儿童继发性血栓性血小板减少性紫癜1例并文献复习
王春燕 童桂霞 孙 利 刘海梅 沈 茜 徐 虹
·论著·
儿童继发性血栓性血小板减少性紫癜1例并文献复习
王春燕1,3童桂霞2,3孙 利1刘海梅1沈 茜1徐 虹1
目的 提高对儿童不典型继发性血栓性PLT减少性紫癜(TTP)的认识。方法 总结1例无神经系统受累的继发性TTP患儿的临床资料、实验室检查结果、ADAMTS13酶活性和Anti-ADAMTS13抗体检测结果,行系统文献检索并文献复习。结果 男性患儿,12岁,急性起病,病初有发热,双下肢可见瘀点,PLT及Hb进行下降,血涂片可见破碎RBC,高胆红素血症,LDH明显升高,镜下血尿,肾功能正常,补体正常,考虑血栓性微血管病(TTP或非典型溶血尿毒综合征)。为进一步明确诊断, 行ADAMTS13酶活性检测2.3%(正常值40%~130%),ADAMTS13抗体检测90 U·mL-1(正常值<12 U·mL-1),确诊继发性TTP,予血浆置换和激素治疗。4个月后患儿停用所有药物,目前停药6月无复发。系统检索中国知网、万方和PubMed数据库,共有14篇英文文献中40例继发性TTP进入本文分析,发病年龄(10.2±5.2)岁,男19例,女21例,发热36例(90%),神经系统受累28例(70%),肾脏受累18例(45%),均有贫血和PLT降低。3例死亡,37例血浆置换+激素治疗,31例(83.8%)对血浆置换治疗即时反应好,1例因血浆过敏和1例血浆置换导管相关感染改为激素+利妥昔单抗治疗反应好,1例难治性继发性TTP加长春新碱(利妥昔单抗上市前)随访时复发,2例发生血浆置换依赖,加环孢素后治疗反应好,1例治疗反应不好,加长春新碱后治疗反应好,,4例失访(10.8%),平均随访时间29月(3~72个月),13例(39.4%)出现复发,9/13例加利妥昔单抗中仍有2例复发。结论 贫血和PLT降低应怀疑TTP,需行ADAMTS13酶活性及其抗体的检测,有助于区别遗传性和获得性TTP;血浆置换+激素,或+利妥昔单抗是TTP的治疗组合选项。
血栓性PLT减少性紫癜; 儿童; ADATS-13酶活性; ADAMTS13抗体
1 病例报告
患儿,男,汉族,12岁,因“发热后出血性皮疹”就诊于当地医院,不伴神经系统症状,PLT 42×109·L-1,未给予特殊处理,2 d后PLT下降至6×109·L-1,为明确诊断转入复旦大学附属儿科医院。
患儿既往体健,无药物过敏史,无特殊药物使用史。父母非近亲结婚,否认家族中有类似疾病史。
入院查体,T 36.6℃,P 99·min-1,R 22·min-1,BP 100/65 mmHg;神志清楚,全身可见散在粟粒样出血点,以双下肢、左上臂及左颈部显著,左脚趾可见瘀斑。全身皮肤无黄染,巩膜轻度黄染。实验室检查:Hb 96.2 g·L-1,PLT 5×109·L-1,外周血涂片可见破碎RBC,肌酐43.0 μmol·L-1,尿素氮4.60 mmol·L-1,乳酸脱氢酶978 U·L-1(正常值0~200 U·L-1),尿RBC 176.3·HP-1,尿蛋白+++,Comb's试验阴性,大便大肠埃希菌培养阴性,补体C3、C4、CH50均正常,自身抗体阴性,乙肝、梅毒和HIV阴性,腹部B超未见异常。
入院后予80 g IVIG输注后,PLT 13×109·L-1,Hb 118 g·L-1。考虑血栓性微血管病[血栓性PLT减少性紫癜(TTP)和溶血尿毒综合征(HUS)]。行ADAMTS13酶活性检测2.3%(正常值40%~130%),ADAMTS13抗体检测90 U·mL-1(正常值<12 U·mL-1,ELISA法),临床诊断继发性TTP,予冰冻血浆600 mL(10 mL·kg-1·d-1)1 d后,PLT 11×109·L-1,Hb 84 g·L-1,予血浆置换(35 mL·kg-1·d-1),同时行ADAMTS13基因全外显子及其邻近区域测序未见突变,确诊继发性TTP。经过4次血浆置换,1周后复查,PLT 33.0×109·L-1,Hb 89.2 g·L-1,ADAMTS13酶活性(2.5%)及其抗体(85 U·mL-1)均无明显改善,再予以5次血浆置换,同时加强的松龙30 mg bid口服,7 d后PLT、Hb和ADAMTS13酶活性及其抗体逐渐至正常水平。现患儿每月定期随访血、尿常规、肝肾功能和乳酸脱氢酶均正常,外周血涂片未见破碎RBC。6个月随访ADAMTS13酶及其抗体正常,目前停药6个月未复发。
2 文献检索及复习
2.1 文献检索策略 以“儿童 AND (血栓性血小板减少性紫癜 OR TTP)”为关键词或主题词在中国知网、万方数据库中检索相关中文文献; 以(acquired Thrombotic Thrombocytopenic Purpura) AND (children OR pediatrics)为检索式检索PubMed数据库。
