BRAF V600E突变对甲状腺乳头状癌发生及预后的影响
张婷婷,渠 宁,史荣亮 综述,嵇庆海 审校
复旦大学附属肿瘤医院头颈外科,复旦大学上海医学院肿瘤学系,上海 200032
BRAF V600E突变对甲状腺乳头状癌发生及预后的影响
张婷婷,渠 宁,史荣亮 综述,嵇庆海 审校
复旦大学附属肿瘤医院头颈外科,复旦大学上海医学院肿瘤学系,上海 200032
甲状腺乳头状癌(papillary thyroid cancer,PTC)是甲状腺癌最常见的病理类型。PTC通常预后良好,但近年来甲状腺癌的发病率逐年攀升。随着患病人数的不断增多,中晚期难治性甲状腺癌患者不再少见。因此,越发庞大的甲状腺癌患者群体的管理与诊治已成为巨大的考验。BRAF V600E基因突变是乳头状癌经典DNA相关标志物,目前已被广泛应用于甲状腺癌的术前诊断和预后评估,并且作为潜在的治疗靶点受到越来越多的关注。因此,正确全面的了解BRAF V600E基因突变可以帮助我们对PTC的发生、发展及生物学行为有更进一步的了解,并为PTC患者管理方式与治疗策略提供新的方向。
BRAF V600E突变;甲状腺乳头状癌;肿瘤发生;侵袭性;预后;生存分析
甲状腺乳头状癌(papillary thyroid cancer,PTC)是甲状腺癌中最常见的病理类型,占所有甲状腺癌的85%~90%。由于其惰性的生物学行为,PTC患者的预后良好,10年疾病总生存率甚至超过9.0%[1]。但近年来甲状腺癌的发病率逐渐攀升,中国的流行病学研究提示,近30年间甲状腺癌的发病率已升高近3倍,2015年中国新发甲状腺癌发病率达到90.0%[2]。此外,晚期难治性甲状腺癌的患者数量亦逐渐增多[3]。因此探寻甲状腺癌发生、发展的关键分子,既有利于甲状腺癌的早期诊断与合理治疗,亦有利于更好的理解常规治疗无效的原因,从而为新技术在晚期甲状腺癌中的应用奠定基础。
目前甲状腺癌相关标志物有许多,其中BRAF V600E基因突变是乳头状癌经典DNA相关标志物。随着分子诊断技术迅猛的发展,它已被广泛应用于甲状腺癌的术前诊断和预后评估。本文将针对乳头状癌BRAF V600E基因突变及其相关研究进展进行综述。
1 PTC中BRAF V600E基因突变及相关通路
1.1 BRAF V600E基因结构及编码蛋白
BRAF又称鼠类肉瘤滤过性毒菌致癌同源体B1,与ARAF及CRAF具有同源性。该基因定位于人染色体7q34,相对分子质量为190×103,含18个外显子,有CR1、CR2和CR3共3个保守区域,含有7个转录区。该基因编码多种蛋白质,包括相对分子质量为94×103、含783个氨基酸残基的BRAF蛋白。该酶属于丝-苏氨酸蛋白激酶类,参与信号通路的转导[4]。
1.2 BRAF V600E基因突变及通路活化
BRAF基因是RET和RAS的下游信号分子,其编码的BRAF蛋白是RAS-RAF-MEK-ERK信号通路的关键要素,该信号通路调节细胞的生长、增殖和凋亡,当其发生变异后可能导致肿瘤的发生。
BRAF突变可发生于11和15外显子,但热点突变为BRAF T1799A点突变,即第1799位点的胸腺嘧啶被腺嘌呤替代,从而导致蛋白质产物中第600位的赖氨酸(V)被谷氨酸(E)替代(V600E,图1)。这一改变导致第599位的苏氨酸活化磷酸化位点附近插入了一个负性调节残基,从而影响了活化片段与结合ATP的P环的连接,从而致使BRAF的活化。该突变体可模拟活化区域的磷酸化过程,经级联式激活通过RASRAF-MEK-ERK信号传导通路引起细胞的异常增殖和分化,最终导致肿瘤的形成[5-6]。
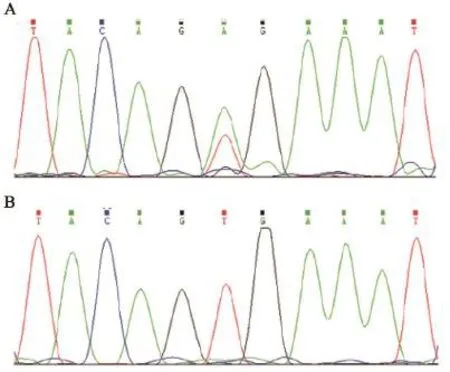
图1 PTC中BRAF T1799A突变(A)和野生型BRAF基因(B)Fig. 1 BRAF T1799A mutation in PTC (A) and wild type BRAF gene (B)
