Life-threatening Spontaneous Retroperitoneal Haemorrhage: Role of Multidetector CT-angiography for the Emergency Management
Zhi-wei Wang, Hua-dan Xue, Xiao-guang Li, Jie Pan, Xiao-bo Zhang, and Zheng-yu Jin*
Department of Radiology, Peking Union Medical College Hospital, Chinese Academy of Medical Science & Peking Union Medical College, Beijing 100730, China
Life-threatening Spontaneous Retroperitoneal Haemorrhage: Role of Multidetector CT-angiography for the Emergency Management
Zhi-wei Wang, Hua-dan Xue, Xiao-guang Li, Jie Pan, Xiao-bo Zhang, and Zheng-yu Jin*
Department of Radiology, Peking Union Medical College Hospital, Chinese Academy of Medical Science & Peking Union Medical College, Beijing 100730, China
spontaneous retroperitoneal haemorrhage; endovascular embolization; contrast enhanced computed tomography
Objective To evaluate the role of multidetector computed tomography-angiography (MDCTA) for management of life-threatening spontaneous retroperitoneal haemorrhage (SRH).
Methods A retrospective analysis of the medical records of all SRH patients admitted to our hospital from January 1, 2005 to November 31, 2014 was performed. SRH was defined as unrelated to invasive procedures, surgery, trauma, abdominal tumor or aortic aneurysm. Life-threatening SRH was defined as hemodynamic instability with hypotension. Sixteen cases met the inclusive criteria. Patients’characteristics, clinical presentation, imaging of MDCTA, treatment modalities, morbidity, and follow-up data were analyzed.
Results The group of 16 patients included 11 men and 5 women, with a mean age of 51.5±16.4 years. All patients underwent MDCTA scan examinations, and active contrast media (CM) extravasation were found in 9 patients. Angiography was performed for 8 patients in the CM extravasation group. Bleeding vessels were found in 7 patients who underwent successful embolization. One patient in the CM extravasation group did not undergo angiography and died of bleeding. Seven patients without active CM extravasation underwent conservative management. Bleeding was controlled for all these 7 patients, and 1 patient died of multiple organ failure. Fourteen patients survived from SRH were successfully discharged. One patient died of heart failure during follow-up.
Conclusion MDCTA was useful in the diagnosis of SRH and proved to be predictive for the outcome of conservative treatment and early intervention.S PONTANEOUS retroperitoneal haemorrhage (SRH) is a potentially fatal disease and it is difficult to diagnose the clinical entity that is defined as bleeding into the retroperitoneal space without associated trauma or iatrogenic manipulation.1It is most commonly seen in patients who are anticoagulated or are on haemodialysis.2-7Diagnosis is often delayed because of the lack of specific presenting symptoms. The rapid and accurate diagnosis is the key for the patients’survival, as the bleeding may be insidious and unrecognized initially.
Chin Med Sci J 2016; 31(1):43-48
Previous studies were small case-based series or single case report that focused on the relationship between SRH and the use of antiplatelet or anticoagulant therapies.2-7Transcatheter arterial embolization has become an accepted treatment option for SRH.2-5However, SRH is a complicated disease, with considerable heterogeneity, and conservative care may be sufficient for selected patients.8,9
The role of conventional computed tomography (CT)-scan in determining the bleeding location of SRH has been well demonstrated.10-14Recently, owing to technological advances, multidetector CT-angiography (MDCTA) has been successful in providing a detailed mapping of the vasculature, which should be helpful for the management of this disease in emergency setting.15In this study we described the experiences obtained in a single hospital of the management of 16 consecutive patients with life-threatening SRH. The purpose of this study was to evaluate the efficacy of MDCTA as the decision-making for the treatment plan.