2.2 文献纳入和排除标准 符合确诊继发性TTP标准[①微血管溶血性贫血(血常规Hb降低且涂片破碎RCB阳性),PLT减少;②大便大肠埃希菌培养、Comb's、自身抗体和ANCA检测阴性;③ADAMTS13酶活性<10%及其抗体升高)]的文献被纳入;排除指南、传统综述和动物实验的文献,排除仅符合临床诊断继发性TTP标准(①临床存在:发热、微血管溶血性贫血、PLT减少、肾功能受损和神经系统受损“五联征”;②大便大肠埃希菌培养、Comb's、自身抗体和抗中性粒细胞胞浆抗体检测阴性)的文献。
2.3 文献汇总结果 中文数据库检索到9篇文献,均为临床诊断TTP;英文数据库14篇[1~14]文献符合确诊继发性TTP进入本文复习,来自9个国家(澳大利亚、美国、法国、英国、意大利、印度、日本、比利时、德国),报告了40例继发性TTP。男19例,女21例,发病年龄(10.2±5.2)岁,发热36例(90%),神经系统受累28例(70%),肾脏受累18例(45%),40例均贫血[Hb平均(76.1±24)g·L-1]和PLT[(14.3±10.1)×109·L-1]明显降低。33例符合临床诊断继发性TTP标准,2例误诊为ITP,2例误诊为Evans,3例误诊为HUS,但均达到ADAMTS13酶活性降低及其抗体升高标准而确诊为继发性TTP。
40例确诊后3例(7.5%)病情危重死亡,37以血浆置换+激素治疗,其中31例(83.8%)对血浆置换治疗即时反应好,1例因血浆过敏和1例血浆置换导管相关感染改为激素+利妥昔单抗治疗反应好,1例难治性继发性TTP加长春新碱(利妥昔单抗上市前)随访时复发,2例发生血浆置换依赖,加环孢素后治疗反应好,1例治疗反应不好,加长春新碱后治疗反应好。随访中4例失访(10.8%),余33例平均随访时间29月(3~72个月),13例(39.4%)出现复发,其中9例加利妥昔单抗中仍有2例复发。
3 讨论
TTP是1924年由 Moschcowitz首次报道[1],主要分为遗传性和继发性TTP,发病率(0.4~6)/10万。遗传性TTP主要是ADAMTS13基因纯合或复合杂合突变所致[15],新生儿即可发病;继发性TTP可在任何年龄起病,10~40岁多见,目前报道的儿童继发性TTP平均年龄10.6岁。继发性TTP患儿临床主要表现为微血管溶血性贫血、PLT减少、发热、肾功能受损、神经系统受损“五联征”,神经系统累及为其区别于非典型HUS的主要临床表现,80%有神经症状[16],其中约50%在起病时即有神经系统症状,包括头痛、意识障碍、神志模糊、谵妄和抽搐,甚至昏迷等,仅有部分患儿同时表现为“五联征”,检索文献对既往报道的继发性TTP患儿临床特点进行分析,约90%患儿存在前期发热,70%患儿累及神经系统,45%的患儿累及肾脏系统,所有患儿均出现微血管溶血性贫血及PLT减少,因此,对于仅表现为微血管溶血性贫血及PLT减少的患儿,应考虑TTP。实验室检查提示TTP患儿的存在Hb和PLT降低,但以PLT降低为主,往往低于20×109·L-1,目前已报道的继发性TTP患儿PLT平均低至14×109·L-1,同时伴网织RBC的升高,乳酸脱氢酶均明显升高,提示患儿存在急性溶血,外周血涂片提示破碎RBC阳性,同时大便大肠埃希菌培养阴性,Comb's试验阴性,补体C3、C4、CH50均正常,自身抗体阴性,乙肝、梅毒和HIV阴性,排除与TTP表现相似的急性溶血性疾病,临床即可考虑诊断为TTP,应给予及时给予血浆疗法,以降低其急性期病死率,同时在血浆治疗前行ADAMTS13酶活性检测[17,18]。
不同分类的TTP的治疗不同,遗传性TTP急性发作期的主要治疗为血浆置换/血浆输注。继发性TTP的主要治疗为血浆置换,必要时联合免疫抑制剂。对于难治性继发性TTP及继发性TTP出现复发,均建议给予利妥昔单抗治疗。本文报告患儿入院后临床表现结合实验室检查,临床考虑诊断为TTP,给予血浆输注治疗,患儿临床表现及实验室检查均未见明显改善,提示患儿为继发性TTP的可能性较大,及时给予血浆置换治疗,患儿临床表现明显改善[16]。
既往主要通过患儿“五联征”来诊断TTP,同时通过患儿是否有神经系统受累来鉴别TTP和非典型HUS,但约35%的TTP患儿并无神经系统累及,因此会导致漏诊或者误诊,TTP的发病机制主要是ADAMTS13酶活性降低,不能剪切血液中超大分子的vWF因子超大多聚体(UL-vWF)为vWF,UL-vWF可引起血流剪切力的改变,在感染、手术等诱因存在的情况下,导致血栓的发生[19,20]。
遗传性TTP是一种常染色体隐性遗传病,主要是ADAMTS13基因纯合或者复合杂合突变,使得ADAMTS13酶活性降低;继发性TTP主要是患儿体内存在Anti-ADAMTS13抗体导致ADAMTS13酶活性降低,UL-vWF能在血流剪切力的作用下诱导PLT聚集和黏附,形成血栓[21]。因此无论是遗传性还是继发性TTP,给予血浆治疗前检测其血浆中ADAMTS13酶活性都极其重要,对于酶活性<10%的患儿,应同时检测其Anti-ADAMTS13抗体,若其抗体阴性,应行ADAMTS13基因编码区外显子测序,以确诊患儿是否为遗传性TTP。若ADAMTS13抗体阳性,则诊断为继发性TTP。在目前报道的40例TTP患儿中,仅通过临床表现和实验室检查,7例(17.5%)误诊为与其临床表现及实验室检查相似的疾病(aHUS或Evans病),但ADAMTS13酶活性检测均<10%,Anti-ADAMTS13抗体均升高而确诊继发性TTP。
