PKP对骨质疏松椎体压缩骨折患者脊柱矢状位平衡的影响
张景涛,耿伟,徐辉,马金柱,李忠,庞良龙,李昆朋,任杭岭
(1.泰山医学院,山东 泰安 271000;2.聊城市人民医院脊柱外科,山东 聊城 252000)
PKP对骨质疏松椎体压缩骨折患者脊柱矢状位平衡的影响
张景涛1,2,耿伟2*,徐辉2,马金柱2*,李忠2,庞良龙2,李昆朋2,任杭岭2
(1.泰山医学院,山东 泰安271000;2.聊城市人民医院脊柱外科,山东 聊城252000)
目的探讨单节段骨质疏松性椎体压缩骨折(osteoporotic vertebral compression fracture,OVCF)患者椎体后凸成形术(percutaneous balloon kyphoplasty,PKP)对全脊柱矢状位平衡的影响。方法回顾性分析2014年2月至2015年10月符合选择标准的OVCF患者65 例。所有患者均行PKP术。术前及术后末次随访时均摄自然站立位全脊柱(包括双侧股骨头)正侧位X线片,测量骨盆入射角(pelvicincidence,PI)、骨盆倾斜角(pelvic tilt,PT)、骶骨倾斜角(sacral slope,SS)、腰椎前凸角(lumbar lordosis,LL)、胸椎后凸角(thoracic kyphosis,TK)、局部矢状面Cobb 角、C7~S1的矢状面轴向距离(sagittal vertical axis,SVA),并对患者进行疼痛视觉模拟评分(visual analogue scale,VAS)和Oswestry功能障碍指数(oswestry disability index,ODI)评定。评估研究组术前脊柱-骨盆各矢状位参数与正常对照组的关系,并分析研究组患者手术前后各矢状位参数的变化及并发症发生情况。结果所有患者均获随访。术后末次随访时,研究组VAS 评分、ODI评分均较术前显著改善(P<0.05);术前研究组C7~S1的矢状面轴向距离长于正常对照组,差异具有统计学意义(P<0.05);术前研究组TK大于正常对照组,差异具有统计学意义(P<0.05);术前骨盆相关参数中除PI与正常对照组比较差异无统计学意义外,PT、SS改变均具有统计学意义(P<0.05)。术后SVA较术前减小,差异具有统计学意义(P<0.05);脊柱相关参数中,术后LL较术前增大而TK较术前减小,差异均具有统计学意义(P<0.05);骨盆相关参数中,PI、PT、SS术后与术前相比均无统计学意义(P>0.05);局部Cobb角术后与术前相比明显减小,差异具有统计学意义(P<0.05)。术前患者局部Cobb角与C7~S1的矢状面轴向距离没有相关性,然而术后局部Cobb角的变化与C7~S1的矢状面轴向距离的变化显著相关。术中及术后随访均未见严重并发症发生。结论对骨质疏松性椎体压缩骨折患者来说,PKP术是一种有效的微创手术方式,不仅可缓解骨折引起的疼痛,还能够通过改善局部后凸畸形来改善全脊柱的矢状位平衡状态。
椎体压缩性骨折;骨质疏松症;经皮椎体后凸成形术;矢状位平衡
随着社会人口老龄化现象的加剧,老年骨质疏松性椎体压缩骨折(osteoporotic vertebral compression fracture,OVCF)的发病率呈上升趋势[12],球囊扩张椎体后凸成形术(percutaneous balloon kyphoplasty,PKP)是一种微创的治疗疼痛性骨质疏松性椎体压缩骨折的有效方法,其不仅具有止痛与加强椎体强度的作用,而且还具有恢复椎体高度,矫正椎体后凸畸形的作用[3-4]。有报道[5-7],脊柱矢状位平衡最近已成为决定脊柱退行性疾病手术疗效的重要因素之一。然而,国内外关于探讨PKP对全脊柱矢状位序列及矢状位平衡的研究甚少。本研究通过对OVCF患者PKP手术前后影像学进行分析,记录脊柱-骨盆各矢状位参数的变化,并进一步探讨其对各矢状位参数的影响。
