Prevalence of latent eosinophilia among occupational gardeners at Babcock University,Nigeria
Ayodele Olushola Ilesanmi,Ginnikachi Jennifer Ekwe,Rosemary Isioma Ilesanmi,Damilola Temitope Ogundele,Jacob Kehinde Akintunde,Oluwasogo Adewole Olalubi*Department of Medical Laboratory Science,Babcock University,Ilishan-Remo,NigeriaDepartment of Medical Microbiology,Olabisi Onabanjo University,Ago-Iwoye,NigeriaDepartment of Chemical,Geological & Physical Sciences,Chemistry Unit,Kwara State University,Malete,NigeriaDrug Metabolism and Molecular Environmental Toxicology Unit,Biochemistry Option,Department of Bioscience andBiotechnology,College of Pure and Applied Sciences,Kwara State University,Malete,NigeriaSchool of Allied Health & Environmental Sciences,Department of Allied Health,Public Health Unit,Kwara State University,Malete,Nigeria
ABSTRACT
Prevalence of latent eosinophilia among occupational gardeners at Babcock University,Nigeria
Ayodele Olushola Ilesanmi1,Ginnikachi Jennifer Ekwe1,Rosemary Isioma Ilesanmi2,
Damilola Temitope Ogundele3,Jacob Kehinde Akintunde4,Oluwasogo Adewole Olalubi5*1Department of Medical Laboratory Science,Babcock University,Ilishan-Remo,Nigeria
2Department of Medical Microbiology,Olabisi Onabanjo University,Ago-Iwoye,Nigeria
3Department of Chemical,Geological & Physical Sciences,Chemistry Unit,Kwara State University,Malete,Nigeria
4Drug Metabolism and Molecular Environmental Toxicology Unit,Biochemistry Option,Department of Bioscience and
Biotechnology,College of Pure and Applied Sciences,Kwara State University,Malete,Nigeria
5School of Allied Health & Environmental Sciences,Department of Allied Health,Public Health Unit,Kwara State University,Malete,Nigeria
ABSTRACT
Keywords:
Eosinophilia
Occupational
Exposure
Gardeners
Duration
Allergens
ARTICLE INFO
Article history:
Received 21 Aug 2015
Received in revised form 7 Sep,2nd revised form 19 Sep 2015
Accepted 25 Dec 2015
Available online 20 Apr 2016
Original article http://dx.doi.org/10.1016/j.apjtb.2015.12.022
Tel: +234 703 603 9078
E-mail: olalubisogo@gmail.com
The study protocol was performed according to the Helsinki declaration and approved by Babcock and Kwara State Universities Ethical Review Boards. Informed written consent was obtained from subjects.
Foundation Project: Supported by Centre for Community Development,Action Research Grant,Kwara State University,Nigeria(Grant No. KWASUCCD/2014AR/ 1/27).
Peer review under responsibility of Hainan Medical University. The journal implements double-blind peer review practiced by specially invited international editorial board members.
1. Introduction
Allergic reactions are distinctive because of excessive activation of certain white blood cells called basophils and mast cells by a type of antibody called immunoglobulin E(IgE)[1,2]. This reaction results in an inflammatory response ranging from mild to severe cases[2]. Allergies can play a major role in conditions such as asthma. In some individuals,severe allergies from environmental,dietary or medication allergens may result in life-threatening reactions called anaphylaxis[3].
Food allergies and reactions to venom of many stinging insects such as wasps and bees are more often associated with these severe reactions[4,5].
