Dent病1型5例病例系列报告并文献复习
张 娅 方晓燕 徐 虹 沈 茜
·论著·
Dent病1型5例病例系列报告并文献复习
张 娅 方晓燕 徐 虹 沈 茜
目的 报告5例Dent病1型患儿的临床资料,提高对其认识。方法 分析5例Dent病1型患儿病史、实验室检查,对先证者进行Dent病相关基因CLCN5、OCRL外显子及附近调控区域的直接测序,验证先证者父母有无相应位点突变,系统复习国内外文献报告的Dent病1型,归纳临床表型与突变类型。结果 5例患儿实验室检查发现24 h尿蛋白定量33.0~68.9 mg·kg-1,尿α1微球蛋白、尿白蛋白和尿免疫球蛋白均明显升高,均伴有高钙尿症,其中镜下血尿1例、肾钙质沉着2例,行CLCN5、OCRL基因测序各发现了1个CLCN5突变,分别为R637X、Y479X、G530V、W103fsX104和R707X,其中Y479X、G530V和W103fsX104为新发现的突变位点。系统文献检索260篇Dent病相关文献,逐篇筛选,共有72篇Dent病1型病例报告和病例系列报告进入本文分析,均为病例报道或病例系列报道,欧美人群422例,亚洲人群176例。欧美与亚洲国家Dent病1型临床表型低分子量蛋白尿表现一致,差异无统计学意义,高钙尿症、肾钙质沉着、肾积石、佝偻病和肾功能异常差异均有统计学意义,不同的临床表型没有突出显现突变类型(错义、无义、移码、剪切和缺失突变)的优势。结论 临床提示Dent病1型可能的患儿可通过基因检测以明确诊断,避免不必要的免疫抑制剂治疗。CLCN5突变具有高度异质性,临床表型与CLCN5突变类型没有显现较好的关联性。
儿童; 低分子量蛋白尿; Dent病1型;CLCN5基因突变; 慢性肾脏病
蛋白尿是儿童肾脏疾病就诊的常见原因,随着对蛋白尿认识的深入,发现儿童期起病的蛋白尿除了常见的肾小球病变外,肾小管性蛋白尿也并不少见,所以对于首诊为蛋白尿的患儿,要了解尿蛋白的来源。Dent病是小管性蛋白尿中研究较多的一类疾病,属于X连锁隐性遗传疾病,所以就诊人群中多为男性,女性携带者症状轻微不易发现,对于有临床表现或家族史的患儿最终可通过基因测序确诊Dent病,CLCN5和OCRL基因突变分别为1型和2型Dent病,未检测出突变的则记为Dent-NI(Dent-not identified)[1]。全球对Dent病有非常多的病例报告或病例系列报告,本课题组前期对Dent病2型做过系统的文献复习,本文报道5例Dent病1型并对相关文献进行复习,以进一步提高对Dent1型的认识。
1 方法
1.1 研究对象 纳入2011年1月以来至复旦大学附属儿科医院(我院)临床诊断Dent病并行相关基因突变检测确诊的Dent病1型的病例。
1.2 资料采集 截取入我院后与Dent病相关的第1次血液、尿液生化指标和泌尿系超声结果,Dent病1型相关基因突变检测结果,基于伦理考量外院已经行肾活检的结果也进入本文分析,同时截取外院行免疫抑制剂使用情况。
1.3 Dent病相关基因检测方法 取得患儿家长或监护人知情同意后,采集患儿及父母外周血2 mL,送北京德易东方转化医学研究中心行相关基因检测。提取基因组DNA(德国QIAGEN公司血液基因DNA抽提试剂盒)。PCR扩增CLCN5和OCRL所有编码序列,扩增引物序列参考文献[2,3]。PCR反应条件:95℃预变性3 min,94℃ 30 s,55~60℃ 35 s,72℃ 40~50 s;35个循环,72℃再延伸5 min。PCR产物经1%琼脂糖凝胶电泳初步鉴定扩增条带是否为目的条带,若为目的条带则进行测序。使用ABI 3730测序列分析仪(美国ABI公司)进行测序,测序结果与美国国家生物技术信息中心(NCBI)GenBank中的序列进行对比。
1.4 文献检索策略 以“Dent Disease” OR “Dent's Disease”在PubMed网站检索,以“Dent病”关键词在万方数据库检索,检索起于建库至2016年7月,手工去除Dent病2型。
1.5 文献提取数据 Dent病临床表型:蛋白尿(泡沫尿)、低分子量蛋白尿(LMWP)、高钙尿症、肾钙质沉着、佝偻病、肾结石、肾功能和CLCN5基因突变类型。
1.6 统计学分析 分类资料(临床表型、CLCN5基因突变类型)应用卡方检验进行统计,病例数不满足卡方检验要求,则使用Fisher确切概率法,统计数据均用SPSS Statistics 22软件进行分析。
2 结果
2.1 病例报告 我院经CLCN5基因检测确诊的Dent病1型5例,均为男性,起病年龄为生后至5.4岁,4例以泡沫尿就诊、1例为体检发现,确诊年龄为4.5~6.8岁,无特殊面容和指趾畸形,无其他系统异常表现,生长发育正常。5例患儿尿液及其他检查结果见表1。
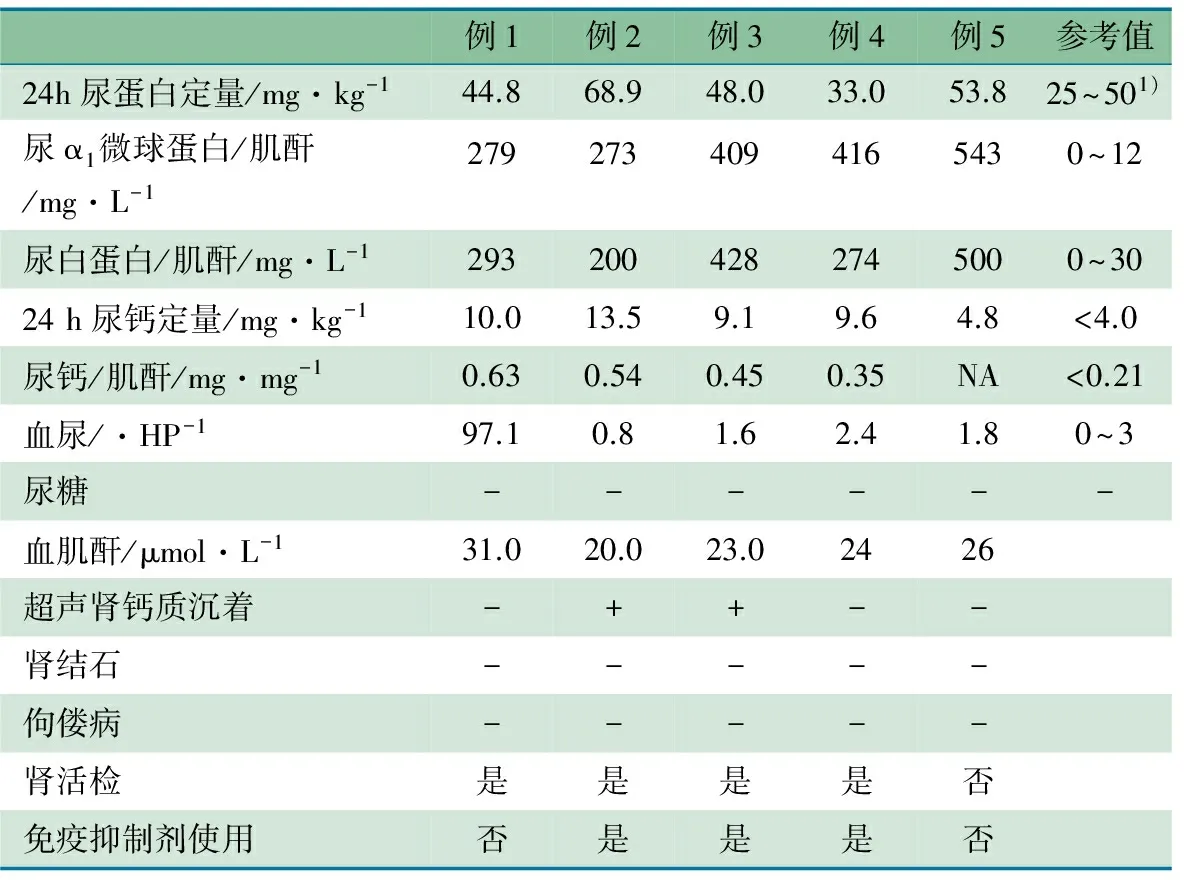
表1 5例Dent病1型实验室、超声和肾活检等检查结果
注 1)25~50mg·kg-1为中等量蛋白尿,>50mg·kg-1为大量蛋白尿;“-”:阴性;“+”:阳性;NA为缺失值
2.2 基因检测及家系验证结果 5例患儿均为CLCN5基因突变。例1:10号外显子c.1909C>T突变(p.637R>X),为CLCN5基因突变热点[4];例2 :9号外显子c.1437C>A突变(p.479Y>X);例3:10号外显子c.1589G>T突变(p.G530V),SIFT和Polyphen-2软件预测其蛋白结构有害;例4:4号外显子c.308缺失G突变(p.103,W>Xfsl);例5:13号外显子c.2119C>T(p.707R>X)。均未发现OCRL相关突变,5例患儿母亲均为相应位点的杂合携带者,父未检测出相关突变。Y479X、G530V和W103fsX104(例2~4)均未在Human Gene Mutation Database和ExAC Browser网站上查阅到为新发现的突变位点,Mutation Taster网站查找,显示均为高度保守。
2 .3 文献复习
