每周单次皮下注射rhPTH(1-34)促进大鼠的骨折愈合
马腾, 张稳, 郭琦, 海宝,刘灿,宋纯理
(北京大学第三医院骨科,北京 100191)
每周单次皮下注射rhPTH(1-34)促进大鼠的骨折愈合
马腾, 张稳, 郭琦, 海宝,刘灿,宋纯理*
(北京大学第三医院骨科,北京 100191)
目的 观察每周单次皮下注射甲状旁腺激素rhPTH(1-34)促进大鼠骨折愈合的效果。方法 50只3月龄雄性SD大鼠左侧胫骨骨折,克氏针内固定术后,根据皮下注射rhPTH(1-34)的剂量及频次,随机分为5组(n=10/组):每周10、20 μg/kg组;每日10、20 μg/kg组;每周皮下注射等量(500 μL)生理盐水作为对照组。治疗4周后处死取材,分别行小动物X线、双能X线、micro-CT及三点弯曲生物力学实验检测骨折愈合情况。结果 无论每周或每日皮下注射rhPTH(1-34)骨密度均高于对照组(P<0.05);每周20 μg/kg组骨折愈合效果好于对照组,其中rhPTH(1-34)每周20 μg/kg组在骨密度、矿化的骨痂体积、骨痂总体积、矿化的骨痂体积占骨痂总体积百分数、最大载荷方面分别比对照组高26.2%、51.4%、21.6%、24.5%、29.3%。每周20 μg/kg、每日10 μg/kg及每日20 μg/kg组的最大载荷均高于对照组(P<0.01);每周20 μg/kg组骨密度、骨微结构、力学强度均与每日10 μg/kg组无统计学差异(P>0.05)。结论 每周皮下注射甲状旁腺激素(rhPTH1-34)(10、20 μg/kg)可以促进骨折愈合,但相同单次剂量,每日皮下注射的效果仍优于每周皮下效果。
甲状旁腺激素片段;骨折愈合;每周给药;每日给药;大鼠
甲状旁腺激素(parathyroid hormone)是骨代谢和骨稳态的重要调节激素。PTH刺激骨形成与骨吸收提高骨转换(bone turnover)。不同剂量或给药间隔对骨量增加或减少产生截然不同的骨骼生物学效应,持续高剂量应用PTH促进骨吸收,而间歇性应用PTH则促进骨形成[1]。目前基因重组人甲状旁腺激素(rhPTH 1-34,商品名特立帕肽)作为一种治疗骨质疏松的药物进入临床应用,对于严重的绝经期骨质疏松的治疗具有非常好的治疗效果,可以增加骨量,减少骨折风险。有研究报道:临床上每日皮下注射rhPTH(1-34)20 μg/d可以治疗骨质疏松[2, 3];每周皮下注射一次rhPTH(1-34)可以治疗骨质疏松[4, 5]。同时有研究报道皮下注射rhPTH(1-34)可以促进骨折愈合[6, 7]。rhPTH(1-34)作为生物制剂价格昂贵,并且具有一些副作用,如果每周一次皮下注射rhPTH也能促进骨折愈合,无疑将具有重要的研究价值。本文主要研究每周皮下注射一次rhPTH(1-34)是否可以促进骨折愈合,并与每日一次皮下注射rhPTH(1-34)对骨折愈合促进的作用效果进行比较。
1 材料与方法
1.1 实验动物
选用SPF级雄性SD大鼠50只,平均体重(312 ± 2.2)g,3月龄。购自北京维通利华实验动物技术有限公司【SCXK(京)2012-0001】。饲养于北京大学医学部实验动物科学部【SYXK(京)2011-0039】。按照实验动物使用的“3R”原则给与人道关怀。1.2 药品与试剂
甲状旁腺激素:基因重组人rhPTH(1-34)多肽片段(teriparatide),规格20 μg/80 μL,2.4 mL/支,礼来(中国)公司生产,批号S20110021。
1.3 手术操作与分组
50只SD大鼠适应性喂养两周后,用10%的水合氯醛3.3 mL/kg 体重腹腔内注射麻醉,麻醉后,左侧膝关节前正中纵切口,暴露向外侧牵开髌韧带,于胫骨平台接近髌韧带处开一个小口,显露胫骨中段,然后用电锯将胫骨中段锯断,用直径1 mm的柯氏针进行髓内针固定[8-10]。根据皮下注射rhPTH(1-34)的剂量及频次,随机分为5组(n=10/组):每周10、20 μg/kg、每日10、20 μg/kg组及每周皮下注射等量(500 μL)生理盐水作为对照组。术后四周处死所有大鼠,取材,-80℃冰箱保存待测。
1.4 X射线检测