The worst allergens are typically from weeds,grasses,and certain specific trees. Because some of these plants are windpollinated,they produce a lot of powdery,easily inhaled pollen that triggers allergic responses. Insect-pollinated plants,such as flowers and vegetables,have pollens that are large and sticky,which generally might not cause much problem compared to many other allergens such as dust,wool or pollen that are of tiny-sized airborne particles. In these cases,symptoms arise in areas in close contact with air,such as eyes,nose,and lungs[5-7]. For instance,allergic rhinitis,also known as hay fever,causes irritation of the nose,sneezing,itching,and redness of the eyes[5,7]. Inhaled allergens can also lead to asthmatic symptoms,caused by narrowing of the airways(bronchoconstriction),shortness of breath(dyspnoea)and coughing[5]. Substances that come into contact with the skin,such as latex,are also common causes of allergic reactions,known as contact dermatitis or eczema[8,9]. Skin allergies frequently cause rashes,swelling and inflammation within the skin,in what is known as“wheal and flare”reaction[10]. Latex is another substance that can trigger an IgE-mediated cutaneous,respiratory,and systemic reaction. The prevalence of latex allergy in the general population is low,being less than one percent;while the sensitivity among healthcare workers is higher,ranging from seven to ten percent[5]. This has been attributed to the high level of exposure that health workers have to wear latex gloves while carrying out their duties.
Host factors for allergy include heredity,gender,race,and age. Heredity is by far the most significant,although other factors have not been exhaustively investigated. However,there have been recent increases in the incidence of allergic disorders that cannot be explained by genetic factors alone [10,11]. Four major noticeable environmental candidates are alterations in exposure to infectious diseases during early childhood,environmental pollution,allergen levels and dietary changes[5].
One of those occupations that bring about exposure to allergens produced by weeds,grasses and trees is gardening. Gardening is an age-old vocation that has been and is still the occupation of many individuals in developing countries. Not all plants produce allergens,but allergen-producing plants are found sandwiched among other allergen-free plants. Gardeners are frequently exposed to allergens during the process of weeding and trimming plants. Individual gardeners that are repeatedly exposed to these plants may develop allergy which is haematologically characterized as eosinophilia. It is imperative to mention that eosinophilia is not limited to allergic situations only but could also be triggered by the presence of parasites in humans. Recent research has shown that some common parasites,such as intestinal worms(e.g.,hookworms),secrete chemicals into the gut wall and,(hence,the bloodstream)that suppress the immune system and prevent the body from attacking the parasite[12]. Indeed,eosinophilic oesophagitis,common among black children,has been attributed to the effect of allergens[12]. Improved hygienic practices,access to education and constant deworming of school children has now led to a low level of parasitic infestation among many individuals in Nigeria[13]. Thus,high levels of eosinophilia in individuals,particularly people exposed to occupational allergens,may correctly be linked to allergic reactions. In this study,quantitative determination of the level of eosinophils present in the blood and sputum samples of Babcock University gardeners,presumably as a result of occupational exposure to allergens while on duty was carried out.
2. Materials and methods
The study was carried out among gardeners of Babcock University,Ilishan-Remo,Ogun State,Nigeria. Forty four(44)blood samples and 21 sputum samples were collected from the gardeners. Thirteen(13)blood and sputum samples were collected from Babcock University non-gardening staff as reference control.
Inclusion criteria included gardeners who engage in mowing of lawn,flower trimming,weeding,nursing,raking/parking and sweeping,all of whom were males and fall within the age range of 20-59 years. Exclusion criteria included non-gardener University staff and students below the age of 20 years. Gardeners who are already known to be asthma patients and persons with Cushing's syndrome are also excluded.
Subject's consent was verbally sought and obtained with a consent form,before sample collection. Babcock University ethical approval committee gave approval to proceed on the project. Demographic data of the subjects were obtained through a questionnaire and samples were collected from Babcock University gardeners. Sputum and blood samples were obtained from subjects. The sputum samples were meant to complement the blood samples. Blood and sputum sample collection took two weeks. Thirteen subjects served as control samples. These were non-gardener workers of other units in Babcock University who belong to the same age range as the subjects under study.
Four millilitres of venous blood sample was collected from each subject using a sterile disposable needle and syringe and dispensed into an ethylene diamine tetra acetic acid anticoagulated bottle. Samples collected were analysed for total eosinophil count within 6 h. Similarly,sputum samples were collected in a sterile universal bottle and analysed within 6 h.
