Comparison of cognitive flexibility and planning ability in patients with obsessive compulsive disorder, patients with obsessive compulsive personality disorder, and healthy controls
Negin PAAST, Zohreh KHOSRAVI, Amir Hossein MEMARI, Monir SHAYESTEHFAR,Mohammad ARBABI
Comparison of cognitive flexibility and planning ability in patients with obsessive compulsive disorder, patients with obsessive compulsive personality disorder, and healthy controls
Negin PAAST1,2, Zohreh KHOSRAVI2, Amir Hossein MEMARI1,*, Monir SHAYESTEHFAR1,Mohammad ARBABI3
obsessive compulsive disorder; obsessive compulsive personality disorder; executive function;neuropsychology; Iran
1. Introduction
Individuals with obsessive compulsive disorder(OCD) suffer from recurrent intrusive thoughts or images (i.e., obsessions) and ritualistic behaviors (i.e.,compulsions). Individuals with obsessive compulsive personality disorder (OCPD) are preoccupied with mental and interpersonal control and orderliness, and are considered rigid, obstinate, and perfectionistic.These conditions are listed as two separate disorders in both the fourth and fifth editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV,DSM-V),[1,2]but there is, nevertheless, considerable overlap of the core behavioral symptoms for the two conditions.[3]Neurobiological investigations report that specific characteristics of the monoamine neurocircuitry of individuals with OCPD are also seen in individuals with OCD; for example, blunted fenf l uramine-mediated prolactin responses has been reported in both OCPD and OCD, suggesting similarities in the serotonergic processing in these disorders.[4]
Another method for assessing the overlap between OCPD and OCD is to determine whether or not they exhibit similar cognitive profiles.[5]Tükel and colleagues[6]and Kashyap and colleagues[7]found that OCD patients have impairments in working memory, attention,problem solving, visuospatial ability, inhibition, and decision-making. Several studies have focused on impaired cognitive flexibility in OCD[8,9]and in persons with obsessive compulsive personality traits.[10]Other studies have reported impaired problem solving and planning among persons with OCD,[11]findings supported by data from neuroimaging studies which suggest that the impairments in planning in individuals with OCD are associated with frontal lobe dysfunction.[12]
Previous studies of OCPD have focused on population-based samples, so they include few individuals with moderate to severe disability due to their personality disorder. Moreover, several issues about cognitive dysfunction in OCD and OCPD remain controversial. For example, Kuelz and colleagues[12]reported that set shifting and planning abilities might be intact in patients with OCD, and Sasso[13]found no significant correlation between OCPD and cognitive inflexibility. To provide additional information about this issue, the current study enrolled patients with OCPD (i.e., those who are significantly disabled due to the condition) and compared cognitive flexibility and planning ability across three groups of individuals: OCPD patients, OCD patients, and healthy controls.
2. Methods
2.1 Participants

Figure 1. Flowchart of the study
As shown in Figure 1, a total of 98 potential participants were identified from patient records and by using recruitment fliers over a 4-month period at a psychology outpatient clinic specializing in mood and personality disorders in Tehran. These individuals were assessed for eligibility by clinic psychiatrists. Inclusion criteria for the two patient groups included: (a) meets DSM-IV diagnostic criteria for OCD or OCPD (but not both) based on administration of the Structured Clinical Interview for DSM-IV Axis I disorders (SCID-I)[14]and the Structured Clinical Interview for Axis II disorders (SCID-II)[15]; (b)aged 20 to 50 years old; (c) Intelligence Quotient (as assessed using Raven Progressive Matrices[16]) of 85 or higher; (d) had not used any psychotropic medications in the two previous weeks; and (e) no history of serious head injury, neurological disorder, or other co-morbid mental disorder.
Potential control group participants included staff members at Alzahra University and community members recruited through local advertisements. They were asked to complete the self-completion Millon Clinical Multiaxial Inventory-III (MCMI-III)[17]and the Raven Progressive Matrices[16]to exclude individuals with possible personality disorders, mental retardation,or common mental or substance abuse disorders.
Enrolled patients and controls were asked to return to the clinic to complete a battery of psychological measures. All participants received general information about the study and signed an informed consent statement before participating. The study received approval from the ethics committee of Alzahra University.
