Cross-sectional study of the severity of self-reported depressive symptoms in heroin users who participate in a methadone maintenance treatment program
Yafei WU, Shiyan YAN, Yanping BAO, Zhi LIAN, Zhi QU, Zhimin LIU,*
Cross-sectional study of the severity of self-reported depressive symptoms in heroin users who participate in a methadone maintenance treatment program
Yafei WU1, Shiyan YAN3, Yanping BAO2, Zhi LIAN2, Zhi QU2, Zhimin LIU2,*
methadone maintenance treatment; heroin abuse; depression; China
1. Introduction
Heroin use is a global public health problem that seriously affects the users themselves, their families,and the economic and social stability of their communities. Chronic use of heroin can directly cause physical problems and is often associated with comorbid psychiatric disorders, particularly depression.[1-4]Methadone maintenance treatment (MMT) is a widely recognized method for reducing narcotic addiction that involves the long-term use of methadone to reduce cravings for narcotics combined with various psychological and behavioral treatments aimed at restoring social functioning.[5]The present study compares the severity of depressive symptoms between heroin users currently participating in voluntary outpatient MMT programs in nine locations around China to that of heroin users who have registered at the clinics but have not yet started MMT.
2. Methods
2.1 Participants
As shown in Figure 1, the selected participants were heroin users from nine voluntary outpatient methadone clinics in three cities - seven clinics in Xi'an (Shaanxi Province), one clinic in Beijing, and one clinic in Taiyuan(Shanxi Province). The participants were either already receiving MMT in October 2012 (the MMT group) or newly enrolled patients at the clinics (from October 2012 to April 2014) who had not yet started the MMT program (untreated group). Participants in both groups meet screening criteria for the outpatient use of MMT in heroin users in China:[6](a) 20 years of age or older;(b) registered as a permanent resident of the local community; (c) had full legal capacity for civil conduct;( d) had two court-imposed periods of compulsory drug rehabilitation or one period of ‘re-education through labor' (i.e., legal incarceration for drug abusers); and (e)provided written informed consent to participate in the study.
2.2 Intervention
The MMT at the nine clinics was provided by clinicians who had been trained to provide MMT according to national standards established by experts in the China Drug Dependence Center.[7]This involves the administration of daily doses of 10 to 100 mg of methadone that is directly observed by the treating clinician. All the patients in MMT group had at least one month of MMT treatment before enrollment in the study; at the time of enrollment their mean (sd)duration of MMT treatment was 8.9 (3.7) months and their mean MMT dosage was 47.7 (22.2) mg/d.
The protocol for this project was approved by the Ethics Committee of Beijing University. Informed consent was obtained from all participants.
2.3 Assessment
We developed an expanded demographic and current treatment form to collect information on the demographic characteristics and pattern of heroin use of participants. We also administered the short 13-item version of the Beck Depression Inventory (BDI-13),[8]which has been shown to have good reliability and validity when evaluating the severity of depression in substance abusers.[9]The BDI items are scored on 4-point Likert scales (0-4) resulting in a range in total scores of 0 to 52, with higher scores representing more severe depression. Total scores of 0 to 4 indicate no depression,scores of 5 to 7 indicate mild depression, scores of 8 to 15 indicate moderate depression, and scores of 16 or more indicate serious depression.
2.4 Statistical analysis

Figure 1. Flowchart of patient enrollment in the study
Epidata (version 3.1) was used to double enter the data, and SPSS 11.3 was used to conduct the statistical analysis. Chi-square tests, t-tests, and rank tests were used to compare characteristics between the two groups. We used Spearman correlation coefficients to assess the relationship between the duration of MMT treatment and the severity of depression in the treated group. We used multivariate linear regression analysis to identify the factors independently associated with the severity of depressive symptoms. All statistical tests were two-tailed and the level of statistical significance was set at p<0.05.
3. Results
There were 929 patients in the MMT treatment group and 238 in the untreated group who completed the assessment; completion rates in the two groups were 95.9% (929/969) and 97.1% (238/245), respectively.As shown in Table 1, there were several statistically significant differences in the characteristics of the two groups. Compared to individuals in the untreated group, individuals in the MMT group were less likely tobe male, were older, had a higher level of education,were less likely to be married, were more likely to be unemployed, had lower monthly incomes, and reported poorer family relationships.