图1归纳了TTP病例特点,描绘了TTP诊断与治疗的流程图。遗传性TTP主要为定期给予血浆输注治疗或者给予浓缩的Ⅷ因子输注治疗[22]。继发性TTP首选血浆置换治疗,患儿在进行血浆置换治疗的同时,若ADAMTS13酶活性持续<10%,ADAMTS13抗体浓度持续升高或者持续不下降,则可加用泼尼松龙1~2 mg·kg-1[23],对于严重病例大剂量冲击可改善预后[24]。TTP患儿对血浆过敏、血浆置换过程中出现导管相关感染、严重累及神经系统或者心血管系统及难治性TTP(血浆置换或者联合激素治疗疗效差),可加用利妥昔单抗治疗[1],降低继发性TTP患儿的复发,也有部分学者建议继发性TTP首次发作时即可给予利妥昔单抗,以降低其复发率,但目前还缺少大样本研究来支持这一观点。
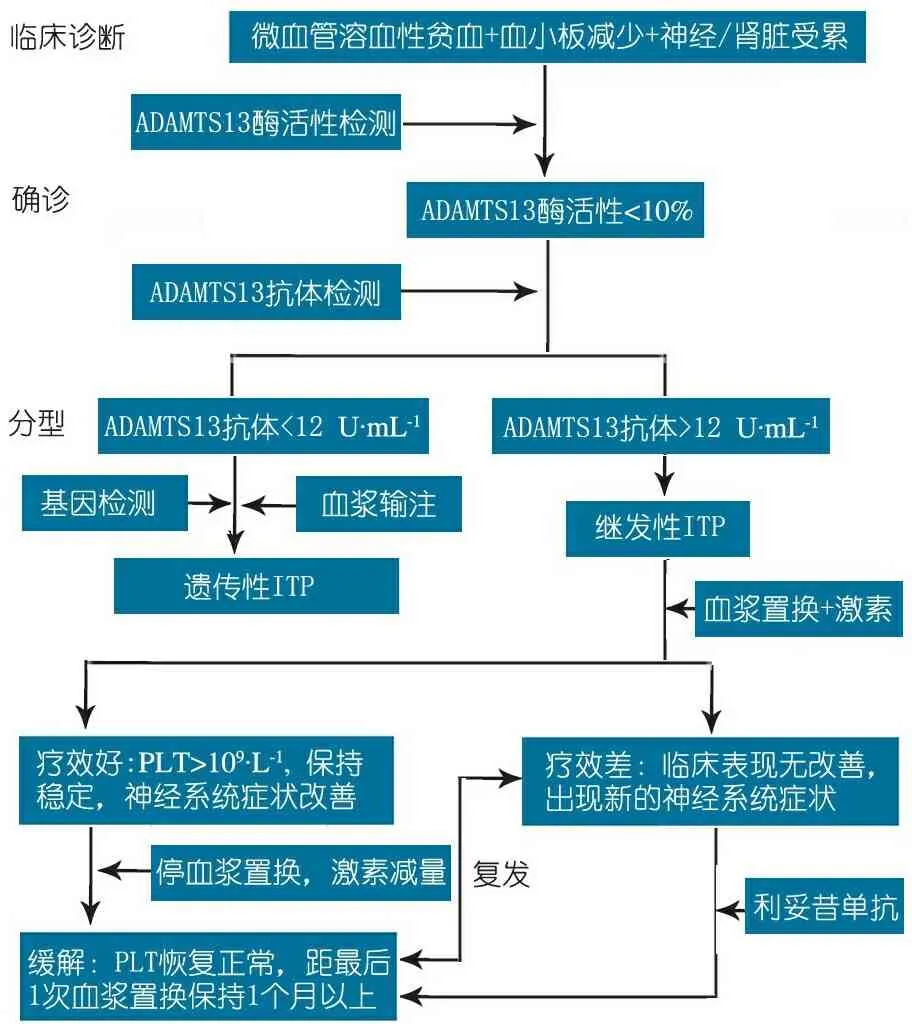
图1 TTP的诊断与治疗流程图
目前国外文献报道40例儿童继发性TTP患儿,急性期死亡3例,85%的患儿对血浆置换的疗效好,其中35%患儿出现复发,对于复发的及难治性TTP患儿,给予利妥昔单抗治疗后患儿再复发率明显降低。本文患儿经血浆置换后监测ADAMTS13酶活性无明显升高,ADAMTS13抗体浓度持续不下降,在第1疗程血浆置换后加用足量强的松龙30 mg bid(1 mg·kg-1·d-1)口服治疗,后动态监测各种实验室指标均在正常范围,在4个月内激素逐渐减停。目前随访处于完全缓解状态。
给予血浆置换+激素治疗,PLT>150×109·L-1并稳定2 d,则可停止血浆置换治疗,继续激素治疗,若PLT恢复正常,保持1~2周,则激素逐渐减量,PLT正常维持在1月以上,则说明患儿完全缓解[25,26]。
[1]Albaramki JH, Teo J, Alexander SI. Rituximab therapy in two children with autoimmune thrombotic thrombocytopenic purpura. Pediatr Nephrol,2009,24(9):1749-1752
[2]Horton TM, Stone JD, Yee D, et al. Case series of thrombotic thrombocytopenic purpura in children and adolescents. J Pediatr Hematol Oncol,2003, 25(4): 336-339
[3]Curtillet C, Poullin P, Doré E, et al. Paediatric case report of an acquired autoimmune thrombotic thrombocytopenic purpura. Arch Pediatr,2006, 13(12): 1521-1524
[4]Harambat J, Lamireau D, Delmas Y, et al. Successful treatment with rituximab for acute refractory thrombotic thrombocytopenic purpura related to acquired ADAMTS13 deficiency: a pediatric report and literature review. Pediatr Crit Care Med,2011, 12(2): e90-93
[5]Lawlor ER, Webb DW, Hill A, et al. Thrombotic thrombocytopenic purpura: a treatable cause of childhood encephalopathy. J Pediatr,1997, 130(2): 313-316
[6]Piastra M, Currò V, Chiaretti A,et al. Intracranial hemorrhage at the onset of thrombotic thrombocytopenic purpura in an infant: Therapeutic approach and intensive care management. Pediatr Emerg Care, 2001,17(1):42-45