2.3.1 文献检索结果 共检索到260篇Dent病相关文献,逐篇筛选,共有72篇Dent病1型病例报告和病例系列报告。考虑到女性为携带者,目前发病人数相对较少,所以有症状的女性患者未纳入;家系报告中经基因验证证实CLCN5突变的男性患者也纳入;可识别的重复病例只记录1次;共有598例Dent病1型患者进入本文分析,根据作者医院所在国家划分为美欧和亚洲,欧美人群422例包括意大利、西班牙、德国、英国、法国、奥地利、芬兰、葡萄牙、黑山共和国、比利时、塞尔维亚、瑞士、乌克兰、美国、南美、加拿大、乌拉圭、阿根廷、玻利维亚,亚洲人群176例[5~76]包括中国、日本、韩国、以色列、印度。
2.3.2 临床表型 复习598例Dent病1型临床诊断发现,以低分子量蛋白尿+以下任意一项,高钙尿症、肾钙质沉着、肾结石、肾功能异常、镜下血尿、低磷酸盐血症作为临床诊断为180例,以低分子量蛋白尿和高钙尿症+以下任意一项肾钙质沉着、肾结石、肾功能异常、镜下血尿、低磷酸盐血症作为临床诊断为120例,298例没有具体描述临床诊断的相关症状无法归类。
表2显示欧美与亚洲国家Dent病1型临床表型高钙尿症、肾钙质沉着、肾结石、佝偻病(低磷酸盐血症导致)和肾功能异常差异均有统计学意义。欧美人群有无肾钙质沉着导致肾功能不全38.2%(21/55)和14.3%(8/56),差异有统计学意义(χ2=8.209,P=0.005),亚洲人群有无肾钙质沉着导致肾功能不全24.1%(7/29)和12.9%(4/31),差异无统计学意义(精确检验,P=0.327)。欧美人群有无CLCN5突变导致高钙尿症97.1%(68/70)和40.0%(24/60),差异有统计学意义(精确检验,P=0.009)。
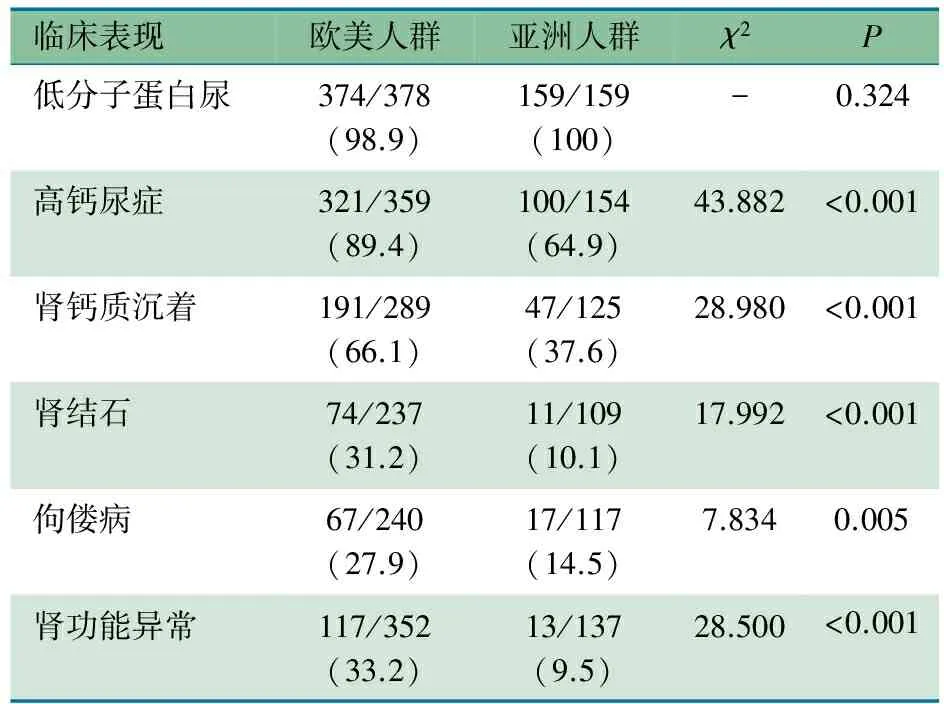
表2 不同地区Dent病1型临床表现[n/N(%)]
2.3.3 欧美与亚洲人群Dent病1型CLCN5突变类型比较 图1显示,欧美与亚洲人群间错义、无义、移码、剪切和缺失突变差异均无统计学意义,Dent病1型CLCN5突变以错义、无义、移码为主要类型,鉴于无义、移码突变均可导致蛋白截短,在统计临床表型与突变类型时归为截短突变,表3显示,在欧美人群和亚洲人群不同的临床表型没有突出显现突变类型的优势。
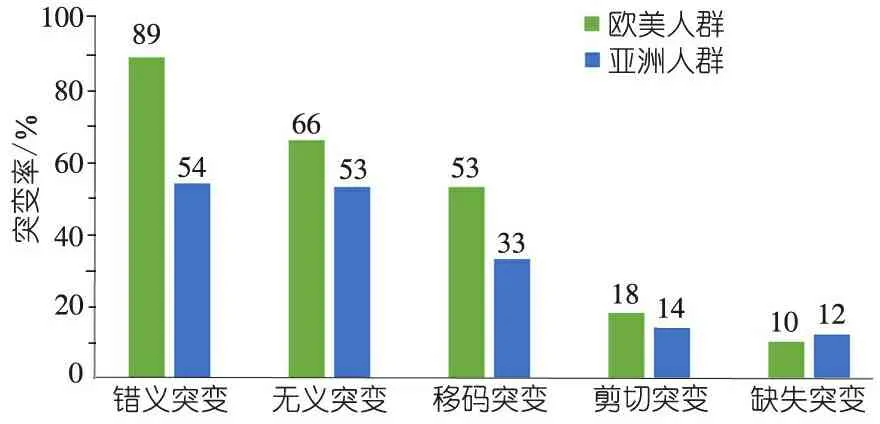
图1 不同地区CLCN5突变类型
注:错义突变组(χ2=1.142,P=0.285),无义突变组(χ2=0.734,P=0.392),移码突变组(χ2=0.385,P=0.535),剪切突变组(χ2=0.087,P=0.769),缺失突变组(χ2=1.686,P=0.694)
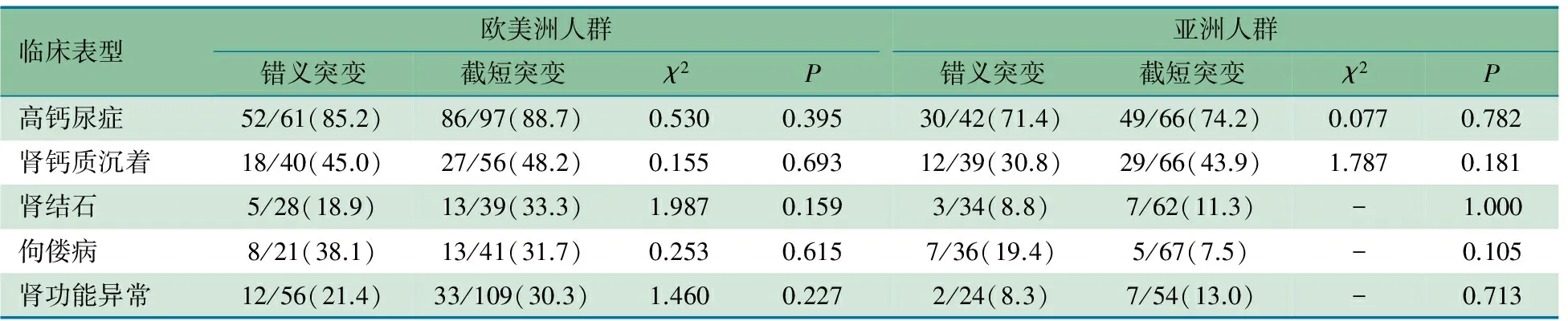
表3 不同地区CLCN5突变类型与临床表型关系[n/N(%)]
3 讨论
随着对蛋白尿认识的深入,肾小管病因导致的蛋白尿也越来越受到关注,也提醒蛋白尿不仅是量的问题,尿蛋白成分的定性也显得尤为重要。Dent病1型属于罕见病,大部分Dent病1型患者在儿童时期临床表现不明显,甚至进展为慢性肾衰竭才被发现,而且Dent病1型表现各异,即使是同一患病家庭的成员,临床表型也可不同,所以早期诊断存在一定的难度[76]。
Dent病1型国内外报道的就诊原因基本一致,包括泡沫尿、多饮多尿、佝偻病、感染、多发性骨折、生长受限和体检发现等。多数患儿在初诊时被诊断为肾病综合征、肾小球肾炎、抑或是Bartter综合征等,部分患儿使用了不同的免疫抑制剂治疗。当Dent病1型患者出现肾病水平的蛋白尿或混合型蛋白尿时,往往是在肾小管病变后出现的继发性改变,所以Dent病1型的早期发现就显得尤为重要,日本多以尿液筛查形式发现尿蛋白,进而分析尿蛋白成分,从而有助于诊断Dent病1型,所以推荐行尿液筛查,以降低漏诊误诊的发生[48]。
典型的Dent病1型临床诊断包括以下2种标准,一是2 项必备加任意一项,必备项:①低分子蛋白尿至少升高5 倍,包括尿α1微球蛋白、β2微球蛋白和视黄醇结合蛋白,或尿蛋白电泳提示低分子蛋白﹥50%;②高钙尿症:随机尿钙/肌酐>0.25,或24 h尿钙定量>4.0 mg·kg-1;任意项:③肾钙盐沉着症、④肾结石、⑤肾功能异常、⑥镜下血尿、⑦低磷血症[19]。二是有日本学者认为,只需符合上述必备项之一加任意项之一即可诊断。由于诊断不一致,日本降低了总体亚洲人群高钙尿症的发生率[77]。
对于高钙尿症是否能够提示CLCN5突变存在争议,欧美病例系列报道数据汇总发现,在有高钙尿症的Dent病1型患者中,更能发现CLCN5突变,但没有高钙尿症的患者也不能否定Dent病1型的可能,尤其是已经进展为慢性肾脏病的患者中[19, 45, 66]。根据之前报道的肾穿结果,Dent病1型患者主要表现为肾小管萎缩、肾间质纤维化、小管或间质钙化管型和肾小球非特异性改变,发现局灶节段性肾小球硬化可能是Dent病1型的表现之一,所以推测如果患者出现不明原因的大量蛋白尿或混合型蛋白尿,没有原发性肾小球疾病、肾活检与上述表现一致,应该考虑是否存在Dent病1型,尤其是不伴有水肿和低蛋白血症的患者[51, 52, 63]。图2显示的Dent病1型诊断流程。临床诊断的Dent病1型最终需要通过基因检测确诊。
欧美人群和亚洲人群低分子蛋白尿是相似的,而高钙尿症、肾钙质沉着、肾结石、佝偻病以及肾功能异常,亚洲人群发病较欧美人群是明显减少。目前对于Dent病1型主要是对症治疗,包括低钙饮食、氢氯噻嗪药物治疗,国内外文献都有报道氢氯噻氢类药物有助于降低尿钙、钙盐沉积,部分患者肾钙质沉着可消退,而有些患者停用药物后有钙质反跳现象,所以推测肾钙质沉着和肾结石发病的差异可能与不同的生活习惯有关,欧美人群多饮用富含矿物质水和奶制品,进而增加了Dent病1型患者钙质排泄的风险,促进了肾钙质沉着和肾结石的发生[11, 56, 74]。目前Dent病1型肾功能进展的确切机制尚不明确,对于肾钙质沉着是否与肾功能异常有关存在争议,由于亚洲人群肾钙质沉着和肾功能异常较欧美人群明显少,考虑两者是否存在相关性,欧美人群肾功能不全更易出现在肾钙质沉着的患者中,而亚洲人群没有发现两者相关[55]。欧美文献报道30%~80%的Dent病1型患者将在其30~50岁发展为慢性肾功能不全,考虑到目前亚洲人群随访年限较短,进展为慢性肾脏病的比例和年限的观察还需要大量的随访资料予以证实[78]。