分别于手术后1周、2周、 4周,10%的水合氯醛(3.3 mL/kg)腹腔内注射麻醉后,对大鼠左侧胫骨进行小动物X线(高频便携式X射线机北京朗安影像技术公司,中国)检查(60 kVp,5 mA)。
1.5 左侧胫骨骨密度(bone mineral density, BMD)测量
用双能X线骨密度仪(Hologic Discovery,美国)在高分辨率和小型动物扫描模式下评定左侧胫骨(n=6/组)的骨密度(mg/cm2)。设定感兴趣区(region of interesting, ROI)为胫骨干中段0.8 cm×1 cm的区域的矩形,与位于中心的横向骨折线垂直,利用去除内固定软件,扫描后得到的BMD值将用于数据分析。
1.6 Micro-CT扫描与重建分析
将左侧胫骨标本沿长轴垂直固定于样品固定器内,应用小动物micro-CT(Inveon, Siemens Medical Solutions USA, Inc., IL, USA),在相同条件下对大鼠胫骨标本进行三维 CT扫描重建,扫描的各项参数设置如下:空间分辨率 18 μm,电压 600 kV,电流300 μA,扫描时间 900 ms。扫描完成后,分别选取胫骨骺线以下100个层面的松质骨为第一个感兴趣区域(volume of interest,VOI)[11];选取以骨折线为中心,上下各100个层面(共计3.6 mm)的骨痂为第二个VOI[12],使用micro-CT自带的软件进行定量分析。物理参数分析如下:骨小梁数量(trabecular number, Tb.N)、骨小梁厚度(trabecular thickness, Tb.Th)、骨小梁分离度(trabecular separation, Tb.Sp)、骨矿化百分数(BV/TV)、矿化的骨痂体积(mineralized callus volume, BVcallus)、骨痂总体积(total callus volume, TVcallus)、矿化的骨痂体积占骨痂总体积百分数(BVcallus/TV callus)。
1.7 骨生物力学检测
将-80℃保存的胫骨4℃过夜,常温解冻,生理盐水复湿。根据文献报道的方法[13],仔细旋转拔出克氏针,标本置于生物力学试验机(Landmark, MTS Inc., Eden Prairie, MN, USA)上进行三点弯曲生物力学实验,加载速度为0.01 mm/s,跨距为15 mm。量取骨干正中的内外径,由载荷,桡度换算并绘制应力-应变曲线,从曲线上读取及计算最大强度(maximum strength)[13, 14]。
1.8 统计学分析
采用SPSS 13.0统计软件包进行数据处理,所有数据以均值±标准差表示。组间数据比较采用One-Way ANONA方差分析(One-Way ANONA followed by the LSD post hoc test)和LSD检验,以P<0.05为统计学显著性差异。
2 结果
2.1 X线检查
术后第1、2、4周,X线结果显示,皮下注射rhPTH(1-34)显著促进大鼠胫骨骨折愈合。术后4周,rhPTH(1-34)每周20 μg/kg组和rhPTH(1-34)每日10 μg/kg组以及rhPTH(1-34)每日20 μg/kg组的骨折线几乎消失,而对照组还有骨痂存在(图1)。
皮下注射rhPTH(1-34)每周20 μg/kg组骨折愈合速度快于rhPTH(1-34)每周10 μg/kg组和对照组;而皮下注射rhPTH(1-34)每周20 μg/kg组骨折愈合速度和皮下注射rhPTH(1-34)每日10 μg/kg组相当。

注:A.对照组; B.每周10 μg/kg;C:每周20 μg/kg;D: 每日10 μg/kg;E:每日20 μg/kg。(其他图注同图1)。图1 不同组别骨折术后1、2、4周X线检查结果Note: A. Control group. B.10 μg/kg per week group. C.20 μg/kg per week group. D.10 μg/kg per day group. E.20 μg/kg per day group.(Other notes are the same as in Fig.1)Fig.1 X-ray of fractured tibias at 1,2, and 4 weeks after operation.
