微血管形成在腰椎间盘退变过程中的表现特征及影响因素
魏海峰,钱 军,鲍丙波,付 凯,郑宪友
(1.上海交通大学附属第六人民医院,上海 200233;2.上海市松江区泗泾医院,上海 200233)
微血管形成在腰椎间盘退变过程中的表现特征及影响因素
魏海峰1,钱军2,鲍丙波1,付凯1,郑宪友1
(1.上海交通大学附属第六人民医院,上海200233;2.上海市松江区泗泾医院,上海200233)
目的观察微血管形成在腰椎间盘退变过程中的病理表现特征,并分析其相关影响因素.方法选取48例行单节段腰椎后路经椎间孔减压椎间植骨融合内固定术患者,术中切取患处组织,冷冻切片后HE染色,观察病理改变,Weidner微血管计数法统计微血管密度.根据是否有微血管分为有微血管组、无微血管组,比较微血管形成的可能影响因素,对差异具有统计学意义的因素进一步行Logistics回归分析.结果25例患者椎间盘内存在明显微血管形成,组织切片中存在典型的条形管腔结构,血管内皮细胞核有明显蓝染,微血管形成率为52.08%,MVD值平均为11.9±2.5.有微血管组椎间盘钙化率明显高于无微血管组,差异具有显著统计学意义(P<0.01);有微血管组JOA评分明显低于无微血管组,腰椎疼痛VAS评分明显高于无微血管组,差异具有统计学意义(P<0.05);椎间盘退变程度、椎间盘疝出程度两组间比较差异无统计学意义(P>0.05).多因素回归分析显示:椎间盘钙化、腰椎疼痛VAS评分与退变椎间盘内微血管形成有明显相关性(OR值分别8.992,7.359,P值均<0.05).结论椎间盘退变伴随着微血管形成,椎间盘钙化、腰椎疼痛VAS评分与退变腰椎间盘微血管形成有关.
腰椎间盘;退变;微血管形成
【引用格式】魏海峰,钱军,鲍丙波,等.微血管形成在腰椎间盘退变过程中的表现特征及影响因素[J].北华大学学报(自然科学版),2016,17(5):632-635.
新生儿阶段椎间盘组织中存在丰富血管,之后微血管逐渐退化到椎间盘终板和纤维环外层,到成年阶段椎间盘成为体内最大的无血管组织,依赖软骨终板和纤维环的渗透作用提供营养[1].在椎间盘退变过程中又有微血管形成,成为一种特征性病理改变[2].目前该领域对退变椎间盘组织中微血管形成的研究还十分少见,如何平衡椎间盘内微血管形成的利弊,促进其发挥积极作用是亟待解决的问题.本次研究分析48例因腰椎间盘退变行手术治疗的患者,观察椎间盘组织病理学改变,分析可能与退变椎间盘内微血管形成有关的因素,旨在为椎间盘退变性疾病治疗提供参考.
1 资料与方法
1.1一般资料
选取2014年1月—2015年12月在上海交通大学附属第六人民医院行单节段腰椎后路经椎间孔减压椎间植骨融合内固定术的患者48例.其中,男性26例,女性22例,年龄26~75岁,平均(52.91±10.38)岁;腰椎间盘突出症29例,滑脱症10例,椎管内狭窄症9例.筛选标准:有完整的术前CT、X线等影像学资料;无严重骨质疏松和退变性腰椎侧凸;无腰椎间盘穿刺术、射频消融等腰椎手术史.患者均自愿参与本次研究并签署知情同意书.
1.2病理学观察
术中分别切取疼痛责任节段椎间盘纤维环、髓核、椎体软骨终板组织标本.-20 ℃快速冻存,8 μm冰冻切片,常规行HE染色.光学显微镜下观察内皮细胞形态,判断微血管.根据椎间盘内是否存有微血管分为有微血管组、无微血管组;Weidner微血管计数法统计微血管密度(MVD).
1.3微血管形成的相关因素评价标准
1)椎间盘退变程度:参考改良Pfirrmann分级标准,根据术前患者责任节段椎间盘MRI矢状面信号改变,将椎间盘退变程度分为Ⅰ~Ⅴ级.2)椎间盘钙化:依据患者术前腰椎CT和矢状面三维影像重建评价椎间盘是否存在钙化.分析CT骨窗位图像:病灶椎间盘节段存在骨性高信号改变为椎间盘脱出伴钙化,未见明显改变为无钙化.3)椎间盘疝出程度:根据术前MRI矢状面T2加权像对疝出程度进行分级,分为膨出型、突出型、脱出型、游离型.膨出型:外周纤维环对称性超出椎体终板边缘正常限度,CT横断面显示超出椎体周边1.6~2.3 mm;突出型:疝出部分的最大高度均小于相同层面基底部宽度;脱出型:多个层面上疝出部分的高度大于相同层面基底部宽度;游离型:疝出部分与椎间隙内部不相连,在椎管内游离分布.4)术前神经功能与疼痛程度:使用JOA腰椎功能评分表评估术前神经功能情况,总分29分;使用VAS疼痛量表评估术前腰椎疼痛程度,0~10分,0分为无痛,10分为剧痛.
