血浆sLOX-1水平与冠状动脉慢血流的相关性
任引刚, 刘 军, 任一然, 张 昕, 韩 伟, 楚 轶, 李宏增*
(1第四军医大学唐都医院老年病科,西安 710038; 2第四军医大学唐都医院心内科;*通讯作者,E-mail: tangduzhaoly@126.com)
血浆sLOX-1水平与冠状动脉慢血流的相关性
任引刚1, 刘军1, 任一然1, 张昕1, 韩伟2, 楚轶2, 李宏增1*
(1第四军医大学唐都医院老年病科,西安710038;2第四军医大学唐都医院心内科;*通讯作者,E-mail: tangduzhaoly@126.com)
摘要:目的探讨血浆可溶性凝集素样氧化型低密度脂蛋白受体-1 (sLOX-1)水平与冠状动脉慢血流的相关性。 方法该研究共纳入82名冠脉慢血流患者(慢血流组,n=82)及184名冠脉血流正常者(对照组,n=184),采用酶联免疫吸附(ELISA)法测定两组的血浆sLOX-1水平并比较,采用参照心肌梗死溶栓治疗后(thrombolysis in myocardial infarction,TIMI)血流帧数(TFC)评价冠脉血流速度。通过多元Logistic 回归分析评价血浆sLOX-1水平与合并冠心病的独立相关性,采用Spearman相关分析评价血浆sLOX-1水平与平均TMI-TFC的相关性。结果慢血流组患者血清sLOX-1水平显著高于对照组[0.94(0.48-1.30)vs 0.47(0.39-0.86) ng/ml,P﹤0.001]。多元Logistic回归分析显示血浆sLOX-1水平是预测冠脉慢血流独立危险因子(优势比2.044, 95% 可信区间1.274-3.279;P=0.003)。Spearman相关分析结果显示,血浆sLOX-1水平与TIMI-TFC呈显著正相关(rs=0.315,P=0.004)。结论血浆sLOX-1水平与冠脉慢血流的发生及严重程度存在独立正相关,sLOX-1有望成为预测冠脉慢血流风险并对其进行危险分层的重要生物标记物。
关键词:心血管疾病;冠状动脉慢血流;可溶性凝集素样氧化型低密度脂蛋白受体-1;生物学标记物
冠状动脉慢血流现象(coronary slow flow phenomenon,CSFP)是一种冠脉造影时的血流现象,主要指在冠状动脉不存在显著狭窄(狭窄程度﹤40%)的情况下,远端冠脉血管发生血流灌注延迟的现象[1,2]。据报道,在疑诊冠心病进行冠脉造影的人群中,大约有7%的患者会出现CSFP[3]。研究表明,CSFP与心绞痛发作、心肌梗死、恶性心律失常甚至心源性猝死等不良心血管事件有一定关联[4,5],因此越来越受到重视。
CSFP的病理生理机制仍未完全明确,前期研究表明,炎症反应、氧化应激、冠脉内皮功能不全等都可能在CSFP的发生发展中起一定作用[5,6]。凝集素样氧化低密度脂蛋白受体-1(LOX-1)是一种主要表达于内皮细胞、血管平滑肌细胞(VSMC)及巨噬细胞的Ⅱ型糖蛋白,其主要功能是结合、内吞并降解氧化型低密度脂蛋白(ox-LDL)[7]。LOX-1与其配体的结合,可激活下游的信号转导通路,广泛参与炎症反应、氧化应激、内皮功能不全等病理生理过程[8,9]。基于此,LOX-1的高表达可能与CSFP的发生发展存在一定关联。LOX-1跨膜的结构域可以被水解为可溶性的sLOX-1,sLOX-1能够反映LOX-1的表达水平[10]。因此,本研究检测CSFP患者的血浆sLOX-1水平,并评价其与CSFP发生发展的关系。
1材料与方法
1.1研究对象
本研究设计为前瞻性的横断面研究,研究对象为2013-05~2015-05在我院住院行冠脉造影的患者,共纳入CSFP患者82例(慢血流组,n=82),另外纳入冠脉造影正常者184例作为对照(对照组,n=184)。CSPF定义为任一冠脉主支血管心肌梗死溶栓治疗(thrombolysis in myocardial infarction,TIMI)血流帧数(TIMI frame count,TFC)>27[11]。主要排除标准:①急性冠脉综合征;②心脏节律异常如心房颤动及病态窦房结综合征;③其他器质性心脏病,如心肌病、严重的心瓣膜病、先天性心脏病或严重的心功能不全;④2型糖尿病;⑤严重的肝肾功能障碍;⑥恶性肿瘤。所有入选者(包括慢血流组及对照组)在行冠脉造影之前均按照临床常规给予双联抗血小板、他汀稳定斑块等治疗。