2.1. Estimation of total eosinophil count using 1% aqueous eosin Y
Whole blood was diluted appropriately using a diluent which consisted of 1%aqueous eosin Y(5 mL),acetone(5 mL),distilled water(90 mL). This diluent lyses the red cells and stains the granules in the eosinophil,but does not stain the other leucocytes. The eosinophils were identified in the Neubauer counting chamber by their bright red stained granules[14].
2.2. Sputum eosinophil count using Giemsa stain
Sputum was stained using Giemsa solution which consisted of eosin-methylene blue(which stains the nuclei blue and cytoplasm pinkish red). Methylene blue chloride and azure 2 eosinate improves the intensity of nuclear staining and capability to resolve selective cellular structures[15].
2.3. Blood eosinophil count
A total volume of 20 μL of blood was added to 380 μL of diluting fluid in a test tube. It was mixed properly and allowed to stand at room temperature for 5 min to allow lysing of red cells. An improved Neubauer counting chamber was assembled and charged with the mixture of blood and diluent. The cells were allowed to settle in the moist chamber for 3 min. Numbers of eosinophils in the four large corner squares of the counting chamber were counted using 40×objective lens. Eosinophils were identified by their bright red stained granules.
The calculation is as following: Total eosinophil count/ mm3= Number of eosinophil counted×1/Area counted (mm2)×1/Depth(mm)×Dilution = Number of eosinophil counted×1/4×1/0.1×20 = Number of eosinophil counted×50/mm3. The normal range is 50-450/mm3for adults[15].
2.4. Sputum differential eosinophil count
Sputum smear was made on a clean grease-free slide. It was allowed to air dry. It was fixed in 95%methanol for 30 min. Giemsa stain(1 mL)was diluted with 9 mL of phosphate buffer (pH 6.8)and poured on the smear for 10 min. It was differentiated in phosphate buffer for 10 s. It was air dried and viewed microscopically with oil immersion objective. A total of 100 leucocytes were counted and the number of eosinophils present was recorded in percentage(%). The normal range is<2.5% [16].
2.5. Statistical analysis
Data obtained from laboratory analysis of 44 blood samples and 21 sputum samples were analysed with SPSS software. Summary of the results were presented in graphical form. A P<0.05 is considered statistically significant.
2.6. Ethical considerations
All aspects of the study were approved by Babcock and Kwara State Universities Ethical Review Boards.
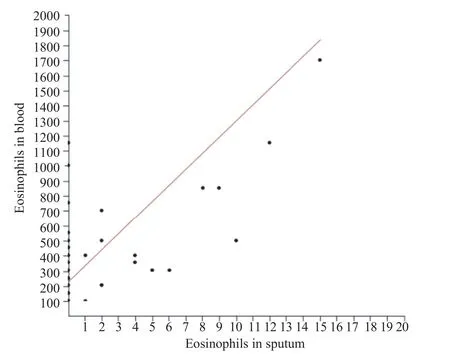
Figure 1. Correlation between eosinophils in sputum and eosinophils in blood among Babcock University gardeners[r = 0.54,F = 17.36,P<0.05 (0.000)].
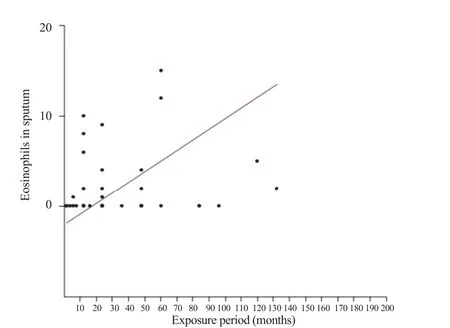
Figure 2. Correlation between eosinophil in sputum and exposure period among Babcock University gardeners[r = 0.15,t = 4.55,P>0.05(0.17)].
