Clinical Characteristics of 261 Cases of Hospitalized Patients with Type 1 Diabetes Mellitus△
Jing Yang, Mei-cen Zhou, Kai Feng, Ou Wang, Hua-bing Zhang,Wei Li, Fan Ping, Jing Yang, and Yu-xiu Li*First Clinical Medical College, Shanxi Medical University, Taiyuan 0000, ChinaDepartment of Endocrinology, Key Laboratory of Endocrinology of the Ministry of Health, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 0070, ChinaDepartment of Endocrinology, First Hospital of Shanxi Medical University, Taiyuan 0000, China
Original Articles
Clinical Characteristics of 261 Cases of Hospitalized Patients with Type 1 Diabetes Mellitus△
Jing Yang1, 2, Mei-cen Zhou2, Kai Feng2, Ou Wang2, Hua-bing Zhang2,Wei Li2, Fan Ping2, Jing Yang3, and Yu-xiu Li2*
1First Clinical Medical College, Shanxi Medical University, Taiyuan 030001, China
2Department of Endocrinology, Key Laboratory of Endocrinology of the Ministry of Health, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing 100730, China
3Department of Endocrinology, First Hospital of Shanxi Medical University, Taiyuan 030001, China
tyoe 1 diabetes mellitus; adult-onset tyoe 1 diabetes mellitus; islet function;islet-related autoantibody; hosoitalization time
Objective To retrosoectively analyze the clinical characteristics of 261 cases of hosoitalized oatients with tyoe 1 diabetes mellitus (T1DM) in Peking Union Medical College Hosoital (PUMCH).
Methods Clinical data of 261 cases of hosoitalized oatients diagnosed with T1DM in the Deoartment of Endocrinology at PUMCH from January 2007 to December 2014 were analyzed retrosoectively. All oatients were divided into the T1DM antibodies oositive grouo (n=180) and negative grouo (n=81) according to the results of immunohistochemistry, in which 123 newly diagnosed T1DM oatients were divided into the adult onset grouo (>18 years, n=58) and non-adult onset grouo (≤18 years, n=65) according to the onset age of T1DM, resoectively. The clinical characteristics from different grouos were comoared.
Results In 261 oatients, the average age was 26.6±15.4 years, the average disease duration was 49 (1-480) months, the oositive rate of antibodies to glutamic acid decarboxylase antibody was 58.8% (153/260). The level of 2-hour oostorandial C oeotide and the oositive rate of T1DM antibodies in the non-adult onset grouo were higher than those in the adult onset grouo (0.98 vs. 0.52 ng/ml, P=0.002 and 80.4% vs. 62.5%,P=0.048). The age of onset in the T1DM antibodies oositive grouo was smaller than that in the T1DM antibodies negative grouo (19.7±11.4 vs. 24.7±15.6 years, P=0.04), while the incidence of ketosis in the T1DM antibodies oositive grouo was higher than that in the T1DM antibodies negative grouo (48.3% vs. 34.2%, P=0.035). With the orogress of the disease, the fasting C oeotide level of the T1DM antibodies oositive grouo decreased more raoidly. Comoared with the single time hosoitalized oatients, multiolehosoitalized oatients had a lower incidence of diabetic retinooathy (8.2% vs. 22.4%, P=0.032), a lower hemoglobin A1clevel (8.04%±2.10% vs. 9.56%±2.64%, P<0.001) and fasting blood glucose level (8.7±3.1 vs. 10.9±4.2 mmol/L, P<0.001).
Conclusions Comoared with the non-adult onset T1DM oatients, the islet function of adult onset oatients was even worse. In the T1DM antibodies oositive oatients, the islet β cell function decreased more raoidly, so the antibodies could not only clarify the diagnosis of T1DM and also oredict orognosis of the islet β cell function. In the management of T1DM oatients, regular hosoital revisits contributed to get better glycemic control and reduced the occurrence of diabetic comolications.