2.2 Measures
2.2.1 Millon Clinical Multiaxial Inventory-III (MCMI-III)
The MCMI-III[17]is a self-report questionnaire consisting of 175 true-false items which assess 14 DSM-IV Axis II personality disorders and 10 DSM-IV Axis I clinical syndromes. A weighted score that ranges from 0 to 115,the Base Rate Score (BRS), is generated for each of the personality disorders and clinical syndromes: scores between 75 and 84 are classified as ‘traits' and scores of 85 and higher are considered ‘disorders'. In this study this inventory was administered to potential control participants to screen out individuals with possible personality disorders or other common mental disorders such as anxiety, major depression, and somatoform disorders.
2.2.2 Wisconsin Card Sorting Test (WCST)
The WCST[18]has been widely used to examine set shifting or cognitive flexibility. We used a computerized version of WCST-64 and asked participants to sort a series of cards according to one of three possible categories (color, number, or form). We extracted the scores for perseverative errors and for number of categories completed from the WCST for the current analysis.
2.2.3 Tower of London test (TOL)
Planning ability was evaluated by the computerized version of the TOL[19]in which participants were asked to solve a number of problems by moving three colored beads (red, green, and blue) among three sticks with different heights. The test used in this study consisted of 12 trials that required from 2 to 5 moves each; the total number of moves, the total response times, and time of planning (i.e., the time between the start of the trial and the fi rst move) across all 12 trials were the outcome measures used in the current study.
2.2.4 General Health Questionnaire
The GHQ-28[20]was used to measure the level of current psychological distress. It is subdivided into four subscales, including somatic symptoms, anxiety and insomnia, social dysfunction, and depression. Each question was scored from 0-3, with a total possible score ranging of 0-84; a total score of 24 was the cut-offpoint for classifying 'significant social distress'.[21]
2.3 Statistical methods
All analyses were conducted using SPSS 17. Chi-square tests were used to compare the gender and educational status (i.e., with or without college degree) of the three groups of subjects. One-way analysis of variance(ANOVA) was used to compare the age, IQ, and total and subscale scores of the GHQ-28 across the three groups. The two measures from the WCST (considered perseverative errors and categories completed) and the three measures from the TOL (considered total number of moves, total response time, and planning time) were compared using analysis of covariance(ANCOVA) adjusting for age, gender, IQ, educational status, and total score on the GHQ-28. The two WCST measures, which assessed cognitive flexibility, were simultaneously considered in a multivariate analysis of covariance (MANCOVA), and the three TOL measures,which assessed planning ability, were simultaneously considered in a second MANCOVA. Statistical tests were two-tailed and the level of statistical significance was set at p<0.05. Post-hoc comparisons between the OCD, OCPD, and normal control groups were conducted adjusting the level of significance using the Bonferroni correction.
3. Results
As shown in Table 1, there were no statistically significant differences in the gender, age, IQ, or educational attainment of the participants in the three groups.
As expected, patients in the OCD and OCPD groups had significantly higher levels of psychological distress than control group subject (assessed by GHQ-28). This is also the case for the three GHQ-28 subscale scores -somatic symptoms, social dysfunction, and depressive symptoms (Table 2). The total score of the GHQ-28 was significantly higher in the OCD group than in the OCPD group, but this was not the case for any of the subscales.Based on the cutoff for the total GHQ-28 score of 24, 45% (9/20) of OCD patients, 24% (6/25) of OCPD patients, and 4% (1/25) of control subjects had clinically significant psychological distress (X2=10.62, p=0.005).

Table 1. Characteristics of patients with obsessive compulsive disorder (OCD), patients with obsessive compulsive personality disorder(OCPD), and healthy controls

Table 2. General Health Questionnaire (GHQ-28)[20] results of patients with obsessive compulsive disorder (OCD), patients with obsessive compulsive personality disorder(OCPD), and healthy controls
As shown in Table 3, even after adjusting for demographic variables and the level of psychological distress, there were statistically significant differences between the three groups in both measures of cognitive flexibility assessed by the WCST. Follow-up multiple comparison tests found that perseverative errors were significantly more common in the two patient groups than in the control group but not significantly differentfrom each other; the number of categories completed was significantly greater in control group subjects than in OCD patients, but not significantly different from the number of categories completed by OCPD patients.Combining the results for the two measures of cognitive flexibility in a MANCOVA also identified significant differences between the groups (F (4, 132) = 3.79, p=0.006; Wilks' lambda = 0.80).
