Hepatocellular Carcinoma with Hypersplenic Thrombocytopenia and Situs Inversus Totalis: A Case Report
Jian-bo Xu, Gang Xu, Guo-feng Chen, Dian-hua Gu, Jian-huai Zhang, and Fu-zhen Qi*Department of General Surgery, Huai’an First People’s Hospital, Nanjing Medical University, Huai’an, Jiangsu 223300, China
Hepatocellular Carcinoma with Hypersplenic Thrombocytopenia and Situs Inversus Totalis: A Case Report
Jian-bo Xu, Gang Xu, Guo-feng Chen, Dian-hua Gu, Jian-huai Zhang, and Fu-zhen Qi*
Department of General Surgery, Huai’an First People’s Hospital, Nanjing Medical University, Huai’an, Jiangsu 223300, China
situs inversus totalis; heoatocellular carcinoma; hyoersolenic thrombocytooenia
Chin Med Sci J 2016; 31(2):134-136
S ITUS inversus totalis (SIT) is a complete mirror image of the thoracic and abdominal viscera,occurring at an incidence of 1 in 5000-20 000 live births.1, 2It is supposed to originate from an abnormal rotation of the cardiac tube during embryogenesis. Although SIT is a congenital anomaly, most of patients are detected accidentally at the time of radiological investigation. Hepatocellular carcinoma (HCC) is usually associated with liver cirrhosis and portal hypertension in Chinese. Presence of hypersplenic thrombocytopenia is a common consequence of long-term portal hypertension in cirrhotic patients. We report a case of HCC with hypersplenic thrombocytopenia, which was successfully treated by splenectomy and liver resection.
CASE DESCRIPTION
A 45-year-old man with epigastric pain was admitted to our hospital in November 2009 for the treatment of suspected HCC in the left lobe of the liver. He had presented with epigastrium unwell for nearly one month. There was no prior history of diabetes, hypertension,abdominal surgery or trauma. Physical examination showed no generalized lymphadenopathy existed. He did not present with symptoms of fever and jaundice. The apex beat was in the right fifth intercostal space, midclavicular line within 2 cm. Nothing abnormal was found in heart auscultation and the respiratory system. The abdomen was soft with little tenderness, but no rebound tenderness. The liver was enlarged with its edge 2 cm below xiphoid. The spleen was 7 cm below the right costal margin with hard texture. Nervous system did not show dysfunction.
The laboratory findings showed hemoglobin of 14.8×103kg/L, white blood cells of 2.84×103/mm3, and blood platelets of 35×103/mm3. Serum alanine aminotransferase, serum aspartate aminotransferase, serum bilirubin,and total protein were all within normal limits. Hepatitis B surface antigen (HBsAg), hepatitis B e antigen (HBeAg),and hepatitis B core antibody (HBcAb) tests were positive and serum α-fetoprotein (AFP) was elevated to 400 ng/ml. Magnetic resonance imaging presented a distinct liver tumor with about 7 cm in diameter as well as an enlarged spleen (Fig. 1).
The patient was operated under general anesthesia with inverted L subcostal incision and the diagnosis of SIT was confirmed at laparotomy. The liver showed micronodular cirrhosis and a mass in segment 2 and 3. The size of spleen was about 17 cm×13 cm×6 cm. So we conducted the liver resection and a concomitant splenectomy (Fig. 2). The surgery was uncomplicated with a blood loss of 300 ml and an operation time of 3 hours and 20 minutes. No blood product transfusion was required. Histologic examination of the specimen showed HCC and chronic congestive splenomegaly (Fig. 3). The postoperative course was uneventful. The patient was doing well without recurrence for 3 years after the operation and symptoms of splenomegaly and hypersplenism were obviously relieved.