PATIENTS AND METHODS
Patients
A retrospective analysis of the clinical and radiologic records of all patients diagnosed with SRH admitted to our hospital from January 1, 2005 to November 31, 2014 was done. Patients whose presentations were associated with invasive procedures, surgery, trauma, abdominal tumor or aortic aneurysm were excluded from the study. Life-threatening SRH was defined as hemodynamic instability with hypotension and systolic blood pressure <100 mm Hg, pulse >100 beats/min, hemoglobin concentration <100 g/L, or transfusion requirements of more than 4 U of packed red blood cells per 24 hours. Totally, 16 cases met the inclusive criteria and had an acute active severe SRH upon primary presentation to the Emergency Department or developed SRH during inpatient admission.
MDCTA scan protocol
All patients were initially underwent MDCTA scan examinations on either a 64-slice (Sensation 64, Siemens Healthcare, USA) or dual-source CT (Definition Flash, Siemens Healthcare) for the source of hemorrhage was not obvious. All scans were performed in 3 phases including an unenhanced, arterial, and portal phase covering the abdomen and pelvis from the xyphoid process to the inferior pubic ramus. After unenhanced CT scanning, all patients had an 18-gauge angiocatheter placed in an antecubital vein and 100 ml of 350 mgI/ml iohexol iodinated contrast media (CM) (Omnipaque 350, GE Healthcare, Shanghai, China) was administered intravenously at a rate of 4.0 ml per second by an automated power injector. The start of arterial phase scanning was controlled by bolus tracking with a region of interest in the descending aorta at the level of the diaphragm and a trigger threshold of 100 Hounsfield units (HU). The arterial phase was initiated 5 seconds after the bolus-triggering threshold was reached. The portal phase was performed 25 seconds after the arterial phase imaging acquisition. Images were reconstructed with a thin slice thickness of 1 mm for diagnostic evaluation. Two radiologists reviewed the transverse and reconstructed CT images prospectively on a Wizard workstation (Siemens Medical Solutions, USA) and determined positive CT findings in consensus. The diagnosis of active bleeding was made when any CM extravasation was found.
The decision to perform transcatheter arterial embolization was made by the interventional radiologist in consultation with the surgeon. For patients who underwent angiography and endovascular embolization, informed consent for the embolization procedure was obtained. Vital signs were monitored with pulse oximeter, blood pressure monitor, and electrocardiography. Midazolam was intravenously administered before the procedure. Angiography was performed under local anaesthesia with a common femoral artery approach via a 5-Fr vascular sheath (Cordis Europa N.V., Neth). Selective angiography using a Cobra catheter or Simmons catheter (TERUMO, JP) was performed on selected lumbar, internal iliac, intercostal and visceral arteries on the side ipsilateral to SRH according to CTA findings. Microcatheters (2.7/2.9 Fr. Progreat, TERUMO) were used coaxially when Simmons catheters or Cobra catheters could not be advanced into the distal arteries. The embolization was individually chosen to be accomplished with coils (Cook, IN, China). However, if the catheter could not be navigated distal to the bleeding site of the vessel, gelatin (Gelfoam, 500-700 μm, Hangzhou Alicon Pharm Sci & Tec Co., Ltd, China) was used and the embolization was accompanied by proximal coiling. Technical success was defined as cessation of active extravasation on catheter angiography.
Follow-up
All patients underwent close follow-up with the clinical examination, and ultrasonography or CT examination. Clinical success was defined as control of bleeding without repeat embolization or surgical intervention. The follow-up with the interval from 1 to 14 months was done retrospectively by patient’s records.
Statistical analysis
Statistical analyses were performed using statistical software (SPSS, version 13.0). Comparison of mean value between two groups was calculated using a Fisher’s exact t test. P value of 0.05 and below was considered statistically significant.
RESULTS
A total of 16 patients including 11 men and 5 women with a mean age of 51.5±16.4 years were included. Nine patients had an acute SRH upon primary presentation to the Emergency Department and seven patients developed SRH during inpatient admission. The underlying diseases were noted: hemophilia A (n=4), factor X deficiency (n=1), anticoagulation with warfarin (n=3), haemodialysis for chronic renal failure (n=4), hemophagocytic syndrome (n=2), and no obvious underlying diseases (n=2) (Table 1).
