Effectsof acupuncture treatment for irritablebowel syndrome:a systematic review and meta-analysis
Ji-Ye Liu,Ying-Hua Chen
1Clinical Medical School,Heilongjiang University of Chinese Medicine,Harbin,China.2Department of Acupuncture&Moxibustion,First Affiliated Hospital of Heilongjiang University of Chinese Medicine,Harbin,China.
1.Introduction
Irritablebowelsyndrome(IBS)isthe most commonfunctionalgastrointestinal disorder[1],which is majorly characterized by abdominal pain,bloating,and disturbed defecation and is coupled with psychological conditions[2].Some studies indicated that IBS has a prevalence of 1%to 20%worldwide,although up to 75%affected individuals never seek care[3-6].IBS has an intensely negative effect on patients’quality of life,and impose a substantial economic burden on patients and thewhole society[7].The combined direct and indirect costs associated with IBS patients in the United States in 2004 were estimated at over$1 billion[8].
Pharmacologic,psychologic,and complementary approaches are considered as therapeutic options in IBS patients[9].Pharmacologic and psychologic therapy as a conventional treatment includes antidiarrheals,antispasmodics,prokinetics,osmotics,bulking agents and tranquilizers[10-12].But there is a limitation to conventional therapy as no drug is effective against all IBS symptoms[13].Besides,due to lack of favorable efficacy and associated adverse eventswith conventional treatments,some IBSpatients look for alternative treatments such as herbal medications and Chinese acupuncture[14].Among a variety of alternative treatments,acupuncture is the most popular and acceptable in the world.It has been used to treat several gastrointestinal symptoms in treat several gastrointestinal symptoms in functional and organic diseases,and has been shown to influence visceral reflex activity,gastric emptying, and acid secretion[15].Besides,it has been shown that acupuncture is green,safe,simple and minimally aggressive with few side effects.In the past 30 years,many studies reported the use of acupuncture for the treatment of IBS.However results of these researches didn’t have enough evidences to conform the effectiveness of acupuncture for IBS.Therefore,it is difficult for doctors to make decisions to regard acupuncture as a conventional treatment and includeit in IBSpatient’streatment plan.
There are six reviews about the acupuncture treatment for IBS[16-21].However,these articles included three systematic reviews[17,19,21]and three literature reviews[16,18,20].The review by Z.Hussain,et al just included one randomized clinical trial(RCT)about acupuncture treatment for IBS[17].The review by Schneider,et al included seven studies,but among them five articles were not RCTs[19].A recent review published in 2012 [21]included seventeen RCTs,but nine RCTs were about acupuncturewith moxibustion.
Therefore,it is necessary to perform a systematic review again about acupuncture for IBS to renewal current knowledge and assess available experimental evidencesin order to lead futurestudies.
2.Method and Analysis
2.1 Search Strategy.
The following 7 databaseswere electronically searched from their inception to May 2015:PubMed,EMBASE,the Cochrane Central Register of Controlled Trials(CENTRAL), China National Knowledge Infrastructure (CNKI),Chinese Scientific Journal Database(VIP database),Wanfang Database,and Chinese Biomedical Literature Database(Sinomed).For the last four Chinese databases,we only included the studies published on core journals,such as Chinese Acupuncture and Moxibustion,Shanghai Journal of Acupuncture and Moxibustion. No language restrictions were applied.The following search terms were used as subject terms and free terms:irritable bowel syndrome,irritablecolon,intestinal dysfunction,functional colonic disease, acupuncture,electroacupuncture, manual acupuncture, warm acupuncture, and needle acupuncture. EndNote software was applied to manage citations obtained through the databases search.The search strategies in detail arepresented in the Appendix.
2.2 Inclusion Criteria
2.2.1 Typeof Studies.
All randomized controlled trials(RCTs)involving acupuncturefor treating IBSwereincluded.
2.2.2 Typeof Participants.
Participants with IBSwere included regardless of sex,race,ageor educational and economic status.
2.2.3 Typesof Interventions.
Interventions in the acupuncture group included acupuncture,electroacupuncture,warm acupuncture,needle acupuncture, manual acupuncture or acupuncture as an adjuvant for other standard therapies for IBS. Controlled interventions with sham acupuncture,placebo,no specific treatment,or other active non-TCM treatment(e.g.pharmacological therapies)were included.Adjunctive treatments,either Modern Medicine or TCM,were permitted as long as they had been given to both the acupuncture and control groups. RCTs appraising acupuncture combined with another treatment compared with that other treatment alonewasalso included.
2.2.4 Outcomesof interest.
The primary outcome was the evaluation of symptom,such as the IBS Symptom Severity Scale(IBS-SSS).The secondary outcome was quality of life,such as the IBSQuality of Lifemeasure(IBS-QoL).
2.3 Exclusion Criteria
2.3.1 Other Typesof Researches
Nonrandomized controlled trials,quasi-randomized controlled trials,unequal randomized controlled trials,cluster randomized controlled trials,randomized crossover trials, animal studies, case reports,descriptivesurveysand review studieswereexcluded.
2.3.2 Other Participants.
Participantswith severe physical or mental illnesswere excluded.