2 BRAF V600E突变在甲状腺结节术前分子诊断中的作用
2015年美国甲状腺协会发布的甲状腺结节术前分子诊断共识[7]指出,BRAF V600E突变对于PTC的诊断、预后及选择合适的治疗方案均具有关键作用。术前穿刺基因诊断可用于甲状腺结节良恶性的鉴别。BRAF V600E突变常用的检测技术包括聚合酶链反应、桑格测序法和焦磷酸测序法等。由于术前细胞学穿刺组织稀少,因此目的基因的检测结果会因组织的获取量多少存在异质性。术前分子检测的出现有效地提高了甲状腺癌的检出率,但分子检测的应用需考虑费用及诊治不足带来的不良后果等因素。目前,BRAF V600E突变检测多应用于甲状腺结节术前细针穿刺细胞学检查(fine-needle aspiration biopsy,FNAB)标本。但有文献报道,单纯的术前FNAB对于甲状腺癌诊断的假阴性率低于3%[8],因此绝大部分患者此时并不需进行分子检测,只有单纯FNAB无法明确诊断或高度怀疑恶性的患者才需要进行。此外,由于BRAF V600E突变与许多临床病理学因素相关,基因诊断在对患者病情全面术前评估中的作用正在探索中。
3 PTC中BRAF V600E基因突变概率及其与临床病理因素和预后的关系
3.1 PTC中BRAF V600E突变情况
据文献报道,BRAF V600E突变在所有恶性实体肿瘤中发生的概率为7%~9%,其中恶性黑色素瘤中的突变概率最高,接近60%[9-13]。PTC被发现为BRAF V600E突变比例较高的实体性肿瘤。由于各个单中心报道中所采用的检测手段、测序方法和组织获取等因素的差异,BRAF V600E突变概率不尽相同。BRAF V600E突变概率为31.3%~86.1%[14-15]。各研究报道的突变概率总结见图2。近年来全球范围内甲状腺癌发病率呈现不断上升的趋势,这其中PTC新发病例的增多占主要原因[16-17]。其中超过50%的乳头状癌为微小乳头状癌(papillary thyroid micro-carcinoma,PTMC),因此如何更好的处理已有且不断增多的PTMC患者成为甲状腺专科医师面临的突出问题。这其中如何理解PTMC的生物学行为起到关键作用。尽管在所有PTC患者中,BRAF V600E基因突变的平均概率达到40%,但在PTMC患者中,其突变概率明显偏低[18],甚至有报道指出,在小于5 mm的PTMC患者中,BRAF V600E基因突变者仅为18%[19-22]。因此对于PTMC患者,BRAF V600E基因突变的识别更有利于危险度分层及个体化治疗方案的选择。
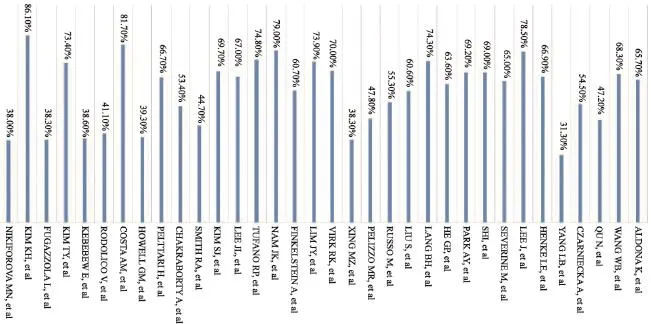
图2 BRAF V600E突变率情况Fig. 2 BRAF V600E mutation rate
3.2 PTC中BRAF V600E突变与临床病理学因素关系研究
众多国内外文献相继报道了PTC中BRAF V600E突变与不良临床病理学因素之间的关系,如疾病晚期、侵袭性特征等,而这些特征已作为PTC危险分层的关键因素被越来越多的评价系统所接纳[23-27]。一系列文献提示,BRAF V600E突变与患者高龄、原发肿瘤较大、经典PTC亚型、原发肿瘤腺外侵犯、多灶性、双侧病灶、初治时局部淋巴结转移、远处转移和TNM高分期等不良因素密切相关[28-33]。BRAF V600E突变与患者性别之间的关联,目前仍有争论[15,32,34-36]。此外,Smith等[32]和Lim等[35]的研究均指出,BRAF V600E突变与合并桥本氏甲状腺炎呈显著负相关,这提示淋巴细胞浸润性炎症与PTC的发生有密切关联。Qu等[9]的一项回顾性研究首次指出,BRAF V600E突变与高体重指数(body mass index,BMI)密切相关,当BMI超过24.9 kg/m2时,BRAF V600E突变风险增加约7.6倍(OR=7.645,95%CI:1.275~45.831)。