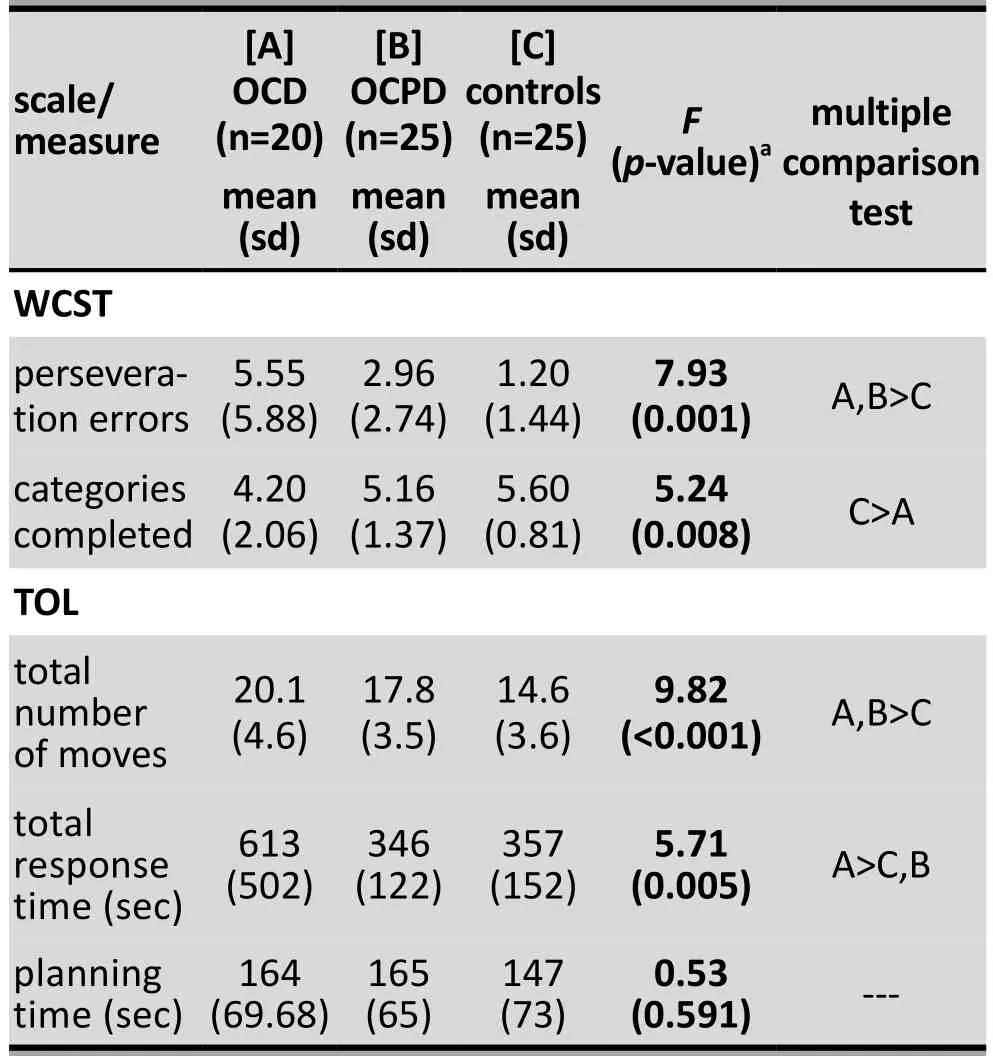
Table 3. Results of Wisconsin Card Sorting Test(WCST)[18] and Tower of London test(TOL)[19] of patients with obsessive compulsive disorder (OCD), patients with obsessive compulsive personality disorder(OCPD), and healthy controls
Table 3 also shows the results of the ANCOVA for the three measures of planning assessed by the TOL.After adjusting for demographic variables and level of distress, there were statistically significant differences between the three groups in the number of moves required to complete the 12 tasks and in the total response time for the 12 tasks, but the differences in the planning time for the 12 tasks were not statistically different across the three groups. Follow-up multiple comparison tests showed that the two patient groups required a significantly greater number of moves to complete the tasks than the control group, but the number of moves used by the OCD and COPD patient groups was not statistically different. Unexpectedly, the time required to complete the tasks in the OCD group was significantly greater than that required both by the control group and by the OCPD group, but there was no significant difference in response time between the OCPD and control groups. Combining the results for the three measures of planning ability in a MANCOVA, there were significant differences between the three groups (F[6, 130] = 4.87, p < 0.001; Wilks' lambda = 0.66).