2.3.3 Other Typesof Interventions.
We did not include trials in which points were irritated without needle insertion(such as laser irradiation,acupressure,or transcutaneous electrical stimulation).We didn’t also include trials of dry needling/trigger point therapy,a therapy which isbased on principles of Western anatomy and physiology and rejects TCM concepts of energy and meridians[21].And trials of microacupuncture which is based on the principle that ear(or head,finger,etc)is a microsystem of the whole body were excluded.Besides,RCTs that can’t evaluate the treatment effectiveness of acupuncture (e.g.comparing different forms of acupuncture or comparing one form of acupuncture with a different type of TCM(e.g.herbal medicine)were excluded.We also excluded individual therapeutic plans because of statistical comparison between groups.
2.4 Study Selection and Data Extraction.
Two researchers(Jiye Liu and Yinghua Chen)independently assessed the studies according to the inclusion criteria and extracted the data.We resolved any disagreementsby discussion and consensusby a third reviewer(Zhongren Sun).The risk of bias was assessed using the Cochrane risk of bias assessment tool.
2.5 Data Synthesis.
Review Manager Software(V5.3)was used to perform the meta-analysis.Dichotomous and continuous data were presented as relative risk(RR)and mean difference(MD),respectively,with 95%confidence interval(CI).Heterogeneity among the included studies was assessed using Chi-square and I2statistic.When I2≤50%with a P>0.1,it was considered heterogeneous;in contrast,if P,I2>50%with a P≤0.1,it wasconsidered homogeneous.I2valueslessthan 50%were accepted as homogeneous.If substantial heterogeneity was perceived,we explored the reason for heterogeneity.
2.6 Quality of Evidence
We used the Grading of Recommenations Assessment,Development and Evaluation(GRADE)to grade the quality of evidence,and the results were summarized using GRADEpro 3.6.1 software.
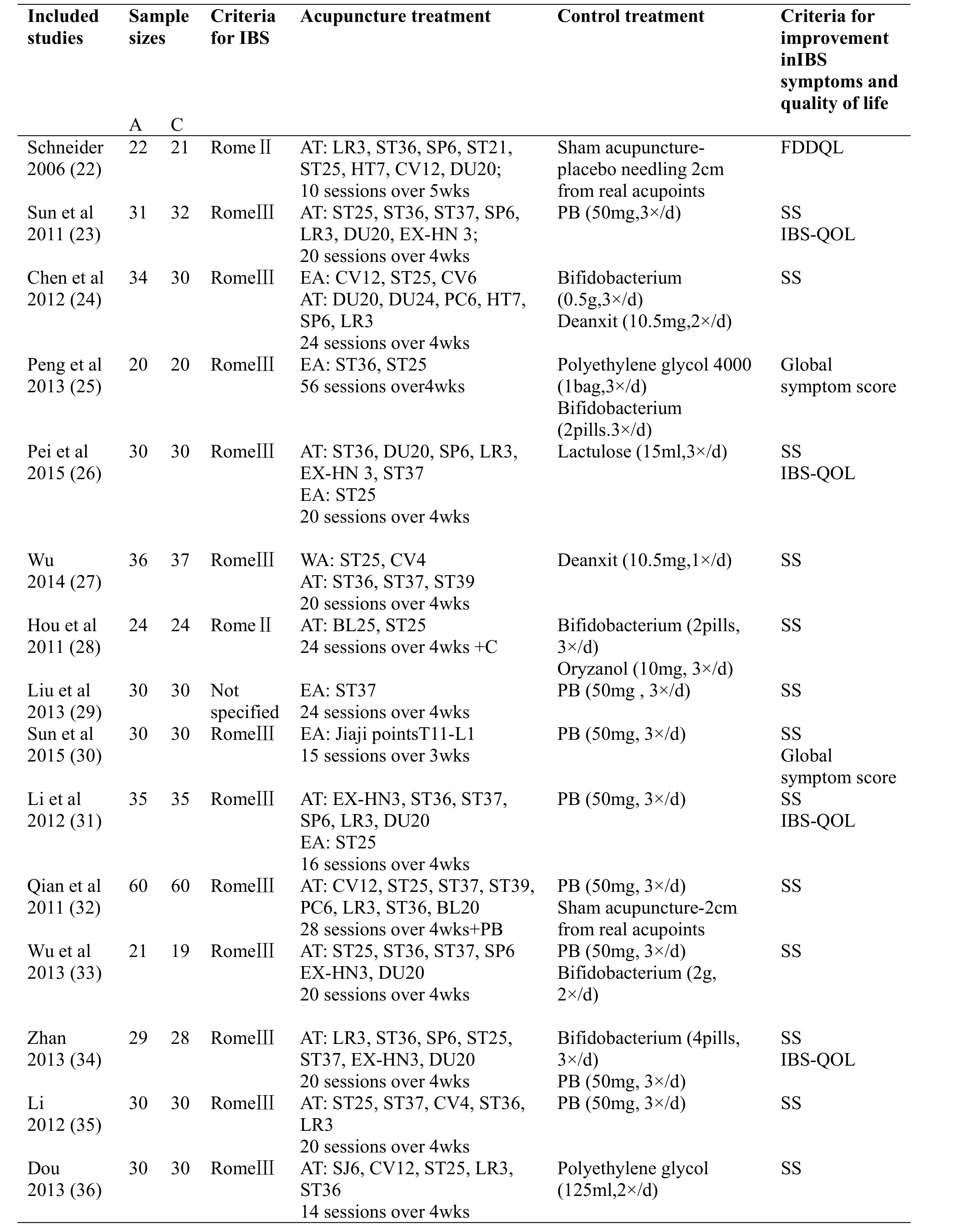
Table1 Characteristicsof theincluded studies.