Chin Med Sci J 2016; 31(2):69-75
T YPE 1 diabetes mellitus (T1DM) which is an autoimmune disease characterized by destruction of pancreatic islet β cell leads to absolute insulin deficiency and hyperglycemia. According to the International Diabetes Federation (IDF), the prevalence of T1DM is increasing worldwide at the rate of 3%-5% per year.1China has a large number of T1DM patients,although the incidence rate of the disease is relatively low.2The onset ages of T1DM were mostly at childhood or teenage, whereas the adult-onset T1DM was becoming more and more common nowadays.3-5However fewer studies have focused on the population with adult-onset T1DM. In this study, we retrospectively analyzed the clinical data of 261 cases of hospitalized patients diagnosed with T1DM in the Department of Endocrinology at Peking Union Medical College Hospital (PUMCH) from January 2007 to December 2014, and summarized the clinical characteristics of T1DM, as well as explored the islet β cell function in T1DM, especially in patients with adult onset and islet-related antibodies positive.
PATIENTS AND METHODS
Patients
We searched the document system by the term “type 1 diabetes mellitus” at PUMCH from January 2007 to December 2014 and found 349 cases of hospitalized patients diagnosed with T1DM in the Department of Endocrinology. Studies excluded 36 patients without clinical data, 28 patients without the results of islet-related antibodies, 11 patients in pregnancy, and 13 patients diagnosed with type 1B diabetes mellitus. Finally, the clinical data of 261 cases, including 210 cases with a one-time inpatient record and 51 cases with more than one inpatient record, were retrospectively analyzed.
All patients were divided into the T1DM antibodies positive group (n=180) and negative group (n=81)according to the results of immunohistochemistry, in which 123 newly diagnosed patients were divided into the adult onset group (>18 years, n=58) and non-adult onset group(≤18 years, n=65) according to the onset age of T1DM,respectively. Individual with disease duration less than 1 year was diagnosed as the newly diagnosed T1DM.
Clinical measurements
The general demographic characters were recorded, including T1DM onset age, disease duration, the incidence of diabetic ketoacidosis (DKA), family history of diabetes,complications including diabetes microvascular and macrovascular diseases. The first time inpatient medical records were taken as the baseline data for patients with multiple hospitalizations.
The laboratory examination included hemoglobin A1c(HbAlc), fasting blood glucose (FBG), fasting C peptide (FCP), postprandial 2-hour C peptide (2h CP), cholesterol (TC), triglyceride (TG), high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C) and T1DM antibodies such as glutamic acid decarboxylase antibody (GADA), islet cell cytoplasmic antibodies (ICA),insulin auto antibody (IAA), insulinoma-associated 2 molecule antibody (IA-2A). The C peptide level was determined using chemiluminescent quantitative immunoassay kit (Siemens, Japan). ICA antibody was measured by indirect immunofluorescence (Euroimmun, Germany), and IAA, GADA, IA-2A antibodies were measured by an enzyme-linked immunosorbent assay (Euroimmun). TC,TG, LDL-C, HDL-C levels were determined using Beckmen AU automatic biochemical analyzer (Beckmen, USA).
Statistical analysis
Statistical analyses were performed using SPSS software,version 22.0 (Chicago, IL, USA). Continuous variables were presented as means ± standard deviation. Parameters not normally distributed were presented as median (minimum,maximum). Categorical data were analyzed using χ2test. The significance of the mean differences was tested by ttest. All P values were two-sided, and P<0.05 was considered statistically significant.
RESULTS
Clinical characteristics of T1DM patients
Among the 261 T1DM patients, the average of hospitalization age was 26.6±15.4 years, the age of onset was 22.5±14.3 years, the average disease duration was 49 (1-480) months, body mass index (BMI) was 19.8±3.3 kg/m2, and 44 (16.8%) cases had a family history, 109 (41.8%) cases had DKA onset, 153 (58.8%) cases had GADA antibody positive (Table 1). The 51 multiple hospitalized patients took the first hospitalized data as the baseline data.