1 资料与方法
1.1一般资料收集2014年2月至2015年10月就诊本院脊柱外科符合入组标准的65 例患者作为研究组;选取本院体检中心30 例健康老年人作为正常对照组,其影像学参数值在体检中心影像学资料数据库中获取。
研究组:男24 例,女41 例;年龄62~93 岁,平均74 岁。骨折部位:T81例,T92例,T117例,T1216例,L121例,L212 例,L34 例,L42 例。随访时间5~11个月,平均6个月。正常对照组:男13例,女17例,年龄60~91岁,平均年龄76岁。
1.2患者入组标准所有患者均有明显腰背疼痛,疼痛评分视觉模拟评分(visual analogue scale,VAS)大于等于5分,无神经压迫症状;侧位X线片测量椎体高度丢失在0~80%之间(术前椎体高度丢失率=术前椎体前缘高度/估算的原椎体高度,其中估算的原椎体高度为伤椎相邻上下椎体高度的平均值);CT检查示椎体后壁基本完整;MRI显示伤椎在T1WI呈低信号,抑脂像STIR,SPAIR,IDEAL AST呈高信号,T2WI呈稍高信号或中等信号;无脊柱骨折及手术史;排除脊柱转移瘤;保守治疗2周无效;术前检查无禁忌证,心肺等各项术前检查评估后能耐受手术。手术由同一组医师完成。
1.3手术方法患者取俯卧位,连接心电监护监测生命体征后,在C型臂X线机透视下定位,常规消毒铺巾,以1%利多卡因局部浸润麻醉至骨膜。采用经皮椎体球囊成形手术系统,透视下经单侧椎弓根穿刺,将套管针刺入椎体。在侧位观察针尖超过椎体后缘约2~3 mm停止穿刺,取出内芯,建立工作通道。穿刺成功后抽出穿刺针内芯,置入导丝使其指向近椎体前缘下1/3,拔出穿刺针套管,沿导针置入套管,用精细钻扩大针道,然后置入球囊进行加压扩张,逐渐增加压力,当球囊已扩张达终板或预计的椎体复位效果时停止(预计的椎体复位效果指术中体位复位,我们专门的脊柱手术床可以使患者术中俯卧位,分别以胸部及髂前上棘为支点,腹部悬空,患者处于前驱后仰状态;术中局麻加强化降低患者的疼痛程度以使患者腰背部肌肉充分放松;球囊尽可能的撑开)。调制骨水泥,取出球囊,C型臂X线机监测下将骨水泥缓慢推入椎体空腔内,使空腔完全填充。
1.4术后处理患者术后平卧24 h,吸氧并监测生命体征。常规系统性抗骨质疏松治疗,术后24 h可在腰托保护下站立行走,复查自然站立位全脊柱(包括双侧股骨头)正侧位X线片,观察全脊柱矢状位曲度的变化及伤椎骨水泥的填充情况。
1.5影像学测量及随访指标所有患者在术前及末次随访时均拍摄自然站立位全脊柱(包括双侧股骨头)正侧位X线片,(摄片时人体自然站立,膝部伸直,双目平视,双上肢抱于胸前并上抬45°[8])。测量脊柱-骨盆矢状位参数,各项参数(测量方法见图1)的定义如下:a)C7~S1的矢状面轴向距离(sagittal vertical axis,SVA):C7PL与S1终板后上角的垂直距离(C7PL在骶骨后上角前方为正,后方为负);b)胸椎后凸角(thoracic kyphosis,TK):T4上终板与T12下终板之间的夹角;c)腰椎前凸角(lumbar lordosis,LL):L1上终板与S1上终板之间的夹角;d)骨盆入射角(pelvic incidence,PI):经S1上终板中点作一条S1终板的垂直线,再经S1上终板中点与两股骨头中心连线中点作一直线,夹角为PI角。若双侧股骨头不重叠,取两股骨头中心连线的中点作为中心点;e)骶骨倾斜角(sacrum slope,SS):S1上终板与水平面成角;f)骨盆倾斜角(pelvic tilt,PT):经S1上终板中点与两股骨头中心连线中点作一直线,其与铅垂线之间夹角;g)Cobb角:采用Phillips[9]的测量方法,测量从病椎上一个椎体的上终板到病椎下一个椎体的下终板的Cobb角,定义为“局部矢状面Cobb角”。正常对照组及试验组的各项影像学数据测量均由1名脊柱专科医师完成。所有数据测量3次后取均值。