1.4统计学分析

2 结 果
2.1退变椎间盘内微血管形成
退变椎间盘组织标本HE染色显示:具有典型的条形管腔结构,血管内皮细胞核有明显蓝染.见图1.本次研究的48例患者中有25例椎间盘内存在明显微血管形成,微血管形成率为52.08%,MVD值平均为11.9±2.5.其中微血管主要分布于纤维环11例,软骨终板6例,纤维环和髓核组织8例.
2.2退变椎间盘内微血管形成的单因素分析
有微血管组椎间盘钙化率明显高于无微血管组,差异具有显著统计学意义(P<0.01);有微血管组JOA评分明显低于无微血管组,腰椎疼痛VAS评分明显高于无微血管组,差异具有统计学意义(P<0.05);两组间椎间盘退变程度、椎间盘疝出程度差异均无统计学意义(P>0.05).见表1.
2.3退变椎间盘内微血管形成的多因素分析
自变量为单因素分析中差异具有统计学意义的椎间盘钙化、JOA评分、VAS评分三个相关因素,因变量为微血管形成,进行多因素Logistics回归分析,赋值方法见表2.结果显示:椎间盘钙化、腰椎疼痛VAS评分与退变椎间盘内微血管形成有明显相关性(P<0.05);JOA评分与退变椎间盘内微血管形成无明显相关性(P>0.05).见表3.

表1 两组间影响退变椎间盘内微血管形成的因素比较
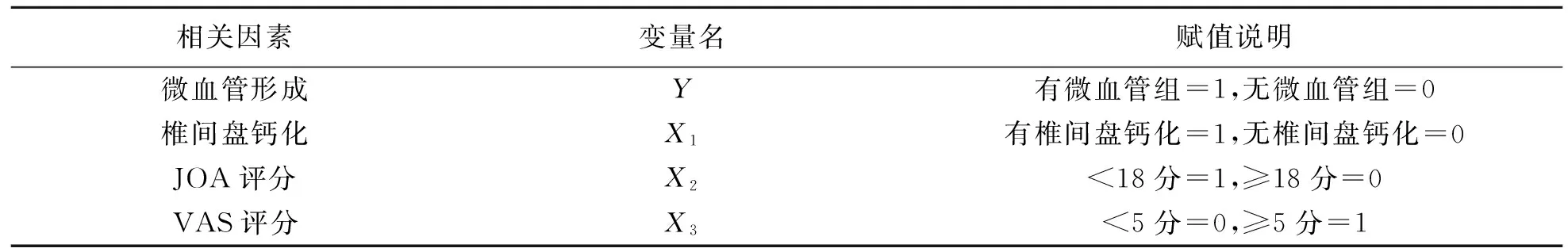
表2 微血管形成相关因素赋值说明

表3 微血管形成相关因素Logistics回归分析
3 讨 论
椎间盘是人体最先退变的组织,从20岁起就开始进入退变过程.目前关于腰椎间盘退变机制的研究较为全面,年龄、基因、炎症、机体组织结构等众多因素均可参与退变过程[3].在退变过程中一种显现已被观察到,即伴随腰椎间盘退变过程的微血管形成,但目前却仍缺乏相关系统研究.本次研究显示:52.08%的退变腰椎间盘标本中存在微血管形成,主要分布于纤维环、软骨终板、髓核组织,其中以纤维环组织中微血管形成最明显.腰椎间盘内微血管形成多出现在病情早期或急性发作阶段,提示微血管形成并非腰椎间盘自然老化退变过程出现的现象,其是否在腰椎间盘致病过程中发挥始动作用仍需深入研究.
椎间盘退变伴随着组织钙化,两者所处的病程和机制不同[4].本次研究显示:腰椎间盘钙化与退变过程中微血管形成具有明显相关性,说明二者关系对腰椎间盘退变进程具有重要影响,腰椎间盘纤维环、软骨终板、髓核组织的钙化会进一步阻碍椎间盘营养和代谢,加剧椎间盘内的缺氧环境,改变椎间盘胶原成分,同时上调生物蛋白酶、巨噬细胞浸润、细胞因子表达水平.细胞外基质环境的改变可诱导微血管形成,例如MMPs可降解细胞外基质诱导内皮细胞出芽和移行,TNF-α可诱导VEGF上调,VEGF可使血管内皮细胞排成管腔样结构[5].椎间盘退变性疾病是引发腰腿疼的一个主要原因,而退变椎间盘内神经末梢和微血管的植入与疼痛症状存在关联[6].本次研究显示:患者术前腰椎间盘疼痛VAS评分和退变椎间盘内微血管形成存在明显相关性,提示退变椎间盘中微血管形成可加重患者临床症状.
