不同糖化血红蛋白控制水平糖尿病并发肺炎克雷伯杆菌肝脓肿患者的临床和影像学表现
刘 波,丁 炎,王爱花,周群燕,邬匡杰,程海燕
·临床诊疗提示·
不同糖化血红蛋白控制水平糖尿病并发肺炎克雷伯杆菌肝脓肿患者的临床和影像学表现
刘 波,丁 炎,王爱花,周群燕,邬匡杰,程海燕
目的探讨不同糖化血红蛋白(HbA1c)控制水平糖尿病并发肺炎克雷伯杆菌肝脓肿(KPLA)患者的临床和影像学表现。方法选取2008年1月—2015年9月南京医科大学附属无锡人民医院收治的146例糖尿病并发KPLA患者,根据HbA1c水平分成3组:A组31例,HbA1c水平控制好,HbA1c≤7.0%;B组52例,HbA1c水平控制较好,7.0%
糖尿病;肝脓肿;肺炎克雷伯菌;血红蛋白A,糖基化
刘波,丁炎,王爱花,等.不同糖化血红蛋白控制水平糖尿病并发肺炎克雷伯杆菌肝脓肿患者的临床和影像学表现[J].中国全科医学,2016,19(23):2840-2844.[www.chinagp.net]
LIU B,DING Y,WANG A H,et al.Clinical and imaging features of patients with bacterial liver abscess caused by Klebsiella pneumoniae in diabetics at different levels of glycosylated hemoglobin control[J].Chinese General Practice,2016,19(23):2840-2844.
近年来,研究报道充分证实了肺炎克雷伯杆菌已成为细菌性肝脓肿优势致病菌[1-4]。糖尿病患者为肝脓肿的高发人群[5]。国内外已明确了糖化血红蛋白(HbA1c)水平与糖尿病并发症之间的关系[5-7]。本研究回顾性分析不同HbA1c控制水平糖尿病并发肺炎克雷伯杆菌肝脓肿(Klebsiella pneumoniae liver abscesses,KPLA)患者的基本资料、基础疾病、症状和体征、穿刺引流术前影像学表现、并发症、脓肿转移、治疗及预后情况等,以期对其诊治提供参考。
1 资料与方法
1.1临床资料2008年1月—2015年9月南京医科大学附属无锡人民医院共收治289例细菌性肝脓肿患者,经超声引导下穿刺抽取脓液培养证实为KPLA 190例(65.74%),其中糖尿病并发KPLA患者146例。
1.2分组根据入院时HbA1c水平分成3组:A组31例,HbA1c水平控制好,HbA1c≤7.0%;B组52例,HbA1c水平控制较好,7.0%
1.3方法收集糖尿病并发KPLA患者基本资料(性别、年龄、发热时间、住院时间),基础疾病〔高血压、高脂血症、胆管疾病(包括胆囊炎、胆囊结石、胆管囊状扩张等)、恶性肿瘤、肝硬化、慢性肾功能不全〕,症状和体征〔发热(体温>38 ℃)、寒战、乏力、腹痛、恶心呕吐、意识改变(包括嗜睡、昏睡、昏迷等)、腹泻、黄疸、右上腹压痛、腹直肌紧张〕,穿刺引流术前影像学表现(超声检查:脓肿数量、脓肿位置、脓肿大小、胆管系统积气,CT检查:脓腔内积气、肝静脉血栓性静脉炎、胸膜增厚征象),并发症〔胸腔积液、腹腔积液、脓毒血症、急性肾衰竭、急性呼吸衰竭、糖尿病酮症酸中毒(DKA)、急性呼吸窘迫综合征(ARDS)〕,脓肿转移(膈下脓肿、腹腔脓肿、心包积液、肾脓肿、皮肤软组织脓肿、肺脓肿、脑脓肿),治疗及预后。