[7]Jayabose S, Dunbar J, Nowicki TS, et al. Rituximab therapy to prevent relapse in chronic relapsing thrombotic thrombocytopenic purpura (TTP) in a child.Pediatr Hematol Oncol,2011 28(2): 167-172
[8]Jayabose S, Nowicki TS, Dunbar J, et al. Acquired thrombotic thrombocytopenic purpura in children: a single institution experience. Indian J Pediatr,2013, 80(7): 570-575
[9]Morishima T, Nomura A, Saida S, et al. Pediatric idiopathic TTP diagnosed with decreased ADAMTS13 activity. Pediatr Int, 2012, 54(3): 422-423
[10]Narayanan P, Jayaraman A, Rustagi RS, et al. Rituximab in a child with autoimmune thrombotic thrombocytopenic purpura refractory to plasma exchange. Int J Hematol,2012, 96(1): 122-124
[11]Arni D, Gumy-Pause F, Ansari M, et al. Successful liver transplantation in a child with acute-on-chronic liver failure and acquired thrombotic thrombocytopenic purpura. Liver Transpl,2015, 21(5): 704-706
[12]Reese JA, Muthurajah DS, Kremer Hovinga JA, et al. Children and adults with thrombotic thrombocytopenic purpura associated with severe, acquired Adamts13 deficiency: comparison of incidence, demographic and clinical features. Pediatr Blood Cancer,2013, 60(10): 1676-1682
[13]Ashida A, Nakamura H, Yoden A, et al. Successful treatment of a young infant who developed high-titer inhibitors against VWF-cleaving protease (ADAMTS13): important discrimination from Upshaw-Schulman syndrome. Am J Hematol,2002, 71(4): 318-322
[14]Zenno A, Richardson M. Coombs Positive Thrombotic Thrombocytopenic Purpura in a Male Pediatric Patient: An Urgent Diagnostic Challenge. Pediatr Blood Cancer,2016, 63(10): 1860-1862
[15]George JN, Nester CM. Syndromes of thrombotic microangiopathy. N Engl J Med,2014, 371(7): 654-666
[16]Rock GA. Management of thrombotic thrombocytopenic purpura. Br J Haematol,2000,109:496-507
[17]Shenkman B,Einav Y. Thrombotic thrombocytopenic purpuraand other thrombotic microangiopathic hemolytic anemia:diagnosis and classification.Autoimmun Rev,2014,13(4-5):584-586
[18]Cataland SR,Wu HM.Atypical hemolytic uremic syndrome and thrombotic thrombocytopenic purpua :clinically differentiating the thrombotic microangiopathies.Eur J Intern Med,2013,24(6):486-491