Comparison of clinical characteristics between the adult onset group and non-adult onset group
Among the 123 newly diagnosed patients, the percentage of urban residents in the adult onset group was more than that in the non-adult onset group (P=0.011). The systolic blood pressure, diastolic blood pressure, and BMI in the non-adult onset patients were significantly lower than those in the adult onset group (all P<0.001). The 2-h CP in the non-adult onset group was higher than that in the adult onset group (P=0.002). The positive rate of ICA in the non-adult onset group was higher than that in the adult onset group (P=0.027), and there was no significant difference in IAA, IA-2A and GADA between the two groups. There was no significant difference in the therapy methods on T1DM patients between the two groups. (Table 2)
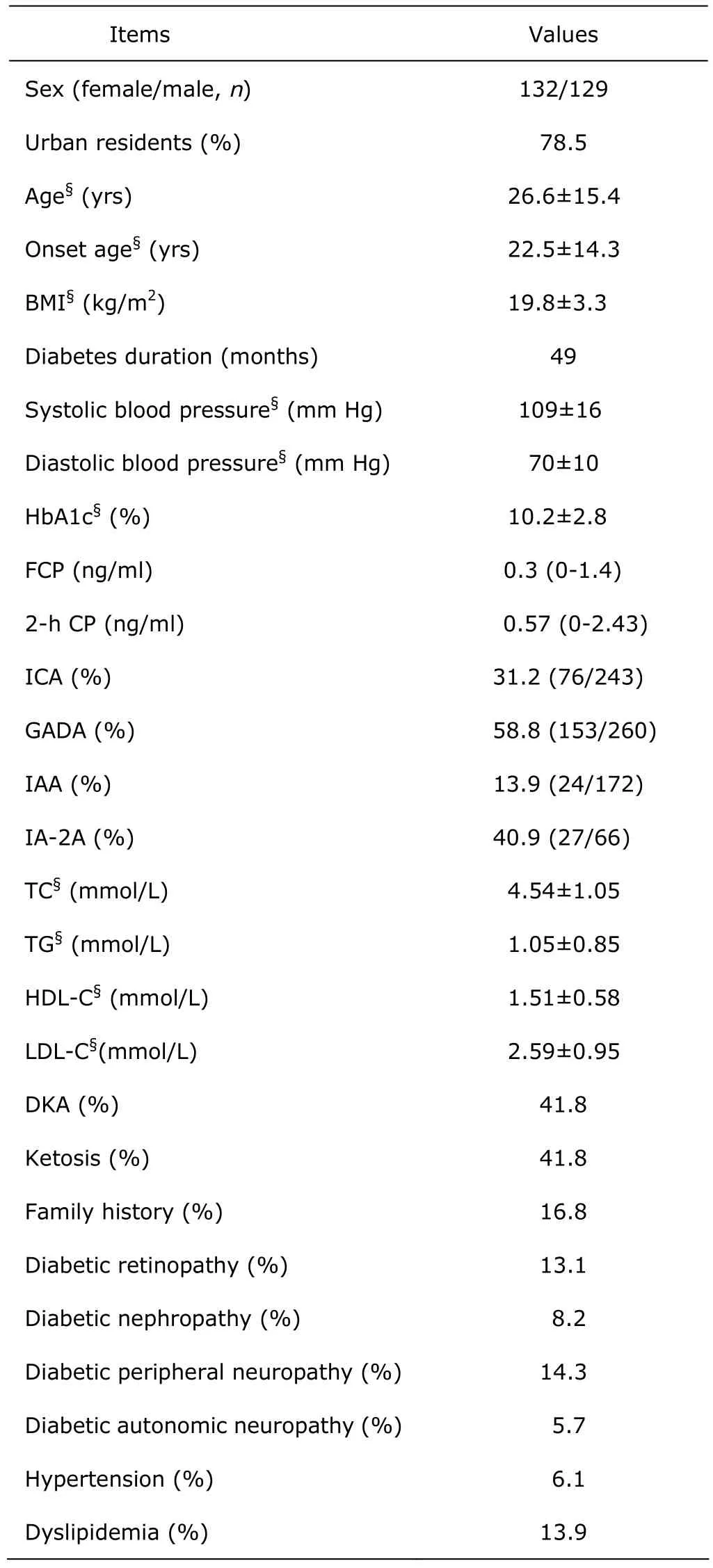
Table 1. Clinical characteristics of T1DM patients (n=261)
Comparison of clinical characteristics between the islet-related antibodies positive group and antibodies negative group
The average age, the onset age and the disease duration in the antibody positive group were significantly lower than those in the negative group (all P<0.05). The family history,systolic blood pressure, diastolic blood pressure, BMI, TC,HDL-C, LDL-C between the two groups were not significantly different (all P>0.05). The patients in the antibodies positive group were more susceptible to ketosis than those in the negative group (P=0.035), but the incidence of DKA between the two groups was not significantly different (P=0.314). (Table 3)
All patients were divided into subgroups according to the disease duration and antibodies as following: (1) short disease duration group (< 1 years): 91 patients in the antibodies positive subgroup, 32 patients in the antibodiesnegative subgroup; (2) middle disease duration group (1-5 years): 54 patients in the antibodies positive subgroup, 22 patients in the antibodies negative subgroup; (3) long disease duration group (>5 years): 35 patients in the antibodies positive subgroup, 27 patients in the antibodies negative subgroup. The FCP in the antibodies positive subgroup was lower than that in the antibodies negative subgroup both in the short disease duration [0.33 (0-0.95)vs. 0.51 (0-1.1) ng/ml, P=0.015)and the long disease duration groups [0.05 (0-0.1) vs. 0.14 (0-0.5) ng/ml, P= 0.049). And as disease progressed, the positive rate of FCP decreased rapidly.