A:acupuncture or electroa-cupuncture.C:control treatment.AT:acupuncture.EA:electroa-cupuncture.PB:pinaverium bromide.FDDQL:Functional Digesitive Diseases Quality of Life Questionnaire.IBS-QOL:IBS Quality of Life Measure.IBS-SSS:IBSSeverity Scoring System.wks:weeks.SS:symptom severity.Most trials conducted in China,s symptom scale was used to assess the severity of the patients’overall IBS-related symptom both at baseline and after treatment.A percentage improvement from baseline scores was calculated,and the change was grouped into 4 categories,which were converted into 2 categories for the meta-analysis.
3.Results
A total of 1088 articles were screened,and 656 were stepped into the next process after duplicated.Another 441 articles were removed after checked the title and abstract.198 articles were excluded based on full-text because of following reasons: mixed other interventions,compared different formsof acupuncture,or were non-RCTs.Total 17 studies involving 1032 patients were included eventually in our meta-analysis,of which 16 trials were published in Chinese and one was published in English.Flow diagram of the article selection processwassummarized in Figure 1.
3.1 Study Description(Table1)
3.1.1 Participants
17 studies were included in the final qualitative analysis.One was published in English and all others were published in Chinese.The largest sample size was 120 cases in a study by Qian et al[32].While the smallest sample size was 40 cases in a study by Wu et al[33].Two trials compared acupuncture with sham acupuncture [22,32].Fourteen trials compared acupuncture with drug[23-27,29-31,33-38].One trial compared acupunctureplusdrug with drug alone[28].
3.1.2Acupuncture Interventions
The acupuncture style,selected acupoints,number of sessions,and duration of acupuncture treatment all diversified among these trials.The majority of the trials used manual acupuncture.Three studies used electroacupuncture[25,29,30].Three studies used manual acupuncture with electroacupuncture[24,26,31],and one study used manual acupuncture with warm acupuncture[27].For acupoint selection,all the trials used a predesigned set of acupoints.The needle feeling,a DeQi sensation came to realize as soreness,numbness that is usually generated by acupuncture needles for the intended treatment effect,was reported in all studies.
3.1.3 Controls
In one study,acupuncture was compared with sham acupuncture[22],and in one other study,acupuncture combined with conventional drug was compared with sham acupuncture combined with conventional drug[32].In fifteen studies,acupuncture was compared with drug[23-27,29-31,33-38].In one study,acupuncture combined with drug was compared with drug alone[28].
源于“长富2号”外观品质优良变异。2011年通过贵州省品种审定委员会审定。黔选3号果型高桩端正,偏果率低(11.2%),果实圆形或近圆形,果形指数0.87,单果重180~220克。底色黄绿,着色早,条纹红,果面光滑,蜡质多,果梗较长,果皮较薄,果肉黄白色,肉质松脆,去皮硬度9.43公斤/平方厘米,汁液多,可溶性固形物含量14.93%。
3.1.4 Outcomes
Fourteen studies used a symptom scale which assessed the severity of the patients’overall IBS-related symptoms(e.g.,abdominal pain,diarrhea,constipation)as the primary outcomes to evaluate the effectiveness of acupuncture treatment for IBS[23,24,26-37].But one study used IBS-SSSas the primary outcome[38].For the secondary outcomes,four studies used the IBS Quality of Life measure(IBS-QoL)[23,26,31,34].However,the one other study used global symptom score[25].
3.1.5 Risk of Bias
All included RCTs were associated with a high risk of bias.Seven RCTs of the seventeen studies used random-number table to generate subject ID[23,24,30-34],one trial used block randomization[22],two RCTs used computerized randomization[37,38],one RCT used false randomization[27],and the remained RCTs didn’t describe the randomization method in detail.One RCT used sealed envelope to perform allocation concealment[32]and other one carried out it using telephone method[22],but the remained studies didn’t provide enough information about the allocation concealment.Besides,one RCT [22]described blinding of both participants and outment evaluation.Furthermore,five RCTs reported dropout[23,33-35,38].Risk of other bias domains may exist in these analyzed trials.However,there was no sufficient information to assess the possibility for the existence of other biases.This result of risk of bias was depicted in Figure2.

Figure2 Summary of risk of bias.
3.1.6 Quality of Evidence
The GRADE was used to perform a systematic review of the results.The quality of evidence was from very low to moderate.All of the studies reported the randomization method,but all of the RCTs did not describe the method of allocation concealment except for one study[22].Besides,the small number of subjects of all outcomes also made the quality downgrade(Table 2).
4.Meta-Analysis
4.1 Symptom Severity
One RCT compared the effects of acupuncture plus drug with sham acupuncture plusdrug[32].The results showed that acupuncture plus drug was superior to sham acupuncture plus drug in terms of symptom severity(n=120,RR=1.29,CI=1.11-1.50,P=0.001)(see Figure 3).Only one trial compared acupuncture plus drug with drug alone[28].Our results showed no statistically significant difference between acupuncture plus drug and drug alone (n=48, RR=1.28,CI=1.00-1.63,P=0.05)(see Figure 4).Twelve RCTs compared the effects of acupuncture with conventional drug therapies[23,24,26-27,29-36].Meta-analysis showed significant heterogeneity(P=0.04,I2=46%).A random-effect model was used for statistical analysis(see Figure 5).The results showed that acupuncture was superior to drug therapy on symptom severity(n=705,RR=1.20,CI=1.09-1.32,P=0.0002).