术前及末次随访时,采用疼痛视觉模拟评分(visual analogue scale,VAS)及Oswestry功能障碍指数(oswestry disability index,ODI)评价研究组疗效。

2 结 果
研究组和对照组两组性别构成比、年龄等一般资料以及术前各项观察指标之间的差异均无统计学意义(P>0.05),具有可比性。
所有患者手术顺利,术中未发生脊髓、神经损伤及球囊破裂。手术时间35~50 min,平均45 min;术后患者常规C型臂下透视,共发现6 例不同程度的骨水泥渗漏患者,所有骨水泥渗漏患者均未出现临床不适症状。1 例患者术中出现轻微胸痛、呼吸困难,考虑骨水泥肺小动脉栓塞,及时抗凝治疗症状缓解。患者均获随访,随访时间5~11个月,平均6个月。随访时拍摄自然站立位全脊柱(包括双侧股骨头)正侧位X线片,均见伤椎骨水泥填充满意。患者疼痛症状均得到明显缓解。随访中发现2 例患者发生邻近椎体再骨折,1 例患者发生手术椎体再骨折。术后末次随访时VAS、ODI评分均较术前明显降低,差异具有统计学意义(P<0.05)。局部Cobb角较术前减小,差异具有统计学意义(P<0.05)。术前患者局部Cobb角与C7~S1SVA没有相关性,然而术后局部Cobb角的变化与C7~S1SVA的变化显著相关。
术前研究组C7~S1的矢状面轴向距离长于正常对照组,差异具有统计学意义(P<0.05);术前研究组TK大于正常对照组,差异具有统计学意义(P<0.05);术前骨盆相关参数中除PI与正常对照组比较差异无统计学意义外,PT、SS改变均差异具有统计学意义(P<0.05),见表1。
术后C7~S1的矢状面轴向距离较术前减小,差异具有统计学意义(P<0.05);脊柱相关参数中,术后LL较术前增大而TK较术前减小,差异均具有统计学意义(P<0.05);骨盆相关参数中,PI、PT、SS术后与术前相比差异均无统计学意义(P>0.05);局部Cobb角术后与术前相比明显减小,差异具有统计学意义(P<0.05),见表2。

表1 研究组术前与正常对照组脊柱骨盆各参数对比±s)

表2 研究组术前与术后脊柱骨盆各参数对比±s)
典型病例为一68 岁男性患者,因“扭伤致腰背部疼痛2 d”入院治疗。术前全脊柱正侧位X线片示T12椎体楔形变扁,T12椎体压缩骨折,行PKP手术;术后8个月复查,全脊柱正侧位X线片示T12椎体内见致密物影。术前测量C7~S1SVA为4.70 mm,PKP术后为2.10 mm,较术前明显减小;术前测量Cobb角为10.10°,PKP术后为4.60°,较术前明显减小;术前测量PI为52.4°,PKP术后为53.5°,手术后未见明显改变;术前测量PT为26.7°,PKP术后为25.4°,手术后未见明显改变;术前测量SS为25.7°,PKP术后为28.1°,手术后未见明显改变;术前测量LL为37.9°,PKP术后为43.6°,较术前增大;术前测量TK为60.1°,PKP术后为50.2°,较术前减小。手术前后各参数示意见图2~3。
3 讨 论