Table 1. Comparison of the demographic characteristics of heroin users who are or are not enrolled in an outpatient methadone maintenance treatment (MMT) program
As shown in Table 2, the total daily dose of heroin at the time of enrollment in the MMT program was similar in the two groups, but the average single dose of heroin and the maximum single dose of heroin in the week prior to enrollment was greater in the MMT group than in the untreated group. However, the duration of heroin use and the frequency of daily use were greater in untreated individuals than in treated individuals.
The BDI-13 score was not normally distributed, so we used rank tests and Chi-squares to compare results between groups. Both analyses show that the reported severity of depressive symptoms was significantly greater in the untreated group than in the treated group. Among the 929 patients in the MMT group,longer participation in MMT was associated with lower scores on the BDI-13 (rs=-0.24, Z=2.88, p=0.004).
We considered the treatment status and all assessed sociodemographic variables in a multivariate linear regression analysis (n=1138) to determine which variables were independently associated with the reported severity of depression. As shown in Table 3,depressive symptoms were significantly more severe in persons who reported poor family relationships, in persons in the untreated group, and in persons who were divorced. Other variables, including gender, age,educational level, income level, and employment status were not independently associated with the selfreported severity of depressive symptoms.
4. Discussion
4.1 Main findings
We found that the prevalence of depressive symptoms among heroin users (79% in the untreated group and 68% in the MMT group) is much higher than in the general population,[10]a finding that is similar to several other studies of substance users.[11]The depressive symptoms frequently reported by heroin users include pessimism, dissatisfaction, guilt, self-denial, work-related difficulty, fatigue, and anorexia.[12]These symptoms can be exacerbated immediately after drug withdrawal and by social-environmental stressors including the stigma and discrimination that many drug abusers must often endure.[13]Several studies have shown that depressive and anxiety symptoms in heroin users are important causes of relapse after detoxification,[14]so addressing these symptoms needs to be a key component of drug rehabilitation programs.
We also found that reported depressive symptoms among heroin users engaged in a MMT program were less severe than the depressive symptoms reported by heroin users who are not engaged in a MMT program,and that this difference persists after controlling for key demographic variables. Moreover, individuals who had participated in the MMT program longer had less severe depressive symptoms than individuals who only recently started participating in the MMT program, suggesting -but not proving - that MMT was having a positive effect on participants' depressive symptoms. A similar study by Brienza and colleagues among 528 heroin users found that the rates of depression among individuals receiving MMT were lower than those of attendeesat a Needle Exchange Program (NEP).[15]A one-year follow-up treatment study[16]of adjunctive treatment with MMT and rehabilitation therapy (without a control group) in 485 heroin users reported that the prevalence of core depressive symptoms dropped from 26% to 11%over the course of treatment.