2 结果
2.1基本资料3组患者性别构成、发热时间比较,差异均无统计学意义(P>0.05);3组患者年龄、住院时间比较,差异均有统计学意义(P<0.05);其中B组患者住院时间较A组延长,差异有统计学意义(P<0.05);C组患者年龄较A组和B组小、住院时间较A组和B组延长,差异均有统计学意义(P<0.05,见表1)。

表1 3组患者基本资料比较
注:A组为糖化血红蛋白(HbA1c)水平控制好组,B组为HbA1c水平控制较好组,C组为HbA1c水平控制差组;与A组比较,aP<0.05;与B组比较,bP<0.05
2.2基础疾病糖尿病并发KPLA患者基础疾病第一位是高血压〔60.27%(88/146)〕,其次为高脂血症〔58.22%(85/146)〕、胆管疾病〔41.10%(60/146)〕等。3组患者高血压、胆管疾病、肝硬化发生率比较,差异均无统计学意义(P>0.05);B组无恶性肿瘤患者,A组与C组患者恶性肿瘤发生率比较,差异无统计学意义(P>0.05);3组患者高脂血症、慢性肾功能不全发生率比较,差异均有统计学意义(P<0.05);其中B组患者高脂血症、慢性肾功能不全发生率较A组升高,C组患者高脂血症、慢性肾功能不全发生率较A组和B组升高,差异均有统计学意义(P<0.01,见表2)。
2.3症状和体征3组患者发热、寒战、乏力、腹痛、恶心呕吐、意识改变、腹泻、黄疸、右上腹压痛、腹直肌紧张发生率比较,差异均无统计学意义(P>0.05,见表3)。
2.4穿刺引流术前影像学表现糖尿病并发KPLA患者脓肿以单发为主,多见于肝右叶,脓肿大小以5~10 cm为主。3组患者超声检查脓肿数量、脓肿位置、脓肿大小构成比及CT检查肝静脉血栓性静脉炎发生率比较,差异均无统计学意义(P>0.05);3组患者超声检查胆管系统积气、CT检查脓腔内积气、胸膜增厚发生率比较,差异均有统计学意义(P<0.05);其中B组患者超声检查胆管系统积气、CT检查脓腔内积气、胸膜增厚发生率较A组升高,C组患者超声检查胆管系统积气、CT检查脓腔内积气、胸膜增厚发生率较A组和B组升高,差异均有统计学意义(P<0.01,见表4)。
2.5并发症糖尿病并发KPLA患者主要并发症为胸腔积液、腹腔积液、脓毒血症等。3组患者腹腔积液、脓毒血症发生率比较,差异均无统计学意义(P>0.05)。A组患者无急性肾衰竭、急性呼吸衰竭、DKA发生,B组与C组患者急性肾衰竭、急性呼吸衰竭、DKA发生率比较,差异均无统计学意义(P>0.05)。A组和B组患者均无ARDS发生,C组3例(4.8%)患者发生ARDS。3组患者胸腔积液发生率比较,差异有统计学意义(P<0.05);其中B组患者胸腔积液发生率较A组升高,差异有统计学意义(P<0.01);C组患者胸腔积液发生率较A组和B组升高,差异均有统计学意义(P<0.01,见表5)。
