北京协和医院成年人不安腿综合征调查
陈健华,黄 蓉,罗金梅,肖 毅,钟 旭,刘秀琴
中国医学科学院 北京协和医学院 北京协和医院 1神经科 2呼吸内科,北京 100730
·论 著·
北京协和医院成年人不安腿综合征调查
陈健华1,黄 蓉2,罗金梅2,肖 毅2,钟 旭2,刘秀琴1
中国医学科学院 北京协和医学院 北京协和医院1神经科2呼吸内科,北京 100730
目的 调查北京协和医院成年人不安腿综合征(RLS)患者的患病情况、疲劳严重度、睡眠质量、日间嗜睡、病情严重度及焦虑抑郁情况。方法 连续入组有睡眠相关症状主诉的门诊患者4739例,年龄小于18岁者排除在外。所有受试者回答RLS量表,满足4个条件的患者将接受随访以及进一步检查。RLS症状严重度使用中国国际RLS量表(IRLS-C)评估。收集同时期年龄性别匹配的无睡眠障碍或肢体不适、未服用任何药物的健康者和连续门诊就诊的失眠而非RLS的患者作为正常对照组(n=42)和非RLS失眠对照组(n=42)。采用皮茨堡睡眠质量量表(PSQI)、疲劳严重度量表(FSS)、爱泼沃斯嗜睡量表(ESS)和综合医院焦虑抑郁量表(HADS)对原发性RLS患者和正常对照组及非RLS失眠对照组患者进行评估和比较。结果 4739例有睡眠相关症状主诉的门诊患者中,有162例(3.42%)满足4条标准,其中,24例因为临床资料不完整或失访归为原因不明分类不清的RLS,42例(0.89%)为原发性RLS,63例(1.33%)为继发性RLS,33例(0.70%)为RLS样疾病。42例原发性RLS患者中,41例(97.6%)睡眠质量差,13例(31.0%)存在焦虑,4例(9.5%)有抑郁。原发性RLS患者的PSQI(q=11.69,P=0.000)、HADA(q=8.02,P=0.000)和HADD(q=6.60,P=0.000)得分明显高于正常对照组,FSS(q=3.74,P=0.001)、ESS(q=2.97,P=0.012)和HADD(q=4.15,P=0.000)得分明显低于非RLS失眠对照组患者。HADA和HADD评分与PSQI评分(r=0.340,P=0.028;r=0.383,P=0.012)、FSS评分(r=0.445,P=0.003;r=0.511,P=0.001)及IRLS评分(r=0.477,P=0.001;r=0.578,P=0.000)呈显著正相关。结论 对因为失眠和/或肢体不适感而就诊的患者应考虑RLS的可能。原发性RLS患者睡眠质量差,焦虑抑郁发生率高。临床医生需要对原发性和继发性RLS进行鉴别诊断,同时除外RLS样疾病。
不安腿综合征;睡眠;疲劳;焦虑;抑郁
ActaAcadMedSin,2016,38(5):548-553
不安腿综合征(restless legs syndrome,RLS)是指非活动状态下出现的下肢难以忍受的不适,夜间明显,迫使患者不停地活动患肢,通过活动症状可以得到暂时缓解。不同国家和地区的RLS患病率差异很大,北美和西欧国家为4%~29%[1],日本为0.85%~1.80%[2- 5],韩国为0.9%~12.1%[6- 11],新加坡为0.1%~0.6%[12]。本研究调查了北京协和医院42例RLS患者的患病情况、睡眠质量、疲劳严重度、日间嗜睡、病情严重度及焦虑抑郁情况,以期为今后的临床诊疗提供参考。
对象和方法
对象 2012年10月至2014年6月在北京协和医院门诊以任何与睡眠相关性症状为主诉(包括失眠和/或肢体不适感)就诊的患者。年龄小于18岁的患者排除在外。
RLS诊断 在取得知情同意后,所有受试者回答 国际不安腿综合征研究组(International Restless Legs Syndrome Study Group,IRLSSG)制定的RLS自评量表,具体为:(1)你由于肢体不适感,导致有强烈运动肢体的愿望吗?(2)这种想要运动肢体的愿望或不适感是出现于坐着或躺下休息时或者在那时会加重吗?(3)这种不适感会在运动时暂时缓解吗?(4)这种安静时出现的想要运动肢体的不适感是只发生于夜间或在夜间休息时加重吗[13- 14]?