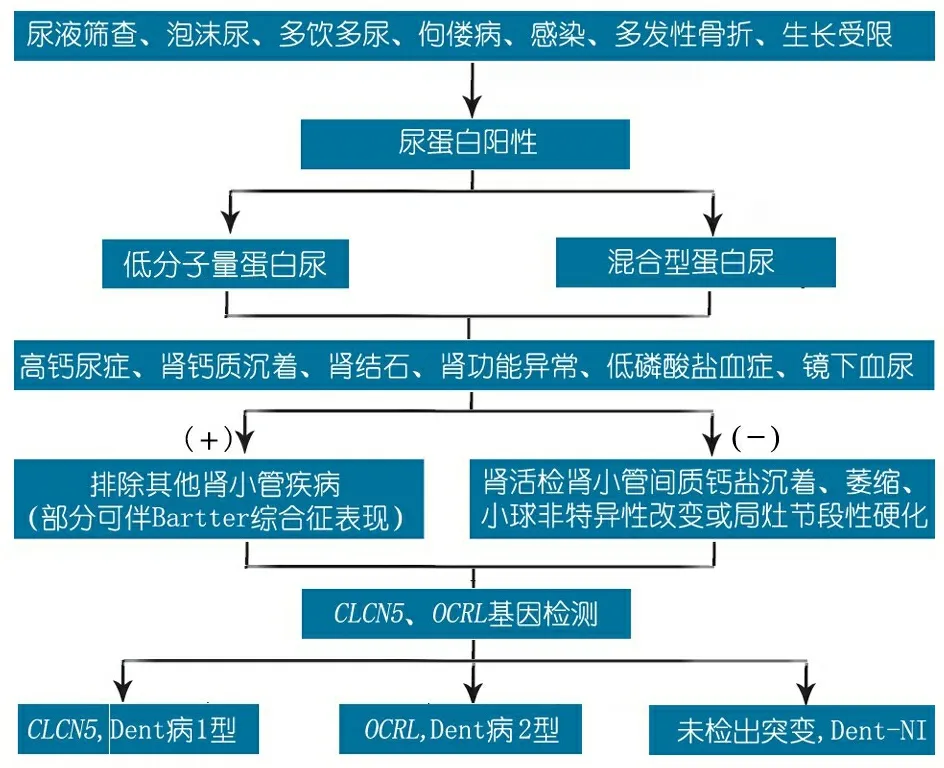
图2 Dent病1型诊断流程图
注 基于文献[78]改编
欧美人群和亚洲人群CLCN5突变类型分布一致,比较不同人群临床表型与突变类型的相关性,没能发现不同的突变类型凸显出不同临床表型的优势。虽然各研究团队都在寻找 Dent病1型临床表型和基因型的关联性,但是结果都没有给出明确的提示,还需要更多的基础研究、进而指导后续的临床诊疗。
[1]Tosetto E, Ceol M, Mezzabotta F, et al. Novel mutations of the CLCN5 gene including a complex allele and A 5' UTR mutation in Dent disease 1. Clin Genet, 2009,76(4):413-416
[2]Lloyd SE, Pearce SH, Gunther W, et al. Idiopathic low molecular weight proteinuria associated with hypercalciuric nephrocalcinosis in Japanese children is due to mutations of the renal chloride channel (CLCN5). J Clin Invest, 1997,99(5):967-974
[3]Addis M, Loi M, Lepiani C, et al. OCRL mutation analysis in Italian patients with Lowe syndrome. Hum Mutat, 2004,23(5):524-525
[4]Dinour D, Davidovitz M, Levin-Iaina N, et al. Truncating mutations in the chloride/proton ClC-5 antiporter gene in Seven Jewish Israeli families with Dent's 1 disease. Nephron Clin Pract, 2009,112(4):c262-c267
[5]Hoopes RJ, Hueber PA, Reid RJ, et al. CLCN5 chloride-channel mutations in six new North American families with X-linked nephrolithiasis. Kidney Int, 1998,54(3):698-705
[6]Igarashi T, Gunther W, Sekine T, et al. Functional characterization of renal chloride channel, CLCN5, mutations associated with Dent'sJapan disease. Kidney Int, 1998,54(6):1850-1856
[7]Morimoto T, Uchida S, Sakamoto H, et al. Mutations in CLCN5 chloride channel in Japanese patients with low molecular weight proteinuria. J Am Soc Nephrol, 1998,9(5):811-818
[8]Oudet C, Martin-Coignard D, Pannetier S, et al. A secondfamily with XLRH displays the mutation S244L in the CLCN5 gene. Hum Genet, 1997,99(6):781-784
[9]Nakazato H, Hattori S, Furuse A, et al. Mutations in the CLCN5 gene in Japanese patients with familial idiopathic low-molecular-weight proteinuria. Kidney Int, 1997,52(4):895-900
[10]Lloyd SE, Pearce SH, Fisher SE, et al. A common molecular basis for three inherited kidney stone diseases. Nature, 1996,379(6564):445-449
[11]Blanchard A, Vargas-Poussou R, Peyrard S, et al. Effect of hydrochlorothiazide on urinary calcium excretion in dent disease: an uncontrolled trial. Am J Kidney Dis, 2008,52(6):1084-1095
[12]Sheffer-Babila S, Chandra M, Speiser PW. Growth hormone improves growth rate and preserves renal function in Dent disease. J Pediatr Endocrinol Metab, 2008,21(3):279-286
[13]Ramos-Trujillo E, Gonzalez-Acosta H, Flores C, et al. A missense mutation in the chloride/proton ClC-5 antiporter gene results in increased expression of an alternative mRNA formthat lacks exons 10 and 11. Identification of seven new CLCN5 mutations in patients with Dent's disease. J Hum Genet, 2007,52(3):255-261