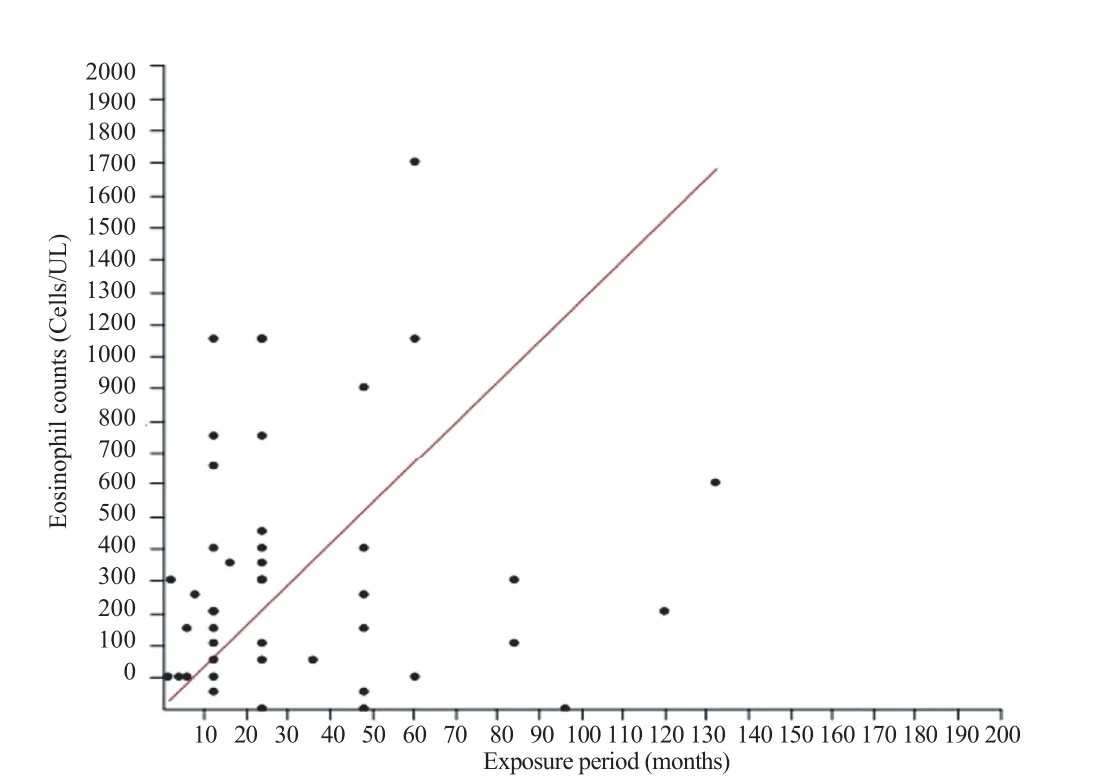
Figure 3. Relationship between eosinophil in blood and exposure period among Babcock University gardeners[r = 0.08,t = 4.55,P<0.05(0.000)].
3. Results
Eosinophil levels of blood and sputum were utilized to assess occupational allergic responses among Babcock University gardeners.
Six out of eleven mowers(54.5%)had allergic reactions[i.e.,2(18.2%)for nasal itching and 4(36.4%)for eye itching]. Twenty-four out of twenty-eight trimmers(85.7%)had allergic reactions of which 19(67.9%)had nasal itching,4(14.3%)had eye itching and only 1(3.6%)had skin itching,respectively. None of the 5 weeders had allergic reactions.
In the study to determine the relationship between blood eosinophil level and the nature or kind of responsibility of gardening undertaken by individuals,3 out of 11(27.3%)mowers,6 out of 28(21.4%)trimmers and none of the 5 weeders had blood eosinophilia. There was no significant relationship[χ2= 1.62,P>0.05(0.45)],suggesting that the nature of job undertaken by gardeners has nothing to do with eosinophilia in blood.
Figure 1 is a scatter diagram that shows the relationship between eosinophils in sputum and eosinophils in blood among Babcock University gardeners. This result displayed a significant positive correlation[r = 0.54,F = 17.36,P<0.05(0.000)]. There is a direct relationship between eosinophil in blood and sputum among Babcock University gardeners. This indicates that an increase in either blood or sputum eosinophil level may serve as a marker of allergic response.