[19]王春燕,方晓燕,沈茜,等. ADAMTS13基因突变致遗传性血栓性血小板减少性紫癜一例. 中华儿科杂志,2016, 54(5): 387-388
[20]Naito C, Ogawa Y, Yanagisawa K, et al. Acquired thrombotic thrombocytopenic purpura after vascular prosthesis implantation for impending rupture of an abdominal aortic aneurysm. Rinsho Ketsueki,2016, 57(3): 364-368
[21]Dahlan R, Sontrop JM, Li L,et al. Primary and Secondary Thrombotic Microangiopathy Referred to a Single Plasma Exchange Center for Suspected Thrombotic Thrombocytopenic Purpura: 2000-2011. Am J Nephrol, 2015, 41(6): 429-437 [22]Ueda Y. Treatment of thrombotic thrombocytopenic purpura. Rinsho Ketsueki,2014, 55(10): 2076-2086
[23]Yarranton H,Cohen H,Pavord SK,et al. Venous thromboembolism associated with the management of acute thrombotic thrombocytopenic purpura. Br J Haematol,2003,121(5):778-785
[24]Balduini CL,Gugliotta L,Luppi M,et al.High versus standard dose methylprednisolone in the acute phase of idiopathic thrombotic thrombocytopenic purpura:a randomized study.Ann Hematol,2010,89:591-596
[25]Sayani FA, Abrams CS. How I treat refractory thrombotic thrombocytopenic purpura. Blood,2015, 125(25): 3860-3867
[26]Scully M, Hunt BJ, Benjamin S, et al. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol,2012, 158(3): 323-335
(本文编辑:张崇凡)
The acquired thrombotic thrombocytopenic purpura in children: a case report and literature review
WANG Chun-yan1,3,TONG Gui-xia2,3,SUN Li1,LIU Hai-mei1,SHEN Qian1,XU Hong1
(1 Department of Renal Rheumatism, Children's Hospital of Fudan University, Shanghai 201102;2 Department of Renal Rheumatism, Jinan Children's Hospital, Shandong Province, Jinan 250022, China;3 Co-first author)
SUN Li,E-mail:lillysun@263.net
Objective To improve the knowledge of the acquired thrombotic thrombocytopenic purpura (TTP) in children.MethodsThe clinical data of the acquired TTP case without nervous system involvement were summarized and related literatures were reviewed.ResultsThe 12-year-old boy was admitted to our hospital because of fever and rash on the lower limbs as the first symptom. The blood test showed anemia, thrombocytopenia