2.2 骨密度检测结果
rhPTH(1-34)每周20 μg/kg组的骨密度高于对照组和rhPTH(1-34)每周10 μg/kg组(P<0.05)。rhPTH(1-34)每周20 μg/kg组的骨密度和rhPTH(1-34)每日10 μg/kg组相比差异无显著性(P>0.05);但仍低于rhPTH(1-34)每日20 μg/kg组(P<0.05)(图2)。
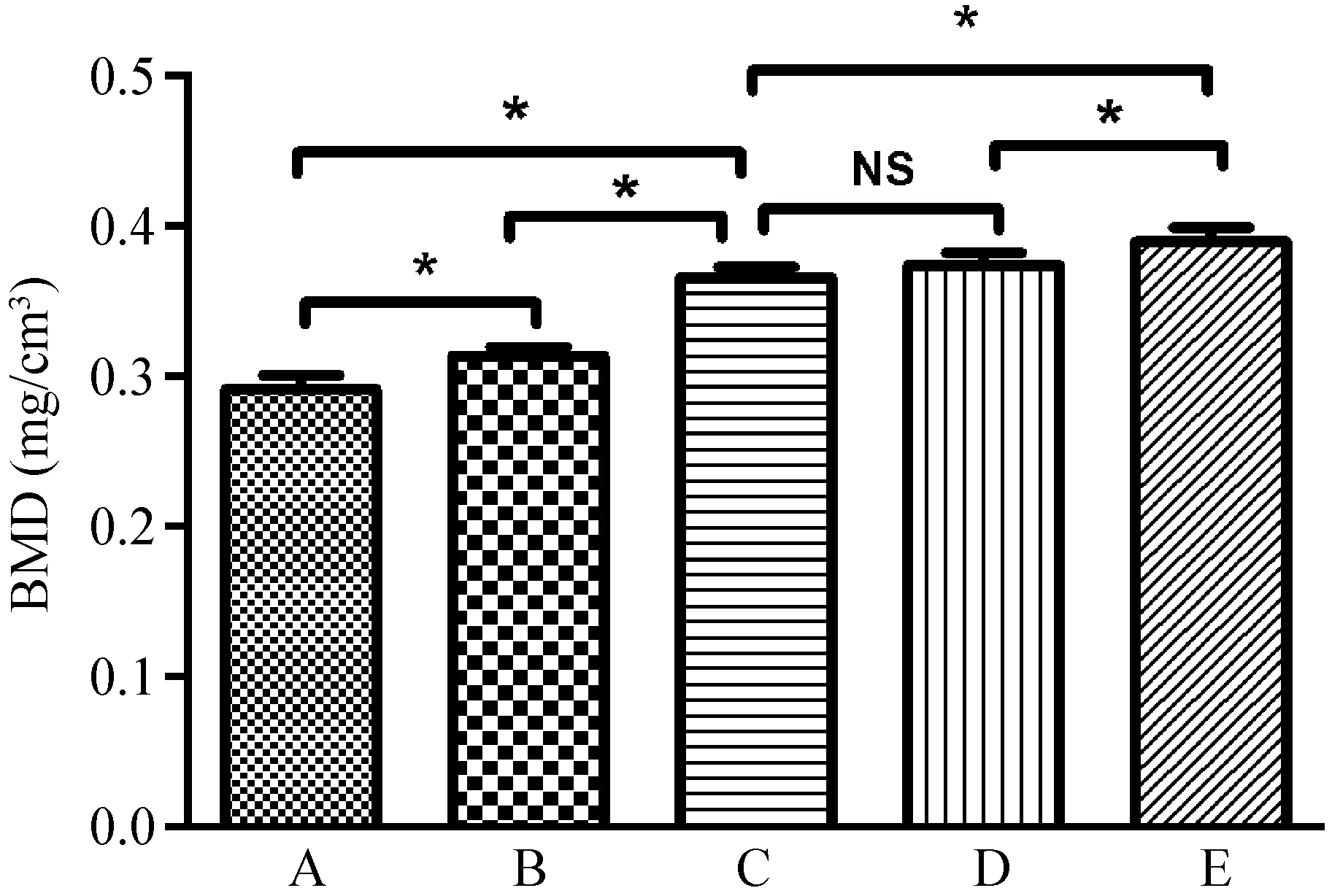
图2 各组胫骨骨密度检测结果(n=6,*P<0.05)Fig.2 BMD of fractured tibias at 4 weeks after operation
2.3 Micro-CT检测结果
Micro-CT扫描的截面图,肉眼清晰可见rhPTH(1-34)每周20 μg/kg组骨折愈合效果好于对照组和rhPTH(1-34)每周10 μg/kg组,rhPTH(1-34)每周20 μg/kg组骨折愈合效果和rhPTH(1-34)每日10 μg/kg组相当(图3)。Micro-CT扫描的三维立体图,肉眼清晰可见rhPTH(1-34)每周20 μg/kg组骨折愈合效果好于对照组和rhPTH(1-34)每周10 μg/kg组,rhPTH(1-34)每周20 μg/kg组骨折愈合效果和rhPTH(1-34)每日10 μg/kg组相当(图4)。
胫骨近端micro-CT定量分析显示,rhPTH(1-34)每周20 μg/kg组松质骨的骨小梁数量、骨小梁厚度比对照组高,差异有显著性(P<0.05)。rhPTH(1-34)每周20 μg/kg组松质骨的骨小梁数量、骨小梁厚度和rhPTH(1-34)每日10 μg/kg组差异无显著性(P>0.05)。rhPTH(1-34)每周20 μg/kg组松质骨的骨小梁分离度比对照组高,差异有显著性(P<0.05)。rhPTH(1-34)每周20 μg/kg组松质骨的骨小梁骨小梁分离度和rhPTH(1-34)每日10 μg/kg组相差无几,差异无显著性(P>0.05)(图5)。
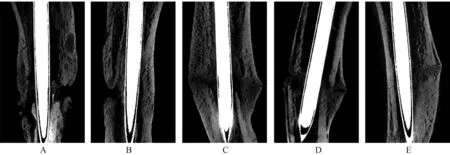
图3 Micro-CT扫描形成的截面图Fig.3 Micro-CT longitudinal profiles of fractured tibias at 4 weeks after operation
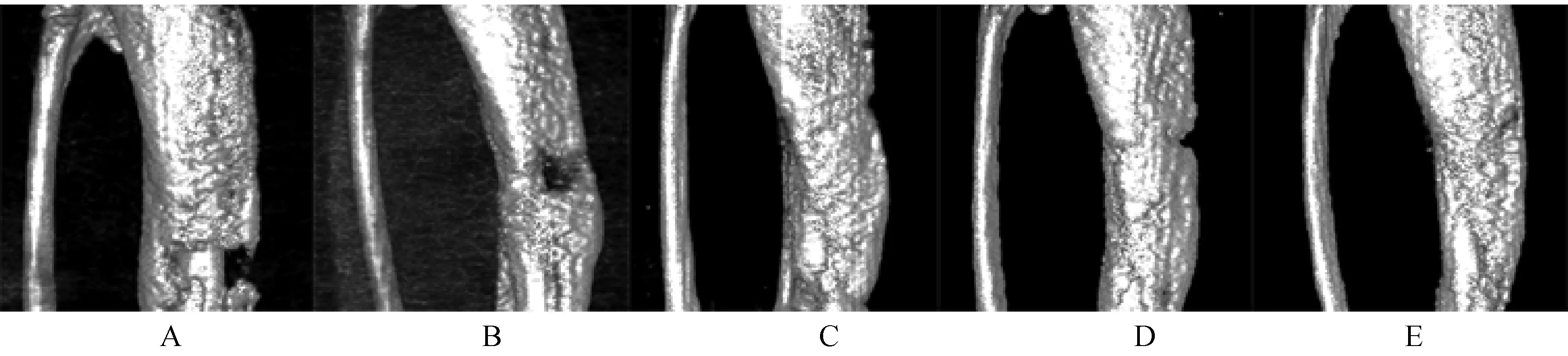
图4 Micro-CT扫描形成的三维立体图Fig.4 3D micro-CT reconstruction of fractured tibias at 4 weeks after operation
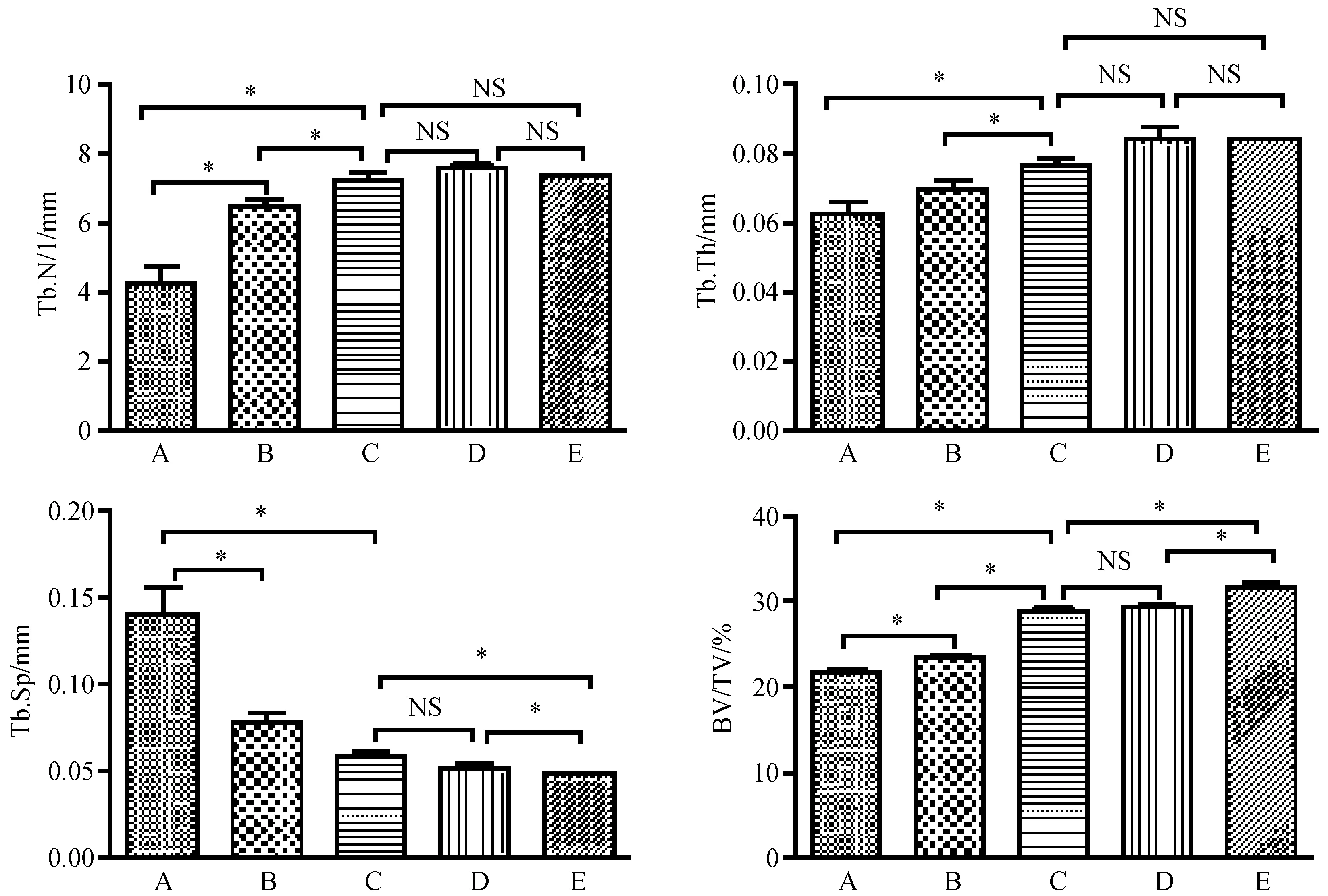