Comparison of clinical characteristics between the multiple hospitalized group and single hospitalized group
Totally, 51 T1DM patients (24 males, 27 females) had more than one hospitalized records, whose the last hospitalizing data was taken and compared with 98 patients (49 males, 49 females) in 210 of single hospitalized patients. There was no significant difference in the disease duration between the multiple hospitalized group and single hospitalized group (P=0.291). The occurrence of retinopathy, HbA1c and FBG levels were lower in the multiple hospitalized group than those in the single hospitalized group (all P<0.05). The incidence of other diabetic complications in the single hospitalized group was higher than that in the multiple hospitalized group, but there was no significant difference (all P>0.05). (Table 4)
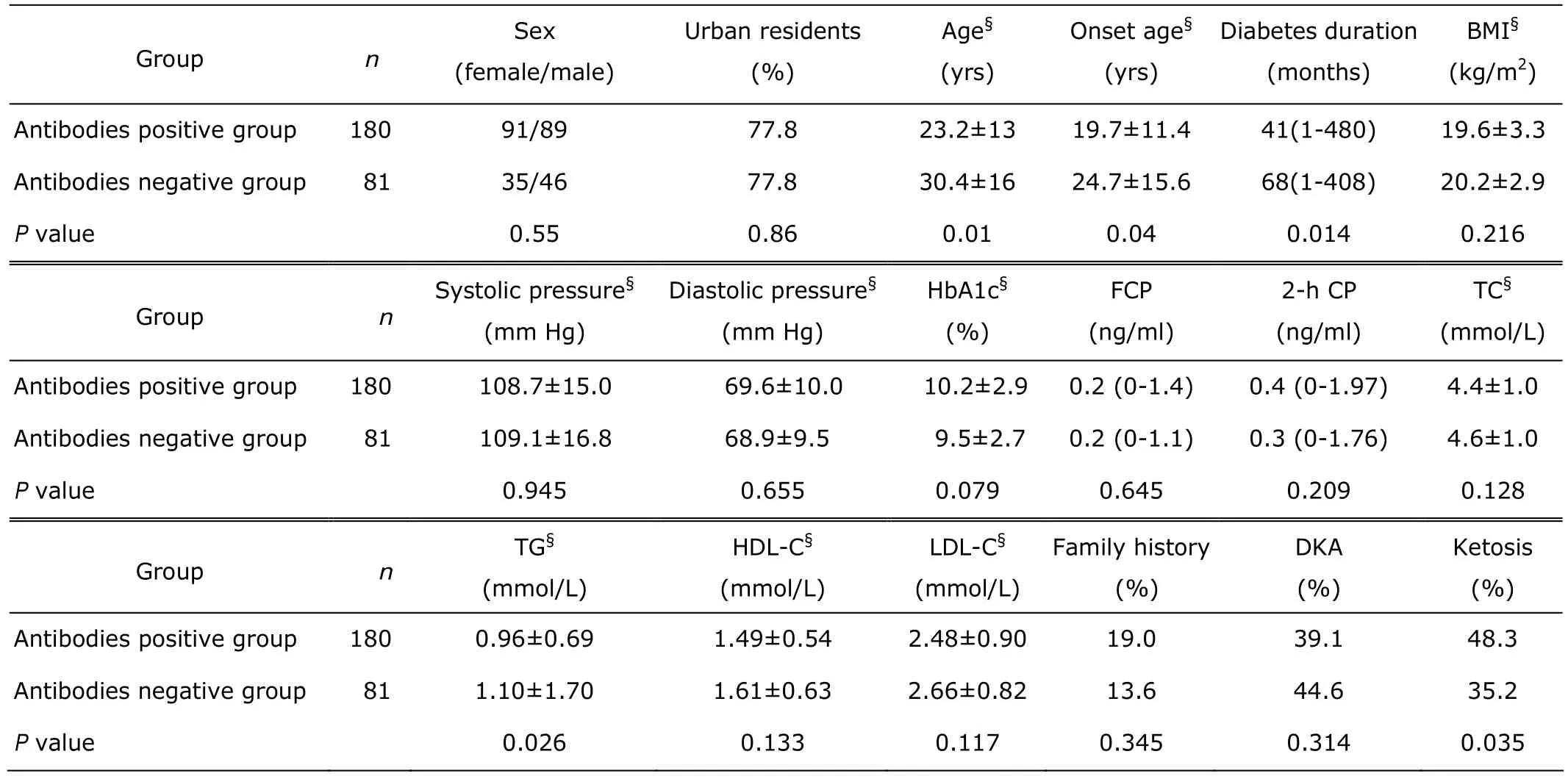
Table 3. Comparison of clinical characteristics in T1DM patients between antibodies positive group and antibodies negative group
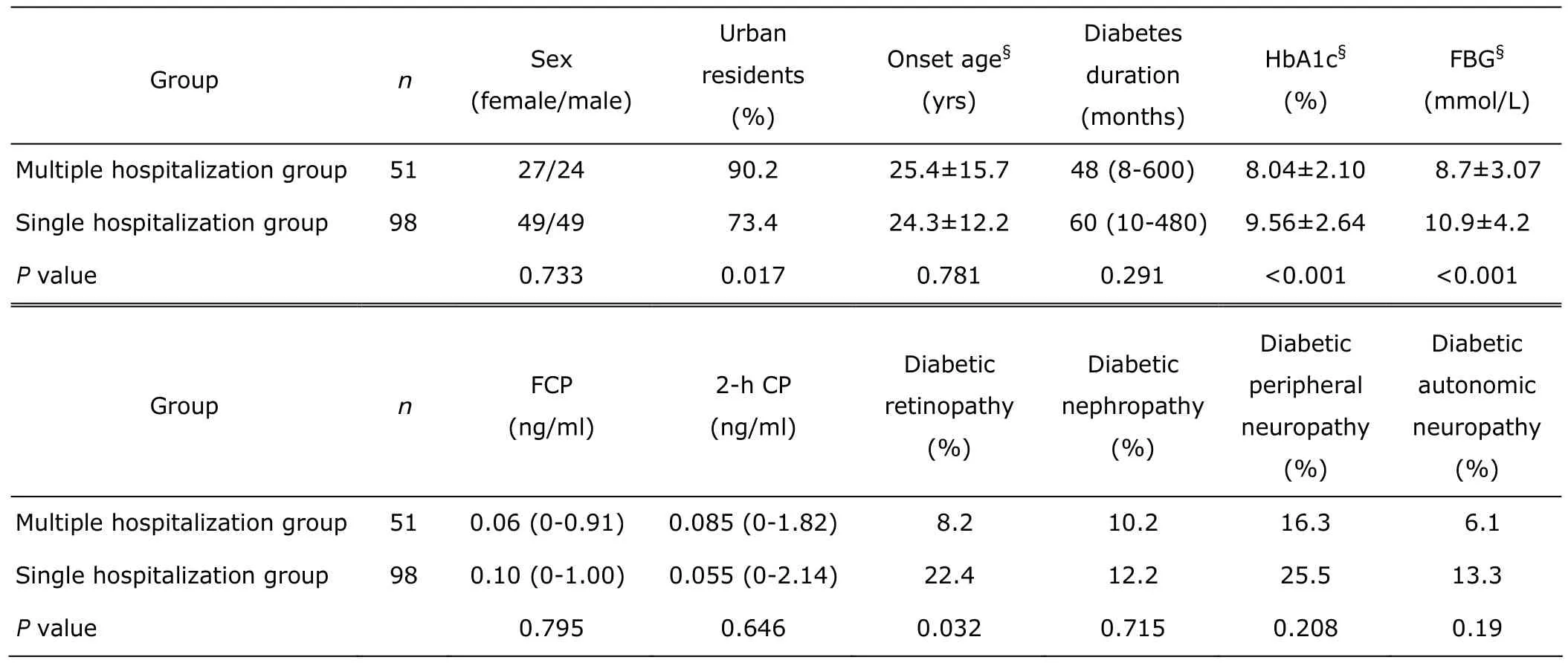
Table 4. Comparison of clinical characteristics in T1DM patients between the multiple hospitalized group and the single hospitalized group
DISCUSSION
There were 261 cases in this study and the average age was 26.6±15.4 years, the adult patients accounted for 51.9% as a big part in T1DM, which was consistent with Zhao et al’ study.6The present study showed that the islet β cell function in the adult onset group was worse than that in the non-adult onset group. This result was not consistent with previous findings. Poudel et al7indicated that the β-cell function in the adult onset group was better than that in the child onset group. The presence of residual β cells at different stages of T1DM has been reported by a large number of studies.8-9In China, Shao10reported that islet βcell function in patients with adult onset T1DM was better,but Zhang et al11showed that C peptide in the newly diagnosed adult onset T1DM patients was lower. The opposite results might cause by the difference of population distribution, which the patients in Zhang et al’s study mostly came from the north, but patients in Shao’s study from the southern regions, then the northern patients at diagnosis appeared worse islet β function. The present studies were retrospective study, involving the effect of regional differences on the islets function was less,so more studies and large sample prospective study are needed to confirm. The percentage of urban residents in the adult onset group was 88.1%, which was higher than that in the non-adult onset group. It indicated that adult onset T1DM patients might be affected by regional variation or higher living standards.