BRAF V600E在微小肿瘤中的突变概率偏低,而Virk等[10]及Rodolico等[18]的2项针对PTMC患者的回顾性研究均指出,BRAF V600E突变是区域淋巴结转移的独立预测因素;Lang等[12]在一项纳入845例原发灶小于2 cm的PTC患者的研究中指出,单因素分析提示,BRAF V600E突变与肿瘤大小、原发肿瘤腺外侵犯、淋巴结转移数目、单侧Ⅵ区淋巴结转移数目及Ⅵ区淋巴结转移比例呈正相关(P均<0.001);而校正后的多因素研究提示,BRAF V600E突变仅与中央区淋巴结转移(OR=1.647,95%CI:1.101~2.463)呈显著正相关。Pelttari等[34]的研究关注51例TNM Ⅰ、Ⅱ期的PTC患者,结果显示,BRAF V600E突变与性别、年龄、肿瘤大小、腺外侵犯和区域淋巴结转移均无显著相关性(P>0.05)。因此,BRAF V600E突变在PTMC或早期PTC中的危险预测作用仍需进一步探索。
3.3 PTC中BRAF V600E突变与疾病预后的关系
许多研究认为,BRAF V600E突变与疾病不良预后有关[11,30-31,37]。例如Howell等[11]、Kebebew等[30]、Costa等[31]和Xing等[37]的研究均指出,BRAF V600E突变是PTC复发的独立危险因素;Russo等[38]在研究中指出,生存风险单因素分析结果提示,BRAF V600E突变与肿瘤复发(HR=3.5,95%CI:1.2~10.3)呈正相关,但多因素结果提示,其与肿瘤复发(HR=2.8,95%CI:0.7~11.8)无显著相关性。此外,Fugazzola等[13]、Kim等[15]的研究亦显示,BRAF V600E突变与肿瘤复发无显著相关性。这与各项研究纳入病例数、患者特征及随访时间等因素均有关联。
近期研究提示,在BRAF V600E突变且治疗后复发肿瘤中,碘代谢机制被下调,导致不良预后。可能机制为BRAF V600E突变致MAPK途径下游基因持续激活,引起钠-碘同向转运体(sodium iodide symporter,NIS)的表达稍下降,而NIS的定位异常更为明显,BRAF野生型NIS定位于甲状腺滤泡膜,而BRAF V600E者NIS未能精确定位于细胞膜,更多地弥散分布于细胞质中[36]。另外,垂体瘤转化基因结合因子及转化生长因子β表达增加[39]、TSH受体启动子甲基化等都与BRAF V600E突变致摄碘下降有关。
由PTC引发的肿瘤特异性死亡较为少见。Niederer-Wüst等[40]在回顾性单因素生存分析中发现,BRAF V600E突变与总生存率无显著相关(HR=0.46,95%CI:0.14~1.49),且与肿瘤特异死亡亦无显著相关性。另外几项回顾性研究的结果类似[31,41],但考虑到BRAF V600E突变与肿瘤复发的关联,对于晚期BRAF V600E突变的PTC患者需给于积极治疗以改善预后。
4 结语
综上所述,BRAF V600E突变与PTC的发生、发展及生物学行为存在密切的联系。通过检测患者BRAF V600E突变状态,不仅可以提高术前确诊率,同时可指导PTC的治疗及预后预测。然而,在PTC患者中,BRAF V600E突变检测的应用指征及具体实行策略还需进一步的明确。正确评价BRAF V600E突变与临床病理及预后的关系,可为表达BRAF V600E突变的晚期PTC患者提供新的治疗思路。BRAF V600E突变作为PTC的重要分子标志物,会对其未来的诊疗产生深远的影响。
[1] HUNDAHL S A, FLEMING I D, FREMGEN A M, et al. A National Cancer Data Base report on 53 856 cases of thyroid carcinoma treated in the U.S., 1985-1995[J]. Cancer, 1998, 83(12): 2638-2648.