图5 术后4周各组micro-CT定量检测指标(n=6,*P<0.05)Fig.5 Parameters of the micro-structure of cancellous bone of each group
胫骨骨折周围micro-CT定量分析显示,rhPTH(1-34)每周20 μg/kg组的矿化的骨痂体积、骨痂总体积、矿化的骨痂体积占骨痂总体积百分数比对照组高,差异有显著性(P<0.05)。rhPTH(1-34)每周20 μg/kg组的矿化的骨痂体积、骨痂总体积、矿化的骨痂体积占骨痂总体积百分数和rhPTH(1-34)每日10 μg/kg组差异无显著性(P>0.05)。rhPTH(1-34)每日 20 μg/kg组的骨痂体积、骨痂总体积、矿化的骨痂体积占骨痂总体积百分数高于rhPTH(1-34)每周20 μg/kg组和rhPTH(1-34)每日10 μg/kg组,差异有显著性(P<0.05)(图6)。
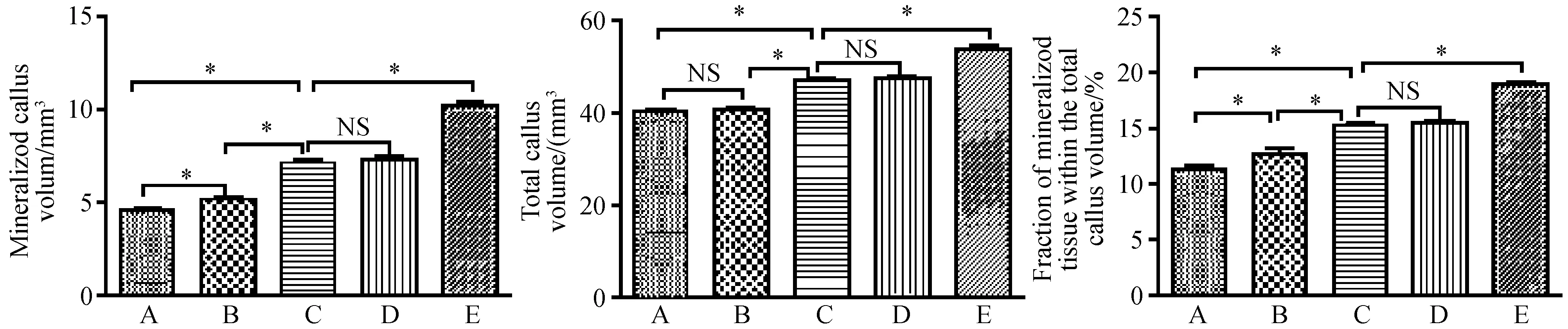
图6 术后4周各组micro-CT定量检测指标(n=6,*P<0.05)Fig.6 Parameters of the micro-structure of callus in each group
2.4 大鼠胫骨三点弯曲生物力学
三点弯曲生物力学实验显示,rhPTH(1-34)每周20 μg/kg组的最大载荷高于对照组和每周10 μg/kg组,差异有显著性(P<0.05)。rhPTH(1-34)每周20 μg/kg组的最大载荷和每日10 μg/kg组相差无几,差异无显著性(P>0.05)。rhPTH(1-34)每日20 μg/kg组的最大载荷高于每周20 μg/kg组和每日10 μg/kg组,差异有显著性(P<0.05)(图7)。
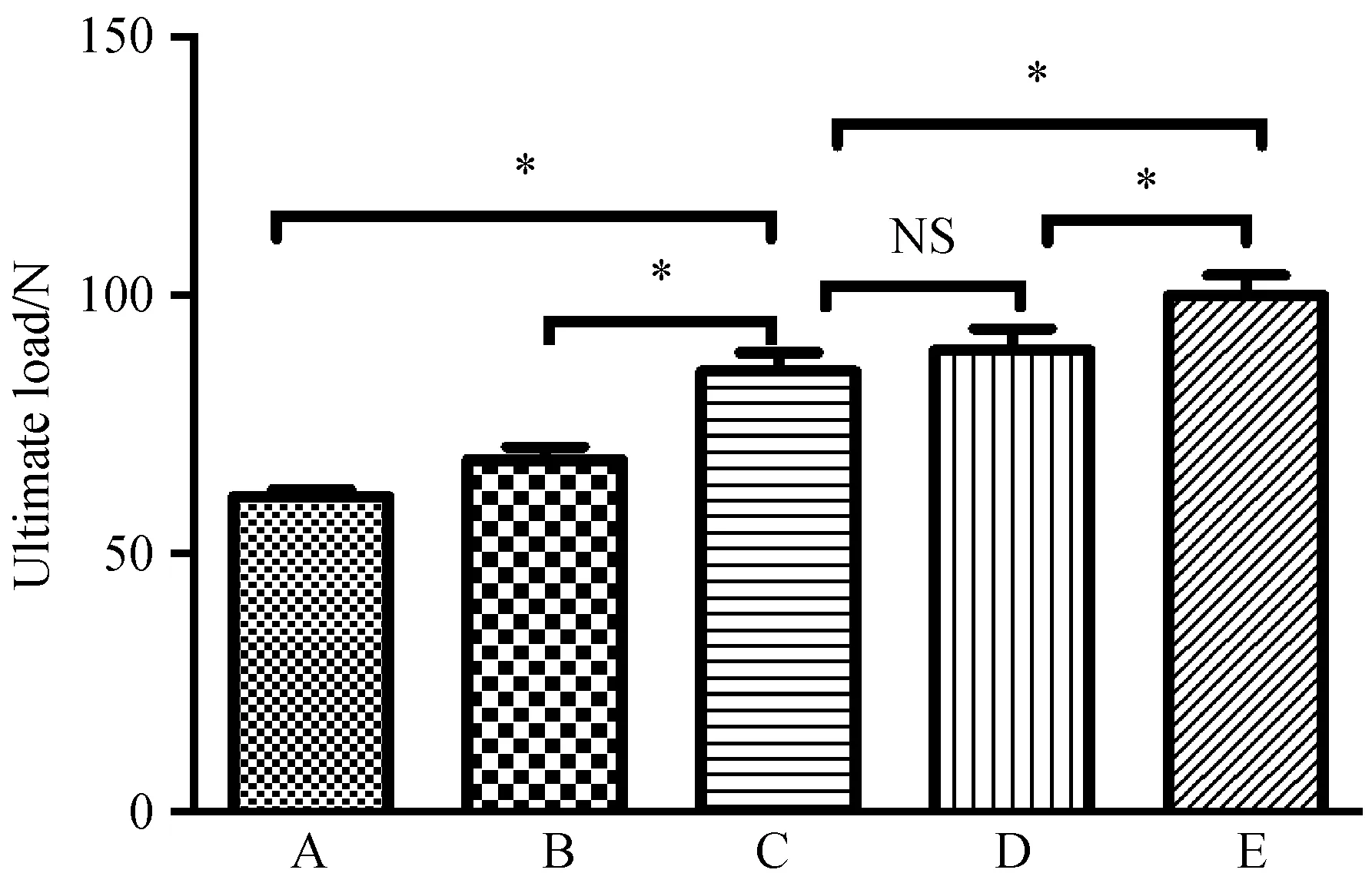
图7 术后4周各组左侧胫骨最大载荷(N,n=6,*P<0.05)Fig.7 Ultimate load of fractured tibias in each group
3 讨论
骨折是临床上的常见的骨骼系统损伤。伴随着内固定器材和手术技术的发展,采用手术进行内固定在一定程度上促进了骨折愈合。骨骼虽然是一种具有再生能力的器官,但因骨代谢周期长,骨折愈合缓慢,并且大约有5%~10%的骨折最终发展为延迟愈合甚至不愈合。如何促进骨折愈合具有重要的现实意义,目前常用的作用于骨代谢的治疗药物多是抑制骨吸收[15],如何促进骨形成、增加骨量、促进骨折愈合的治疗手段较少。