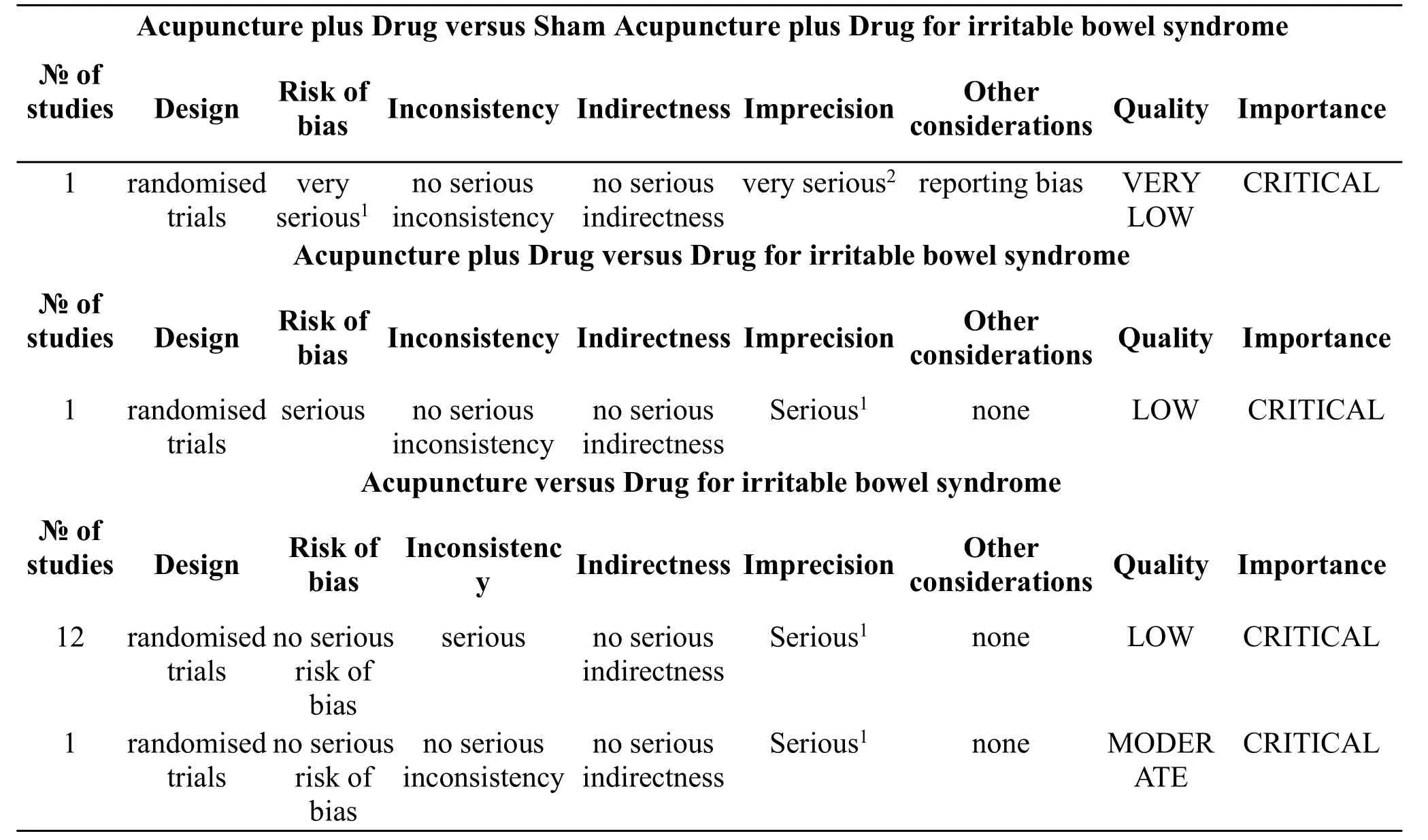
Table2 Summary of quality assessments
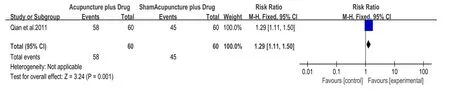
Figure3 Acupunctureplus Drug vssham acupuncture plus Drug on Symptom severity.
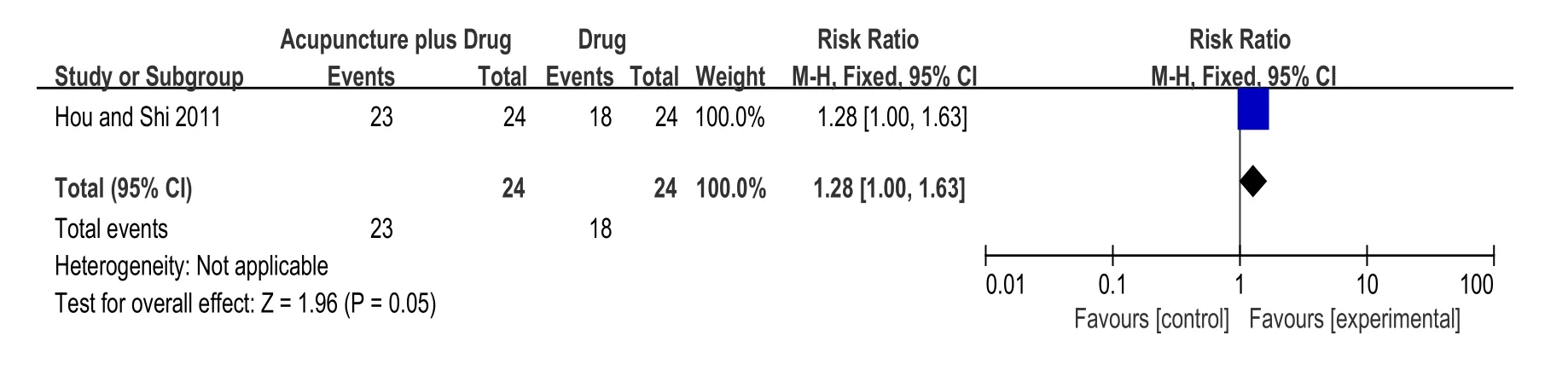
Figure4Acupunctureplus Drug vs Drug on Symptom severity.