临床研究显示[10],目前临床对骨质疏松性椎体压缩骨折研究已较为成熟透彻,经皮椎体成形术(percutaneous vertebroplasty,PVP)及由其衍生的球囊扩张椎体后凸成形术(percutaneous balloon kyphoplasty,PKP)是近年来治疗骨质疏松性椎体压缩骨折(osteoporotic vertebral compression fracture,OVCF)的两种微创手术方法,并已得到临床广泛应用,临床报道疗效确切,其疼痛缓解率可达70%~95%[11]。大量临床研究报道[12-13],PVP对椎体高度、后凸畸形没有恢复作用,而PKP在注入骨水泥前,通过向骨折椎体内插入一可扩张的气囊,使塌陷椎体复位,恢复椎体高度,矫正后凸畸形,恢复脊柱序列。甚至有许多报道表明[14-16],PKP术后骨折椎体高度的恢复以及后凸畸形的矫正程度是显著的。因此,对于OVCF患者来说,PKP对缓解与骨折有关的疼痛、恢复骨折椎体高度、矫正脊柱局部后凸畸形等方面有重要影响。然而,到目前为止,国内外关于探讨PKP对全脊柱矢状位序列及矢状位平衡的研究甚少。

图1 脊柱骨盆各矢状位参数测量方法示意

图2 PKP术前各参数测量示意
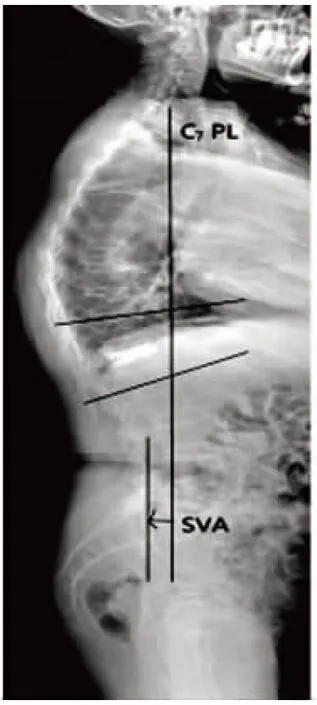
图3 PKP术后各参数测量示意
脊柱矢状位序列及矢状位平衡对维持正常的脊柱生物力学至关重要,越来越多的研究发现在研究脊柱矢状位平衡变化时必须包括骨盆的形态研究,正常的脊柱和骨盆形态曲线使得身体处于最佳平衡状态并消耗最小的能量[17]。脊柱矢状位序列的改变会很大程度上影响脊柱的力学平衡。然而脊柱矢状位不平衡成为评估脊柱畸形程度的重要因素之一。研究表明[18-19]大多脊柱疾患者者自诉的临床症状与脊柱-骨盆矢状面失衡相关。最近的文献表明[20],腰椎手术后,患者的满意度与脊柱矢状位平衡的恢复具有明显相关性。对于OVCF患者来说,脊柱矢状位序列会发生相应改变以代偿脊柱失衡。
C7铅垂线普遍被认为是人体躯干负重的轴线[21-22],可简便快速地帮助判断脊柱矢状位平衡情况。相关研究显示[23]:由C7铅垂线测量定位发现,健康的成年人往往站在负的矢状面平衡状态。躯体矢状面平衡主要包括脊柱、骨盆及下肢的矢状面排列三大组成部分,三者各自的平衡及两者之间的排列关系对维持躯体整体的矢状面平衡具有重要意义。由于下肢关节的活动度大,在正常生理情况下可随前两者的变化而变化,因此躯干矢状面的平衡主要由脊柱和骨盆的排列决定[24]。文献报道[25],骨折椎体的楔形变导致后凸畸形的发展和重心前移,导致C7铅垂线前移,从而导致“平背综合征”。而胸腰椎压缩性骨折导致的平背畸形,临床表现为患者身体向前倾斜,其本质是C7~S1矢状面轴向距离的增加及腰椎前凸角度的丢失。有文献报道[26-27],脊柱融合术后,由于腰椎前凸角度丢失,也导致平背畸形。本研究中,OVCF患者术前C7~S1的矢状面轴向距离明显长于正常对照组(P<0.05),提示正向矢状位失平衡。术前OVCF患者LL小于正常对照组,提示腰椎前凸角度的丢失,与Jang等[25]的研究结果相似。
研究发现,退行性腰椎疾病的患者腰椎前凸角的丢失伴随着胸椎后凸角的减小,因为腰椎前凸角的丢失会使躯干前倾,而胸椎后凸角的减小则能使躯干后仰,从而起到代偿作用,该代偿机制最常出现在年龄较轻,胸段脊柱活动度较大的患者,而老年患者尤其是胸腰段骨折患者由于胸腰段活动度小、活动受限制,该代偿作用受到一定限制。本研究中,术前OVCF患者TK大于正常对照组,提示胸椎后凸较大,从而使躯体重心前移,加重了脊柱矢状位的失平衡。
自从Legaye等[28]提出PI这一解剖学参数以来,其常用于描述骨盆的解剖学形态,PI不受人体姿势的影响,具有个体特异性,而PT与SS常用于描述骨盆的空间位置,随着人体姿势的变化而变化[29]。相关研究已经证实,以髋关节为轴心的骨盆后旋,可以在一定程度上代偿脊柱矢状位失衡。这种代偿机制导致骶骨倾斜角减小及骨盆倾斜角增大。本研究中,术前OVCF患者与正常对照组相比,表现出明显的骶骨倾斜角减小及骨盆倾斜角增大,而骨盆入射角值未见明显变化。因此这种骨盆后旋的代偿机制同样作用于OVCF患者。