The most common symptom of SRH was pain, with abdominal pain prevailing in 9 (56%) patients, followed by back pain in 8 (50%) cases, hip pain in 4 (25%) cases, and leg pain in 3 (19%) cases. Other symptoms were noted: nausea (3 patients, 19%), weakness (3 patients, 19%), altered mental status (1 patient, 6%), and dizziness (1 patient, 6%). One (6%) patient showed no obvious symptom.
The mean hemoglobin concentration of the enrolled patients was 74.1±21.4 g/L. All patients were initially treated with fluid resuscitation, and 14 patients had received blood transfusion (2-11 units of packed red blood cells) before MDCTA examination. Platelet count, international normalized ratio (INR), and activated partial thromboplastin time (aPTT) were available for all patients. The mean value of platelet count, INR, and aPTT were (133.1± 71.1)×109/L, 1.73±1.07, and 49.5±18.6 seconds respectively. INR was subtherapeutic for 1 warfarin anticoagulated patient (case 6) (Table 1).
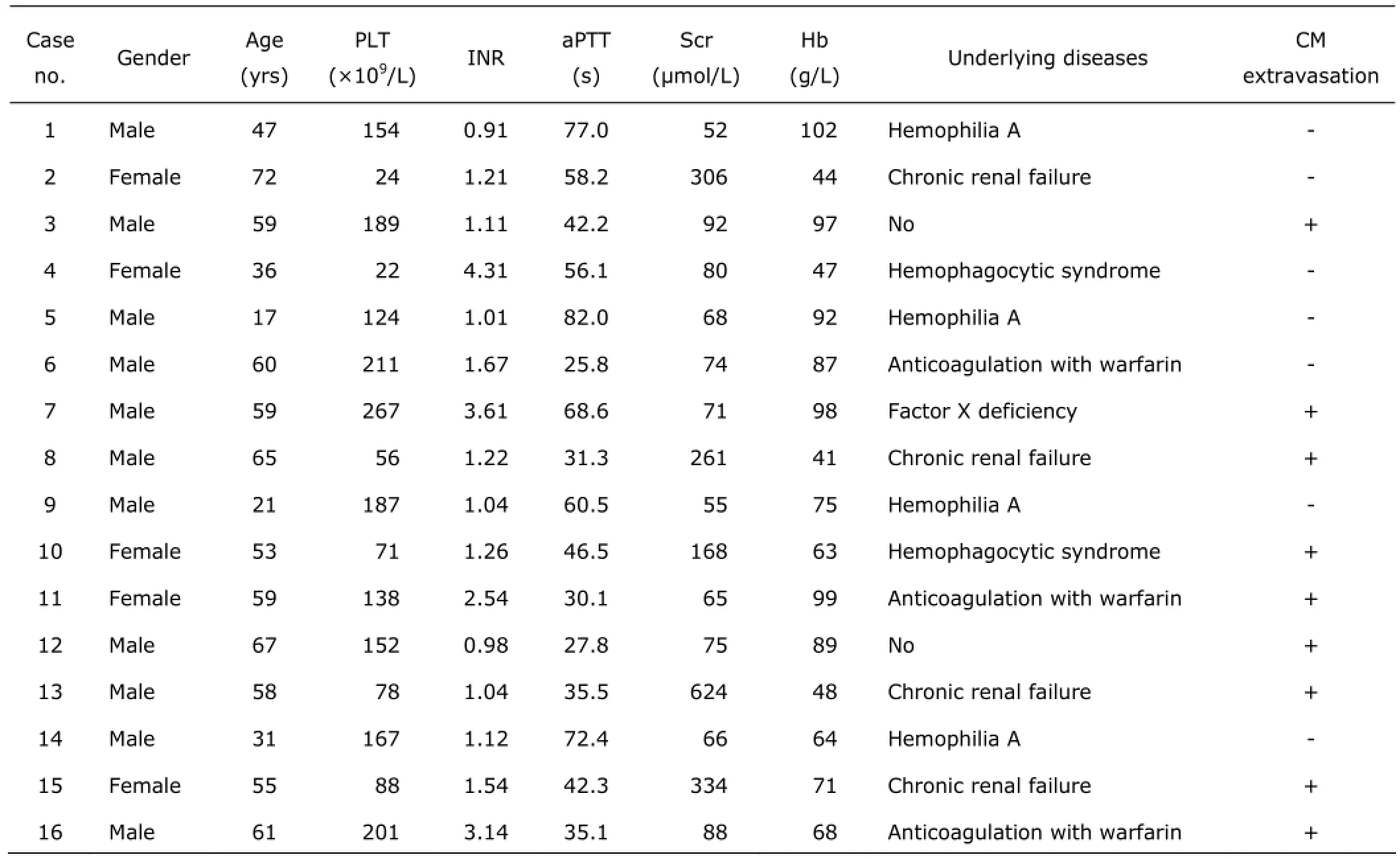
Table 1. Characteristics of the 16 enrolled patients
Active CM extravasation was found in 9 patients during CT scan (Fig. 1A and 1B). The mean hemoglobin concentration was 74.9 g/L for patients with CM extravasation, and 73.0 g/L for patients without CM extravasation, with no significant difference (P=0.961). Angiography was performed in 8 patients. Angiography showed extravasation in 7 (88%) of 8 cases. Selective catheterization of bleeding vessel was successful in the 7 patients (Table 2, Fig. 1C and 1D), and no embolization related complications were noted. Bleeding was controlled in 6 patients immediately after the procedure. And hemoglobin of 1 patient still declined from 46 to 41 g/L (case 13) despite 4 U of packed red blood cells transfusion within 48 hours after embolization. He was evaluated by repeated MDCTA examination, however, CM extravasation was not found. He continued to receive conservative treatment, and bleeding was controlled without repeat embolization or surgical intervention. Empirical embolization was not performed in 1 patient as contrast extravasation was not identified during angiography. He continued to undergo conservative treatment, and bleeding was controlled.
One patient (case 7) with active CM extravasation was treated for attempted correction of abnormal coagulation parameters before angiography. However, during conservative management, his condition suddenly deteriorated with a decreasing hemoglobin concentration and ultrasound revealed hematoma ruptured into the abdominal cavity. The patient died soon after ultrasound examination.