4. Discussion
4.1 Main finding
As expected, we found that persons with OCD and OCPD experience significantly higher levels of psychological distress than individuals without mental disorders. We also found that the overall level of distress was greater among individuals with OCD than among individuals with OCPD.
There are several studies that assess the relationship between OCD and OCPD[3-5]but, to our knowledge, this is the first study that compares the cognitive flexibility and planning ability of OCD and OCPD patients to that of healthy controls. We found that after adjusting for demographic variables and severity of overall distress, OCD patients had significantly worse functioning than normal controls on both measures of cognitive flexibility assessed by the WCST and on two of the three measures of planning ability assessed by the TOL. OCPD patients also had worse functioning than normal controls on one of the two measures of cognitive flexibility and on one of the three measures of planning ability. The overall psychological distress reported by OCD patients on the GHQ-28 was greater than that reported by OCPD patients, and for one of the fi ve cognitive measures considered - total responsetime on the TOL - OCD patients were significantly more impaired than OCPD patients; but none of the other four cognitive measures showed significant differences between the two patient groups.
Our findings are in agreement with previous published studies which examined cognitive flexibility in patients with OCD. Tükel and colleagues[6]reported that OCD patients, independent of medication use,show high numbers of perseverative errors and low numbers of completed categories when completing the WCST. A recent study examining the neuropsychological characteristics of a community-based sample reported that individuals with OCPD have significant cognitive inflexibility and executive planning deficits, though their decision-making abilities are intact.[22]Studies of clinical samples report that individuals with obsessivecompulsive personality traits underperform on specific executive function tests related to set-shifting and planning abilities.[10]Another report found that individuals with co-morbid OCD and OCPD had more impaired cognitive flexibility than those with OCD without co-morbid OCPD,[4]suggesting that cognitive inflexibility is a symptom of both OCD and OCPD, and that the severity of the cognitive impairment parallels the clinical severity of the obsessive compulsive symptoms.
Our results about planning ability in OCD and OCPD are also in line with previous studies, but there are some unique results in our study.[9]Both groups of patients required more moves to complete the twelve TOL tasks than healthy controls, indicating that their ability to plan and resolve complex problems was impaired. Despite this poorer performance, the OCD patients also took significantly longer to complete the tasks than controls,suggesting that they think much longer than others before trying a complex task. Thus the need to perform tasks based on a ‘perfect standard' and the intolerance of uncertainly often reported in OCD patients[22,23]may be associated with the cognitive dysfunction reported among these patients. However, our study found that despite their relatively poor performance on the TOL tasks, OCPD patients did not take longer to complete the tasks than control subjects and, in fact, completed the tasks significantly faster than OCD patients.
Recent brain imaging studies[24,25]report similar changes in the activity of several brain regions (e.g.,the dorsolateral prefrontal cortex and the orbitofrontal cortex) of both OCD and OCPD patients while preforming tasks that require cognitive flexibility, planning ability,and decision making ability. These findings appear to support the hypotheses that the underlying mechanisms in both clinical disorders are similar. But our detailed assessment of cognitive flexibility and planning ability identified differences between the two conditions which suggest that additional, as yet unknown,condition-specific factors influence the relationship between obsessive compulsive symptoms and cognitive functioning.
4.2 Limitations
The present study had some limitations that should be noted. First, the sample size was relatively small, so the failure to identify differences between OCD and OCPD patients on several of the measures may have been due to Type II errors. Second, we used a relatively limited number of cognitive measures that may not have assessed all aspects of cognitive flexibility and planning ability, and definitely did not include other aspects of cognitive functioning that may be impaired in OCD and OCPD. Third, individuals with OCD, OCPD, and other mental disorders were excluded from the control group based on a self-completion measure (MCMI-III) which may not have identified all such individuals. Finally, the study did not include a control group of individuals with co-morbid OCD-OCPD, so it was not possible to assess the increased (or decreased) effect of the comorbid condition on cognitive functioning.
Future studies should recruit larger samples,include a comorbid OCD-OCPD group, conduct a more comprehensive neuropsychiatric battery, and follow subjects over time to assess the evolution of the cognitive impairment as the obsessive compulsive symptoms wax and wane.