所有满足上述4个条件的受试者将被介绍给睡眠障碍专业的临床医生以进一步了解病史和进行体格检查。这些受试者还将接受包括血常规、铁四项、肝肾功能、血糖、甲状腺功能在内的血液检查及定期门诊和电话随访,必要时加做肌电图、头颅或脊髓核磁共振检查。采用IRLSSG 2014年修订的标准[14]将患者分为原发性RLS、继发性RLS和RLS样疾病。
量表评估和组间比较 以同期年龄性别匹配的无睡眠障碍或肢体不适、未服用任何药物的健康者(正常对照组,n=42)和同时期连续门诊就诊的失眠而非RLS的患者(非RLS失眠对照组,n=42)为对照,采用皮茨堡睡眠质量量表(Pittsburgh Sleep Quality Index,PSQI)、疲劳严重度量表(Fatigue Severity Scale,FSS)、爱泼沃斯嗜睡量表(Epworth Sleeping Scale,ESS)、综合医院焦虑抑郁量表(Hospital Anxiety and Depression Scale,HADS)和中国国际RLS量表(International RLS Study Group Rating Scale,IRLS-C)[15]评估受试者的睡眠质量、疲劳严重度、日间嗜睡情况、病情严重度、焦虑抑郁状态和RLS症状严重度,并与与原发性RLS患者(原发性RLS组)进行比较。
统计学处理 采用SPSS 20.0统计软件,RLS组和对照组比较采用方差分析和q检验方法,RLS组焦虑抑郁相关因素的分析采用Spearman相关分析,P<0.05为差异有统计学意义。
结 果
一般情况 4739例有睡眠相关症状主诉的门诊患者中,有162例(3.42%)满足4条标准,其中,24例因为临床资料不完整或失访归为原因不明分类不清的RLS,42例(0.89%)为原发性RLS,63例(1.33%)为继发性RLS,33例(0.70%)为RLS样疾病。
42例原发性RLS患者中,男16例,女26例;平均年龄为(54.4±13.3)岁(20~80岁);确诊时平均病程(10.2±9.1)个月(0.5~38个月);平均随访时间(24.0±6.0)个月(12~32个月);平均IRLS评分(20.4±8.2)分(7~36分),其中,50%为重度RLS患者(IRLS>20分)。40例(95.2%)为慢性持续型,未治疗时在1年时间里症状出现次数大于或等于每周2次;2例(4.8%)为间歇型,未治疗时在1年时间里症状出现次数小于每周2次,并且出现过至少5个周期。4例(9.5%)患者以上肢症状首发起病,38例(90.5%)以下肢症状首发起病。3例患者(7.1%)有阳性家族史。9例患者(21.4%)未服药,3例患者(7.1%)按需服药,30例患者(71.4%)长期服药;所服用的药物主要包括多巴胺受体激动剂、左旋多巴类药物、加巴喷丁和镇静催眠药。41例患者(97.6%)睡眠质量差,38例患者(90.5%)为睡眠始动性失眠(入睡困难),26例患者(62.1%)有睡眠中期失眠(夜醒频繁),14例患者(33.3%)存在终期失眠(早醒)。13例患者(31.0%)存在焦虑,4例患者(9.5%)有抑郁,其中,4.8%为重度焦虑,2.4%为重度抑郁。
63例继发性RLS 患者中,男23例,女40例,平均年龄(57.4±15.3)岁(24~90岁)。最常见的病因是铁缺乏(15例,23.8%)和周围神经病(15例,23.8%),其次为终末期肾病(9例,14.3%)、神经根病(5例,7.9%)、类风湿性关节炎(3例,4.8%)、甲状腺功能减退(3例,4.8%)、缺血性脑梗死(3例,4.8%)、抗抑郁药物治疗(3例,4.8%),然后依次为脊髓病(2例,3.2%)、干燥综合征(2例,3.2%)、甲状腺功能亢进(1例,3.2%)、多发性硬化(1例,1.6%)、强直性脊柱炎(1例,1.6%)。临床方面全部为慢性持续型。
33例RLS样疾病患者中,男10例,女23例,平均年龄(60.7±15.6岁)(24~85岁)。病因分别为关节痛(18例,54.5%)、全面性焦虑(9例,27.3%)、痛性痉挛(2例,6.1%)、静脉淤滞(2例,6.1%)、肌痛(1例,3.0%)、多重状态(1例,3.0%)。其中,5例(15.2%)为慢性持续型,28例(84.8%)为间歇型。