[14]Copelovitch L, Nash M A, Kaplan B S. Hypothesis: Dent disease is an underrecognized cause of focal glomerulosclerosis. Clin J Am Soc Nephrol, 2007,2(5):914-918
[15]Ramos-Trujillo E, Garcia-Nieto V, Gonzalez-Acosta H, et al. Molecular analysis of the CLCN5 gene in Dent's disease: first mutation identified in a patient from South America. Clin Nephrol, 2007,68(6):367-372
[16]Lim IS, Yun KW, Moon KC, et al. Proteinuria in a boy withinfectious mononucleosis, C1q nephropathy, and Dent's disease. J Korean Med Sci, 2007,22(5):928-931
[17]Anglani F, Bernich P, Tosetto E, et al. Family history may be misleading in the diagnosis of Dent's disease. Urol Res, 2006,34(1):61-63
[18]Ludwig M, Utsch B, Balluch B, et al. Hypercalciuria in patients with CLCN5 mutations. Pediatr Nephrol, 2006,21(9):1241-1250
[19]Tosetto E, Ghiggeri GM, Emma F, et al. Phenotypic and genetic heterogeneity in Dent's disease--the results of an Italian collaborative study. Nephrol Dial Transplant, 2006,21(9):2452-2463
[20]Lingenhel A, Lhotta K, Neyer U, et al. Role of the kidney in the metabolism of apolipoprotein A-IV: influence of the type of proteinuria. J Lipid Res, 2006,47(9):2071-2079
[21]Anton-Gamero M, Claverie-Martin F, Garcia-Nieto V, et al. Chloride and sodium renal tubular handling in Dent's disease. Pediatr Nephrol, 2005,20(8):1198-1199
[22]Besbas N, Ozaltin F, Jeck N, et al. CLCN5 mutation (R347X) associated with hypokalaemic metabolic alkalosis in a Turkish child: an unusual presentation of Dent's disease. Nephrol Dial Transplant, 2005,20(7):1476-1479
[23]Neild GH, Thakker RV, Unwin RJ, et al. Dent's disease. Nephrol Dial Transplant, 2005,20(10):2284-2285
[24]Cheong HI, Lee JW, Zheng SH, et al. Phenotype and genotype of Dent's disease in three Korean boys. Pediatr Nephrol, 2005,20(4):455-459
[25]Claverie-Martin F, Flores C, Anton-Gamero M, et al. The Alu insertion in the CLCN5 gene of a patient with Dent's disease leads to exon 11 skipping. J Hum Genet, 2005,50(7):370-374
[26]Yanagida H, Ikeoka M, Kuwajima H, et al. A boy with Japanese Dent's disease exhibiting abnormal calcium metabolism and osseous disorder of the spine: defective megalin expression at the brushborder of renal proximal tubules. Clin Nephrol, 2004,62(4):306-312
[27]Brakemeier S, Si H, Gollasch M, et al. Dent's disease: identification of a novel mutation in the renal chloride channel CLCN5. Clin Nephrol, 2004,62(5):387-390
[28]Santo Y, Hirai H, Shima M, et al. Examination of megalin in renal tubular epithelium from patients with Dent disease. Pediatr Nephrol, 2004,19(6):612-615