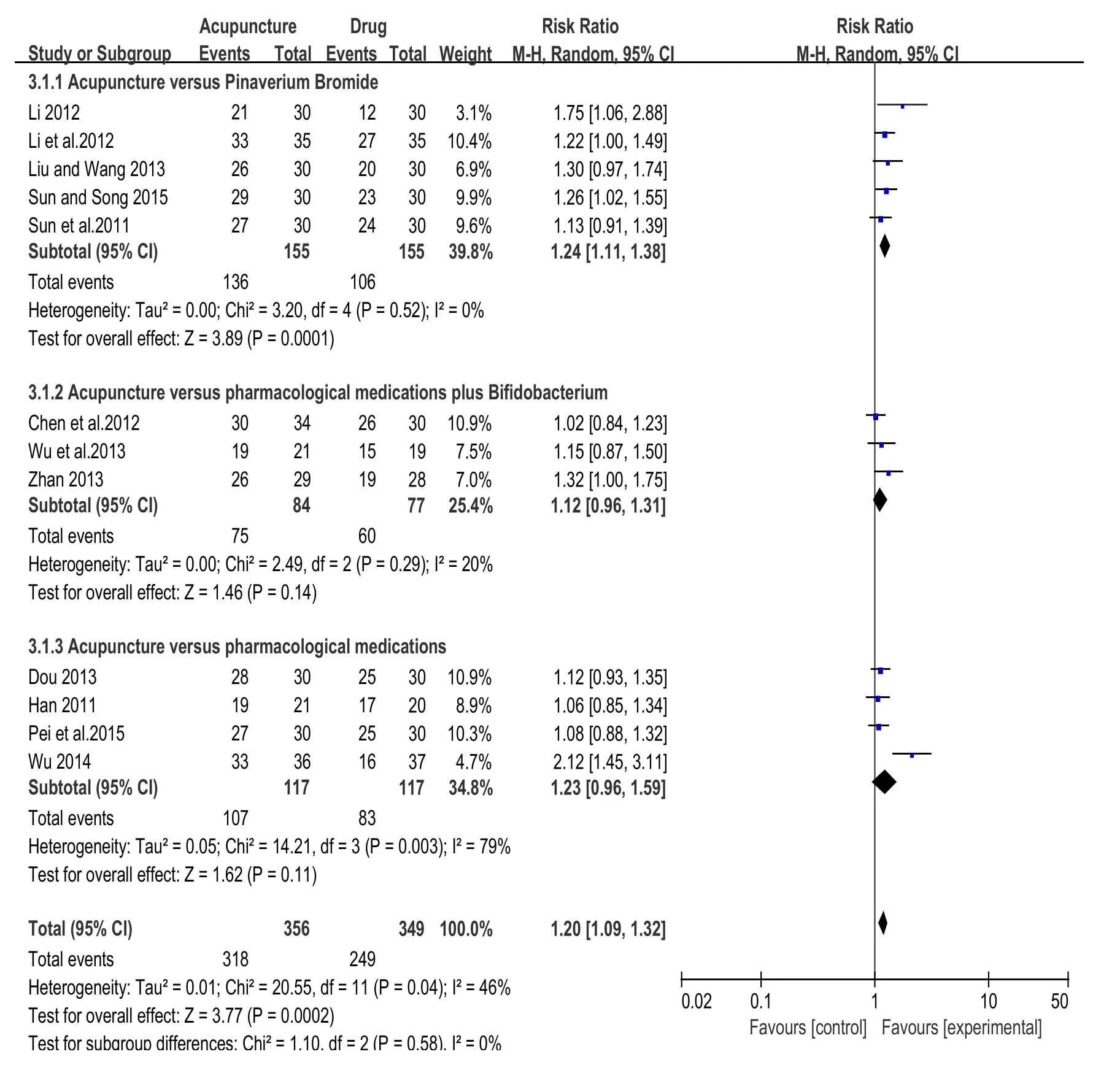
Figure5 Acupuncturevs Drug on Symptom severity.
4.2 IBS-SSS
Only one RCT(38)compared acupuncture with drug on IBS-SSS(see Figure 6).Our results failed to show statistically significant difference between acupuncture and drug(n=73,SMD=-0.45,CI=-0.91-0.02).
4.3 Global Symptom Score.
Two RCTs[25,30]compared acupuncturewith drug on global symptom score. Meta-analysis showed significant heterogeneity (P=0.004, I2=88%). A random-effect model was used for statistical analysis(Figure 7).The results didn’t show statistically significant difference between acupuncture and drug(n=100, SMD=-2.41, CI=-4.07-0.75). The heterogeneity(I2=88%)was not acceptable,because symptom score of one trial[25]was made by author himself.After it was removed,the results showed statistically significant(P<0.00001).