1.2研究方法
1.2.1冠脉造影按照常规方法行冠脉造影术,按照Gibson等[12]提供的方法计算主支冠脉血管的TIMI-TFC,将前降支血管的TFC除以1.7以校正其长度[9],将前降支(校正后)、回旋支、右冠的TFC加起来除以3取均值,即得到平均TFC。
1.2.2血生化检测所有研究对象均采集清晨静脉血10 ml,各常规血生化指标如空腹血糖(FBG)、总胆固醇(TC)、甘油三酯(TG)、低密度脂蛋白胆固醇(LDL-C)、高密度脂蛋白(HDL-C)由Hitachi 7600全自动生化分析仪检测。使用Abbott ci8200全自动分析仪测量超敏C反应蛋白(Hs-CRP)。采用酶联免疫吸附法(ELISA)法检测各组的sLOX-1水平,试剂盒购自美国Cloud-Clone公司,各组血清标本的吸光光度值由BIO-RAD680酶标仪检测。
1.3统计分析
采用Kolmogorov-Smirnov检验检测数据分布的正态性。正态分布的数据采用均数±标准差表示,两组比较采用t检验;非正态分布的数据采用中位数(四分位差)表示,两两比较采用Mann-WhitneyU检验;计数资料用百分率表示,两两比较采用秩和检验。采用多因素Logistic逐步回归法评价其与存在CSFP的独立相关性。采用Spearman相关分析评价血浆sLOX-1水平与平均TFC的相关性。所有统计分析均采用SPSS17.0软件进行。双侧检验P﹤0.05为差异有统计学意义。
2结果
2.1基本临床资料
除慢血流组的Hs-CRP 水平及TIMI-TFC均较对照组显著升高外,其余各基线临床资料两组间差异无统计学意义(见表1)。
表1两组患者的基本临床特征及冠脉造影结果
Table 1Baseline characteristics and angiographic findings

组别n年龄(岁)男性[例(%)]吸烟[例(%)]BMI(kg/m2)收缩压(mmHg)舒张压(mmHg)FBG(mmol/L)TC(mmol/L)对照组18456(50-63)112(60.87)79(42.93)25.27(23.98-26.25)131.65±16.6981.85±10.615.49±0.734.48±1.07慢血流组8255(50-65)53(64.63)41(50.00)25.30(24.37-26.42)133.10±17.2383.18±11.045.50±0.884.47±1.07检验统计量-0.1300.3411.143-0.543-0.648-0.936-0.0900.054 P 0.8970.5590.285 0.587 0.517 0.350 0.9280.957
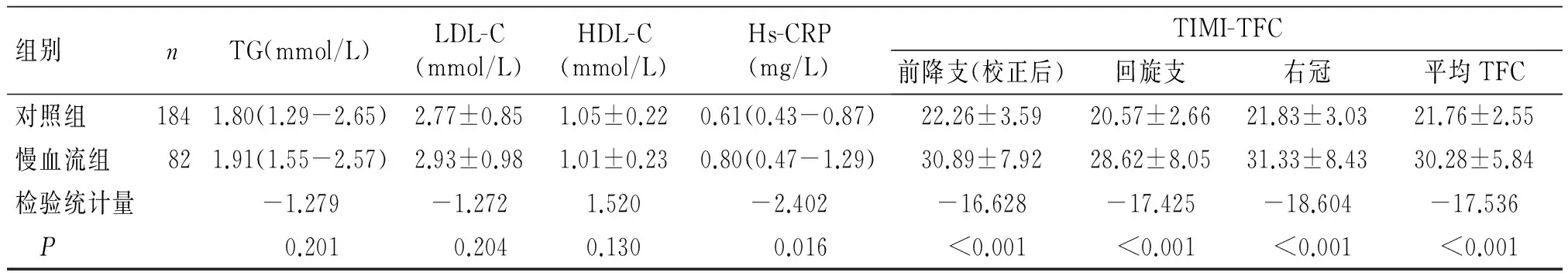
组别nTG(mmol/L)LDL-C(mmol/L)HDL-C(mmol/L)Hs-CRP(mg/L)TIMI-TFC前降支(校正后)回旋支右冠平均TFC对照组1841.80(1.29-2.65)2.77±0.851.05±0.220.61(0.43-0.87)22.26±3.5920.57±2.6621.83±3.0321.76±2.55慢血流组821.91(1.55-2.57)2.93±0.981.01±0.230.80(0.47-1.29)30.89±7.9228.62±8.0531.33±8.4330.28±5.84检验统计量-1.279-1.2721.520-2.402-16.628-17.425-18.604-17.536 P0.2010.2040.1300.016﹤0.001﹤0.001﹤0.001﹤0.001
BMI:体质量指数;FBG:空腹血糖;TC:总胆固醇;TG:甘油三酯;LDL-C:低密度脂蛋白胆固醇;HDL-C:高密度脂蛋白胆固醇;Hs-CRP:超敏C-反应蛋白;TIMI-TFC:血管心肌梗死溶治疗血流帧数;与对照组相比,*P﹤0.05
2.2血浆sLOX-1水平
慢血流组患者血浆sLOX-1水平较对照组显著升高,差异有统计学意义[0.94(0.48-1.30)ng/mlvs0.47(0.39-0.86)ng/ml,P﹤0.001]。