Seven patients with negative CM extravasation continued conservative management, including careful monitoring, fluid resuscitation, blood transfusion, and correction of abnormal coagulation factors. Bleeding was controlled for all patients, however, 1 patient died of multiple organ failure.
Five of the 14 patients survived abdominal compartment syndrome caused by SRH (Table 2) after 72 hours of angiography to avoid an abdominal compartment syndrome: 2 were treated surgically, and 3 with CT-guided drainage of hematoma. These 14 patients were successfully discharged. One patient died of heart failure during follow-up.
DISCUSSION
This study is a single-center retrospective analysis. Our result suggests that MDCTA is a useful modality in the management of severe SRH.
SRH is a complicated disease, with considerable heterpogeneity.1It is most commonly happened in patients with anticoagulation therapy, bleeding abnormalities, and haemodialysis.2-7However, we found SRH may develop in patients without coagulopathy, or with subtherapeutic INR of warfarin anticoagulation.
Whatever the etiology of retroperitoneal bleed is, all patients should initially be managed with careful monitoring, fluid resuscitation, blood transfusion, and normalization of coagulation factors. In the presence of coagulopathy, inherited clotting disorders, such as congenital haemophilia, it is generally accepted that clotting factor replacement and a conservative non-intervention approach may be sufficient.8,9However, 1 patient with factor X deficiency in our study died during he underwent conservative therapy. With respect to the life-threatening condition, the need for correction of coagulation disorder cannot be overemphasized, especially for patients with CM extravasation revealed by MDCTA.
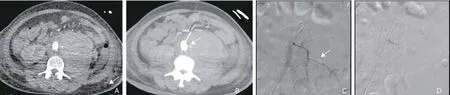
Figure 1. A 53-year-old woman with hemophagocytic syndrome.A. Transverse arterial computed tomography (CT) shows a large left retroperitoneal haematoma with active extravasation of contrast media (arrow).B. Maximal intensity projection (MIP) reconstruction of arterial phase CT depicts bleeding from the left L3lumbar artery (arrow).C. She underwent an emergency abdominal angiogram, and selective angiogram reveals bleeding from the left L3lumbar artery.D. Following embolization with coils, angiography through the microcatheter shows a satisfactory result.