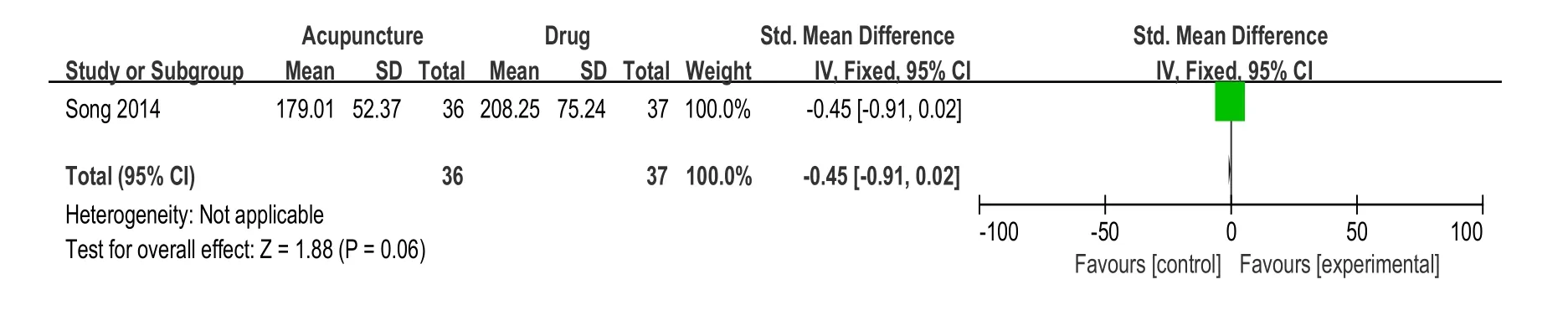
Figure 6 Acupuncture vs Drug on IBS-SSS.
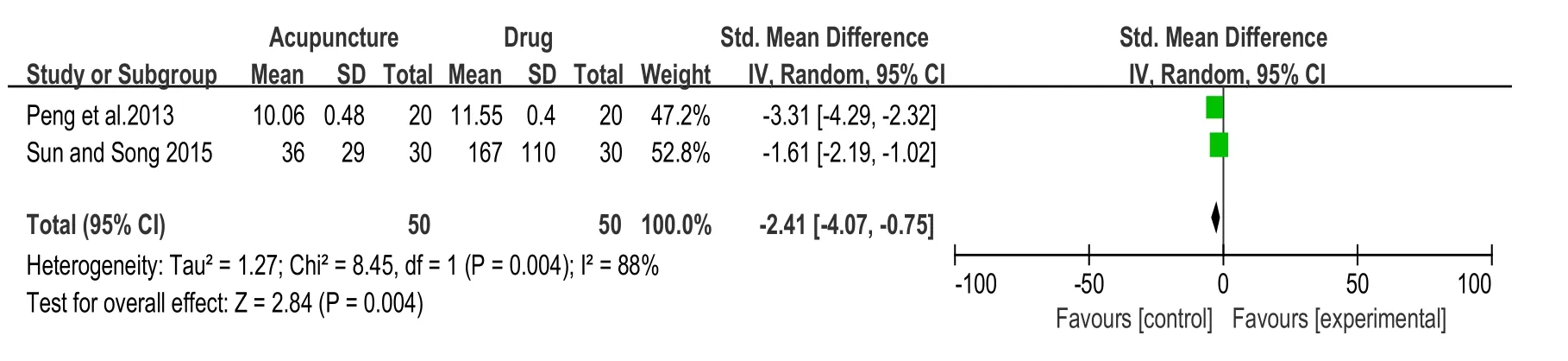
Figure 7 Acupuncture vs Drug on Global Symptom Score.
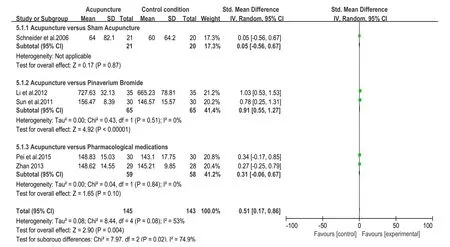
Figure 8 Acupuncture vs Controll condition on Quality of Life.
4.4 Quality of Life
Five RCTs compared acupuncture with control condition on quality of life[22,23,26,31,34]for which heterogeneity test was not acceptable(I2=53%,P=0.08).Therefore,a random-effect model was used for statistical analysis(see Figure 8).Our results showed that acupuncture showed superior effects to control condition on quality of life(n=288,SMD=0.51,CI=0.17-0.86,P=0.04).As different types of control conditions were included in different trials,a sub-analysis was performed to explore whether the heterogeneity could be partially explained by different types of control conditions.The results showed that acupuncture therapy could only improve the quality of life in “Pinaverium Bromide”subgroup.Since the IBS-QOL of one trial[31]wasmade by author himself,it was excluded from the sensitivity analysis,and the heterogeneity was reduced as a result(I2=15%,P=0.32).
4.5 Adverse Events.
All of these studies reported that no serious adverse event wasdetected during thetrial.