各组间睡眠质量、疲劳严重度、日间嗜睡和焦虑抑郁情况的比较 原发性RLS患者的PSQI(q=11.69,P=0.000)、综合医院焦虑量表(Hospital Anxiety and Depression Scale for Anxiety,HADA)(q=8.02,P=0.000)和综合医院抑郁量表(Hospital Anxiety and Depression Scale for Depression,HADD)(q=6.60,P=0.000)得分明显高于正常对照组,FSS(q=3.74,P=0.001)、ESS(q=2.97,P=0.012)和HADD(q=4.15,P=0.000)得分明显低于非RLS失眠对照组患者(表1)。
焦虑抑郁相关危险因素 相关分析结果显示,原发性RLS患者HADA和HADD评分与PSQI评分(r=0.340,P=0.028;r=0.383,P=0.012)、FSS评分(r=0.445,P=0.003;r=0.511,P=0.001)及IRLS评分(r=0.477,P=0.001;r=0.578,P=0.000)呈显著正相关。
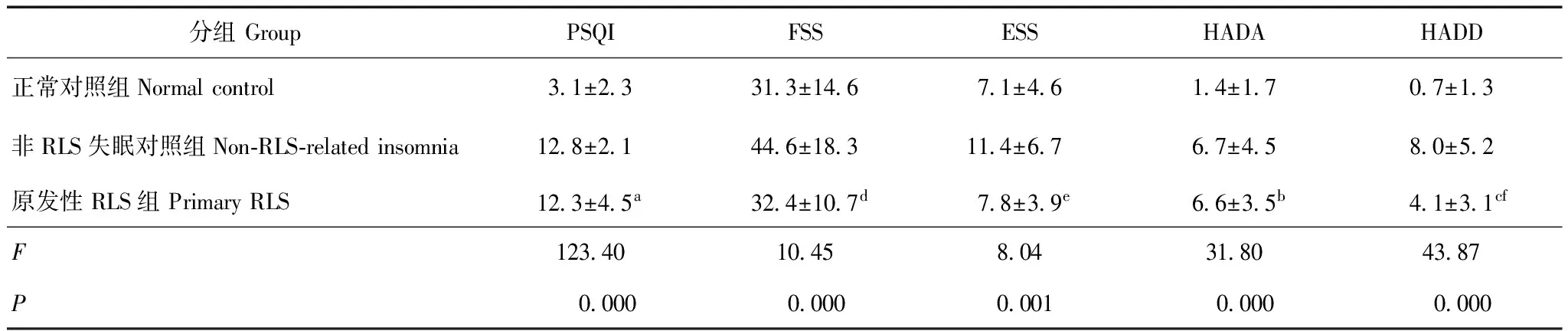
表 1 各组睡眠质量、 疲劳严重度、日间嗜睡和焦虑抑郁情况的比较(n=42,x-±s,分)
RLS:不安腿综合征;PSQI:皮茨堡睡眠质量量表;FSS:疲劳严重度量表;ESS:爱泼沃斯嗜睡量表;HADA:综合医院焦虑量表;HADD:综合医院抑郁量表;与正常对照组比较,aq=11.69,P=0.000;bq=8.02,P=0.000;cq=6.60,P=0.000;与非RLS失眠对照组比较,dq=3.74,P=0.001;eq=2.97,P=0.012;fq=4.15,P=0.000
RLS: restless legs syndrome; PSQI: Pittsburgh Sleep Quality Index; FSS: Fatigue Severity Scale; ESS: Epworth Sleepiness Scale; HADA: Hospital Anxiety and Depression Scale for Anxiety; HADD: Hospital Anxiety and Depression Scale for Depression;aq=11.69,P=0.000;bq=8.02,P=0.000;cq=6.60,P=0.000 compared with normal control group;dq=3.74,P=0.001;eq=2.97,P=0.012;fq=4.15,P=0.000 compared with Non-RLS-related insomnia group
讨 论
尽管亚洲已有关于RLS患病情况的报道[2- 12,16- 30],但还存在如下缺憾:(1)绝大多数报道中关于RLS的诊断标准还是基于1995年或2003年的诊断标准,只要满足4个条件即诊断为RLS,而没有除外继发性RLS或者RLS样疾病,这样会高估RLS的患病情况;还有些研究采用仅满足1个问题或2条及以上标准即诊断,这样显然不合适[3,5- 7,27]。(2)由于既往一些研究中关于原发性RLS和继发性RLS混淆不清,不利于临床病因及特点分析。(3)既往多数研究仅仅为症状诊断,缺乏血液检查和神经传导速度和肌电检查,这使得RLS的诊断具有不确定性。Hening等[31]研究发现,普通人群中许多情况都可满足RLS诊断中的4个标准,但这并不是真正的RLS。Benes等[32]估算RLS诊断的假阳性率可高达10%。因此国际RLS联盟于2012年重新修订了RLS诊断标准,增加了需要除外RLS样疾病一项。本研究则避免了上述缺陷,分别调查了原发性、继发性RLS和RLS样疾病的患病情况。结果显示,原发性、继发性RLS和RLS样疾病均以女性患者居多,半数以上年龄大于45岁。大部分原发性RLS以下肢症状为首发起病,得到确诊时常常已是慢性持续性重症患者。RLS的症状可导致明显的不适,使患者痛苦不堪,是一种中重度影响健康的疾病[33- 34]。
本研究中,原发性RLS患者的睡眠质量差,发生率高达97.6%,睡眠初期、中期、末期失眠常见,焦虑抑郁发生率高,近1/3患者合并焦虑,1/10患者合并抑郁。与非RLS的失眠患者比较,在睡眠质量严重程度相差不大的情况下,焦虑的发生率相差不大,抑郁、日间嗜睡、疲劳感发生率低于非RLS失眠患者。合并失眠和焦虑是RLS患者的突出问题,抑郁的发生可能与失眠有关。推测原发性RLS患者早期就诊率低的原因可能与日间嗜睡和疲劳感不突出有一定关系。