[29]Forino M, Graziotto R, Tosetto E, et al. Identification of a novel splice site mutation of CLCN5 gene and characterization of a new alternative 5' UTR end of ClC-5 mRNA in human renal tissue and leukocytes. J Hum Genet, 2004,49(1):53-60
[30]Moulin P, Igarashi T, Van der Smissen P, et al. Altered polarity and expression of H+-ATPase without ultrastructural changes in kidneys of Dent's disease patients. Kidney Int, 2003,63(4):1285-1295
[31]Claverie-Martin F, Gonzalez-Acosta H, Flores C, et al. De novo insertion of an Alu sequence in the coding region of the CLCN5 gene results in Dent's disease. Hum Genet, 2003,113(6):480-485
[32]Carballo-Trujillo I, Garcia-Nieto V, Moya-Angeler F J, et al. Novel truncating mutations in the ClC-5 chloride channel gene in patients with Dent's disease. Nephrol Dial Transplant, 2003,18(4):717-723
[33]Raja KA, Schurman S, D'Mello RG, et al. Responsiveness of hypercalciuria to thiazide in Dent's disease. J Am Soc Nephrol, 2002,13(12):2938-2944
[34]Takemura T, Hino S, Ikeda M, et al. Identification of two novel mutations in the CLCN5 gene in Japanese patients with familial idiopathic low molecular weight proteinuria (Japanese Dent's disease). Am J Kidney Dis, 2001,37(1):138-143
[35]Yamamoto K, Cox JP, Friedrich T, et al. Characterization of renal chloride channel (CLCN5) mutations in Dent's disease. J Am Soc Nephrol, 2000,11(8):1460-1468
[36]Igarashi T, Inatomi J, Ohara T, et al. Clinical and genetic studies of CLCN5 mutations in Japanese families with Dent's disease. Kidney Int, 2000,58(2):520-527
[37]Scheinman SJ, Cox JP, Lloyd SE, et al. Isolated hypercalciuria with mutation in CLCN5: relevance to idiopathic hypercalciuria. Kidney Int, 2000,57(1):232-239
[38]Thakker RV. Pathogenesis of Dent's disease and related syndromes of X-linked nephrolithiasis. Kidney Int, 2000,57(3):787-793
[39]Suzuki S, Suzuki J, Kume K, et al. Poor renal accumulation of 99mTc-DMSA in idiopathic tubular proteinuria. Nephron, 1999,81(1):49-54
[40]Cox JP, Yamamoto K, Christie PT, et al. Renal chloride channel, CLCN5, mutations in Dent's disease. J Bone Miner Res, 1999,14(9):1536-1542
[41]Santucci L, Candiano G, Anglani F, et al. Urine proteome analysis in Dent's disease shows high selective changes potentially involved in chronic renal damage. J Proteomics, 2016,130:26-32
[42]Szczepanska M, Zaniew M, Recker F, et al. Dent disease in children: diagnostic and therapeutic considerations. Clin Nephrol, 2015,84(4):222-230
[43]Armanet N, Metay C, Brisset S, et al. Double Xp11.22 deletion including SHROOM4 and CLCN5 associated with severe psychomotor retardation and Dent disease. Mol Cytogenet, 2015,8:8