甲状旁腺激素(parathyroid hormone)可以刺激成骨,间歇性使用甲状旁腺激素可以促进骨形成。有文献报道,甲状旁腺激素作为一种生物制剂每日皮下注射甲状旁腺激素可以治疗骨质疏松。目前基因重组的人类甲状旁腺激素片段(商品名特立帕肽,rhPTH 1-34)作为一种治疗骨质疏松的药物进入临床应用阶段,对于绝经期骨质疏松的治疗具有非常好的治疗效果,可促进骨形成。目前临床上使用rhPTH(1-34)治疗严重骨质疏松常用的使用方法是皮下注射20 μg /d[16, 17]。近年来,有研究报道,每周一次皮下注射rhPTH(1-34)也可以促进骨形成,治疗骨质疏松[18-20]。
在本研究中,通过X线影像学证实,每周一次注射rhPTH(1-34)可以显著促进骨折愈合。Micro-CT检测进一步证实每周一次rhPTH(1-34)不仅可以增加胫骨近端松质骨的骨量、改善骨微结构,还可以促进骨折愈合,骨折断端的骨痂形成增多,更重要的是,在生物力学测试中,皮下注射rhPTH(1-34)每周20 μg/kg组最大载荷力和皮下注射rhPTH(1-34)每日10 μg/kg组相当,均明显优于生理盐水对照组。因此,每周皮下注射甲状旁腺激素20 μg/kg能够产生和每日皮下注射甲状旁腺激素10 μg/kg相当的治疗效果,且每周给皮下注射甲状旁腺激素20 μg/kg和每日皮下注射甲状旁腺激素10 μg/kg均表现出好于皮下注射生理盐水组的效果。
甲状旁腺激素可以刺激骨形成与骨吸收提高骨转换。不同剂量或给药间隔产生截然不同的骨骼生物学效应:持续高剂量应用PTH促进骨吸收,而间歇性应用PTH则促进骨形成。其作用机制尚不清楚。甲状旁腺激素的成骨作用机制主要是以下几个方面:促进成骨细胞增殖和分化[21, 22],抑制成骨细胞凋亡[23],刺激经典Wnt/β-catenin通路[24]。本研究发现,虽然每周皮下注射rhPTH(1-34)20 μg/kg可显著促进骨折愈合,但与每日皮下注射rhPTH(1-34)20 μg/kg仍有一定的差异,说明每周皮下注射甲状旁腺激素的剂量仍然是一个值得进一步深入探讨的科学问题。
总之,本研究发现每周皮下注射rhPTH(1-34)可显著促进骨折愈合,相比每日皮下注射,不仅可以减少每日注射的繁琐,更重要的是,降低了rhPTH(1-34)的使用量,治疗费用将大大减少,具有良好的经济效益。
[1] Lotinun S, Sibonga JD, Turner RT. Differential effects of intermittent and continuous administration of parathyroid hormone on bone histomorphometry and gene expression[J]. Endocrine. 2002. 17(1):29-36.