继发性RLS是指发生原发性疾病随后出现的RLS相关症状,其责任病灶大多位于脑桥、放射冠、基底节区或脊髓[35- 37],发病机制不清。本研究中,3例脑梗死和1例多发性硬化患者的病灶位于脑桥、放射冠和基底节区;2例脊髓病患者的病灶位于颈段和胸段脊髓。继发性RLS最常见的病因是铁缺乏和周围神经病,在排查RLS相关病因时有必要行血常规、铁四项、肝肾功能、血糖等化验,必要时行肌电图检查。精神类药物也是主要导致继发性RLS的原因之一,机制尚不清楚。其中,抗抑郁药物最常见,其他如喹硫平、锂剂、阿片类药物撤药也有报道[38]。此外,止吐药、抗组胺药物、钙通道阻滞剂降压药也可诱发或加重RLS症状。RLS样疾病包括腿部痉挛、位置性不适、关节痛、神经质性动作、睡眠痉挛、习惯性晃腿或扣脚等,通过详细询问病史有助于鉴别诊断,临床发作类型大部分为间歇型。
与高加索人种相比,亚洲人种RLS患病率更低[26]。本研究中,原发性RLS占所有失眠和/或肢体不适主诉患者的构成比为0.89%,远低于北美和西欧国家,比以往亚洲国家和区域报道的也低。关于RLS患病率在不同区域有差异的原因,推测可能与采用的RLS诊断标准有关,一些研究中没有把继发性RLS和RLS样疾病排除在外。本研究结果与Mizuno等[2]、Tsuboi等[4]和Cho等[8]的数据相近,后者分别为0.85%、0.96%和0.90%。
尽管本研究在随访过程中再次询问了家族史,但依然发现原发性RLS的家族史仅为7.1%,远低于以往国际上的报道(60%以上)[39],也低于亚洲国家的报道(18.5%~54.7%),推测原因可能是临床医生既往对RLS认识和诊断不足,患者给予重视度不够,以及患病后未寻求医学帮助。然而,本研究中的家族史也明显低于Li等[25]和Ma等[26]在上海和青岛区域调查得出的22.2%和27.0%的阳性家族史结果,推测原因为上述地区属于华东,而本研究中73.5%的患者来自于华北地区,华东地区仅占7.1%,RLS可能在不同区域的患病情况不同。Tan等[12]研究结果显示,人种和地理区域可以导致RLS患病率不同。
目前国际上关于RLS的诊断标准共有3个,分别是IRLSSG修订标准、国际睡眠障碍分类第3版(International Classification of Sleep Disorders,third edition,ICSD- 3)标准和精神类疾病诊断和统计手册第5版(Diagnostic and Statistical Manual of Mental Disorders,fifth edition,DSM- 5)[40],与DSM- 5标准不同,ICSD- 3的诊断标准更贴近于IRLSSG修订标准[40]。相对而言,IRLSSG修订后的5条标准更加严密,有助于临床确诊,更多地被临床所采用。尽管RLS在普通人群中较常见,但临床医生的认识以及患者寻求医学帮助的意识还是不够,导致RLS诊断率低。因此,对于因为失眠和/或肢体不适感而就诊的患者需询问RLS自评量表中的4个问题,避免漏诊或误诊。在诊断时需要对原发性和继发性RLS进行鉴别,同时除外RLS样疾病,继发性RLS尚需治疗原发病。
[1]Innes KE,Selfe TK,Agarwal P. Prevalence of restless legs syndrome in North American and Western European populations: a systematic review [J]. Sleep Med,2011,12(7):623- 634.
[2]Mizuno S,Miyaoka T,Inagaki T,et al. Prevalence of restless legs syndrome in non-institutionalized Japanese elderly [J]. Psychiatry Clin Neurosci,2005,59(4): 461- 465.
[3]Nomura T,Inoue Y,Kusumi M,et al. Prevalence of restless legs syndrome in a rural community in Japan [J]. Mov Disord,2008,23(16):2363- 2369.