[2] CHEN W, ZHENG R, BAADE P D. Cancer statistics in China, 2015 [J]. CA Cancer J Clin, 2016, 66(2): 115-132.
[3] PEREZ C A, SANTOS E S, ARANGO B A, et al. Novel molecular targeted therapies for refractory thyroid cancer[J]. Head Neck, 2012, 34(5): 736-745.
[4] COHEN Y, XING M, MAMBO E, et al. BRAF mutation in papillary thyroid carcinoma [J]. J Natl Cancer Inst, 2003, 95(8): 625-627.
[5] XING M, COHEN Y, MAMBO E, et al. Early occurrence of RASSF1A hypermethylation and its mutual exclusion with BRAF mutation in thyroid tumorigenesis [J]. Cancer Res, 2004, 64(5): 1664-1668.
[6] XING M. BRAF mutation in thyroid cancer [J]. Endocr Relat Cancer, 2005, 12(2): 245-262.
[7] FERRIS R L, BALOCH Z, BERNET V, et al. American Thyroid Association statement on surgical application of molecular profiling for thyroid nodules: current impact onperioperative decision making [J]. Thyroid, 2015, 25(7):760-768.
[8] KASPER K A, STEWART J 3rd, DAS K. Fine-needle aspiration cytology of thyroid nodules with Hürthle cells:cytomorphologic predictors for neoplasms, improving diagnostic accuracy and overcoming pitfalls [J]. Acta Cytol, 2014, 58(2): 145-152.
[9] SHI R L, QU N, LIAO T, et al. Relationship of body mass index with BRAF mutation In papillary thyroid cancer [J]. Tumour Biol, 2016, 37(6): 8383-8390.
[10] VIRK R K, VAN DYKE A L, FINKELSTEIN A, et al. BRAF V600E mutation in papillary thyroid microcarcinoma: a genotype-phenotype correlation [J]. Mod Pathol, 2013, 26(1): 62-70.
[11] HOWELL G M, CARTY S E, ARMSTRONG M J, et al. Both BRAF V600E mutation and older age (≥65 years) are associated with recurrent papillary thyroid cancer [J]. Ann Surg Oncol, 2011, 18(13): 3566-3571.
[12] LANG B H, Y J CHAI, B J COWLING, et al. Is BRAF V600E mutation a marker for central nodal metastasis in small papillary thyroid carcinoma?[J]. Endocr Relat Cancer, 2014, 21(2): 285-295.
[13] FUGAZZOLA L, PUXEDDU E, AVENIA N, et al. Correlation between BRAF V600E mutation and clinico-pathologic parameters in papillary thyroid carcinoma: data from a multicentric Italian study and review of the literature [J]. Endocr Relat Cancer, 2006, 13(2): 455-464.
[14] YANG L B, SUN L Y, JIANG Y, et al. The clinicopathological features of BRAF mutated papillary thyroid cancers in Chinese patients [J]. Int J Endocrinol, 2015, 2015: 642046.
[15] KIM T Y, KIM W B, RHEE Y S, et al. The BRAF mutation is useful for prediction of clinical recurrence in low-risk patients with conventional papillary thyroid carcinoma [J]. Clin Endocrinol (Oxf), 2006, 65(3): 364-368.