2.3各变量与合并慢血流的独立相关性
将各变量纳入多因素Logistic逐步回归分析,结果显示,血浆sLOX-1水平是存在CSFP的独立危险因子(优势比2.044,95% CI 1.274-3.279;P=0.003,见表2)。
表2多元Logistic回归分析评价CSFP的独立危险因子
Table 2Multiple Logistic regression analysis for the independent predictor of CSFP

变量BSEWalsOR95%CIP年龄0.0030.0150.0511.0030.974-1.0340.822男性0.0460.3160.0211.0470.563-1.9460.884吸烟-0.3020.3040.9870.7390.407-1.3420.321BMI0.0340.0640.2871.0350.913-1.11720.592收缩压0.0050.0110.2041.0050.983-1.0270.652舒张压0.0070.0170.1701.0070.973-1.0420.680FBG0.0480.1840.0691.0490.732-1.5050.793TC-0.0510.1390.1320.9510.723-1.2490.716TG0.1310.1620.6591.1410.830-1.5670.417LDL-c0.2040.1621.5831.2260.893-1.6830.208HDL-c-0.9360.6452.1080.3920.111-1.3880.147Hs-CRP0.0700.0591.4121.0720.956-1.2030.235sLOX-10.7150.2418.7802.0441.274-3.2790.003
2.4血浆sLOX-1水平与平均TFC的相关性
在CSFP患者中,我们进一步评价了血浆sLOX-1水平与平均TFC的关系,Spearman相关分析结果显示,血浆sLOX-1水平与平均TFC的关系呈显著正相关(rs=0.315,P=0.004,见图1)。
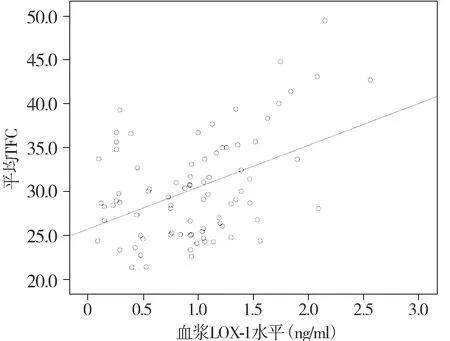
图1 患者血浆sLOX-1水平与平均TFC的相关性Figure 1 Correlation between plasma sLOX-1 levels and mean-TFC
3讨论
随着冠脉介入技术的普及,临床上观察到的CSFP越来越多,因为CSFP与患者的预后存在一定的关联[4,5],其受到的重视程度也越来越高,早期预测CSFP发生的风险对于降低与其相关的各种临床不良事件的发生率具有重要意义。而无创、简便快捷的生物学标记物检测在疾病的风险评估和危险分层方面发挥着越来越重要的作用。
LOX-1是由ox-LDL受体1(OLR1)基因编码的Ⅱ型糖蛋白,与大多数糖蛋白一样,LOX-1可以通过其特有的结构域特异性地结合下游的活性分子,广泛参与机体的病理生理过程。LOX-1的主要配体有AGEs、CRP等,LOX-1与其配体结合后,通过激活多条信号转导通路,会加重冠脉内皮细胞损伤,并促进平滑肌细胞和巨噬细胞吞噬脂质,并转化为泡沫细胞[13-15]。另外,LOX-1能诱导各种黏附分子和炎症因子的表达,促进单核细胞和淋巴细胞的黏附聚集[16-18]。上述病理生理过程与CSFP的发生密切相关。
LOX-1位于细胞外的结构域可以被水解成sLOX-1并释放入血,使其具备了成为血生物标记物的基本条件。本研究首先发现,CSFP的血浆sLOX-1水平较对照者显著升高,这初步表明血浆sLOX-1水平越高者在冠脉造影过程中出现CSFP的可能性就越大。在进一步的多元Logistic回归分析中发现,在排除了混杂因素干扰后,血清sLOX-1水平与CSPF存在具有独立正相关的趋势,这一结果表明高血浆sLOX-1水平是CSFP发生的独立危险因子。因两组患者在基线临床资料方面的不一致性,我们进一步进行了多项二元Logistic回归分析,结果表明,在排除了各种混杂因素干扰后,高血清sLOX-1水平是CSFP发生的独立危险因子。因临床实践中常用平均TFC来评价CSFP的严重程度,我们进一步在CSFP患者中评价了血浆sLOX-1水平与平均TFC的相关性,研究结果显示,血浆sLOX-1水平与CSFP患者的冠脉平均TFC呈正相关,这一研究结果表明,血浆sLOX-1水平也能反映CSFP的严重程度。