5.Discussion
Extensive search was manipulated through 7 electronic databases for acupuncture in treating in IBS.The studies election,data extraction,and analysis were conducted by two review authors independently.In this systematic review,seventeen randomized controlled trials[22-38]with 1032 subjects suffering from IBS.Of all RCTs,one study[32]was designed to compare acupuncture plus drug with sham acupuncture plus drug,one trial[22]compared acupuncture with sham acupuncture,fourteen trials compared acupuncture with drug[23-27,29-31,33-38],and one trial compared acupuncture plus drug with drug alone[28].In the outcomes,one RCT[32]and twelve trials[23,24, 26-27, 29-36] showed that acupuncture intervention significantly alleviated symptom severity.One trial[28]showed no statistically significant difference between acupuncture plus drug and drug alone on symptom severity.One RCT[38]compared acupuncture with drug failed to show statistically significant difference between acupuncture and drug on IBS-SSS.Two RCTs [25,30] compared acupuncture with drug on global symptom score didn’t show statistically significant difference.Five RCTs[22,23,26,31,34]compared acupuncture with control condition on quality of life showed that acupuncture showed superior effects to control condition.So far,there were three systematic reviews[17,19,21]that have assessed acupuncturetreatment for IBS.All of the reviews have assessed the effects and safety of acupuncture for IBS.However,the review by Z.Hussain,et al just included one randomized clinical trial(RCT)about acupuncture for IBS[17].The review by Schneider,et al included seven studies,but among them five articles were not RCTs[19].A recent review published in 2012[21]included seventeen RCTs,but nine RCTs were about acupuncture with moxibustion.All of them did not have enough evidence to authenticate the effectiveness of acupuncture for IBS.Therefore,we manipulated this systematic review to evaluate the effects of acupuncture for IBS on symptom severity,IBS-SSS,Global symptom score,and quality of life.In the current review, we analyzed seventeen RCTs accounting for 1032 subjects to confirm the effectivenessof acupuncturefor IBS.
There are still several limitations in this review.The key limitation was the poor quality of methodology of the included studies.Most of the RCTs did not provide detailed definition of the randomization process,such as information about allocation concealment,blinding process,information on dropout.The low quality of the included studies limited the reliability of outcomes of the systematic review.In addition,most of the RCTs did not follow up patients after acupuncture,and the long-t effect was unclear.Besides,the RCTs did not describe adverse effect;we can not evaluate the safety of acupuncturefor IBS.
Currently,based on this systematic review,no credible conclusion can be drawn regarding the effect of acupuncture for IBS.Although seventeen RCTs were identified,the methodological quality of the studies was low.In the end,in order to confirm the effects of acupuncture for IBS,large prospective trials with strict design should beconducted in thefuture.
Conflict of Interests
The authors claim that there is no conflict of interests regarding thepublication of thispaper.
1.Yan Y,Yan C.Complementary and Alternative Medicine for Treatment of Irritable Bowel Syndrome.Canadian Family Physician Medecin De Famille Canadien 2012,55(2):143-148.
2.Ma XP, Hong J, An CP, et al.Acupuncture-moxibustion in treating irritable bowel syndrome:How does it work?World J Gastroenterol 2014,20(20):6044-6054.
3.Drossman DA,Li Z,Andruzzi E,et al.U.S.householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact.Dig Dis Sci 1993,38(9):1569-1580.
4.El-Serag HB.Impact of irritable bowel syndrome:prevalence and effect on health-related quality of life.Rev Gastroenterol Disord 2003,3(Suppl 2):S3-S11.
5.Hungin A,Chang L,Locke G,et al.Irritablebowel syndrome in the United States:prevalence,symptom patterns and impact.Aliment Pharmacol Ther 2005,21(11):1365-1375.
6.Longstreth GF, Wolde-Tsadik G. Irritable bowel-type symptoms in HMO examinees.Prevalence,demographics,and clinical correlates.Dig Dis Sci1993,38(9):1581-1589.
7.Hulisz D.The Burden of Illness of Irritable Bowel Syndrome:Current Challenges and Hope for the Future.J Manag Care Pharm 2004,10(4):299-309.
8.Everhart,JE.The burden of digestive diseases in the United States.US Department of Health andHuman Services,Public Health Service,National Institutes of Health,National Institute of Diabetes and Digestive and Kidney Diseases.US Government Printing Office;Washington,DC:2008.p.142NIH,Publication No.09-6443.
9.Quigley EM,Craig OF.Irritable bowel syndrome;update on pathophysiology and management.Turk JGastroenterol 2012,23(4):313-322
10.Mayer EA.Irritable bowel syndrome.N Engl J Med 2008,358(16):1692–1699.
11.Dalrymple J, Bullock I. Diagnosis and management of irritable bowel syndrome in adults in primary care:summary of NICE guidance.BMJ 2008,336(7643):556–558.
12.Tack J,Fried M,Houghton LA,et al.Systematic review:the efficacy of treatments for irritable bowel syndrome—a European perspective.Aliment Pharmachol Ther 2006,24(2):183–205.
13.Chang FY,Lu CY.Treatment of Irritable Bowel Syndrome Using Complementary and Alternative Medicine.J Chin Med Assoc 2009,72(6):294-300.
14.Didari T, Mozaffari S, Nikfar S, et al.Effectiveness of probiotics in irritable bowel syndrome:Updated systematic review with meta-analysis.World J Gastroenterol 2015,21(10):3072-3084.
15.Enck?P,Martens?U,Klosterhalfen S.The psyche?and the?gut.World J Gastroenterol 2007,13(25):3405-3408.
16.Ouyang H,Chen JD.Review article:therapeutic roles of acupuncture in functional gastrointestinal disorders.Aliment Pharmacol Ther 2004,20(8):831–841.
17.Hussain Z,Quigley EM.Systematic review:complementary and alternative medicine in the irritable bowel syndrome.Aliment Pharmacol Ther 2006,23(4):465–471.
18.Toku Takahashi.Acupuncture for functional gastrointestinal disorders.J Gastroenterol 2006,41(6):408–417.