[16] KENT W D, HALL S F, ISOTALO P A, et al. Increased incidence of differentiated thyroid carcinoma and detection of subclinical disease [J]. CMAJ, 2007, 177(11): 1357-1361.
[17] PAKARINEN M P, RINTALA R J, KOIVUSALO A, et al. Increased incidence of medullary thyroid carcinoma in patients treated for Hirschsprung’s disease [J]. J Pediatr Surg, 2005, 40(10): 1532-1534.
[18] RODOLICO V, CABIBI D, PIZZOLANTI G, et al. BRAF V600E mutation and p27 kip1 expression in papillary carcinomas of the thyroid <or=1 cm and their paired lymph node metastases [J]. Cancer, 2007, 110(6): 1218-1226.
[19] COSKUN A K. The significance of BRAF V600E mutation and preoperative ultrasound for central compartment lymph node metastasis in papillary thyroid microcarcinoma [J]. World J Surg, 2016, 40(3): 759-760.
[20] CHEN Y, SADOW P M, SUH H, et al. BRAF (V600E) is correlated with recurrence of papillary thyroid microcarcinoma:a systematic review, multi-institutional primary data analysis, and Meta-analysis [J]. Thyroid, 2016, 26(2): 248-255.
[21] TALLINI G, DE BIASE D, DURANTE C, et al. BRAF V600E and risk stratification of thyroid microcarcinoma: a multicenter pathological and clinical study [J]. Mod Pathol, 2015, 28(10): 1343-1359.
[22] SUN Y, SHI C, SHI T, et al. Correlation between the BRAF (V600E) gene mutation and factors influencing the prognosis of papillary thyroid microcarcinoma [J]. Int J Clin Exp Med, 2015, 8(12): 22525-22528.
[23] TUTTLE R M, TALA H, SHAH J, et al. Estimating risk of recurrence in differentiated thyroid cancer after total thyroidectomy and radioactive iodine remnant ablation:using response to therapy variables to modify the initial risk estimates predicted by the new American Thyroid Association staging system [J]. Thyroid, 2010, 20(12): 1341-1349.
[24] ITO Y, HIROKAWA M, KIHARA M, et al. Prognostic value of poorly differentiated carcinoma in Japanese Society of Thyroid Surgery in a series of papillary thyroid carcinoma patients:comparison with risk classification system in Kuma Hospital[J]. Endocr J, 2012, 59(9): 817-821.
[25] EBINA A, SUGITANI I, FUJIMOTO Y, et al. Risk-adapted management of papillary thyroid carcinoma according to our own risk group classification system: is thyroid lobectomy the treatment of choice for low-risk patients?[J]. Surgery, 2014, 156(6): 1579-1579.
[26] PITOIA F, JERKOVICH F, URCIUOLI C, et al. Implementing the modified 2009 American Thyroid Association risk stratification system in thyroid cancer patients with low and intermediate risk of recurrence [J]. Thyroid, 2015, 25(11):1235-1242.
[27] YOON J H, LEE H S, KIM E K, et al. Malignancy risk stratification of thyroid nodules: comparison between the thyroid imaging reporting and data system and the 2014 American Thyroid Association management guidelines [J]. Radiology, 2016, 278(3): 917-924.
[28] NIKIFOROVA M N, KIMURA E T, GANDHI M, et al. BRAF mutations in thyroid tumors are restricted to papillary carcinomas and anaplastic or poorly differentiated carcinomas arising from papillary carcinomas [J]. J Clin Endocrinol Metab, 2003, 88(11): 5399-5404.
[29] KIM K H, SUH K S, KANG D W, et al. Mutations of the BRAF gene in papillary thyroid carcinoma and in Hashimoto’s thyroiditis [J]. Pathol Int, 2005, 55(9): 540-545.
[30] KEBEBEW E, WENG J, BAUER J, et al. The prevalence and prognostic value of BRAF mutation in thyroid cancer [J]. Ann Surg, 2007, 246(3): 466-471.
[31] COSTA A M, HERRERO A, FRESNO M F, et al. BRAF mutation associated with other genetic events identifies a subset of aggressive papillary thyroid carcinoma [J]. Clin Endocrinol (Oxf), 2008, 68(4): 618-634.