总之,我们发现血浆sLOX-1水平与CSFP的发生及严重程度存在独立正相关,sLOX-1有望成为预测CSFP风险并对其进行危险分层的重要的生物标记物。然而,本研究是一个小样本量的横断面研究,在将本研究结论应用于临床实践之前,研究结论尚需要大样本的前瞻性研究来证实。
参考文献:
[1]Tambe AA,Demany MA,Zimmerman HA,etal. Angina pectoris and slow flow velocity of dye in coronary arteries-a new angiographic finding[J].Am Heart J,1972,84(1):66-71.
[2]Beltrame JF,Limaye SB,Horowitz J.The coronary slow flow phenomenon-a new coronary microvascular disorder[J].Cardiology,2002,97(4):197-202.
[3]Beltrame JF,Turner SP,Leslie SL,etal.The angiographic and clinical benefits of mibefradil in the coronary slow flow phenomenon[J].J Am Coll Cardiol,2004,44(1):57-62.
[4]Hawkins BM,Stavrakis S,Rousan TA,etal.Coronary slow flow-prevalence and clinical correlations[J].Circ J,2012,76(4):936-942.
[5]Demir B,Caglar IM,Tureli HO,etal.Coronary slow flow phenomenon associated with high serum levels of soluble CD40 ligand and urotensin Ⅱ:a multi-marker approach[J].Clin Lab,2014,60(11):1909-1920.
[6]Beltrame JF,Cutri N,Kopetz V,etal.The role of nitric oxide in the coronary slow flow phenomenon[J].Coron Artery Dis,2014,25(3):187-189.
[7]Yoshida H,Kondratenko N,Green S,etal.Identification of the lectin-like receptor for oxidized low-density lipoprotein in human macrophages and its potential role as a scavenger receptor[J].Biochem J,1998,334(Pt1):9-13.
[8]Navarra T,Del Turco S,Berti S,etal.The lectin-like oxidized low-density lipoprotein receptor-1 and its soluble form:cardiovascular implications[J].J Atheroscler Thromb,2010,17(4):317-331.
[9]Yan M,Mehta JL,Zhang W,etal.LOX-1,oxidative stress and inflammation:a novel mechanism for diabetic cardiovascular complications[J].Cardiovasc Drugs Ther,2011,25(5):451-459.