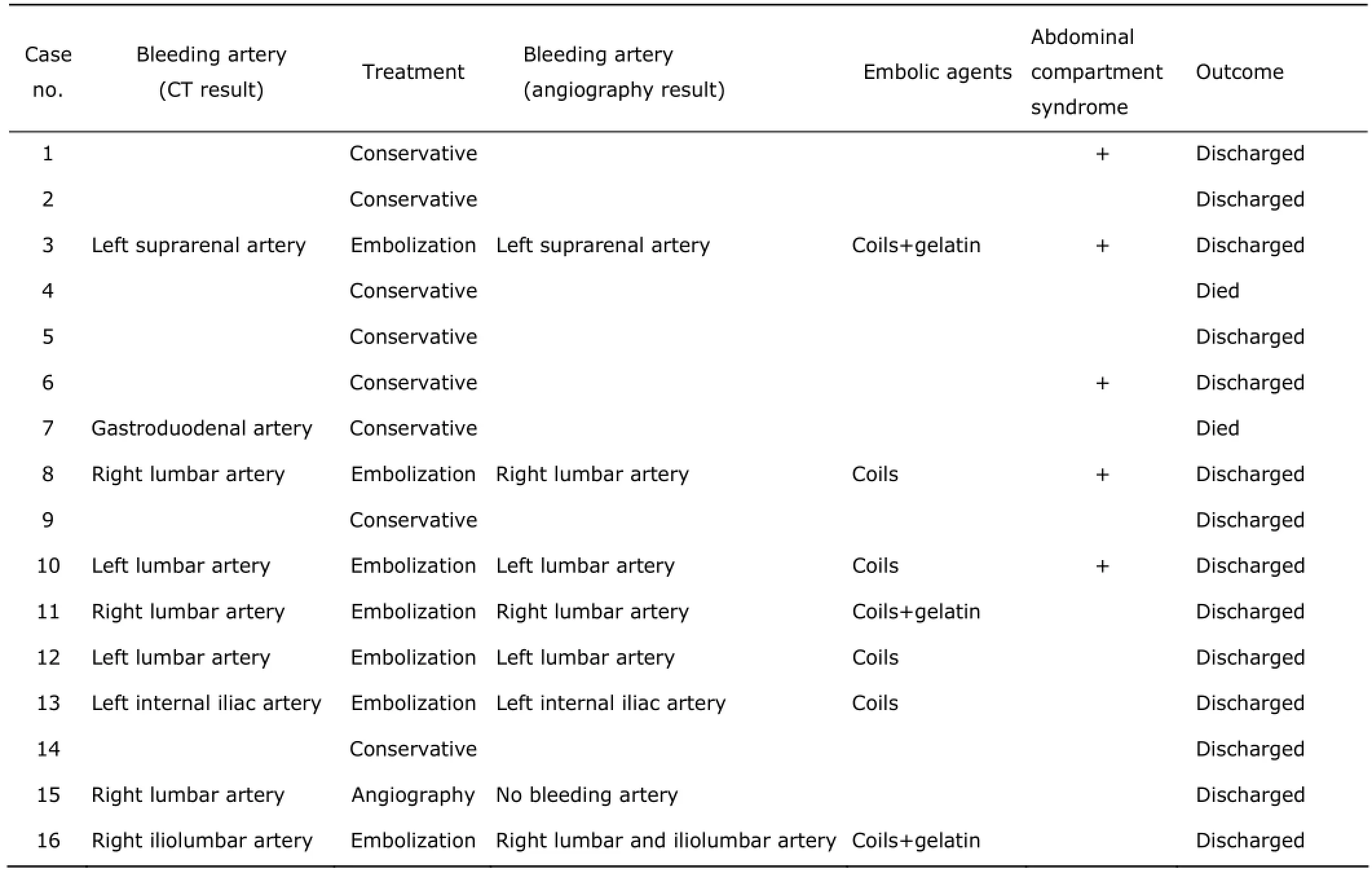
Table 2. Treatment and outcome of the 16 patients
There is a growing trend in the use of endovascular techniques as an alternative to open surgery in treatment of retroperitoneal haemorrhage, especially for patients with coagulopathy.2-5,16-18In the past, indications for embolisation were active bleeding and based on the haemodynamic instability. Panetta et al19considered that haemodynamic instability despite 4 or more units of blood transfusion within 24 hours, or 6 or more units of blood transfusion within 48 hours was an indication for urgent investigation and endovascular treatment. Patients with life-threatening SRH would develop refractory shock or transient hypotension, and there was no significant difference of mean hemoglobin concentration between patients with conservative therapy and those with angiography in our study, so it was very difficult to select which patient would benefit from invasive intervention therapy based on initial clinical evaluation.