Table 2. Characteristics of heroin use and depressive symptoms among heroin users who are or are not enrolled in an outpatient methadone maintenance treatment (MMT) program
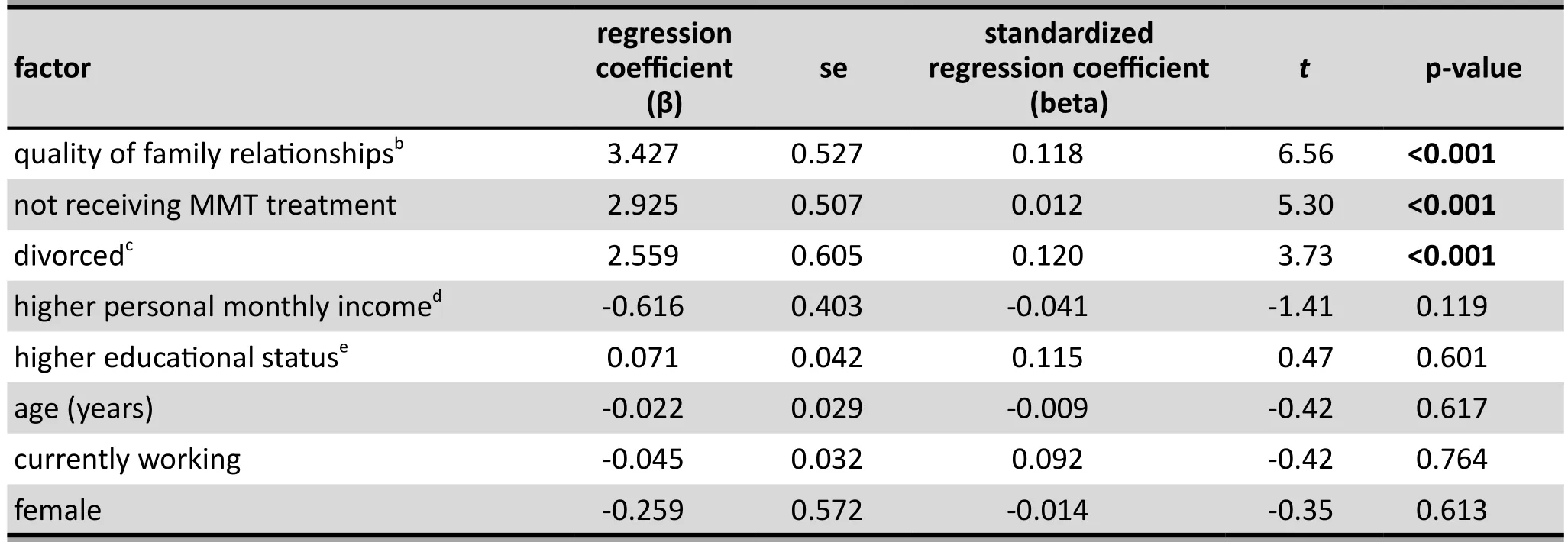
Table 3. Multivariate linear regression of factors associated with total score of the 13-item Beck Depression Inventory (BDI-13)[7] among 1138 heroin users in Chinaa
Our findings that divorce and poor family relationships are associated with more severe depressive symptoms in individuals who use heroin, a finding that remains robust even after adjusting for the effect of participating in a MMT program, highlight the importance of addressing environmental stressors while using methadone to reduce the physical addiction.Some studies[17]report that providing psychological support to spouses and family members of heroin users both reduces the stress experienced by the family members and promotes the social rehabilitation and quality of life of the patient.
4.2 Limitations
There are several limitations with the study that need to be considered. (a) Individuals included in the study voluntarily entered a MMT program after having participated in court-mandated compulsory treatment(which is typically a minimum of two years in China),so they have long histories of heroin use (10 years on average) and, thus, are not representative of individuals who have only recently started using heroin. (b) The level of use of heroin was assessed at the time of enrollment in the MMT program in both groups; for the untreated group the BDI-13 evaluated the level of depression at the same time period (i.e., depression at the time of enrollment), but for the MMT group the BDI-13 assessed the individual's level of depression on average 9 months after the time of enrollment.This made it impossible to correlate the heroin use variables (other than the total duration of use) to the level of depression or to include these variables in the multiple linear regression model. (c) There were major unexplained differences in the demographic and heroin use variables between the two groups. Even though we controlled for these variables in the linear regression, these differences may reflect underlying differences in the groups that could have confounded the results about depression between the groups. (d)The prior treatment history of participants was not considered. (e) No formal diagnosis was conducted to distinguish patients who did and did not meet formal diagnostic criteria for depression. Finally, (f) this was a cross-sectional study, so the identified relationships are associations, not causal; we cannot conclude the MMT treatment improves depression in heroin users, we can only conclude that MMT is associated with lower levels of depression in heroin users. Randomized controlled studies are needed to determine whether or not MMT actually improves the depressive symptoms of persons who use heroin.
4.3 Importance
We found that concurrent depression is common in individuals who seek outpatient treatment for heroin addiction in China. Individuals who are participating in the comprehensive methadone maintenance therapy programs in China report substantially less severe depressive symptoms than heroin users who have enrolled in MMT programs but have not yet started the treatment. Poor family relationships (including divorce) magnify the depressive symptoms experienced by heroin users, so programs aimed at rehabilitating heroin users need to develop and test creative ways for improving the emotional re-integration of heroin users back into their families after their physical addiction is under control.