2.6脓肿转移糖尿病并发KPLA患者脓肿转移常见有膈下脓肿、腹腔脓肿、心包积液等。3组患者膈下脓肿发生率比较,差异有统计学意义(P<0.05);其中C组患者膈下脓肿发生率较A组和B组升高,差异均有统计学意义(P<0.01)。3组患者腹腔脓肿、心包积液发生率比较,差异均无统计学意义(P>0.05)。A组患者无肾脓肿、皮肤软组织脓肿发生,B组与C组患者肾脓肿、皮肤软组织脓肿发生率比较,差异均无统计学意义(P>0.05)。A组和B组患者均无肺脓肿、脑脓肿发生,C组2例(3.2%)患者发生肺脓肿,1例(1.6%)患者发生脑脓肿(见表6)。

表2 3组患者基础疾病发生率比较〔n(%)〕
注:-为采用Fisher确切概率法;与A组比较,aP<0.01;与B组比较,bP<0.01

表3 3组患者症状和体征发生率比较〔n(%)〕
注:-为采用Fisher确切概率法
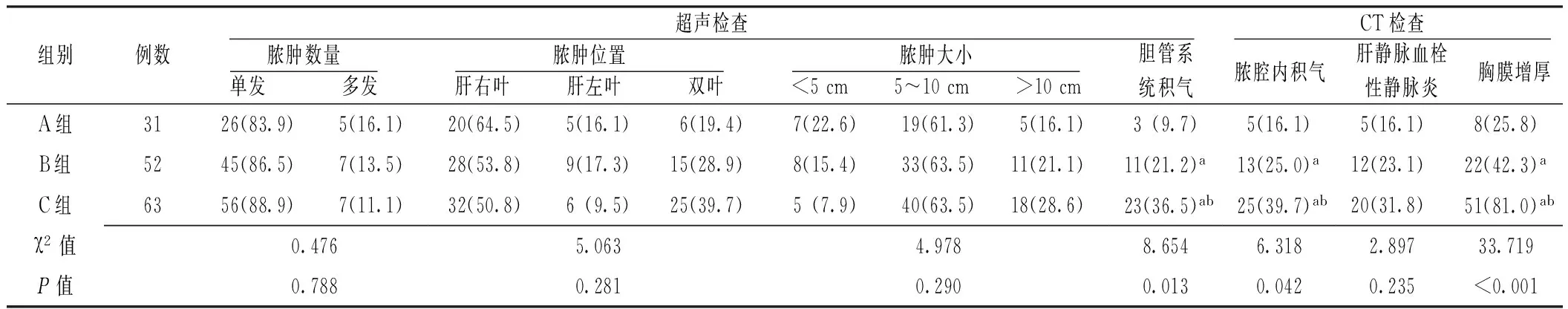
表4 3组患者穿刺引流术前影像学表现比较〔n(%)〕
注:与A组比较,aP<0.01;与B组比较,bP<0.01
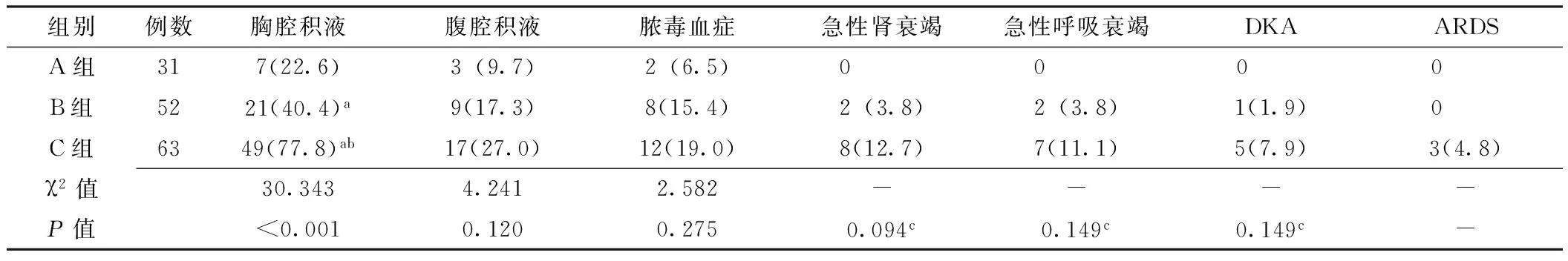
表5 3组患者并发症发生率比较〔n(%)〕
注:DKA=糖尿病酮症酸中毒,ARDS=急性呼吸窘迫综合征;与A组比较,aP<0.01;与B组比较,bP<0.01;c为采用Fisher确切概率法;-表示无此项数据

表6 3组患者脓肿转移发生率比较〔n(%)〕
注:与A组比较,aP<0.01;与B组比较,bP<0.01;c为采用Fisher确切概率法;-表示无此项数据
2.7治疗及预后患者入院后,采用超声引导定位下肝脓肿穿刺引流,若脓液不多,穿刺过程中完全抽取;脓液多,则摆放引流管,持续引流。抗生素包括第二代头孢菌素或第三代头孢菌素,外加甲硝唑或奥硝唑联合氟喹诺酮类为主的抗感染治疗。C组中有1例因全身多发感染并发多器官衰竭死亡,其余患者均恢复出院。
3 讨论
肺炎克雷伯杆菌属于革兰阴性杆菌,目前多项研究证实,其已经取代了大肠埃希菌成为细菌性肝脓肿的主要致病菌[1-2]。糖尿病患者为肝脓肿的高发人群[5]。糖尿病患者易并发KPLA,学者认为这可能与糖尿病患者血管内膜异常,使其成为肺炎克雷伯杆菌血源性播散有关[9]。肺炎克雷伯杆菌经过胆管、门静脉、肝动脉和开放性损伤的创口直接进入肝脏。肝脏由于其血运丰富且具有单核-巨噬细胞系统的强大吞噬作用,故肝脏原发性肺炎克雷伯杆菌化脓性感染不易发生,KPLA多为在基础疾病基础上继发感染引起。本研究中,有胆管疾病的患者60例(41.1%),与文献报道相符[3-4]。
3.1HbA1c的重要意义大量临床研究证实,HbA1c可作为糖尿病患者长期血糖控制的指标,其与糖尿病并发症的发生和发展有密切联系[5-7]。在糖尿病和心血管疾病行动(ADVANCE)研究中,要求糖尿病强化治疗组平均HbA1c水平下降到7.0%,标准治疗组下降到9.0%[7-8]。因此本研究根据HbA1c水平分为:HbA1c水平控制好,HbA1c≤7.0%;HbA1c水平控制较好,7.0%