PKP手术后,C7~S1的矢状面轴向距离较术前减小,部分改善了矢状位失平衡。而且腰椎前凸角较术前增大,胸椎后凸角较术前减小,使躯体重心前移减小,表明PKP能改善局部后凸畸形,进而促进了对矢状位平衡的改善。而骶骨倾斜角及骨盆倾斜角的变化可以看做是对矢状位失衡的一种代偿性变化,本研究中,PKP术后骶骨倾斜角及骨盆倾斜角没有明显变化,考虑与我们的随访期限短有一定关系,通过长期随访,它们也许会有所改善。
据报道[30],膝关节、上胸椎和颈椎也参与了对全脊柱矢状位不平衡的代偿。它们的代偿机制被看作是能够降低与髋、膝关节骨关节炎、颈椎病有关的日常生活能力的关键因素。本研究中,术后ODI评分较术前明显降低。因此,任何病理情况下脊柱畸形的治疗应尽可能地矫正矢状位不平衡。
本研究表明:与健康老年人相比,骨质疏松性椎体压缩骨折患者表现出明显的前矢状位不平衡。对骨质疏松椎体压缩性骨折患者来说,球囊扩张椎体后凸成形术是一种有效的微创手术方式,其不仅可缓解骨折引起的疼痛,而且能够通过改善局部后凸畸形来改善全脊柱的矢状位平衡状态。
本研究的不足:本样本随访时间较短,长时间随访也许会有不同的结果;未将骨密度数据纳入分析,骨密度的差异是否对于压缩椎体复位率的保持、末次随访矢状位力线的变化以及PKP手术并发症的发生有影响,有待进一步研究;另外,我们不能忽视术后疼痛的缓解对脊柱矢状位平衡的影响。
[1]Cotton A,Boutry N,Cortet B,etal.Perutaneous vertebroplasty:state of the art[J].Radiographics,1998,18(1):311-320.
[2]Theodorou DJ,Theodorou SJ,Duncan TD,etal.Percutaneous balloon kyphoplasty for the correction of spinal deformity in painful vertebral body compression fractures[J].Clin Imaging,2002,26(1):1-5.
[3]Coumans JV,Reinhardt M,Lieberman IH.Kyphoplasty for vertebral compression fractures:1 year clinical outcomes from a prospective study[J].J Neurosurg,2003,99(1 suppl):44-50.
[4]Lieberman IH,Dudency S,Reinhardt MK,etal.Initial outcome and efficacy of “kyphoplasty”in the treatment of painful osteoporotic vertebral compression fractures[J].Spine,2001,26(14):1631-1638.
[5]Endo K,Suzuki H,Tanaka H,etal.Sagittal spinal alignment in patients with lumbar disc herniation[J].Eur Spine J,2010,19(3):435-438.
[6]Berven SH,Deviren V,Smith JA,etal.Management of fixed sagittal plane deformity:outcome of combined anterior and posterior surgery[J].Spine,2003,28(15):1710-1715.