CT plays an important role in the diagnosis of retroperitoneal haemorrhage, providing useful information on the location and extension of the bleeding.10-14With the introduction of MDCTA, the faster acquisition of thinner slices improves spatial resolution, and offers the possibility of isotropic reconstructions. CM extravasation on MDCTA indicates active bleeding. MDCTA can provide a detailed mapping of the vasculature. Thus, MDCTA is a helpful tool in treatment planning even in emergent hemodynamic instability caused by SRH. Active hemorrhage identified on MDCTA predicts failure of conservative treatment and indicates the need for early intervention. Timely endovascular treatment was very important for these patients.
In our study, MDCTA was effective in the diagnosis of SRH and also provided detail information for further angiography (Table 2). Negative CM extravasation results by MDCTA were obtained in 7 patients in our study. Although failure to demonstrate active bleeding is not proof of cessation of bleeding, the lesions may have a low bleeding rate.20Conservative care could also be undertaken secondary to a natural tamponade in this compartment, which allows for hemostasis, not like bleeding in gastrointestinal tract, where no natural tamponade would be formed. Conservative management was successful in 6 patients, except 1 patient who died due to multiple organ failure. Only 1 case died directly due to SRH. Moreover, with respect to management, our results suggest that angiography examinations following a negative contrast enhanced CT may be not necessary.
Life-threatening SRH are relatively rare to occur, making it difficult to collect a large number of cases forstudy. The limitations of our study are its retrospective nature and small number of cases examined.
SRH is an uncommon but potentially lethal entity. MDCTA was useful in the diagnosis of SRH and proved to be a predictive method in evaluating outcome of conservative treatment and need for early intervention.
REFERENCES
1. Chan YC, Morales JP, Reidy JF, et al. Management of spontaneous and iatrogenic retroperitoneal haemorrhage: conservative management, endovascular intervention or open surgery? Int J Clin Pract 2008; 62:1604-13.
2. Isokangas JM, Perälä JM. Endovascular embolization of spontaneous retroperitoneal hemorrhage secondary to anticoagulant treatment. Cardiovasc Intervent Radiol 2004; 27:607-11.
3. Sharafuddin MJ, Andresen KJ, Sun S, et al. Spontaneous extraperitoneal hemorrhage with hemodynamic collapse in patients undergoing anticoagulation: management with selective arterial embolization. J Vasc Interv Radiol 2001; 12:1231-4.
4. Park SH, Lee SW, Jeon U, et al. Transcatheter arterial embolization as treatment for a life-threatening retroperitoneal hemorrhage complicating heparin therapy. Kor J Intern Med 2011; 26:352-5.
5. Sunga KL, Bellolio MF, Gilmore RM, et al. Spontaneous retroperitoneal hematoma: etiology, characteristics, management, and outcome. J Emerg Med 2012; 43: e157-61.
6. Surani S, Estement B, Manchandan S, et al. Spontaneous extraperitoneal lumbar artery hemorrhage. J Emerg Med 2011; 40:e111-4.
7. Morita N, Kashihara K, Tagashira H, et al. Two cases of retroperitoneal hematoma caused by combination of anticoagulant therapy and 5-fluorouracil. J Med Invest 2005; 52:114-7.