[44]Mansour-Hendili L, Blanchard A, Le Pottier N, et al. Mutation Update of the CLCN5 Gene Responsible for Dent Disease 1. Hum Mutat, 2015,36(8):743-752
[45]Anglani F, D'Angelo A, Bertizzolo LM, et al. Nephrolithiasis, kidney failure and bone disorders in Dent disease patients with and without CLCN5 mutations. Springerplus, 2015,4:492
[46]Platt C, Jadresic L, Dudley J, et al. Dent's disease complicated by an acute Budd-Chiari syndrome. BMJ Case Rep, 2014,2014
[47]Cramer MT, Charlton JR, Fogo AB, et al. Expanding the phenotype of proteinuria in Dent disease. A case series. Pediatr Nephrol, 2014,29(10):2051-2054
[48]Sekine T, Komoda F, Miura K, et al. Japanese Dent disease has a wider clinical spectrum than Dent disease in Europe/USA: genetic and clinical studies of 86 unrelated patients with low-molecular-weight proteinuria. Nephrol Dial Transplant, 2014,29(2):376-384
[49]Ashida A, Yamamoto D, Nakakura H, et al. Molecular effect of a novel missense mutation, L266V, on function of ClC-5 protein in a Japanese patient with Dent's disease. Clin Nephrol, 2014,82(1):58-61
[50]Park E, Choi HJ, Lee JM, et al. Muscle involvement in Dent disease 2. Pediatr Nephrol, 2014,29(11):2127-2132
[51]Valina MR, Larsen CP, Kanosky S, et al. A novel CLCN5 mutation in a boy with asymptomatic proteinuria and focal global glomerulosclerosis. Clin Nephrol, 2013,80(5):377-384
[52]Fervenza FC. A patient with nephrotic-range proteinuria and focal global glomerulosclerosis. Clin J Am Soc Nephrol, 2013,8(11):1979-1987
[53]Addis M, Meloni C, Tosetto E, et al. An atypical Dent's disease phenotype caused by co-inheritance of mutations at CLCN5 and OCRL genes. Eur J Hum Genet, 2013,21(6):687-690
[54]Ramos-Trujillo E, Claverie-Martin F, Garcia-Nieto V, et al. Dent's disease: Identification of seven new pathogenic mutations in the CLCN5 gene. J Pediatr Genet, 2013,2(3):133-140
[55]Okamoto T, Tajima T, Hirayama T, et al. A patient with Dent disease and features of Bartter syndrome caused by a novel mutation of CLCN5. Eur J Pediatr, 2012,171(2):401-404
[56]Vaisbich MH, Henriques LS, Igarashi T, et al. The long-term use of enalapril and hydrochlorothiazide in two novel mutations patients with Dent's disease type 1. J Bras Nefrol, 2012,34(1):78-81
[57]Becker-Cohen R, Rinat C, Ben-Shalom E, et al. Vitamin A deficiency associated with urinary retinol binding protein wasting in Dent's disease. Pediatr Nephrol, 2012,27(7):1097-1102
[58]Samardzic M, Pavicevic S, Ludwig M, et al. Effect of growth hormone replacement therapy in a boy with Dent's disease: a case report. J Med Case Rep, 2011,5:400