[2] Chen JF, Yang KH, Zhang ZL, et al. A systematic review on the use of daily subcutaneous administration of teriparatide for treatment of patients with osteoporosis at high risk for fracture in Asia[J]. Osteoporos Int. 2015. 26:11-28.
[3] Qiu Z, Wei L, Liu J, et al. Effect of intermittent PTH (1-34) on posterolateral spinal fusion with iliac crest bone graft in an ovariectomized rat model[J]. Osteoporos Int. 2013. 24:2693-2700.
[4] Ito M, Oishi R, Fukunaga M, et al. The effects of once-weekly teriparatide on hip structure and biomechanical properties assessed by CT[J]. Osteoporos Int. 2014. 25:1163-1172.
[5] Gittens SA, Wohl GR, Zernicke RF, et al. Systemic bone formation with weekly PTH administration in ovariectomized rats[J]. J Pharm Pharm Sci. 2004. 7:27-37.
[6] Zhang D, Potty A, Vyas P, et al. The role of recombinant PTH in human fracture healing: a systematic review[J]. J Orthop Trauma. 2014. 28:57-62.
[7] Liu A, Li Y, Wang Y, et al. Exogenous parathyroid hormone-related peptide promotes fracture healing in Lepr(-/-) mice[J]. Calcif Tissue Int. 2015. 97:581-591.
[8] Komrakova M, Stuermer EK, Werner C, et al. Effect of human parathyroid hormone hPTH (1-34) applied at different regimes on fracture healing and muscle in ovariectomized and healthy rats[J]. Bone. 2010. 47:480-492.