[4]Tsuboi Y,Imamura A,Sugimura M,et al. Prevalence of restless legs syndrome in a Japanese elderly population [J]. Parkinsonism Relat Disord,2009,15(8):598- 601.
[5]Kagimura T,Nomura T,Kusumi M,et al. Prospective survey on the natural course of restless legs syndrome over two years in a closed cohort [J]. Sleep Med,2011,12(9):821- 826.
[6]Kim J,Choi C,Shin K,et al. Prevalence of restless legs syndrome and associated factors in the Korean adult population: the Korean Health and Genome Study [J]. Psychiatry Clin Neurosci,2005,59(3):350- 353.
[7]Cho YW,Shin WC,Yun CH,et al. Epidemiology of restless legs syndrome in Korean adults[J]. Sleep,2008,31(2):219- 223.
[8]Cho SJ,Hong JP,Hahm BJ,et al. Restless legs syndrome in a community sample of Korean adults: prvevalence,impact on qualtiy of life,and association with DSM-Ⅳ psychiatric disorders [J]. Sleep,2009,32(8):1069- 1076.
[9]Kim KW,Yoon IY,Chung S,et al. Prevalence,comorbidities and risk factors of restless legs syndrome in the Korean elderly population-results from the Korean Logitudinal Study on Health and Aging [J]. J Sleep Res,2010,19(1 Pt 1):87- 92.
[10]Park YM,Lee HJ,Kang SG,et al. Prevalence of idiopathic and secondary restless legs syndrome in Korean women [J]. Gen Hosp Psychiatry,2010,32(2):164- 168.
[11]Kim WH,Kim BS,Kim SK,et al. Restless legs syndrome in older people: a community-based study on its prevalence and association with major depressive disorder in older Korean adults [J]. Int J Geriatr Psychiatry,2012,27(6):565- 572.
[12]Tan EK,Seah A,See SJ,et al. Restless legs syndrome in an Asian populaiton: a study in Singapore [J]. Mov Disord,2003,16(3):577- 579.
[13]Allen RP,Picchietti D,Hening WA,et al. Restless legs syndrome: diagnostic criteria,special considerations,and epidemilogy: a report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institues of Health [J]. Sleep Med,2003,4(2):101- 119.