3.2不同HbA1c控制水平糖尿病并发KPLA患者一般情况比较国内外文献报道,糖尿病患者并发肝脓肿平均发病年龄比非糖尿病患者大4岁,住院时间多3~4 d[5-7]。本研究中C组患者较另外两组平均发病年龄更低,且住院时间更长。糖尿病患者存在血脂代谢紊乱,其血脂水平随着血糖水平升高而升高,C组患者较其他两组更易合并高脂血症。HbA1c水平控制差,使体内2,3-二磷酸甘油酸的反应性降低,血红蛋白对氧的结合能力增强而不易释放氧,造成局部组织细胞长期缺氧,这些变化和糖尿病肾病、视网膜、微血管等部位的慢性并发症有极密切的关系。因此控制好HbA1c水平就能有效控制并发症,反之,HbA1c水平控制差易合并慢性肾功能不全等并发症。本研究结果显示,B组患者高脂血症、慢性肾功能不全发生率较A组升高,C组患者高脂血症、慢性肾功能不全发生率较A组和B组升高。糖尿病并发KPLA患者最常见的症状为发热、寒战、乏力、腹痛、恶心呕吐、意识改变、腹泻等,但上述症状特异性较低,本研究中不同HbA1c控制水平糖尿病并发KPLA患者主要症状和体征发生率并无差异。
3.3不同HbA1c控制水平糖尿病并发KPLA患者的影像学特征及临床意义既往报道只是笼统地认为糖尿病是KPLA的致病及预后不良的因素[10-11]。当糖尿病患者发生KPLA时,必然存在应激性血糖水平升高,且常规血糖水平测定只代表瞬间血糖,而HbA1c水平代表测定前8~12周的平均血糖水平,能弥补常规血糖水平测定的不足。最新研究通过评估不同HbA1c水平来了解糖尿病并发KPLA患者的临床特点,得出结论认为:HbA1c水平控制不良,而非入院时高血糖水平,与糖尿病并发KPLA患者的不良预后相关[12]。但此项研究并未系统评估患者CT及超声的影像学特点。当脓腔中出现气体时,超声表现为散在点状、短棒状强高回声光斑,后方伴彗星尾征;CT表现为低密度,常可见液平面。本研究中C组患者胆管系统积气及脓腔内积气发生率较A组和B组升高。既往研究认为形成气腔的肝脓肿和肝静脉血栓性静脉炎等影像学征象可能与病死率及并发症有关[13-14]。某些影像学证据会有助于临床治疗方案的制定,当发现特定影像学特征时必须提高警惕,应进行适当的血糖控制、脓肿引流、营养支持及抗生素的调整,以避免并发症。有研究报道,如果在72 h内准确预测及识别KPLA的转移性感染的风险,有75%的转移性感染是可以避免[15]。本研究还发现C组患者胸腔积液、膈下脓肿发生率升高,甚至有文献报道可致眼球及前列腺的转移性感染[16],提示在诊治过程中不能低估其他部位转移性感染的发生,胸部CT、颅脑MRI、泌尿系统超声及超声心动图均是有必要的。
总之,糖尿病并发KPLA患者HbA1c水平控制差者年龄偏小、住院时间较长,高脂血症、慢性肾功能不全发生率高,超声检查胆管系统积气、CT检查脓腔内积气、胸膜增厚发生率高,胸腔积液和膈下脓肿发生率较高,重症者可发生死亡。HbA1c水平控制不佳与气体形成、脓肿转移等有关,早期发现这些影响预后的影像学征象在治疗过程中起重要作用。但由于本研究样本量相对较小,故得出的结果有一定局限性,尚需更大样本的研究来进一步证实。
作者贡献:刘波、丁炎进行课题设计与实施、资料收集整理、撰写论文、成文并对文章负责;王爱花、周群燕、邬匡杰、程海燕进行课题实施、评估、资料收集;丁炎进行质量控制及审校。
本文无利益冲突。
[1]QU T T,ZHOU J C,JIANG Y,et al.Clinical and microbiological characteristics of Klebsiella pneumoniae liver abscess in East China[J].BMC Infect Dis,2015,15:161.