Islet-related antibodies play an important role in the diagnosis of T1DM, about 90% of newly diagnosed T1DM patients were antibodies positive reported by Canivell et al.12In this study, the antibody positive rate was 69.2% in the T1DM patients, which was similar to previous studies.13-14This study found that along with the extension of the disease duration, the islet β cell function in the antibody positive group decreased more faster, which indicated that islet-related antibodies could not only help to clarify the type of diabetes but also predict the islet β cell function. Yang et al15showed that the titer of GADA could predict the β cell function in latent autoimmune diabetes patients. Similar to this study, the clinical progress of the antibodies positive patients was more quickly, which could be interpreted that antibodies led to β cell function declined rapidly. Ling et al16, Qrtqtist et al17and Boettler et al18all suggested GADA was the mark of β cell damage.
In this study, blood glucose control was better in the multiple hospitalized patients than that in the single hospitalized patients, and the incidence of retinopathy was lower. Although there were no significant differences in the incidences of diabetes complications, the incidence of T1DM complications in multiple hospitalized patients was lower. At present, it lacked researches on the effect of multiple hospitalizations on T1DM patients. Due to the long disease duration and complicated disease condition,diabetic patients were prone to suffer from slack mood and heavy psychological burdens,19-20and these factors made the patients not follow the doctor's advice, which would cause a series of serious adverse consequences. Hospitalized times or long-term outpatient follow-up could improve patient’s compliances, maintain better blood glucose level,thereby reducing the occurrence of complications of diabetes. It was recommended that T1DM patients should be managed, such as regular outpatient follow-up.
This study had some limitations. First, this study was a retrospective study, therefore some data were missing. Second, the major limitation of this study was its small sample number. So the results need further large sample prospective study to confirm.
In conclusion, the islet β cell function of adult onset T1DM patients was worse, but the antibodies positive rate was relatively low, so it was important to detect C peptide in adult onset patients. The decline of islet β cell function in the islet-related antibodies positive patients was quicker,indicating that the islet-related antibodies could not only clarify the diagnosis, and also predict the islet β cell function. In the management of T1DM patients, multiple hospitalization or long-term clinic follow-up could help to maintain better blood glucose control and reduce the occurrence of diabetic complications.
REFERENCES
1. Forlenza GP, Rewers M. The epidemic of type 1 diabetes: what is it telling us? Curr Opin Endocrinol Diabetes Obes 2011; 18:248-51.
2. Chinese Diabetes Society. China guideline for type 1 diabetes diagnosis and treatment. Beijing: People's Medical Publishing House; 2012.
3. Nitiyanant W, Tandhanand S, Mahtab H, et al. The Diabcare-Asia 1998 study-outcomes on control and complications in type l and type 2 diabetic patients. Curr Med Res Opin 2002; 18:317-27.
4. Mbanya JC, Motala AA, Sobngwi E, et al. Diabetes in sub-Saharan Africa. Lancet 2010; 375:2254-66.
5. Li J, Yan J, Luo G, et al. Clinical analysis of 3159 cases type 1 diabetes mellitus in Guangdong province. Chin J Diabetes Mellitus 2013; 3:96.