Figure 2 is a scatter plot that displays the relationship between the occurrence of eosinophil in sputum and exposure period among Babcock University gardeners. Result demonstrated a positive correlation[r = 0.15,t = 4.55,P>0.05(0.17)],but there is no significant effect of period of exposure on sputum eosinophil level.
Figure 3 presents the relationship between the occurrence of eosinophil in blood and the exposure period among Babcock University gardeners. The result displayed a positive correlation [r = 0.08,t = 4.55,P<0.05(0.000)]. There is a directrelationship between eosinophil in blood and period of exposure to allergens among Babcock University gardeners. This indicates that the longer the exposure period,the higher the eosinophil level in blood.
4. Discussion
This study established the correlation between gardening and elevated eosinophil level in the blood and sputum of Babcock University gardeners,with a view to establishing possible occupational allergic responses. Babcock University is known widely for its consistent well-trimmed lawns,gardens and beautiful flowers among other universities in Nigeria.
Allergic diseases are primed with infiltration of the tissues with increased numbers of eosinophils[16]. Allergy is a hypersensitivity disorder of the immune system caused by an overactive immune system response or reaction to substances that may or may not be harmful. Substances that cause allergic reaction are called allergens. Common allergens include pollen,pesticides,food,insects,dust,or mould[4]. According to Bigoniya[17],occupational gardeners are very prone to skin sensitivity,asthma,musculoskeletal problems,and hypertension because they have a hectic physical work profile in which they have to undergo physical strain in an environment polluted by pesticides,dust,excessive sunlight,severe cold,and different allergic weeds which affect their health and well-being.
Gardeners within the age range of 20-29,had the highest frequency(45.5%)of blood eosinophil,while those within the ages of 50-59,had the lowest frequency(4.5%). This could be because most of the people usually employed for this job are expected to be young and agile at the point of entry the job,preferably below middle age. The mean age for the gardeners with blood eosinophil was 31 years.
It was discovered during the course of this study that 24 (85.7%)out of the 28 trimmers which make up 61.4%of the gardeners’population,have a variety of allergic reactions after gardening. It was also observed that none of them use nose mask and eye goggle while carrying out their tasks,although they all used hand gloves as the safety kit required for gardening. Nineteen(67.9%)of the subjects experienced nasal itching after gardening,while 4(14.2%)experienced eye itching and 1 (3.6%)suffered skin itching. The percentage of those with nasal itching was comparatively very high and greater than those with either skin or eye itching. This is not unconnected to the fact that most of them ignored the use of nose mask while carrying out their civic duties. Also,there could be possibility of inhaled airborne allergens from the plants and flowers during the process of trimming. Furthermore,6(54.5%)mowers out of the total number of 11 developed allergic reaction of the eye and nose after gardening while 5(45.5%)did not. Eleven mowers users declared that they use nose mask and hand gloves when gardening,while none of them use eye goggle. Two(18.2%)experienced nasal itching,4(36.4%)experienced eye itching and none of them suffered skin itching. The percentage of those that developed eye itching was considerably high. The present study is in line with the study carried out by Bigoniya[17],which stated that occupational gardeners demonstrated high prevalent vision disturbance,eye inflammation and stiff nose.
As observed from this study,the highest frequency of sputum eosinophilia was recorded in mowers users(54.5%),followed by trimmers(28.6%)while the least frequency was recorded among weeders(20%). As such,there was an insignificant correlation between sputum eosinophilia and the nature of job of Babcock University gardeners[χ2= 1.62,P>0.05(0.45)]. This result shows that eosinophilia perhaps may not be attributed to the nature of job but due to the exposure periods. However,effect mediated by exposure period could have been minimized if safety and protective wears had been put in place.