[2]ONTANILLA G,HERRERA J M,ALCVAR J M,et al.Liver abscess due to Klebsiella pneumoniae and its relation to colon lesions[J].Rev Esp Enferm Dig,2015,107(1):51-52.
[3]BILAL S,VOLZ M S,FIEDLER T,et al.Klebsiella pneumoniae-induced liver abscesses,Germany[J].Emerg Infect Dis,2014,20(11):1939-1940.
[4]CHAVADA R,NG J,MALEY M,et al.Emergence of Klebsiella pneumoniae liver abscesses in South-western Sydney[J].Infection,2014,42(3):595-596.
[5]MCEWAN P,FOOS V,LAMOTTE M.The impact of baseline HbA1cand HbA1ctrajectories on time to therapy escalation in type 2 diabetes mellitus[J].Value Health,2015,18(7):698-705.
[6]TAIEB V,PACOU M,SCHROEDER M,et al.Network Meta-analysis(NMA) to assess relative efficacy measured as percentage of patients treated to HbA1ctarget with canagliflozin in patients with type 2 diabetes mellitus(T2DM) inadequately controlled on metformin and sulphonylurea(MET+SU)[J].Value Health,2015,18(7):598-603.
[7] 宋静,朱敏.老年2型糖尿病合并高血压患者糖化血红蛋白水平与左心室功能的相关性研究[J].中国全科医学,2013,16(12):4253-4257.
SONG J,ZHU M.Relationship between glycated hemoglobin and left ventricular function in elderly prtients with type 2 diabetes mellitus and hypertension[J].Chinese General Practice,2013,16(12):4253-4257.
[8] 王珊珊,陈莉明,常宝成,等.2型糖尿病患者血清钙与糖代谢的相关关系[J].中华内分泌代谢杂志,2014,30(1):26-30.
WANG S S,CHEN L M,CHANG B C,et al.Correlaion between serum calcium and glucose metabolism in patients with type 2 diabetes mellitus[J].Chinese Journal of Endocrinology and Metabolism,2014,30(1):26-30.
[9]YOON DA H,JEON Y J,BAE E Y,et al.Liver abscess due to Klebsiella pneumoniae in a healthy 12-year-old boy[J].Korean J Pediatr,2013,56(11):496-499.
[10]孙文早,王亮,张高生.2型糖尿病患者社区获得性下呼吸道感染调查及危险因素分析[J].中国全科医学,2012,15(4):1201-1204.
[11]赵小芹,蒋艳敏,朱晓巍,等.糖尿病合并细菌性肝脓肿的临床特征分析[J].中华内分泌代谢杂志,2012,28(1):48-50.
[12]LIAO W I,SHEU W H,CHANG W C,et al.An elevated gap between admission and A1C-derived average glucose levels is associated with adverse outcomes in diabetic patients with pyogenic liver abscess[J].PLoS One,2013,8(5):e64476.
[13]ALSAIF H S,VENKATESH S K,CHAN D S,et al.CT appearance of pyogenic liver abscesses caused by Klebsiella pneumoniae[J].Radiology,2011,260(1):129-138.