[9] Briteno-Vazquez M, Santillan-Diaz G, Gonzalez-Perez M, et al. Low power laser stimulation of the bone consolidation in tibial fractures of rats: a radiologic and histopathological analysis[J]. Lasers Med Sci. 2015. 30:333-338.
[10] Sevimli R, Uzel M, Sayar H, et al. The effect of dexketoprofen trometamol on the healing of diaphysis fractures of rat tibia[J]. Acta Orthop Traumatol Turc. 2013. 47:423-429.
[11] Sugiura T, Kashii M, Matsuo Y, et al. Intermittent administration of teriparatide enhances graft bone healing and accelerates spinal fusion in rats with glucocorticoid-induced osteoporosis[J]. Spine J. 2015. 15:298-306.
[12] Ibrahim N, Khamis MF, Mod Yunoh MF, et al. Targeted delivery of lovastatin and tocotrienol to fracture site promotes fracture healing in osteoporosis model: micro-computed tomography and biomechanical evaluation[J]. PLoS One. 2014. 9:e115595.
[13] Fridoni M, Masteri Farahani R, Nejati H, et al. Evaluation of the effects of LLLT on biomechanical properties of tibial diaphysis in two rat models of experimental osteoporosis by a three point bending test[J]. Lasers Med Sci. 2015. 30:1117-1125.