Acknowledgement
We appreciate the support of the nine collaborative methadone maintenance clinics that participated in this study: the Beijing No.1 Methadone Maintenance Treatment Clinic; the 109 Hospital in Taiyuan, Shanxi Province; the No.1 Methadone Maintenance Treatment Clinic of Xi'an Mental Health Center, Xian, Shaanxi Province; the No.2 Methadone Maintenance Treatment Clinic of Xi'an Mental Health Center, Xian, Shaanxi Province; the Methadone Maintenance Treatment Clinic in Xincheng District, Xian, Shaanxi Province; the Methadone Maintenance Treatment Clinic of Baqiao District Traditional Medicine Hospital, Xian, Shaanxi Province; the Drug Maintenance Clinic in Beilin District,Xian, Shaanxi Province; the Methadone Maintenance Treatment Clinic in Lianhu District Rehabilitation Hospital, Xian, Shaanxi Province; and the Tie Ta Si Clinic of Xi'an Red Cross Hospital, Xian, Shaanxi Province.
Funding
This study was supported by the ‘Shi'er Wu' project of the Ministry of Science and Technology of the People's Republic of China (project number: 2012BAI01B07).
Conflict of interest statement
The authors declare no conflict of interest in the preparation of this manuscript.
Informed consent
Every outpatient who participated in this study signed a consent form at the beginning of the study.
Ethics approval
The biomedicine ethics committee of Peking University approved the study (approval number: 000010-13020).
Authors' contributions
WY was in charge of drafting the manuscript and gathering data; YS and QZ were in charge of quality control while gathering the data; LZ and BY were in charge of processing the data; and LZ was the principal investigator for the study; and all authors read and approved the final manuscript.
1. Christine B, Gillian T. Randomized controlled trial of motivational interviewing, cognitive behavior therapy,and substance use disorders. Am J Psychiatry. 2001;158(10): 1706-1713. doi: http://dx.doi.org/10.1176/appi.ajp.158.10.1706
2. Hill HE, Haertzen CA, Glaser R. Personality characteristics of narcotic addicts as indicated by the MMPI. J Gen Psychol.1960; 62: 127-139
3. Weissman MM, Slobetz F, Prusoff B, Mezritz M, Howard P.Clinical depression among narcotic addicts maintained on methadone in community. Am J Psychiatry. 1976; 133(12):1434-1438. doi: http://dx.doi.org/10.1176/ajp.133.12.1434
4. Ghaffari-Nejad A, Shahabi K. The relationship between heroin withdrawal signs and symptoms and existence of depression. Arch Iran Med. 2005; 8(2): 115-118
5. Minister of Health. Methadone Maintenance Treatment.Ottawa: Health Canada; 2002
6. Ministry of Public Security, State Food and Drug Administration. [Notice on the "Treatment program of the opioid addicts patients in the community"]. Beijing: Disease Control and Prevention, No. 256; 2006. Chinese
7. Lai WS. [Methadone dosage introduction and regulation for patients on methadone maintenance treatment]. Zhongguo Yao Wu Yi Lai Xing Za Zhi. 2008; 17(3): 201-203. Chinese
8. Zhang MY. [Handbook of Psychiatric Rating Scale]. Hunan:Hunan Science and Technology Press; 1998. p. 283, 631, 721.Chinese
9. Beck AT,Beamsderfer A. Assessment of depression:the depression inventory. In: Pichot P, Karger ROS, ed.Psychological measurement in psychopharmacology.Switerland: Basel; 1974. p. 151-169
10. Golin S, Hartz MA. A factor analysis of Beck Depression Inventory in a mildly depressed population. J Clin Psychol.1979; 35(2): 322-325
11. Ryan CF, White JM. Health status at entry to methadone maintenance treatment using the SF-36 health survey questionnaire. Addiction. 1996; 91 (1): 39-45. doi: http://dx.doi.org/10.1046/j.1360-0443.1996.911397.x
12. Conner KR, Pinquart M, Holbrook AP. Meta-analysis of depression and substance use and impairment among cocaine users. Drug Alcohol Depend. 2008; 98: 13-23. doi:http://dx.doi.org/10.1016/j.drugalcdep.2008.05.005
13. Conner KR, Pinquart M, Duberstein PR. Meta-analysis of depression and substance use and impairment among intravenous drug users (IDUS). Addiction. 2008;103: 524-534. doi: http://dx.doi.org/10.1111/j.1360-0443.2007.02118.x