In addition,the highest frequency of blood eosinophilia was shown in mowers(27.3%),followed by trimmers(21.4%)and least in weeders(0%). The result showed an insignificant association between the occurrence of blood eosinophilia and the nature of job undertaken by the Babcock University gardeners (χ2= 1.62,P>0.05). This validates that exposure period,not the job itself is responsible for the eosinophilia in occupational gardeners. Hence,gardening as reflected from this investigation did not show any significant(P>0.05)effect on both the blood eosinophilia(0.29)and sputum eosinophil(0.52)levels.
Most importantly,the period of exposure(r = 0.15,P>0.05)and blood(r = 0.08,P<0.05)showed that gardeners who have been exposed to allergens for longer periods,displayed a considerable correlation with increased eosinophil in both blood and sputum samples. The high levels could be due to continuous sensitization particularly gardeners who have been in the profession for longer period of time[6,17].
This study is the first reported health surveillance on occupational gardeners in Nigeria. Although this study was conducted on a limited number of subjects of which the outcome reveals some facts about the working condition and health status of gardeners. Also,this study is limited because all subjects used are male;hence,it was practically difficult to uncover the influence of gender on occupational allergy. More so,we envisage that these types of studies conducted in a large number of subjects from different geographical,ecological and economic regions may explore the real picture of occupational gardeners,which will definitely help in the improvement of their health status.
We conclude from this study that majority of the occupational gardeners have latent eosinophilic allergic reactions of varying degrees during/and or after gardening. The nature and the gardening are not a predisposing factor but exposure period to allergens. It is therefore recommended that all safety and precautionary kits and wears should be enforced by regulatory authorities and embraced by the concerned occupational gardeners so as to avert and subvert its predisposing deleterious effect on them. Also,workers that had stayed long in the profession should be subjected to more thorough periodic medical screening or examination.
Conflict of interest statement
We declare that we have no conflict of interest.
Acknowledgments
The author wish to thank Babcock University gardeners for their unflinching willingness,cooperation and support throughout the study period. We are also most grateful to Mr. Adewumi Olaosebikan,a trained laboratory technician for sample collection and analysis. The study received financial support from Centre for Community Development,Action Research Grant,Kwara State University,Nigeria(Grant No. KWASUCCD/2014AR/1/27).
References
[1]Kari O,Saari KM. Updates in the treatment of ocular allergies. J Asthma Allergy 2010;3: 149-58.
[2]Crisafulli G,Caminiti L,Pajno GB. Oral desensitization for immunoglobulin E-mediated milk and egg allergies. Isr Med Assoc J 2012;14(1): 53-6.
[3]Pajno GB,Caminiti L,Crisafulli G,Vita D,Valenzise M,De Luca R,et al. Direct comparison between continuous and coseasonal regimen for sublingual immunotherapy in children with grass allergy: a randomized controlled study. Pediatr Allergy Immunol 2011;22(8): 803-7.
[4]Pajno GB,Caminiti L,Salzano G,Crisafulli G,Aversa T,Messina MF,et al. Comparison between two maintenance feeding regimens after successful cow's milk oral desensitization. Pediatr Allergy Immunol 2013;24(4): 376-81.
[5]Bilge U,Unluoglu I,Son N,Keskin A,Korkut Y,Unalacak M. Occupational allergic diseases in kitchen and health care workers: an underestimated health issue. Biomed Res Int 2013;2013: 285420.
[6]Gill D,Tan PH. Induction of pathogenic cytotoxic T lymphocyte tolerance by dendritic cells: a novel therapeutic target. Expert Opin Ther Targets 2010;14(8): 797-824.
[7]Arasi S,Crisafulli G,Caminiti L,Guarneri F,Aversa T,Porcaro F,et al. Treatment with omalizumab in a 16-year-old Caucasian girl with refractory solar urticaria. Pediatr Allergy Immunol 2015;26(6): 583-5.
[8]Muñoz-Furlong A,Weiss CC. Characteristics of food-allergic patients placing them at risk for a fatal anaphylactic episode. Curr Allergy Asthma Rep 2009;9(1): 57-63.