8. Ylmaz S, Oren H, Irken G. et al. Life-threatening mediastinal-retroperitoneal hemorrhage in a child with moderate hemophilia A and high inhibitor titer: successful management with recombinant activated factor Ⅶ. J Pediatr Hematol Oncol 2005; 27: 400-2.
9. Leimkuhler K, Bach F, Kobert K. et al. Acquired hemophilia A as a cause of postoperative bleeding. Anasthesiol Intensivmed Notfallmed Schmerzther 2003; 38:359-65.
10. Scialpi M, Scaglione M, Angelelli G, et al. Emergencies in the retroperitoneum: assessment of spread of disease by helical CT. Eur J Radiol 2004; 50:74-83.
11. Becker CD, Mentha G, Schmidlin F, et al. Blunt abdominal trauma in adults: role of CT in the diagnosis and management of visceral injuries. Part 2: gastrointestinal tract and retroperitoneal organs. Eur Radiol 1998; 8:772-80.
12. Maluenda G, Mitulescu L, Ben-Dor I, et al. Retroperitoneal hemorrhage after percutaneous coronary intervention in the current practice era: clinical outcomes and prognostic value of abdominal/pelvic computed tomography. Catheter Cardiovasc Interv 2012; 80:29-36.
13. Tonolini M, Campari A, Bianco R. Common and unusual diseases involving the iliopsoas muscle compartment: spectrum of cross-sectional imaging findings. Abdom Imaging 2012; 37:118-39.
14. Yang DM, Jung DH, Kim H, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics 2004; 24:1353-65.
15. Farrelly C, Fidelman N, Durack JC, et al. Transcatheter arterial embolization of spontaneous life-threatening extraperitoneal hemorrhage. J Vasc Interv Radiol 2011; 22:1396-402.
16. Yamamura H, Morioka T, Yamamoto T, et al. Spontaneous retroperitoneal bleeding: a case series. BMC Res Notes 2014; 7:659.
17. Caleo O, Bocchini G, Paoletta S, et al. Spontaneous nonaortic retroperitoneal hemorrhage: etiology, imaging characterization and impact of MDCT on management. A multicentric study. Radiol Med 2015; 120:133-48.
18. Patel A, Downing R, Vijay S. Spontaneous rupture of the adrenal artery successfully treated using the endovascular approach: a report of 2 cases. Vasc Endovascular Surg 2013; 47:124-7.
19. Panetta T, Sclafani SJ, Goldstein AS, et al. Percutaneous transcatheter embolization for massive bleeding from pelvic fractures. J Trauma 1985; 25:1021-9.
20. Sun H, Jin Z, Li X, et al. Detection and localization of active gastrointestinal bleeding with multidetector row computed tomography angiography: a 5-year prospective study in one medical center. J Clin Gastroenterol 2012; 46:31-41.
for publication July 28, 2015.
*Corresponding author Tel: 86-10-69155442, Fax: 86-10-69155441, E-mail: zhengyu_jin@163.com
 Chinese Medical Sciences Journal2016年1期
Chinese Medical Sciences Journal2016年1期
- Chinese Medical Sciences Journal的其它文章
- Pathology Verified Concomitant Papillary Thyroid Carcinoma in the Sonographically Suspected Thyroid Lymphoma: A Case Report△
- Percutaneous Removal of Benign Breast Lesions with an Ultrasound-guided Vacuum-assisted System: Influence Factors in the Hematoma Formation△
- Respiratory and Cardiac Characteristics of ICU Patients Aged 90 Years and Older: A Report of 12 Cases
- Establish Albumin-creatinine Ratio Reference Value of Adults in the Rural Area of Hebei Province△
- Positive Rate of Different Hepatitis B Virus Serological Markers in Peking Union Medical College Hospital, a General Tertiary Hospital in Beijing△
- Association Between Geranylgeranyl Pyrophosphate Synthase Gene Polymorphisms and Bone Phenotypes and Response to Alendronate Treatment in Chinese Osteoporotic Women△