[14]LEE C J,HAN S Y,LEE S W,et al.Clinical features of gas-forming liver abscesses:comparison between diabetic and nondiabetic patients[J].Korean J Hepatol,2010,16(2):131-138.
[15]LEE S S,CHEN Y S,TSAI H C,et al.Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess[J].Clin Infect Dis,2008,47(5):642-650.
[16]VANDEVELDE A,STEPANOVIC B.On a boat:a case in Australia of endophthalmitis and pyogenic liver,prostatic,and lung abscesses in a previously well patient due to Klebsiella pneumoniae[J].Case Rep Infect Dis,2014,2014:137248.
(本文编辑:陈素芳)
Clinical and Imaging Features of Patients With Bacterial Liver Abscess Caused by Klebsiella Pneumoniae in Diabetics at Different Levels of Glycosylated Hemoglobin Control
LIUBo,DINGYan,WANGAi-hua,ZHOUQun-yan,WUKuang-jie,CHENGHai-yan.
DepartmentofMedicalUltrasound,WuxiPeople′sHospitalofNanjingMedicalUniversity,Wuxi214023,China
DINGYan,DepartmentofMedicalUltrasound,WuxiPeople′sHospitalofNanjingMedicalUniversity,Wuxi214023,China;E-mail:157817553@qq.com
ObjectiveTo discuss the clinical and imaging features of patients with bacterial liver abscess caused by Klebsiella pneumoniae liver abscesses(KPLA) in diabetics at different levels of glycosylated hemoglobin(HbA1c) control.MethodsA total of 146 patients with diabetes combined with KPLA admitted in Wuxi People′s Hospital of Nanjing Medical University from January 2008 to September 2015 were selected.According to the levels of HbA1c,they were divided into three groups,namely group A including 31 patients with good control of HbA1clevel,HbA1c≤ 7.0%;group B including 52 patients with relatively control of HbA1clevel,7.0%< HbA1c≤ 9.0%;and group C including 63 patients with poor control of HbA1clevel,HbA1c>9.0%.The basic information,underlying diseases,signs and symptoms,imaging features before abscess drainage,complications,abscess metastasis,treatment and prognosis of the patients in 3 groups were collected and compared.ResultsThe time of hospital stay of patients in group B was longer than that in group A(P<0.05).The age of patients in group C was younger than that in group A and group B,the time of hospital stay of patients in group C was longer than that in group A and group B(P<0.05).The incidence of hyperlipidaemia,chronic renal failure,pneumatosis of biliary system by ultrasonic,pneumatosis of vomica exaimined and pleural thickening by CT,pleural effusion of patients in group B were higher than those in group A(P<0.01).The incidence of hyperlipidaemia,chronic renal failure,pneumatosis of biliary system by ultrasonic,pneumatosis of vomica exaimined and pleural thickening by CT,pleural effusion,subphrenic abscesses of patients in group C were higher than those in group A and group B(P< 0.01).All patients1clevel have young and longer time in hospitalization,higher incidence of hyperlipemia and chronic renal failure.The imaging features shows the high incidence of pneumatosis of biliary system by ultrasonic,pneumatosis of vomica exaimined and pleural thickening by CT,as well as higher incidence of pleural effusion,subphrenic abscesses.Patients with severe illness may die and they should be thought highly of and prevented from diseases with poor prognosis.
the ultrasound guided percutaneous catheter drainage for liver abscess after their admission.One case of patient in group C died of systemic multiple infection complicated by organ failure.The rest patients had recovered and been discharged from hospital.ConclusionPatients with diabetes complicated by KPLA and with poor control of HbA
Diabetes mellitus;Liver abscess;Klebsiella pneumoniae;Hemoglobin A,glycosylated
214023江苏省无锡市,南京医科大学附属无锡人民医院超声医学科(刘波,丁炎),医学影像科(王爱花),消化内科(周群燕),肝胆外科(邬匡杰),内分泌科(程海燕)
丁炎,214023江苏省无锡市,南京医科大学附属无锡人民医院超声医学科;E-mail:157817553@qq.com
R 587.1R 575.4
B
10.3969/j.issn.1007-9572.2016.23.021
2015-11-23;
2016-04-01)