[7]Park SJ,Lee CS,Chung SS,etal.Postoperative changes in pelvic parameters and sagittal balance in adult isthmic spondylolisthesis[J].Neurosurgery,2011,68(2 suppl operative):355-363.
[8]Mac-Thiong JM,Labelle H,de Guise JA.Comparison of sacropelvic morphology between normal adolescents and subjects with adolescent idiopathic scoliosis[J].Stud Health Technol Inform,2006(123):195-200.
[9]Phillips FM,Ho E,Campbell HM,etal.Early radiographicand clinical results of balloon kyphoplasty for the treatmentof osteoporotic vertebral compression fractures[J].Spine,2003,28(19):2260-2265.
[10]Campbell PG,Harrop JS.Incidence of fracture in adjacent levels in patients treated with balloon kyphoplasty:a review of the literature[J].Curr Rev Musculoskelet Med,2008,1(1):61-64.
[11]Muto M,Muto E,Izzo R,etal.Vertebroplasty in the treatment of back pain[J].Radiol Med(Torino),2005,109(3):208-219.
[12]Truumees E,Hilibrand A,Vaeearo AR.Percutaneous vertebral augmentation[J].Spine Journal,2004,4(3):218-229.
[13]Wang G,Yang H,Chen K.Osteoporotic vertebral compression fractures with an intravertebral cleft treated by percutaneous balloon kyphoplasty[J].J Bone Joint Surg(Br),2010,92(11):1553-1557.
[14]Kim KH,Kuh SU,Chin DK,etal.Kyphoplasty versus vertebroplasty:restoration of vertebral body height and correction of kyphotic deformity with special attention to the shape of the fractured vertebrae[J].J Spinal Disord Tech,2015,25(6):338-344.
[15]Liu JT,Liao WJ,Tan WC,etal.Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture:a prospective,comparative,and randomized clinical study[J].Osteoporos Int,2010,21(2):359-364.
[16]Bozkurt M,Kahilogullari G,Ozdemir M,etal.Comparative analysis of vertebroplasty and kyphoplasty for osteoporotic vertebral compression fractures[J].Asian Spine J,2014,8(1):27-34.
[17]Blondel B,Jouve JL,Panuel M,etal.Pelvic incidence reliability in spine sagittal balance[J].Rev Chir Orthop Reparatrice Appar Mot,2008,94(4):321-326.
[18]Mangione P,Gomez D,Senegas J.Study of the course of theincidence angle during growth[J].Eur Spine J,1997,6(3):163-167.
[19]Labelle H,Roussouly P,Berthonnaud E,etal.Spondylolisthesis,pelvic incidence,and spinopelvic balance:a correlation study[J].Spine(Phila Pa 1976),2004,29(18):2049-2054.
[20]Berven SH,Deviren V,Smith JA,etal.Management of fixed sagittal plane deformity:outcome of combined anterior and posterior surgery[J].Spine,2013,28(15):1710-1715.
[21]Gelb DE,Lenke LG,Bridwell KH,etal.An analysis of sagittal spinal alignment in 100 asymptomatic middle and older aged volunteers[J].Spine,1995,20(12):1351-1358.
[22]Jackson RP,Mcmanus AC.Radiographic analysis of sagittalplane alignment and balance in standing volunteers and patients with low back pain matched for age,sex,and size:a prospective controlled clinical study[J].Spine,1994,19(14):1611-1618.
[23]Zhu Z,Xu L,Zhu F,etal.Sagittal alignment of spine and pelvis in asymptomatic adults:norms in Chinese populations[J].Spine,2013,39(1):E1-E6.
[24]Le H,Leijssen P,Duarte M,etal.Thoracolumbar imbalance analysis for osteotomy planification using a new method:FBI technique[J].Eur Spine J,2011,20(Suppl 5):669-680.
[25]Jang JS,Lee SH,Min JH,etal.Changes in sagittal alignment after restoration of lower lumbar lordosis in patients with degenerative flat back syndrome[J].J Neurosurg Spine,2007,7(4):387-392.