[32] SMITH R A, SALAJEGHEH A, WEINSTEIN S, et al. Correlation between BRAF mutation and theclinicopathological parameters in papillary thyroid carcinoma with particular reference to follicular variant [J]. Hum Pathol, 2011, 42(4): 500-506.
[33] PELIZZO M R, DOBRINJA C, CASAL IDE E, et al. The role of BRAF (V600E) mutation as poor prognostic factor for the outcome of patients with intrathyroid papillary thyroid carcinoma [J]. Biomed Pharmacother, 2014, 68(4): 413-417.
[34] PELTTARI H, SCHALIN-JANTTI C, AROLA J, et al. BRAF V600E mutation does not predict recurrence after long-term follow-up in TNM stage Ⅰor Ⅱ papillary thyroid carcinoma patients [J]. APMIS, 2012, 120(5): 380-386.
[35] LIM J Y, HONG S W, LEE Y S, et al. Clinicopathologic implications of the BRAF (V600E) mutation in papillary thyroid cancer: a subgroup analysis of 3130 cases in a single center [J]. Thyroid, 2013, 23(11): 1423-1430.
[36] RIESCO-EIZAGUIRRE G, GUTIÉRREZ-MARTÍNEZ P, GARCÍA-CABEZAS M A, et al. The oncogene BRAF V600E is associated with a high risk of recurrence and less differentiated papillary thyroid carcinoma due to the impairment of Na+/I- targeting to the membrane[J]. Endocr Relat Cancer, 2006, 13(1): 257-269.
[37] XING M, LIU R, LIU X, et al. BRAF V600E and TERT promoter mutations cooperatively identify the most aggressive papillary thyroid cancer with highest recurrence [J]. J Clin Oncol, 2014, 32(25): 2718-2726.
[38] RUSSO M, MALANDRINO P, NICOLOSI M L, et al. The BRAF (V600E) mutation influences the short- and mediumterm outcomes of classic papillary thyroid cancer, but is not an independent predictor of unfavorable outcome [J]. Thyroid, 2014, 24(8): 1267-1274.
[39] RIESCO-EIZAGUIRRE G, RODRIGUEZ I, DE LA VIEJA A, et al. The BRAF V600E oncogene induces transforming growth factor beta secretion leading to sodium iodide symporter repression and increased malignancy in thyroid cancer [J]. Cancer Res, 2009, 69(21): 8317-8325.
[40] NIEDERER-WÜST S M, JOCHUM W, FÖRBS D, et al. Impact of clinical risk scores and BRAF V600E mutation status on outcome in papillary thyroid cancer [J]. Surgery, 2015, 157(1): 119-125.
[41] HENKE L E, PFEIFER J D, MA C, et al. BRAF mutation is not predictive of long-term outcome in papillary thyroid carcinoma [J]. Cancer Med, 2015, 4(6): 791-799.
Ef f ects of BRAF V600E mutation on oncogenesis and prognosis in papillary thyroid cancer
ZHANG
Tingting, QU Ning, SHI Rongliang, JI Qinghai (Department of Head and Neck Surgery, Fudan University Shanghai Cancer Center; Department of Oncology, Shanghai Medical College, Fudan University, Shanghai 200032, China)
Papillary thyroid cancer (PTC) is the most common pathological type of thyroid cancer, always with favorable prognosis. However, the incidence of thyroid cancer recently appeared to be an increasing trend. Because of the increased amount of patients, refractory thyroid cancer was not rare anymore. Hence, we are facing a big challenge how to manage and treat the increasing number of patients. BRAF V600E mutation is a classic DNA-relative biomarker for PTC, and widely used in preoperative diagnosis and evaluation of prognosis. As a potential therapeutic target, it attracted more and more attention. Recognizing BRAF V600E mutation can help us to know oncogenesis and biological behavior of PTC better and provide prof i table treatment and management.
BRAF V600E mutation; Papillary thyroid cancer; Oncogenesis; Aggressiveness; Prognosis; Survival analysis
JI Qinghai E-mail: jiqinghai@shca.org.cn
10.19401/j.cnki.1007-3639.2017.06.011
R736.1
A
1007-3639(2017)02-0145-06
2016-09-01
2016-12-10)
嵇庆海 E-mail:jiqinghai@shca.org.cn