[10]Brinkley TE,Kume N,Mitsuoka H,etal.Variation in the human lectin-like oxidized low-density lipoprotein receptor 1(LOX-1)gene is associated with plasma soluble LOX-1 levels[J].Exp Physiol,2008,93(9):1085-1090.
[11]韩伟,任引刚,张利华.血清endocan水平与冠脉慢血流现象的相关性[J].山西医科大学学报,2015,46(11):1061-1064.
[12]Gibson CM,Cannon CP,Daley W,etal.TIMI frame count:a quantitative method of assessing coronary artery flow[J].Circulation,1996,93(5):879-888.
[13]Zhao ZW,Zhu XL,Luo YK,etal.Circulating soluble lectin-like oxidized low-density lipoprotein receptor-1 levels are associated with angiographic coronary lesion complexity in patients with coronary artery disease[J].Clin Cardiol,2011,34(3):172-177.
[14]Kobayashi N,Hata N,Kume N,etal.Soluble lectin-like oxidized low-density lipoprotein receptor-1 as an early biomarker for ST elevation myocardial infarction:time-dependent comparison with other biomarkers:time-dependent comparison with other biomarkers[J].Circ J,2011,75(6):1433-1439.
[15]Chistiakov DA,Orekhov AN,Bobryshev YV.LOX-1-Mediated Effects on Vascular Cells in Atherosclerosis[J].Cell Physiol Biochem,2016,38(5):1851-1859.
[16]Li B,Zhang LH,Yang XG,etal.Postprocedural serum sLOX-1 levels are associated with coronary in-stent restenosis in patients with stable coronary artery disease[J].Coron Artery Dis,2011,22(4):259-263.
[17]Zhao XQ,Zhang MW,Wang F,etal.CRP enhances soluble LOX-1 release from macrophages by activating TNF-α converting enzyme[J].J Lipid Res,2011,52(5):923-933.
[18]Chistiakov DA,Bobryshev YV,Orekhov AN.Macrophage-mediated cholesterol handling in atherosclerosis[J].J Cell Mol Med,2016,20(1):17-28.
作者简介:任引刚,男,1978-03生,本科,主治医师,E-mail:sxrenyingang@163.com
收稿日期:2016-03-16
中图分类号:R541.4
文献标志码:A
文章编号:1007-6611(2016)07-0589-04
DOI:10.13753/j.issn.1007-6611.2016.07.002
Correlation between plasma sLOX-1 levels and coronary slow flow phenomenon
REN Yingang1, LIU Jun1, REN Yiran1, ZHANG Xin1, HAN Wei2, CHU Yi2, LI Hongzeng1*
(1DepartmentofGeriatrics,TangduHospital,FourthMilitaryMedicalUniversity,Xi’an710038,China;2DepartmentofCardiology,TangduHospital,FourthMilitaryMedicalUniversity;*Correspondingauthor,E-mail:tangduzhaoly@126.com)
Abstract:ObjectiveTo explore the correlation between plasma sLOX-1 levels and coronary slow flow phenomenon(CSFP).MethodsEighty-two patients with CSFP and 184 controls with normal coronary flow were enrolled. Plasma sLOX-1 levels were determined by enzyme-linked immunosorbent assay(ELISA) and compared between the two groups. Coronary flow rate was assessed by thrombolysis in myocardial infarction(TIMI) frame count (TFC). Multivariate Logistic regression was used to analyze the independent association between plasma sLOX-1 levels and CSFP. Spearman correlation coefficient was performed to assess the correlation between plasma sLOX-1 levels and mean-TFC.ResultsPlasma sLOX-1 levels in CSFP group were significantly higher than those in control group[0.94(0.48-1.30) ng/ml vs 0.47 (0.39-0.86)ng/ml, P﹤0.001]. Multivariate Logistic regression analysis demonstrated that sLOX-1 was the independent predictor of CSFP(odds ratio 2.044, 95% CI 1.274-3.279; P=0.003). Spearman correlation analysis revealed that plasma sLOX-1 level was positively correlated with mean-TFC (r=0.311,P=0.004). ConclusionThe plasma sLOX-1 levels is independently associated with the presence and severity of CSFP, suggesting that sLOX-1 might be a potential biomarker for CSFP prediction and risk stratification.
Key words:cardiovascular disease;coronary slow flow phenomenon;sLOX-1;biomarker