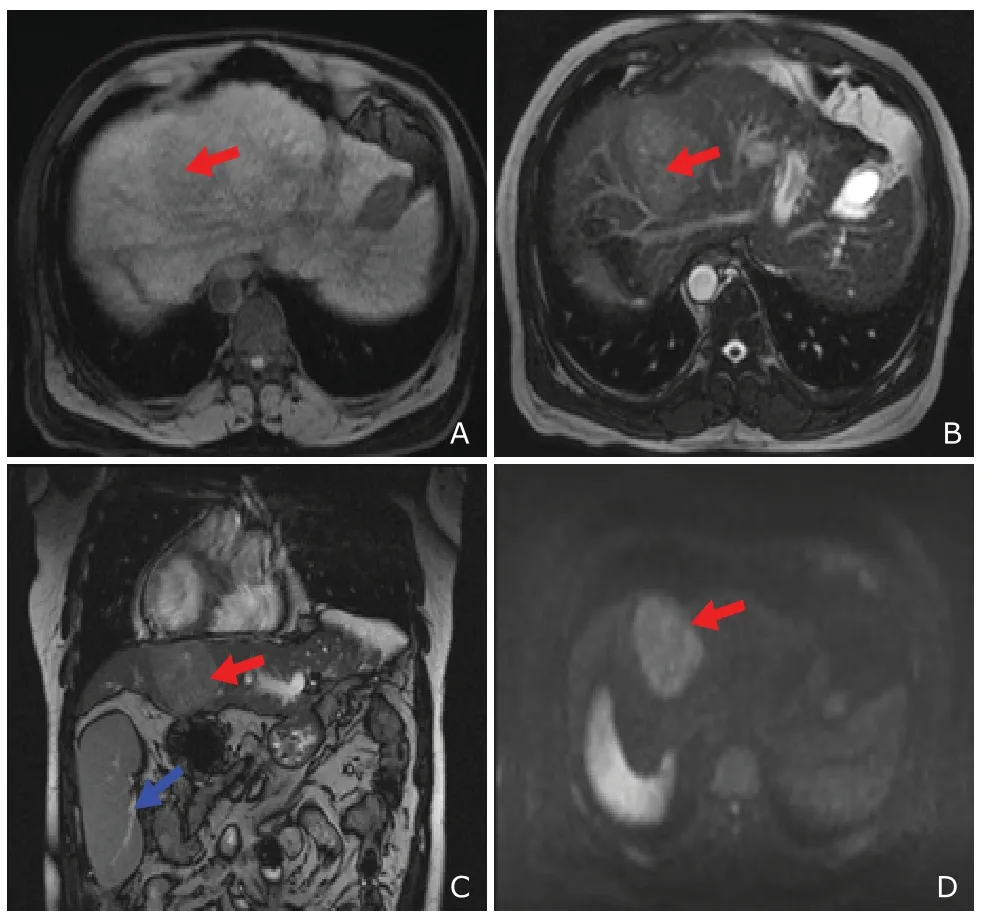
Figure 1. Magnetic resonance imaging of abdomen: a liver tumor (red arrow) and an enlarged (blue arrow)spleen with situs inversus totalis. A. T1-weighted image; B. T2-weighted image; C. cross-sectional coronal image; D. diffusion weighted image.
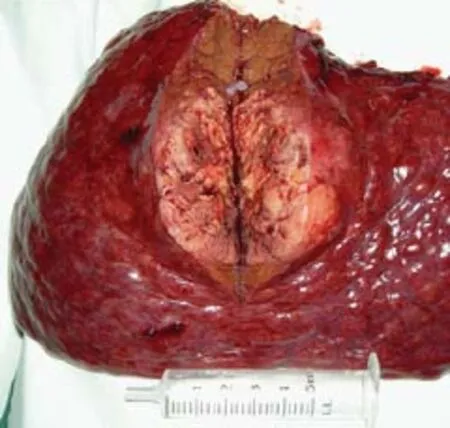
Figure 2. The open resected specimen with liver tumor.
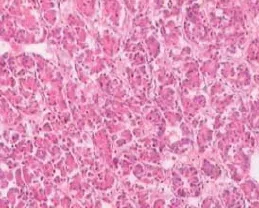
Figure 3. Postoperative pathology confirms hepatocellular carcinoma. HE staining, ×100
DISCUSSION
SIT is a rare congenital condition, in which there is a mirror-image transposition of both the abdominal and thoracic viscera. In 1600, the first case of situs inversus in humans was reported.3Most of patients with SIT are detected accidentally at the time of radiological investigation, however, about 20% to 25% of patients present with Kartagener’s syndrome4and 3% to 5% of patients have congenital heart disease.5Currently, no evidence shows that situs inversus patients have an increased risk of malignancy.6
Chronic hepatitis B virus and hepatitis C virus infection are the most common risk factors of HCC. More than one hundred million chronic hepatitis B patients live in China.7, 8HCC is usually associated with liver cirrhosis and portal hypertension. The platelet count of this patient was less than 50×103/mm3caused by secondary hypersplenism. Splenectomy is suggested for the treatment of secondary hypersplenism and thrombocytopenia.9Although splenectomy may induce thrombosis, liver failure, subsequent mortality,and high operative risk,10the results of most reports11-13conducted that concomitant splenectomy in liver resection for HCC patients was encouraging. According to the Glasgow prognostic score for the operability of hepatectomy,14, 15we considered a concomitant splenectomy was possible in our case.
In 1983, Kanematsu et al16described the first case of a primary HCC associated with situs inversus and only 4 papers of HCC patients with SIT have been reported in Pubmed from 2000.17-20Transcatheter arterial embolization was performed in a HCC patient with SIT by Niki et al17in 2004. Kakinuma et al18reported a case of HCC with SIT treated by hepatectomy. Li et al19carried out transhepatic arterial chemotherapy and embolization in a HCC patient with SIT and polysplenia syndrome. Patel et al20performed a right hepatectomy with the help of electrocautery in aHCC patient with SIT. Our patient is the first reported case of HCC with SIT who underwent liver resection and splenectomy.