4.3 Implications
We found significant impairments in the cognitive flexibility and planning ability of patients with OCD and OCPD, even after adjusting for demographic factors and the patients' level of psychological distress.Defects in cognitive flexibility and planning abilities are potential neurocognitive fingerprints for obsessive compulsive disorders that may have diagnostic value and treatment implications, because they could be employed as measures of changes in the functional severity of the disorders over time and with treatment.However, further work, particularly long-term followup studies that monitor changes in cognitive function and obsessive compulsive symptoms, will be needed to clarify whether or not such neurocognitive measures are of practical value. Interestingly, OCPD patients appeared relatively unaffected in some aspects of cognitive functioning, highlighting a potential area of difference with OCD that deserves further study. Importantly, in our study, the neurocognitive profile was examined in a medication-free group of participants, and, thus, our results were not confounded by the potential effects of medication on cognitive functioning.
Funding
This study received no funding.
Conflict of interest statement
All authors declare that they have no conflict of interest related to this manuscript.
Informed consent
All participants provided written informed consent to participate in the study.
Ethics approval
All procedures performed in this study were approved by the ethics committee of Alzahra University.
Authors' contributions
NP and ZH conceived and designed the study and acquired the data. NP, AHM, and MS analyzed and interpreted the data. NP, AHM, and MS drafted the manuscript. The manuscript was critically revised by AHM and MA. All authors read and approved the final version of the manuscript.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington,DC: American Psychiatric Publishing; 1994
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlingtion, VA:American Psychiatric Publishing; 2013
3. Garyfallos G, Katsigiannopoulos K, Adamopoulou A, Papazisis G, Karastergiou A, Bozikas VP. Comorbidity of obsessivecompulsive disorder with obsessive-compulsive personality disorder: does it imply a specific subtype of obsessivecompulsive disorder? Psychiatry Res. 2010; 177(1-2): 156-160. doi: http://dx.doi.org/10.1016/j.psychres.2010.01.006
4. Fineberg NA, Sharma P, Sivakumaran T, Sahakian B,Chamberlain SR. Does obsessive-compulsive personality disorder belong within the obsessive-compulsive spectrum?CNS Spectr. 2007; 12(6): 467-482
5. Pinto A, Liebowitz MR, Foa EB, Simpson HB. Obsessive compulsive personality disorder as a predictor of exposure and ritual prevention outcome for obsessive compulsive disorder. Behav Res Ther. 2011; 49(8): 453-458. doi: http://dx.doi.org/10.1016/j.brat.2011.04.004
6. Tükel R, Gürvit H, Ertekin BA, Oflaz S, Ertekin E, Baran B, et al. Neuropsychological function in obsessive-compulsive disorder. Compr Psychiatry. 2012; 53(2): 167-175. doi:http://dx.doi.org/10.1016/j.comppsych.2011.03.007
7. Kashyap H, Kumar JK, Kandavel T, Reddy YC.Neuropsychological functioning in obsessive-compulsive disorder: are executive functions the key deficit? Compr Psychiatry. 2013; 54(5):533-540.doi: http://dx.doi.org/10.1016/j.comppsych.2012.12.003
8. Meiran N, Diamond GM, Toder D, Nemets B. Cognitive rigidity in unipolar depression and obsessive compulsive disorder: examination of task switching, Stroop, working memory updating and post-conflict adaptation. Psychiatry Res. 2011; 185(1-2): 149-156. doi: http://dx.doi.org/10.1016/j.psychres.2010.04.044
