yanagawa Y designed the study, gathered data and wrote the manuscript. Jitsuiki K, Ishikawa K, Yoshizawa T, Oode Y, Omori K and Ohsaka H gave technical support and conceptual advice and edited the manuscript.
REFERENCES
1 Suehiro E, Koizumi H, Fujiyama Y, Yoneda H, Suzuki M. Predictors of deterioration indicating a requirement for surgery in mild to moderate traumatic brain injury. Clin Neurol Neurosurg. 2014;127:97–100.
2 Selladurai BM, Vickneswaran M, Duraisamy S, Atan M. Coagulopathy in acute head injury—a study of its role as a prognostic indicator. Br J Neurosurg. 1997; 11(5):398–404.
3 Saggar V, Mittal RS, Vyas MC. Hemostatic abnormalities in patients with closed head injuries and their role in predicting early mortality. J Neurotrauma. 2009;26(10):1665–8.
4 Zhang LD, Liu HB, Li YN, Ma HM, Liu YB, Wang MY. Correlation analysis between plasma D-dimer levels and orthopedic trauma severity. Chin Med J (Engl). 2012;125(17):3133–6.
5 Suehiro E, Koizumi H, Fujiyama Y, Yoneda H, Suzuki M. Predictors of deterioration indicating a requirement for surgery in mild to moderate traumatic brain injury. Clin Neurol Neurosurg. 2014;127:97–100.
6 Hagiwara S, Oshima K, Aoki M, Murata M, Ishihara K, Kaneko M, et al. Usefulness of fi brin degradation products and d-dimer levels as biomarkers that ref l ect the severity of trauma. J Trauma Acute Care Surg. 2013;74(5):1275–8.
7 Raza I, Davenport R, Rourke C, Platton S, Manson J, Spoors C, et al. The incidence and magnitude of fibrinolytic activation in trauma patients. J Thromb Haemost. 2013;11(2):307–14.
8 Turtay MG, Kirimliolu V, Ceylan C. Coagulopathy in multiple traumas. Ulus Travma Acil Cerrahi Derg. 2010;16(3):198–202.
9 Carlin AM, Tyburski JG, Wilson RF, Steffes C. Factors affecting the outcome of patients with splenic trauma. Am Surg. 2002;68(3):232–9.
10 Tornetta P 3rd, Mostafavi H, Riina J, Turen C, Reimer B, Levine R, et al. Morbidity and mortality in elderly trauma patients. J Trauma. 1999;46(4):702–6.
11 Mostafa G, Gunter OL, Norton HJ, McElhiney BM, Bailey DF, Jacobs DG. Age, blood transfusion, and survival after trauma. Am Surg. 2004;70(4):357–63.
12 Malone DL, Dunne J, Tracy JK, Putnam AT, Scalea TM, Napolitano LM. Blood transfusion, independent of shock severity, is associated with worse outcome in trauma. J Trauma. 2003;54(5):898–905; discussion 905–7.
13 Robinson WP 3rd, Ahn J, Stiffler A, Rutherford EJ, Hurd H, Zarzaur BL, et al. Blood transfusion is an independent predictor of increased mortality in nonoperatively managed blunt hepatic and splenic injuries. J Trauma. 2005;58(3):437–44; discussion 444–5.
14 Inoue K, Hifumi T, Kiriu N, Kanemura T, Okada I, Inoue J, et al. Acute coagulopathy after multiple blunt injuries in a case of hemophilia A-consideration for pathophysiology of coagulopathy. Am J Emerg Med. 2017;35(1):194.e1–194.e3.
15 Johansson PI, Sørensen AM, Perner A, Welling KL, Wanscher M, Larsen CF, et al. Disseminated intravascular coagulation or acute coagulopathy of trauma shock early after trauma? An observational study. Crit Care. 2011;15(6):R272.
16 Hayakawa M, Gando S, Ieko M, Honma Y, Homma T, Yanagida Y, et al. Massive amounts of tissue factor induce fi brinogenolysis without tissue hypoperfusion in rats. Shock. 2013;39(6):514–9.
17 Cade J, Regoeczi E, Hirsh J, Buchanan M. The effect of experimental hematoma on serum levels of fibrinogen-related antigen. Blood. 1976;47(5):855–9.
18 Omori K, Ishikawa K, Obinata M, Mishima K, Fukusato S, Ohsaka H, et al. Significance of the vacuum phenomenon in patients with trauma evaluated by whole-body computed tomography. Am J Emerg Med. 2015;33(2):282–5.
19 Obinata M, Omori K, Ishikawa K, Osaka H, Oode Y, Yanagawa Y. Significance of pneumorrhachis detected by single-pass whole-body computed tomography in patients with trauma. J Emerg Trauma Shock. 2015;8(2):120–1.
20 Soen S, Fujiwara S, Takayanagi R, Sato M, Tsujimoto M, Yamamoto T, et al. Japan Fracture Observational Study (JFOS): patient characteristics and interim data on the use of daily teriparatide in Japanese patients with osteoporosis. Curr Med Res Opin. 2015;31(9):1771–9.
21 Arai H, Ouchi Y, Toba K, Endo T, Shimokado K, Tsubota K, et al. Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr Gerontol Int. 2015;15(6):673–87.
Received February 20, 2016
Accepted after revision Auguat 3, 2016
World J Emerg Med 2017;8(2):106–109
10.5847/wjem.j.1920–8642.2017.02.004
Youichi Yanagawa, Email: yyanaga@juntendo.ac.jp
 World journal of emergency medicine2017年2期
World journal of emergency medicine2017年2期
- World journal of emergency medicine的其它文章
- Instructions for Authors
- Information for Readers
- World Journal of Emergency Medicine
- Acute airway emergency caused by an organic foreign body located in the laryngeal mucosa
- Bacteremia or pseudobacteremia? Review of pseudomonas fl uorescens infections
- An unusual case of renal calculi leading to myocardial infarction and cardiogenic shock