14. Li QH, Yao P, Li F, Li QH. [Impact of psychological intervention for the spouse of patients with heroin dependence].Zhongguo Yao Wu Yi Lai Xing Za Zhi. 2009; 18(5): 438-440.Chinese
15. Brienza R, Stein M, Chen M, Gogineni A, Sobota M,Maksad J. Depression among needle exchange program and methadone maintenance clients. J Subst Abuse Treat.2000; 18(4): 331-337. doi: http://dx.doi.org/10.1016/s0740-5472(99)00084-7
16. Havard A, Teesson M, Darke S, Ross J. Depression among heroin users: 12-month outcomes from the Australian Treatment Outcome Study (ATOS). J Subst Abuse Treat.2006; 30(4): 355-362. doi: http://dx.doi.org/10.1016/j.jsat.2006.03.012
17. Li XD, Wen H, Peng BY, Feng ZY, Zeng LN, Wei YA, et al.[Re-discussion of the cause of relapse to drug abuse].Zhongguo Yao Wu Lan Yong Fang Zhi Za Zhi. 2003; 9(3): 49-51. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1006-902X.2003.03.017
(received, 2015-12-04; accepted, 2015-01-15)

Dr. Yafei Wu received a bachelor's degree in 1998 and a master's degree in public health in 2008 from Xi'an Jiao Tong University Health Science Center. Since 1998 she has been working at the Department of Preventive Medicine in the School of Nursing at Weinan Vocational and Technical College. She is currently an associate professor and the deputy party secretary in the School of Nursing, and she also holds a concurrent post as a health consultant for the Weinan's Daily, a local newspaper. Her main research interest is the control of cardiovascular disease.
参与美沙酮维持治疗的海洛因成瘾者自我报告的抑郁症状严重程度:一项横断面调查
吴亚飞,闫世艳,鲍艳萍,连智,曲直,刘志民
美沙酮维持治疗;海洛因滥用;抑郁;中国
Background:Methadone maintenance treatment (MMT) is widely recognized as an effective method of combatting narcotic addiction. MMT reduces heroin withdrawal symptoms and, thus, makes it possible to provide the psychological and social support that is essential to the rehabilitation of drug users.Aim:Compare the severity of depressive symptoms in heroin users who are currently receiving MMT to that of heroin users who are not receiving MMT.Methods:We administered the 13-item version of the Beck Depression Inventory (BDI-13) and a demographic history form to 929 heroin users who had been receiving MMT at nine methadone treatment clinics in three Chinese cities for an average of 9 months and to 238 heroin users who had enrolled in a MMT program at the centers but had not yet begun MMT.Results:Seventy-nine percent (188/238) of the untreated individuals reported depressive symptoms compared to 68% (628/929) of the individuals receiving MMT (X2=11.69, p<0.001). The median (interquartile range) BDI score in the untreated group was 10.4 (7.9-11.4) compared to 8.0 (5.7-11.6) in the MMT group(Z=2.75, p=0.006). In the MMT group, there was a negative correlation between the severity of reported depressive symptoms and the duration of participation in the MMT program (rs=-0.24, Z=2.88, p=0.004).Multivariate linear regression analysis showed that after adjusting for all demographic variables the treated group still had less severe depressive symptoms than the untreated group. After adjusting for the effect of MMT treatment, depressive symptoms were more severe in heroin users who self-reported poor family relationships (standardized regression coefficient [beta]=0.118, t=6.56, p<0.001) and in those who were divorced (beta=0.120, t=3.73, p<0.001).Conclusions:Moderate to severe depressive symptoms are common in heroin users. MMT is associated with lower levels of depressive symptoms in heroin users, but prospective randomized controlled trials are needed to determine whether or not MMT actually improves depressive symptoms in heroin users.Poor relationships with family members are also associated with depressive symptoms in heroin users; this suggests that treatment of heroin addiction needs to incorporate methods for helping heroin users repair the severed social relationships that their addiction has caused.