In our opinion, precise preoperative anatomical evaluation and good adaptation to the mirror-image anatomy are essential for successful treatment. Reversing the positions of the operator and the assistant during surgery may be a good way, however, careful and cautious assessment of abnormalities by preoperative examinations play a key way to the surgery. Hepatic resection and concomitant splenectomy in patients with SIT are recommended as long as liver function within the safe range for surgery.
REFERENCES
1. Murakami S, Terakado M, Misumi M, et al. Situs inversus totalis with malignant lymphoma of the stomach: report of a case. Surg Today 2003; 33:533-6.
2. Varano NR, Merklin RJ. Situs inversus: review of the literature, report of four cases and analysis of the clinical implications. J Int Coll Surg 1960; 33:131-48.
3. Yaghan RJ, Gharaibeh KI, Hammori S. Feasibility of laparoscopic cholecystectomy in situs inversus. J Laparoendosc Adv Surg Tech A 2001; 11:233-7.
4. Douard R, Feldman A, Bargy F, et al. Anomalies of lateralization in man: a case of total situs inversus. Surg Radiol Anat 2000; 22:293-7.
5. Fulcher AS, Turner MA. Abdominal manifestations of situs anomalies in adults. Radiographics 2002; 22:1439-56.
6. Adler HL, Lerner SP. Renal cell carcinoma and situs inversus viscerum. J Urol 1998; 160:2141-2.
7. Soerjomataram I, Lortet-Tieulent J, Parkin DM, et al. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet 2012; 380:1840-50.
8. Xu JB, Qi FZ, Xu G, et al. Value of alpha-fetoprotein and clinical characteristics in patients with liver neoplasm. Neoplasma 2014; 61:218-24.
9. Akahoshi T, Tomikawa M, Kawanaka H, et al. Laparoscopic splenectomy with interferon therapy in 100 hepatitis-C-virus-cirrhotic patients with hypersplenism and thrombocytopenia. J Gastroenterol Hepatol 2012;27:286-90.
10. Hanazaki K, Kajikawa S, Adachi W, et al. Portal vein thrombosis may be a fatal complication after synchronous splenectomy in patients with hepatocellular carcinoma and hypersplenism. J Am Coll Surg 2000;191:341-2.
11. Wang C, Li C, Wen TF, et al. Safety of synchronous hepatectomy and splenectomy for patients with hepatocellular carcinoma and hypersplenism. Hepatogastroenterology 2012; 59:526-8.
12. Kim SH, Kim dY, Lim JH, et al. Role of splenectomy in patients with hepatocellular carcinoma and hypersplenism. ANZ J Surg 2013; 83:865-70.
13. Wu CC, Cheng SB, Ho WM, et al. Appraisal of concomitant splenectomy in liver resection for hepatocellular carcinoma in cirrhotic patients with hypersplenic thrombocytopenia. Surgery 2004; 136:660-8.
14. Horino K, Beppu T, Kuroki H, et al. Glasgow Prognostic Score as a useful prognostic factor after hepatectomy for hepatocellular carcinoma. Int J Clin Oncol 2013; 18: 829-38.
15. Nakagawa K, Tanaka K, Nojiri K, et al. The modified Glasgow prognostic score as a predictor of survival after hepatectomy for colorectal liver metastases. Ann Surg Oncol 2014; 21:1711-8.
16. Kanematsu T, Matsumata T, Kohno H, et al. Hepatocellular carcinoma with situs inversus. Cancer 1983;51:549-52.
17. Niki Y, Shiraki K, Enokimura N, et al. Hepatocellular carcinoma associated with situs inversus totalis. J Clin Gastroenterol 2004; 38:382.
18. Kakinuma D, Tajiri T, Yoshida H, et al. A case of hepatocellular carcinoma with situs inversus totalis. J Nippon Med Sch 2004; 71:209-12.
19. Li T, Wang L, Chen RX, et al. Hepatocellular carcinoma with situs inversus totalis and polysplenia syndrome. Liver Int 2007; 27:1430-1.
20. Patel RB, Gupta NR, Vasava NC, et al. Situs inversus totalis (SIT) with hepatocellular carcinoma (HCC): a rare case report and review of 12 other cases. Indian J Surg 2013; 75:424-9.
for publication September 12, 2015.
*Correspondence author E-mail: qi.fuzhen@163.com
 Chinese Medical Sciences Journal2016年2期
Chinese Medical Sciences Journal2016年2期
- Chinese Medical Sciences Journal的其它文章
- Cytomegalovirus and Helicobacter Pylori Co-infection in an Adult with Ménétrier’s Disease: A Case Report
- Trends and Prospects of Stem Cell Research in China△
- Low-dose Simvastatin Increases Skeletal Muscle Sensitivity to Caffeine and Halothane
- Mechanical Strain Regulates Osteoblast Proliferation Through Ca2+-CaMK-CREB Signal Pathway△
- Effect of 4-week Whole Body Vibration on Distal Radius Density△
- Impact of Intraoperative Blood Pressure Control and Temporary Parent Artery Blocking on Prognosis in Cerebral Aneurysms Surgery