[26]Potter BK,Ienke LG,Kuklo TR,etal.Prevention and management of iatrogenic flatback deformity[J].J Bone Joint Surg(Am),2004,86(8):1793-1808.
[27]Sarwahi V,Boachie Adjei O,Backus SI,etal.Characterization of gait function in patients with postsurgical saginal( flathack) deformity:a prospective study of 21 patients[J].Spine,2002,27(21):2328-2337.
[28]Legaye J,Duval-Beaupère G,Hecquet J,etal.Pelvic incidence:a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves[J].Eur Spine J,1998,7(2):99-103.
[29]Schwab F,Lafage V,Boyce R,etal.Gravity line analysis inadult volunteers:age-related correlation with spinal parameters,pelvic parameters,and foot position[J].Spine,2006,31(25):959-967.
[30]Barrey C,Roussouly P,Le Huec JC,etal.Compensatory mechanisms contributing to keep the sagittal balance of the spine[J].Eur Spine J,2013,22(Suppl 6):834-841.
Effect of PKP on Sagittal Balance of the Whole Spine in Patients with Single Segment OVCF
Zhang Jingtao1,2,Geng Wei2,Xu Hui2,etal
(1.Taishan Medical University,Taian 271000,China;2.The Spinal Surgery of Liaocheng People′s Hospital,Liaocheng252000,China)
ObjectiveTo investigate the effect of PKP on sagittal balance of the whole spine in patients with single segment OVCF.MethodsA retrospective analysis of experimental group of 65 cases of patients with single-level osteoporotic vertebral compression fracture(OVCF) in the period from February 2014 to October 2015.All patients have undergone percutaneous balloon kyphoplasty(PKP).The natural standing position of the whole spine(including bilateral femoral head) positive lateral position X-ray films were taken at pre-and post-operation to measure the pelvic incidence(PI),pelvic tilt(PT),sacral slope(SS),lumbar lordosis(LL),thoracic kyphosis(TK),local sagittal Cobb angle,and C7~S1SVA;the visual analogue scale(VAS) and Oswestry disability index(ODI) were recorded.The relationship between preoperative spine-pelvis sagittal parameters and those of normal control group were assessed.And the changes of the sagittal parameters and the occurrence of complications after operation in the study group were analyzed.ResultsAll patients were followed up.At the last follow-up,the VAS score and ODI score of the study group were significantly improved compared with the preoperative(P<0.05).The preoperative C7~S1SVA values of the study group were larger than those in the normal control group,of which the difference was statistically significant(P<0.05);preoperative TK values of the study group were larger than those of normal control group,the difference was statistically significant(P<0.05).In pelvis-related parameters,the differences of PI values of the study group between those of normal control group showed no significant whilst the corresponding PT,SS changes were both statistically significant(P<0.05) .Post-operative C7~S1SVA was reduced compared with the pre-operative ones,of which the difference was statistically significant(P<0.05);In spine-related parameters,there were an increase in post-operative LL value preoperative than the postoperative ones and a decrease in post-operative TK values compared with the preoperative ones,of which the differences were statistically significant(P< 0.05);In pelvis related parameters,there was no statistical significance in the pre-and post-operative differences of PI,PT,SS values(P>0.05) whilst the post-operative local Cobb angle was significantly reduced compared to the pre-operative onces,of which the difference was statistically significant(P<0.05).There was no obvious correlation between local Cobb angle and C7~S1SVA.However,the change of the local Cobb angle was significantly related to the change of C7~S1in the sagittal plane(SVA C7~S1).No serious complications were found during the operation and postoperative follow-up.ConclusionFor patients with osteoporotic vertebral compression fractures,a percutaneous balloon kyphoplasty(PKP) is a considerable and effective minimally-invasive surgical approach,which can not only relieving fracture-caused pain,but also improve agittal alance through alleviation of local kyphosis.
vertebral compression fractures;osteoporosis;percutaneous balloon kyphoplasty;sagittal balance
1008-5572(2016)09-0777-06
R683.2
B
2016-04-08
张景涛(1990- ),男,研究生在读,泰山医学院,聊城市人民医院脊柱外科,252000。
*本文并列第一作者:耿伟;本文通讯作者:马金柱