[59]Bogdanovic R, Draaken M, Toromanovic A, et al. A novel CLCN5 mutation in a boy with Bartter-like syndrome and partial growth hormone deficiency. Pediatr Nephrol, 2010,25(11):2363-2368
[60]Hellemans R, Verpooten GA, Bosmans J L. A young man presenting with recurrent nephrolithiasis. NDT Plus, 2010,3(6):584-587
[61]Lee BH, Lee SH, Choi HJ, et al. Decreased renal uptake of (99m)Tc-DMSA in patients with tubular proteinuria. Pediatr Nephrol, 2009,24(11):2211-2216
[62]Bokenkamp A, Bockenhauer D, Cheong H I, et al. Dent-2 disease: a mild variant of Lowe syndrome. J Pediatr, 2009,155(1):94-99
[63]Frishberg Y, Dinour D, Belostotsky R, et al. Dent's disease manifesting as focal glomerulosclerosis: Is it the tip of the iceberg?. Pediatr Nephrol, 2009,24(12):2369-2373
[64]Marsenic O, Kaplan BS. Hydrochlorothiazide-induced tubulointerstitial nephritis in a patient with Dent disease. NDT Plus, 2009,2(3):264-265
[65]Tosetto E, Addis M, Caridi G, et al. Locus heterogeneity of Dent's disease: OCRL1 and TMEM27 genes in patients with no CLCN5 mutations. Pediatr Nephrol, 2009,24(10):1967-1973
[66]Wu F, Reed AA, Williams SE, et al. Mutational analysis of CLC-5, cofilin and CLC-4 in patients with Dent's disease. Nephron Physiol, 2009,112(4):53-62
[67]Grand T, Mordasini D, L'Hoste S, et al. Novel CLCN5 mutations in patients with Dent's disease result in altered ion currents or impaired exchanger processing. Kidney Int, 2009,76(9):999-1005
[68]Tosetto E, Ceol M, Mezzabotta F, et al. Novel mutations of the CLCN5 gene including a complex allele and A 5' UTR mutation in Dent disease 1. Clin Genet, 2009,76(4):413-416
[69]Dinour D, Davidovitz M, Levin-Iaina N, et al. Truncating mutations in the chloride/proton ClC-5 antiporter gene in Seven Jewish Israeli families with Dent's 1 disease. Nephron Clin Pract, 2009,112(4):262-267
[70]Sethi SK, Ludwig M, Kabra M, et al. Vitamin A responsive night blindness in Dent's disease. Pediatr Nephrol, 2009,24(9):1765-1770
[71]Ji LN, Chen CY, Wang JJ, et al. A novel CLCN5 mutation in a Chinese boy with Dent's disease. World J Pediatr, 2014,10(3):275-277
[72]Zhang H, Wang C, Yue H, et al. Identification of a novel mutation in the CLCN5 gene in a Chinese family with Dent-1 disease. Nephrology (Carlton), 2014,19(2):80-83
[73]Li P, Huang JP. Phenotype and genotype of Dent's disease in three Chinese boys. Nephrology (Carlton), 2009,14(2):139-142
[74]张宏博, 黄建萍. 药物治疗 Dent 病15例的临床疗效. 中华实用儿科临床杂志, 2016(3):226-230
[75]简珊, 魏珉, 何艳燕, 等. Dent病4例临床及基因分析. 中国当代儿科杂志, 2015(12):1261-1266
[76]朱碧溱, 李鹏, 黄建萍. 以小分子蛋白尿为主要表现的Dent病六例临床及基因分析. 中华儿科杂志, 2010,48(5):329-333