[Shanghai Arch Psychiatry. 2016; 28(1): 35-41.
http://dx.doi.org/10.11919/j.issn.1002-0829.215127]
1Weinan Vocational and Technical College, Shanxi, China
2China Academy of Chinese Medical Sciences, Beijing, China
3National Institute on Drug Dependence, Peking University, Beijing, China
*correspondence: Dr. Zhimin Liu, Beijing University Drug Dependence Research Institute, 38 Xueyuan Road, Beijing 100083, China.E-mail: zhiminliu@bjmu.edu.cn
A full-text Chinese translation of this article will be available at http://dx.doi.org/10.11919/j.issn.1002-0829.215127 on May 25, 2016.
背景:美沙酮维持治疗 (methadone maintenance treatment, MMT) 是一种公认的有效降低毒瘾的措施。美沙酮维持治疗可以减少海洛因成瘾戒断症状,并因此可以提供心理和社会支持,对吸毒者的康复至关重要。目标:比较目前正在接受MMT的海洛因成瘾者和没有接受MMT的海洛因成瘾者之间的抑郁症状严重程度。方法:本研究运用了Beck-13 (13-item version of the Beck Depression Inventory, BDI-13) 抑郁自评量表和人口学历史资料调查表,对中国三个城市9个美沙酮治疗中心的929例正在接受MMT的海洛因成瘾患者(平均已接受9个月MMT治疗)和已经在中心注册参加MMT治疗但尚未开始的238例海洛因成瘾患者进行评估。结果:与正在接受MMT的成瘾者中有68% (628 / 929)报告抑郁症状相比,79% (188/238) 的未治疗成瘾者报告有抑郁症状 (X2=11.69, p<0.001)。未经治疗组的 BDI评分中位数(四分位区间)是10.4 (7.9-11.4),而MMT组BDI评分中位数是8.0 (5.7-11.6),两者有显著差异(Z=2.75, p=0.006)。在 MMT组内,自我报告的抑郁症状严重程度与参加 MMT 时间呈负相关 (rs=-0.24, Z=2.88,p=0.004)。多元线性回归分析发现,在控制所有人口学变量后,治疗组的抑郁症状严重程度仍然轻于非治疗组。在控制MMT疗效后,自我报告家庭关系较差(β= 0.118, t=6.56, p<0.001) 以 及 离 异 (β= 0.120, t=3.73,p<0.001) 的海洛因成瘾患者抑郁症状较严重。结论:中度至重度抑郁症状常见于海洛因成瘾患者。MMT治疗与海洛因成瘾患者抑郁症状较轻相关,但需要采用前瞻性随机对照试验来确定MMT是否确实改善了海洛因成瘾患者的抑郁症状。与家庭成员的关系较差也与海洛因成瘾患者的抑郁症状有关,这表明对海洛因成瘾患者的治疗需要纳入一些方法来帮助海洛因成瘾患者修复由于他们成瘾造成的社会关系割裂。
本文全文中文版从2016年5月25日起在
http://dx.doi.org/10.11919/j.issn.1002-0829.215127 可供免费阅览下载
- 上海精神医学的其它文章
- Relationships among three popular measures of differential risks: relative risk, risk difference, and odds ratio
- Case report of a child's anxiety disorder precipitated by tremors from a distant earthquake that was extensively covered in local news stories
- Case report of body dysmorphic disorder in a suicidal patient
- Inf l uence of cross-disorder analyses on the diagnostic criteria of mental illnesses
- Genetic findings are challenging the symptom-based diagnostic classification system of mental disorders
- Comparison of cognitive flexibility and planning ability in patients with obsessive compulsive disorder, patients with obsessive compulsive personality disorder, and healthy controls