[14]Allen RP,Picchietti DL,Garcia-Borreguero D,et al. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria--history,rationale,description,and significance [J]. Sleep Med,2014,15(8):860- 873.
[15]Chen YL,Lin SW,Chuang LP,et al. Validation assessment of the Chinese version of the international restless legs scale [J]. Thorac Med,2013,28(2):65- 72.
[16]Rangarajan S,Rangarajan S,D’Souza GA. Restless legs syndrome in an Indian urban population [J]. Sleep Med,2007,9(1):88- 93.
[17]Gupta R,Lahan V,Goel D. Restless legs syndrome: a common disorder,but rarely diagnosed and barely treated-an Indian experience [J]. Sleep Med,2012,13(7): 838- 841.
[18]Panda S,Taly AB,Sinha S,et al. Sleep-related disorders among a healthy population in South India [J]. Neurol India,2012,60(1):68- 74.
[19]Sevim S,Dogu O,Camdeviren H,et al. Unexpectedly low prevalence and unusual characteristics of RLS in Mersin,Turkey [J]. Neurology,2003,61(11): 1562- 1569.
[20]Erer S,Karli N,Zarifoglu M,et al. The prevalence and clinical features of restless legs syndrome: a door to door population study in Orhangazi,Bursa in Turkey [J]. Neurol India,2009,57(6):729- 733.
[22]Civi S,Kutlu R,Tokgoz S. Frequency,severity and risk factors for restless legs syndrome in healthcare personnel [J]. Neurosciences (Riyadh),2012,17(3):230- 235.
[23]Çurgunlu A,Döventas A,Karadeniz D,et al. Prevalence and characteristics of restless legs syndrome (RLS) in the elderly and relation of serum ferritin levels with disease severity: hospital-based study from Istanbul,Turkey [J]. Arch Gerontol Geriatr,2012,55(1):73- 76.
[24]Yilmaz NH,Akbostanci MC,Oto A,et al. Prevalence of restless legs syndrome in Ankara,Turkey: an analysis of diagnostic criteria and awareness [J]. Acta Neurol Belg,2013,113(3):247- 251.
[25]Li LH,Chen HB,Zhang LP,et al. A community-based investigation on restless legs syndrome in a town in China [J]. Sleep Med,2012,13(4):342- 345.
[26]Ma JF,Xin XY,Liang L,et al. Restless legs syndrome in Chinese elderly people of an urban suburb in Shanghai: a community-based survey [J]. Parkinsonism Relat Disord,2012,18(3):294- 298.
[27]Shi Y,Yu H,Ding D,et al. Prevalence and risk factors of restless legs syndrome among Chinese adults in a rural community of Shanghai in China [J]. PLoS One,2015,10(3):e0121215.
[28]Chen NH,Chuang LP,Yang CT,et al. The prevalence of restless legs syndrome in Taiwanese adults [J]. Psychiatry Clin Neurosci,2010,64(2):170- 178.
[29]Lin SW,Chen YL,Kao KC,et al. Diseases in patients coming to a sleep center with symptoms related to restless legs syndrome [J]. PLoS One,2013,8(8):e71499.
[30]BaHammam A,Al-shahrani K,Al-zahrani S,et al. The pre-valence of restless legs syndrome in adult Saudis attending primary health care [J]. Gen Hosp Psychiatry,2011,33(2):102- 106.
[31]Hening WA,Allen RP,Washburn M,et al. The four diagnostic criteria for restless legs syndrome are unable to exclude confounding conditons (“mimics”) [J]. Sleep Med,2009,10(9):976- 981.
[32]Benes H,Walters AS,Allen RP,et al. Definition of restless legs syndrome,how to diagnose it,and how to differentiate it from RLS mimics [J]. Mov Disord,2007,22(Suppl 18):S401- S408.
[33]Earley CJ,Silber MH. Restless legs syndrome: understanding its consequences and the need for better treatment [J]. Sleep Med,2010,11(9):807- 815.
[34]Becker PM,Novak M. Diagnosis,comorbidities,and management of restless legs syndrome [J]. Curr Med Res Opin,2014,30(8):1441- 1460.