[77]Sekine T, Komoda F, Miura K, et al. Japanese Dent disease has a wider clinical spectrum than Dent disease in Europe/USA: genetic and clinical studies of 86 unrelated patients with low-molecular-weight proteinuria. Nephrol Dial Transplant, 2014,29(2):376-384
[78]Edvardsson VO, Goldfarb DS, Lieske JC, et al. Hereditary causes of kidney stones and chronic kidney disease. Pediatr Nephrol, 2013,28(10):1923-1942
(本文编辑:张崇凡)
Five case series of Dent-1 disease and literature review
ZHANG Ya, FANG Xiao-yan, XU Hong, SHEN Qian
(Department of Nephrology, Children's Hospital of Fudan University, Shanghai Kidney Development & Pediatric Kidney Disease Research Center, Shanghai 201102, China)
SHEN Qian,E-mail: shenqianjing@aliyun.com
Objective To summarize the clinical data of five cases of Dent-1 disease so as to improve our understanding of the disease. MethodsClinical data of five cases with Dent-1 disease were summarized, including clinical manifestations, laboratory findings and renal pathological changes. Mutation analysis onCLCN5 andOCRLgenes was performed by direct sequencing in these families. Related literatures of Dent-1 disease were reviewed and the phenotypes and genotypes were summarized.ResultsLaboratory findings of five patients showed 24-hr urine protein ranged from 33.0 to 68.9 mg·kg-1, and high levels of urinary α1-microglobulin, albuminuria, immunoglobulin G and hypercalciuria, and one patient with microscopic haematuria and other two patients with nephrocalcinosis. FiveCLCN5 mutations were detected, including R637X, Y479X, G530V, W103fsX104 and R707X, respectively. Y479X, G530V and W103fsX104 were novel mutations. Among 260 articles related to Dent's disease, we found 72 case reports or case series of Dent-1 disease including 598 patients, 422 from Europe and America and 176 from Asia. Except low-molecular-weight proteinuria, the incidence between Europe and America cases and Asia cases of hypercalciuria, nephrocalcinosis, rickets and renal insufficiency were statistically significantly different. No significant correlations between phenotypes and genotypes in all cases were found, including nonsense mutations, missense mutations and frameshift mutations. ConclusionClinical diagnosis of Dent-1 disease should be confirmed byCLCN5 mutation test to avoid unnecessary immunosuppressants therapy.CLCN5 mutations show high heterogenetic, and the relationships between the phenotypes and genotypes of Dent-1 disease are not found yet.
Children; Low-molecular-weight proteinuria; Dent-1 disease;CLCN5 gene mutation ; Chronic renal disease
复旦大学附属儿科医院肾脏科,上海市肾脏发育和儿童肾脏病研究中心 上海,201102
沈茜,E-mail: shenqianjing@aliyun.com
10.3969/j.issn.1673-5501.2016.05.014
2016-08-13
2016-10-08)