and blood smear showed erythroclasis, while the urinalysis showed microscopic haematuria. The blood biochemistry showed elevated bilirubin and LDH levels. However, renal function and complement level were normal. Thrombotic microangiopathy (aHUS or TTP) was considered. In further differential diagnosis, his ADAMTS13 activity showed 5% below , with the presence of ADAMTS13 antibodies. The final diagnosis was acquired TTP. Plasma exchange plus prednisolone were carried out. The patient recovered absolutely, and all the medication was stopped after 4 months. There was no relapse during the six months follow-up. After a systematic analysis of the ChianInfo, CNKI and pubmed. A total of 40 TTP patients were analyzed from 14 articals, The mean age of patients was (10.2±5.2) years old. The study included 19 men and 21 women. All patients presented with anemia and thrombocytopenia, 36 cases with fever (90%), 28 cases (70%) with nervous system involvement, 18 cases (45%) with renal involvement. During the acute phase,3 patients died and 37 patients were treated with the plasma exchange plus glucocorticoid, 31 patients (83.8%) clinical symptoms were quickly improved with plasma exchange plus glucocorticoid, while 6 had other complications were further treated with RTX. The mean follow-up time was 29 months (3-72 months) with 4 lost cases (10.8%). Within the follow-up period, 13 (39.4%) patients suffered relapses. 9 cases were given a further treatment of RTX , while 2 of them still suffered relapse during RTX treatment.ConclusionThe patients presented with anemia and thrombocytopenia should be considered as TTP. Monitoring of the ADAMTS13 activity and anti-ADAMTS13 antibody plays an important role in diagnosis and differential diagnosis in TTP. Plasma exchange plus glucocorticoid or rituximab can be considered as the first line treatment.
Thrombotic thrombocytopenic purpura; Children; ADAMTS13 activity; ADAMTS13 antibodies
1 复旦大学附属儿科医院肾脏风湿科 上海,201102;2 山东省济南市儿童医院肾脏风湿科 济南,250022;3 共同第一作者
孙利,E-mail: lillysun@263.net
10.3969/j.issn.1673-5501.2016.05.015
2016-05-27
2016-09-21)