成年人椎间盘无血管组织,随着椎间盘退变和纤维环破坏而逐渐形成微血管并伴神经末梢植入,进而改变椎间盘组织内环境,炎性细胞、神经递质等聚集会加速椎间盘的退变进程.可见椎间盘内微血管形成在促进突出髓核吸收外,也加重了患者临床症状.微血管形成在椎间盘组织中作用各有利弊,如何通过合理干预措施平衡其利弊,促进其发挥积极作用仍需要进一步研究.
[1] Francisco Garcia Vacas,Francisco Ezquerro Juanco,Ana Perez de la Blanca,etal.The flexion-extension response of a novel lumbar intervertebral disc prosthesis:A finite element study[J].Mechanism and Machine Theory:Dynamics of Machine Systems Gears and Power Tran- dmissions Robots and Manipulator Systems Computer-Aided Design Methods,2014,73:273-281.
[2] Stelzeneder D,Welsch G H,Kovács B K,etal.Qua- ntitative T2 evaluation at 3.0 T compared to morphologi- cal grading of the lumbar intervertebral disc:A standardi- zed evaluation approach in patients with low back pain[J].European Journal of Radiology,2012,81(2):324-330.[3] Ghislain Maquer,Marc Laurent,Vaclav Brandejsky,etal.Finite element based nonlinear normalization of human lumbar intervertebral disc stiffness to account for Its morphology[J].Journal of Biomechanical Engineering,2014,136(6):1-11.
[4] Eric Wagnac,Pierre-Jean Arnoux,Anais Garo,etal.Calibration of hyperelastic material properties of the hu- man lumbar intervertebral disc under fast dynamic comp- ressive loads[J].Journal of Biomechanical Enginee- ring,2011,133(10):101-107.
[5] Park W M,Kim K,Kim Y H,etal.Effects of degenerated intervertebral discs on intersegmental rotations,intr- adiscal pressures,and facet joint forces of the whole lum- bar spine[J].Computers in Biology and Medicine,2013,43(9):1234-1240.
[6] Xu B S,Xia Q,Ma X L,etal.The usefulness of magnetic resonance imaging for sequestered lumbar disc herniation treated with endoscopic surgery[J].Journal of X-ray Sci- ence and Technology,2012,20(3):373-381.
【责任编辑:陈丽华】
Characteristics and Influencing Factors of Micro Vessel Formation in the Process of Lumbar Intervertebral Disc Degeneration
Wei Haifeng1,Qian Jun2,Bao Bingbo1,Fu Kai1,Zheng Xianyou1
(1.No.6 Affiliated Hospital,Shanghai Jiao Tong University,Shanghai 200233,China;2.SijingHospitalofSongjiangDistrict,Shanghai200233,China)
Objective To observe the pathological characteristics of the formation of micro vessels in the process of lumbar disc degeneration and analyze the related influencing factors.Method 48 patients with single segment lumbar interbody fusion and internal fixation were performed.During the operation,the affected tissue was removed and prepared into frozen sections,and dyed with hematoxylin and eosin (HE) staining for the observation of pathological changes;Weidner micro vascular count was used for the observation of microvessel density.According to whether there was microvessel or not,the samples were divided into microvascular group and nonmicrovascular group,for the observation of the possible factors that might affect the formation of micro vessels and the further line Logistics regression analysis of the factors with statistically significant difference.Results An obvious formation of microvessels was found in 25 patients,in which the typical strip lumen structure could be seen in the tissue sections,the vascular endothelial cell nucleus was obviously blue-stained,and the microvessel formation rate was 52.08%,with an average MVD value of 11.9±2.5.The intervertebral disc calcification rate in the microvascular group was significantly higher than that in the non-microvascular group (P<0.01);The JOA score in the microvascular group was significantly lower than that non-microvascular group and the lumbar pain VAS score in the microvascular group was significantly higher than that the non-microvascular group (P<0.05);there was no significant difference in intervertebral disc degeneration and disc herniation between the two groups (P>0.05).The multivariate regression analysis revealed that the intervertebral disc calcification and lumbar pain VAS score were significantly correlated with the microvessel formation in the degenerated intervertebral disc (OR values were 8.992 and 7.359,respectively,P<0.05).Conclusion The disc degeneration accompanies the microvessel formation,and the disc calcification and lumbar pain VAS score are associated with the development of microvessels in the degenerative lumbar disc.
lumbar intervertebral disc;degeneration;microvascular formation
1009-4822(2016)05-0632-04
10.11713/j.issn.1009-4822.2016.05.016
2016-03-25
上海市科学技术委员会西医类引导项目(14412961103).
魏海峰(1977-),男,博士,主治医师,主要从事骨科创伤与修复研究,E-mail:admini@126.com.
R681.5
A