[35]Lee SJ,Kim JS,Song IU,et al. Poststroke restless legs syndrome and lesion location: anatomical considerations [J]. Mov Disord,2009,24(1):77- 84.
[36]Ruppert E,Kilic-Huck U,Wolff V,et al. Brainstem stroke-related restless legs syndrome: frequency and anatomical considerations [J]. Eur Neurol,2015,73(1- 2):113- 118.
[37]Zwartbol RT,Jellema K,Boiten J,et al. Acute exacerbation of restless legs due to cervical spinal cord ischaemia [J]. BMJ Case Rep,2013,pii:bcr2012007930. doi:10.1136/bcr- 2012- 007930.
[38]Cohrs S,Rodenbeck A,Homyak M,et al. Restless legs syn-drome,periodic limb movements,and psychopharmacology [J]. Nervenarzt,2008,79(11):1263- 1264,1266- 1272.
[39]Lavigne GJ,Montplaisir JY. Restless legs syndrome and sleep bruxism: prevalence and association among Canadians [J]. Sleep,1994,17(8):739- 743.
[40]Marelli S,Galbiati A,Rinaldi F,et al. Restless legs syndrome/Willis Ekbom disease: new diagnostic criteria according to different nosology [J]. Arch Ital Biol,2015,153(2- 3):184- 193.
Restless Legs Syndrome in Adults in Peking Union Medical College Hospital
CHEN Jian-hua1,HUANG Rong2,LUO Jin-mei2,XIAO Yi2,ZHONG Xu2,LIU Xiu-qin1
1Department of Neurology,2Department of Respiratory,PUMC Hospital,CAMS and PUMC,Beijing 100730,China
HUANG Rong Tel:010- 69155032,E-mail: huangrong0212@163.com
Objective To investigate the clinical characteristics of restless legs syndrome (RLS) in adults in Peking Union Medical College Hospital and explore the sleep quality,fatigue degree,daytime sleepiness,disease severity,depression and anxiety of RLS patients.Methods Totally 4739 consecutive patients who visited the outpatient departments with any sleep complaint or leg discomforts were recruited in the study. Patients under 18 years were excluded. All participants answered RLS questionnaire. The subjects fulfilled all four criteria would be followed up and given advanced examinations to rule out secondary RLS and RLS mimics. Primary RLS patients were evaluated with International Restless Legs Scale (IRLS),Pittsburgh Sleep Quality Index (PSQI),Fatigue Severity Scale (FSS),Epworth Sleepiness Scale (ESS),and Hospital Anxiety and Depression Scale for depression and anxiety (HADD and HADA). Another two groups of age-and gender-matched healthy subjects and non-RLS insomnia patients were served as normal and non-RLS insomnia controls.Results There were 162 (3.42%,162/4739) subjects fulfilling all four criteria for RLS; 42 (0.89%,42/4739) subjects were diagnosed as primary RLS and 33 (0.70%,33/4739) as RLS mimics. In primary RLS patients,41(97.6%) were found to be with poor sleep,13 (31.0%) with anxiety,and 4(9.5%) with depression. The scores of PSQI(q=11.69,P=0.000),HADA(q=8.02,P=0.000),and HADD(q=6.60,P=0.000)in primary RLS patients were significantly higher than those in normal controls. The scores of FSS(q=3.74,P=0.001),ESS(q=2.97,P=0.012),and HADD(q=4.15,P=0.000) in primary RLS patients were significantly lower than those in non-RLS insomnia controls. The scores of HADA and HADD were significantly correlated with those of PSQI(r=0.340,P=0.028;r=0.383,P=0.012),FSS(r=0.445,P=0.003;r=0.511,P=0.001),and IRLS(r=0.477,P=0.001;r=0.578,P=0.000). Conclusions RLS should be considered in the patients with any sleep-related complaint or leg discomforts. Primary RLS patients suffer from bad sleep and are more susceptible to anxiety and depression. Secondary RLS and RLS mimics should be excluded before the diagnosis of primary RLS.
restless legs syndrome; sleep; fatigue; anxiety; depression
黄 蓉 电话:010- 69155032,电子邮件:huangrong0212@163.com
R741
A
1000- 503X(2016)05- 0548- 06
10.3881/j.issn.1000- 503X.2016.05.010
2016- 01- 26)