9. Krishna R, Udupa S, George CM, Kumar KJ, Viswanath B, Kandavel T, et al. Neuropsychological performance in OCD: a study in medication-naïve patients. Prog Neuropsychopharmacol Biol Psychiatry. 2011; 35(8): 1969-1976. doi: http://dx.doi.org/10.1016/j.pnpbp.2011.09.009
10. García-Villamisar D, Dattilo J. Executive functioning in people with obsessive-compulsive personality trait: evidence of modest impairment. J Pers Disord. 2013; 29(3): 418-430. doi:http://dx.doi.org/10.1521/pedi_2013_27_101
11. Ruocco AC, Rodrigo AH, Lam J, Di Domenico SI, Graves B,Ayaz H. A problem-solving task specialized for functional neuroimaging: validation of the Scarborough adaptation of the Tower of London (S-TOL) using near-infrared spectroscopy. Front Hum Neuroci. 2014; 8: 185. doi: http://dx.doi.org/10.3389/fnhum.2014.00185
12. Kuelz AK, Hohagen F, Voderholzer U. Neuropsychological performance in obsessive-compulsive disorder: a critical review. Biol Psychol. 2004; 65(3): 185-236. doi: http://dx.doi.org/10.1016/j.biopsycho.2003.07.007
13. Sasso L, Cheryl A. Exploring the relationship between neurocognitive personality traits. Pepperdine University Dissertation; 2007
14. First MB, Spitzer RL, Gibbon ML, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P) New York: Biometrics Research, New York State Psychiatric Institute; 2002
15. First MB, Gibbon ML, Spitzer RL, Williams JB, Benjamin LS.Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II). Washington, DC: American Psychiatric Press, Inc.; 1997
16. Raven J, Raven JC, Court JH. Manual for Raven's Progressive Matrices and Vocabulary Scales, Section 1: General Overview. San Antonio, TX: Harcourt Assessment; 1998
17. Millon T. Millon Clinical Multiaxial Inventory-III Manual (3rd ed). MN, Minneapolis: NCS Pearson; 2006
18. Heaton SK, Chelune GJ, Talley JL, Kay GG, Curtiss G.Wisconsin Cart Sorting Test Manual: Revised and Expanded.Odessa, FL: Psychological Assessment Resources; 1993
19. Culbertson W, Zillmer E. Tower of London-Drexel University.Technical manual. 2nded. Toronto: Multi-Health Systems;2005
20. Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med. 1979; 9(1): 139-145.doi: http://dx.doi.org/10.1017/S0033291700021644
21. Sterling M. General Health Questionnaire-28 (GHQ-28). J Physiother. 2011; 57(4): 259. doi: http://dx.doi.org/10.1016/S1836-9553(11)70060-1
22. Fineberg NA, Day GA, de Koenigswarter N, Reghunandanan S,Kolli S, Jefferies-Sewell K. The neuropsychology of obsessivecompulsive personality disorder: a new analysis. CNS Spectr.2015; 20(5): 490-499. doi: http://dx.doi.org/10.1017/S1092852914000662
23. Ciarrochi J. When simplifying life is not so bad: the link between rigidity, stressful life events, and mental health in an undergraduate population. British Journal Of Guidance& Counseling. 2005; 33(2): 185-197.doi: http://dx.doi.org/10.1080/03069880500132540
24. Olley A, Malhi G, Sachdev P. Memory and executive functioning in obsessive-compulsive disorder: a selective review. J Affect Disord. 104(1-3): 15-23. doi: http://dx.doi.org/10.1016/j.jad.2007.02.023
25. Cavedini P, Zorzi C, Piccinni M, Cavallini MC, Bellodi L.Executive dysfunctions in obsessive-compulsive patients and unaffected relatives: searching for a new intermediate phenotype. Biol Psychiatry. 2010; 67(12): 1178-1184. doi:http://dx.doi.org/10.1016/j.biopsych.2010.02.012
(received, 2015-11-16; accepted, 2016-01-15)

Negin Paast obtained her master's in clinical psychology in 2014 from Alzahra University, Iran. She is currently a PhD candidate in Research Psychology in the Neuroscience Institute, Tehran University of Medical Sciences. She is also currently working with the Personality Disorders Research Group and in the Neurosis and Personality Disorders Unit. Her research interests are psychopathology and personality disorders, social cognition, and psychological assessment.