19.Schneider A,Streitberger K,Joos S.Acupuncture treatment in gastrointestinal diseases:A systematic review.World J Gastroenterol 2007,13(25):3417-3424.
20.Li CY1,Li SC.Treatment of irritable bowel syndrome in China:A review.World J Gastroenterol 2015,21(8):2315-2322.
21.Manheimer E,Wieland LS,Cheng K,et al Acupuncture for irritable bowel syndrome:systematic review and meta-analysis.Am J Gastroenterol 2012,107(6):835–848.
22.Schneider A,Enck P,Streitberger K,et al.Acupuncture treatment in irritable bowel syndrome.Gut 2006,55(5):649–654.
23.Sun JH,Wu XL,Xia C,et al.Clinical Evaluation of Soothing Gan(肝)and Invigorating Pi(脾)Acupuncture Treatment on Diarrhea-predominant Irritable Bowel Syndrome.Chin JIntegr Med 2011,17(10):780-785.
24.Chen YH,Chen XK,Yin XJ.Comparison of the Therapeutic Effects of Electroacupuncture and Probiotics Combined with Deanxit in Treating Diarrhea-Predominant Irritable Bowel Syndrome.Chin JIntegr Med 2012,32(5):594-598.
25.Peng SF,Yang JY,Shi T,et al.Clinical observation of electro-acupuncture for treatment of constipation-predominant irritable bowel syndromein patients.Chin JIntegr Trad West Med Dig 2013,21(8):426-428.
26.Pei L,Zhu L,Sun J,et al.Costipation predominent irritable bowel syndrome treated with acupuncture for regulating the mind and strengthening the spleen:a randomized controlled trial.Zhongguo Zhen Jiu 2015,35(11):1095-1098.
27.Wu JH. Clinical observation of warming acupuncture on diarrhea type of irritable bowel syndrome.Chin JInf TCM,2014,21(11):98-99.
28.Hou BG,Shi ZM.Discussion of the Therapeutic Effect of Western Medicine Association with Zi-Wu Dao-jiu Needling Tianshu and Dachangshu on Irritable Bowel Syndrome.Hebei Med 2011,17(9):1169-1172.
29.Liu N,Wang J,et al.Clinical research of acupuncture on Shang Juxu for irritable bowel syndrome.Shandong J Chin Med.2013,32(3):183-184.
30.Sun YZ,Song J.Clinical efficacy of acupuncture at Jiaji(EX-B2)in treating irritable bowel syndrome.Shanghai J Acu-mox.2015,34(9):856-857.
31.Li H,Pei LX,Zhou JL.Comparative observation on the therapeutic effects between acupuncture and western medication for diarrhea-predominant irritable bowel syndrome.Zhongguo Zhen Jiu 2012,32(8):679-682.
32.Qian HH,Zhu YP,Meng S,et al.Acupuncture treatment of diarrhea-predominant irritable bowel syndrome:a randomized controlled trial.Shi Jie Hua Ren Xiao Hua Za Zhi2011,19(3):257-261.
33.Wu XL,Wang YL,Sun JH,et al.Clinical observation on acupuncture for diarrhea-predominant irritable bowel syndrome patients in syndrome of liver-stagnation and spleen-deficiency and its impact on Th1/Th2.Zhongguo Zhen Jiu 2013,33(12):1057-1060.
34.Zhan DW.The acupuncture treatment of soothing the liver and tonifying the spleen method on diarrhea predominant irritable bowel syndrome patients'serum 5-HT,NPY and CGRP level changes.[M.S.thesis].Nanjing University of Chinese Medicine,Nanjing China,2013.
35.Li ZM.The acupuncture of soothing the liver and tonifying the spleen method on diarrhea predominant irritable bowel syndrome.[M.S.thesis].Liaoning University of Chinese Medicine,Liaoning China,2012.
36.Dou BF.The acupuncture of soothing the liver and regulating qi method on constipation predominant irritable bowel syndrome.[M.S.thesis].Liaoning University of Chinese Medicine,Liaoning China,2013.
37.Han GY.Observations on the Effieacy of AcuPuncturewith Soothing Liver Regulating Shell and PurgatingFu organs in Treating ConstiPation Predominan Irritable Bowel Syndrom.[M.S.thesis].Nanjing University of Chinese Medicine,Nanjing China,2011.
38.Song SQ.The long-term clinical curative effect observation of Soothing the liver and tonifying the spleen acupuncture treatment on diarrhea predominant irritable bowelsyndrome patients.[M.S.thesis].Nanjing University of Chinese Medicine,Nanjing China,2014.
 Traditional Medicine Research2016年4期
Traditional Medicine Research2016年4期
- Traditional Medicine Research的其它文章
- Dynamic changesof circulating Th1 and Th17 cellsin psoriasispatients:a report of 3 cases treated by Chineseherbal medicine
- Pharmacokinetic study of dl-tetrahydropalmatinepatchesby UPLC–MS/MSin rabbits
- A prospective,randomized controlled trial of sanguisorba oil in the treatment of tamoxifen-related vaginitisin breast cancer patients
- A Literature Review of the Acupoint Plaster Therapy for Asthma in Summer
- A new idea of electro-acupuncturetreatment for peripheral facial paralysis and thenerve-endocrinehypothesis
- Challengesand opportunitiesof applying P4 medicineand traditional Chinese medicinefor cancer treatment and prevention in the21st century:A medical oncologist’sperspectives