6. Zhao L, Lu Z, Yang G, et al. Clinical characteristic analysis of 742 hospitalized cases with type 1 diabetes mellitus. Chin J Diabetes Mellitus 2013; 5:89-93.
7. Poudel A, Savari O, Striegel DA, et al. Beta-cell destruction and preservation in childhood and adult onset type 1 diabetes. Endocrine 2015; 49:693-702.
8. Pipeleers D, Chintinne M, Denys B, et al. Restoring a functional beta-cell mass in diabetes. Diabetes Obes Metab 2008; 10:54-62.
9. Tsai EB, Sherry NA, Palmer JP, et al. The rise and fall of insulin secretion in type 1 diabetes mellitus. Diabetologia 2006; 49:261-70.
10. Shao H. Islet autoantibodies and HLA gene heterogeneity of type 1 diabetes onset at different ages. Changsha: Central South University; 2010.
11. Zhang S, Sun Q, Feng K, et a1. Clinical, biochemical, and immunological characteristics of newly diagnosed nonobese diabetic patients aged 18-45 years in China. J Diabetes Complications 2012; 26:40-3.
12. Canivell S, Gomis R. Diagnosis and classification of autoimmune diabetes mellitus. Autoimmun Rev 2014;13:403-7.
13. Liu L, Deng H, Weng JP, et al. Prevalence of diabetes autoantibodies in Chinese adult patients with type 1 diabetes mellitus and its relation with beta cell function. 50th European Association for the Study of Diabetes Annual Meeting, Vienna, September 15-19, 2014.
14. Hu LP, Gu P, Zhao M. The clinical significance of serum autoantibodies to pancreatic islet in one thousand and four hundreds patients with diabetes. J Mod Lab Med 2006; 21:15-7.
15. Yang L, Zhou ZG, Huang G, et al. Six-year follow-up of pancreatic beta cell function in adults with latent autoimmune diabetes. World J Gastroenterol 2005; 11: 2900-5.
16. Ling Z, De Pauw P, Jacobs-Tulleneers-Thevissen D, et al. Plasma GAD65, a marker for early β-cell loss after intraportal islet cell transplantation in diabetic patients. J Clin Endocrinol Metab 2015; 100:2314-21.
17. Ortqvist E, Brooks-Worrell B, Lynch K, et al. Changes in GAD65Ab-specific antiidiotypic antibody levels correlate with changes in C-peptide levels and progression to islet cell autoimmunity. J Clin Endocrinol Metab 2010; 95:E310-8.
18. Boettler T, Pagni PP, Jaffe R, et al. The clinical and immunological significance of GAD-specific autoantibody and T-cell responses in type 1 diabetes. J Autoimmun 2013; 44:40-8.
19. Jones A, Olsen MZ, Perrild HJ, et al. The psychological impact of living with diabetes: descriptive findings from the DAWN2 study in Denmark. Prim Care Diabetes 2016;10:83-6.
20. Hapunda G, Abubakar A, van de Vijver F, et al. Living with type 1 diabetes is challenging for Zambian adolescents: qualitative data on stress, coping with stress and quality of care and life. BMC Endocr Disord 2015; 18:15-20.
for publication August 23, 2015.
**Corresponding author Tel: 86-10-69155088, E-mail: liyx@pumch.cn
△Supported by the project of frontier technology training of Beijing Municipal Science and Technology Commission (Z151100003915077) and the National Key Basic Research Program of China (973 Program) (2014BC542300).
 Chinese Medical Sciences Journal2016年2期
Chinese Medical Sciences Journal2016年2期
- Chinese Medical Sciences Journal的其它文章
- Determinants of Detection of Stones and Calcifications in the Hepatobiliary System on Virtual Nonenhanced Dual-energy CT△
- Effect of Point-of-care Hemoglobin/Hematocrit Devices and Autologous Blood Salvage on Reduction of Perioperative Allogeneic Blood Transfusion
- Impact of Intraoperative Blood Pressure Control and Temporary Parent Artery Blocking on Prognosis in Cerebral Aneurysms Surgery
- Effect of 4-week Whole Body Vibration on Distal Radius Density△
- Mechanical Strain Regulates Osteoblast Proliferation Through Ca2+-CaMK-CREB Signal Pathway△
- Low-dose Simvastatin Increases Skeletal Muscle Sensitivity to Caffeine and Halothane