强迫症患者、强迫型人格障碍患者和健康对照者之间的认知灵活性和计划能力比较
Paast N, Khosravi Z, Memari A, Shayestehfar M, Arbabi M
强迫症;强迫型人格障碍;执行功能;神经心理学;伊朗
Background:Cognitive functioning in individuals with Obsessive Compulsive Disorder(OCD) and with Obsessive Compulsive Personality Disorder (OCPD) has not been adequately studied.Aim:Examine the cognitive flexibility and planning ability of individuals with OCD and OCPD.Methods:Twenty patients with OCD and 25 patients with OCPD who had not taken medication in the previous two weeks were identified in an outpatient psychology clinic in Tehran, and 25 healthy control subjects were identified from the university staff and local community residents. All participants were administered the 28-item version of the General Health Questionnaire (GHQ-28), the Wisconsin Card Sorting Test (WCST), and the Tower of London (TOL) test. Two measures of the WCTS (number of perseverative errors and number of categories completed) were used to assess cognitive flexibility and three measures of the TOL (total number of moves in 12 trials, total response time, and planning time) were used to assess planning ability.Results:The level of current psychological distress in the two patient groups was significantly greater than that in the control group. After adjusting for demographic variables and the level of psychological distress,both OCD patients and OCPD patients made more perseverative errors on the WCST than control subjects,and the OCD patients (but not the OCPD patients) completed significantly fewer categories than the control subjects. Both the OCD patients and OCPD patients required significantly more moves than control subjects to complete the 12 TOL tasks and OCD patients took significantly longer than both OCPD patients and control subjects to complete the tasks.Conclusions:Individuals with OCD and OCPD have impaired cognitive flexibility and planning ability compared to healthy controls, and there are some differences in these measures of cognitive functioning between OCD and OCPD. Long term follow-up studies of OCD and OCPD that assess changes in cognitive measures as the severity of obsessive compulsive symptoms wax and wane will be needed to determine whether or not such cognitive measures have diagnostic or clinical relevance for obsessive compulsive disorders.
[Shanghai Arch Psychiatry. 2016; 28(1): 28-34.
http://dx.doi.org/10.11919/j.issn.1002-0829.215124]
1Neuroscience Institute, Sports Medicine Research Center, Tehran University of Medical Sciences, Tehran, Iran
2Department of Psychology, Alzahra University, Tehran, Iran
3Psychiatry and Psychology Research Center, Tehran University of Medical Sciences, Tehran, Iran
*correspondence: Dr. Amir-HosseinMemari, NO 7. Jalale Ale Ahmad Highway , PO Box: 14395-578, Tehran, Iran. E-mail: amirmemari@farabi.tums.ac.ir
A full-text Chinese translation of this article will be available at http://dx.doi.org/10.11919/j.issn.1002-0829.215124 on May 25, 2016.
背 景:强 迫 症 患 者 (Obsessive Compulsive Disorder,OCD) 与强迫型人格障碍患者 (Obsessive Compulsive Personality Disorder, OCPD) 的认知功能还没有得到充分的研究。目标:验证OCD和OCPD患者的认知灵活性和计划能力。方法:本研究在德黑兰心理咨询门诊选定了25例OCD患者和20例OCPD患者,他们在既往两周都没有服药,并且从大学工作人员和当地社区居民中选定了25名健康对照者。对所有参与者均进行28项一般健康问卷 (28-item version of the General Health Questionnaire, GHQ-28)、 威 斯 康 星 卡 片 分 类 测 验(Wisconsin Card Sorting Test, WCST)、 和 伦 敦 塔 试 验(Tower of London test, TOL))。本研究运用 WCTS 的两个测量指标(持续错误数和完成分类数)评估认知灵活性以及TOL的三个测量指标(12个试验总共的移动次数、总应答时和计划时间)评估计划能力。结果:2组患者的当前心理困扰程度显著高于对照组。在控制人口学因素和心理困扰水平后,OCD患者和OCPD患者在WCST测试中比对照组更容易出现持续性错误,而OCD患者(不包括OCPD患者)的完成分类数比对照组显著减少。OCD患者和OCDP患者都比对照组需要更多的移动次数来完成12项TOL任务,并且OCD患者比OCPD患者和对照组需要花更长的时间来完成任务。结论:与健康对照组相比,OCD和OCPD患者的认知灵活性和计划能力都有所受损,并且OCD和OCPD患者之间的认知功能测试也存在一些差异。我们需要对OCD和OCPD患者进行长期随访研究评估在强迫症状严重性加重与减轻时认知功能的改变,从而决定此类认知评估指标对于强迫症是否有诊断或临床关联性。
本文全文中文版从2016年5月25日起在
http://dx.doi.org/10.11919/j.issn.1002-0829.215124 可供免费阅览下载
- 上海精神医学的其它文章
- Relationships among three popular measures of differential risks: relative risk, risk difference, and odds ratio
- Case report of a child's anxiety disorder precipitated by tremors from a distant earthquake that was extensively covered in local news stories
- Case report of body dysmorphic disorder in a suicidal patient
- Inf l uence of cross-disorder analyses on the diagnostic criteria of mental illnesses
- Genetic findings are challenging the symptom-based diagnostic classification system of mental disorders
- Cross-sectional study of the severity of self-reported depressive symptoms in heroin users who participate in a methadone maintenance treatment program