[9]Milner T,Reilly L,Nausch N,Midzi N,Mduluza T,Maizels R,et al. Circulating cytokine levels and antibody responses to human Schistosoma haematobium: IL-5 and IL-10 levels depend upon age and infection status. Parasite Immunol 2010;32(11-12): 710-21.
[10]Keet CA,Savage JH,Seopaul S,Peng RD,Wood RA,Matsui EC. Temporal trends and racial/ethnic disparity in self-reported pediatric food allergy in the United States. Ann Allergy Asthma Immunol 2014;112(3): 222-9.e3.
[11]Mousallem T,Burks AW. Burks. Immunology in the Clinic Review Series;focus on allergies: immunotherapy for food allergy. Clin Exp Immunol 2012;167(1): 26-31.
[12]Rujeni N,Nausch N,Midzi N,Gwisai R,Mduluza T,Taylor DW,et al. Soluble CD23 levels are inversely associated with atopy and parasite-specific IgE levels but not with polyclonal IgE levels in people exposed to helminth infection. Int Arch Allergy Immunol 2013;161(4): 333-41.
[13]Ochei J,Kolhatkar A. Medical laboratory science:theory and practice. 7th ed. New Delhi: Tata McGraw-Hill Education Pvt. Ltd;2000,p. 286-7,364-6.
[14]Umetsu DT. Targeting IgE to facilitate oral immunotherapy for food allergy: a potential new role for anti-IgE therapy?Expert Rev Clin Immunol 2014;10(9): 1125-8.
[15]Pajno GB,Caminiti L,Crisafulli G,Salzano G. Recent advances in immunotherapy: the active treatment of food allergy on the horizon. Expert Rev Clin Immunol 2013;9(10): 891-3.
[16]Rujeni N,Taylor DW,Mutapi F. Human schistosome infection and allergic sensitisation. J Parasitol Res 2012;2012: 154743.
[17]Bigoniya P,Shukla A,Singh C. A survey on the occupational health status of gardeners in Bhopal,India. Indian J Community Med 2010;35(4): 487-90.
Objective:To determine the level of eosinophils present in the blood and sputum samples,presumably as a result of continual occupational exposure to allergens while on duty,as gardeners at Babcock University,Nigeria.
Methods:Haemocytometer and Olympus microscope were utilized to estimate eosinophils population in 44 blood samples and 21 sputum samples respectively.
Results:Relationship between the occurrence of eosinophil in blood and the exposure period among Babcock University gardeners had a positive correlation(r = + 0.08,t = 4.55,P<0.05). It was found that blood eosinophil count in these workers correlated with the length of exposure period.
Conclusions:The nature and the gardening activities are not a risk factor that significantly affect eosinophil level but duration of exposure to allergens. However,all safety precautionary kits and wears should be enforced and embraced by the concerned occupational gardeners so as to avert and subvert its pre-disposing deleterious effect on them.
*Corresponding author:Oluwasogo Adewole Olalubi,School of Allied Health & Environmental Sciences,Department of Allied Health,Public Health Unit,Kwara State University,Malete,Nigeria.
 Asian Pacific Journal of Tropical Biomedicine2016年6期
Asian Pacific Journal of Tropical Biomedicine2016年6期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- Knowledge,attitude and practice of healthcare workers concerning Crimean-Congo hemorrhagic fever in Western Iran
- Epidemiological situation and molecular identification of cercarial stage in freshwater snails in Chao-Phraya Basin,Central Thailand
- Potential drug-drug interactions in pediatric wards of Gondar University Hospital,Ethiopia∶A cross sectional study
- Biofilm formation in clinical isolates of nosocomial Acinetobacter baumannii and its relationship with multidrug resistance
- Preliminary studies of acute and sub-chronic toxicity of the aqueous extract of Guibourtia tessmannii(Harms)J. Leonard stem barks(Caesalpiniaceae)in mice and rats
- Evaluation of the anticonvulsant activity of the essential oil of Myrothamnus moschatus in convulsion induced by pentylenetetrazole and picrotoxin