[14] Erdogan O, Esen E, Ustun Y, et al. Effects of low-intensity pulsed ultrasound on healing of mandibular fractures: an experimental study in rabbits[J]. J Oral Maxillofac Surg. 2006. 64:180-188.
[15] Hao Y, Wang X, Wang L, et al. Zoledronic acid suppresses callus remodeling but enhances callus strength in an osteoporotic rat model of fracture healing[J]. Bone. 2015. 81:702-711.
[16] Krege JH,Wan X. Teriparatide and the risk of nonvertebral fractures in women with postmenopausal osteoporosis[J]. Bone. 2012. 50:161-164.
[17] Augustine M,Horwitz MJ. Parathyroid hormone and parathyroid hormone-related protein analogs as therapies for osteoporosis[J]. Curr Osteoporos Rep. 2013. 11: 400-406.
[18] Miki T, Nakatsuka K, Naka H, et al. Effect and safety of intermittent weekly administration of human parathyroid hormone 1-34 in patients with primary osteoporosis evaluated by histomorphometry and microstructural analysis of iliac trabecular bone before and after 1 year of treatment[J]. J Bone Miner Metab. 2004. 22:569-576.
[19] Kamo K, Miyakoshi N, Kasukawa Y, et al. Intermittent weekly administration of human parathyroid hormone (1-34) improves bone-hydroxyapatite block bonding in ovariectomized rats[J]. J Bone Miner Metab. 2010. 28:634-640.
[20] Nakano T, Shiraki M, Sugimoto T, et al. Once-weekly teriparatide reduces the risk of vertebral fracture in patients with various fracture risks: subgroup analysis of the Teriparatide Once-Weekly Efficacy Research (TOWER) trial[J]. J Bone Miner Metab. 2014. 32:441-446.
[21] Bivi N, Lezcano V, Romanello M, et al. Connexin43 interacts with betaarrestin: a pre-requisite for osteoblast survival induced by parathyroid hormone[J]. J Cell Biochem. 2011. 112:2920-2930.
[22] Jilka RL, Almeida M, Ambrogini E, et al. Decreased oxidative stress and greater bone anabolism in the aged, when compared to the young, murine skeleton with parathyroid hormone administration[J]. Aging Cell. 2010. 9:851-867.
[23] Lara-Castillo N, Kim-Weroha NA, Kamel MA, et al. In vivo mechanical loading rapidly activates beta-catenin signaling in osteocytes through a prostaglandin mediated mechanism[J]. Bone. 2015. 76:58-66.
[24] Kulkarni NH, Halladay DL, Miles RR, et al. Effects of parathyroid hormone on Wnt signaling pathway in bone[J]. J Cell Biochem. 2005. 95:1178-1190.
Once-weekly subcutaneous injection of recombinant human parathyroid hormone (1-34) promotes the bone fracture healing in rats
MA Teng, ZHANG Weng, GUO Qi, HAI Bao, LIU Can, SONG Chun-li*
Department of Orthopedia, Peking University Third Hospital, Beijing 100191, China
Objective To study the effect of once-weekly injection of recombinant human parathyroid hormone rhPTH(1-34) on the healing of bone fracture in rats.Methods Fifty male 3-month old SD rats were used in this study to produce unilateral tibial fracture and received internal fixation with a Kirschner needle. Based on the dose and frequency of rhPTH (1-34) injection, the rats were randomly divided into five groups (n=10 each) as follows: subcutaneous injections of saline, and rhPTH in a dose of 10, 20, 10, and 20 μg/kg/d.After 4 weeks of treatment, the rats were euthanatized and the fractured tibia were assessed by X-ray, dual energy X-ray absorptiometry (DXA),micro-computed tomography (microCT) and three-point bending test.Results The fracture healing in the 20 μg/kg/w group was better than the saline group.The fracture healing in the 20 μg/kg/w group was as well as the 10 μg/kg/dgroup. The BMD of 20 μg/kg/w group was 26.2% higher than the saline group. The mineralized callus volume in the 20 μg/kg/w group was 51.4% higher than the saline group. The total callus volume in the 20 μg/kg/w group was 21.6% higher than the saline group. The ultimate load of the 20 μg/kg/w group was 29.3% higher than the saline group. There was no significant difference between the 20 μg/kg/w group and 10 μg/kg/d group in BMD, bone micro-architecture,and biomechanical strength (P>0.05). Conclusions Once weekly injection of rhPTH (1-34)can promote the bone fracture healing.
Parathyroid hormone; Fracture healing; Weekly injection;Daily injection;Rat
SONG Chun-li, E-mail: schl@bjmu.edu.cn
国家自然科学基金(81171693,81100895);国家高技术研究发展计划(863计划)(No.SS2015AA020304)。
马腾(1989-),硕士研究生。
宋纯理(1971-),研究方向:骨质疏松骨折愈合。E-mail: schl@bjmu.edu.cn
研究报告
Q95-33
A
1005-4847(2016)05-0481-06
10.3969/j.issn.1005-4847.2016.05.008
2016-04-26

