Renal Denervation: Past, Present, and Future
Negiin Pourafshar, Ashkan Karimi, R. David Anderson, Seyed Hossein Alaei-Andabili and David E. Kandzari
1University of Florida, Department of Medicine, Gainesville, fl32610, USA
2University of Florida, Division of Thoracic and Cardiovascular Surgery, Gainesville, fl32610, USA
3Piedmont Heart Institute, Atlanta, GA, USA
Introduction
Hypertension is the largest contributor to cardiovascular death worldwide. Every 20/10 mmHg increase in blood pressure (BP) correlates with a doubling of 10-year cardiovascular mortality. Hypertension also dramatically increases the risk of stroke, heart attack, heart failure, and renal failure [1]. More recent data suggests a more intense blood pressure control strategy is associated with improved cardiovascular outcomes, especially in patients at high risk for cardiovascular disease [2, 3], supporting a role for treatments other than medications to lower blood pressure. Resistant hypertension is defined when blood pressure remains above goal, generally considered 140/90 mmHg, despite treatment with three anti-hypertensive medications of different classes at maximally tolerated doses including a diuretic. The true prevalence of resistant hypertension is unknown but by best estimates it affects 9–12% of hypertensive patients in the United States[4]. However, a much larger population of patients exists with uncontrolled and untreated, or incompletely treated hypertension. Indeed, despite a relatively stagnant prevalence of hypertension over the past several years, both the number of patients receiving treatment and those achieving blood pressure control has declined [5]. Between the 1920s and 1950s, before the advent of oral pharmacotherapy,renal denervation (RDN) via surgical splanchniectomy was advocated as an effective treatment for severe hypertension. Unfortunately, it was associated with high operative morbidity, and with the subsequent development of oral anti-hypertensive medications, it was abandoned in late 1950s[6, 7]. However, by way of human surgical renal denervation experience and further basic research experiments, the role of sympathetic renal regulation of blood pressure became increasingly well understood. In 1980–1990s, development of catheter-based radiofrequency (RF) ablation technology transformed the field of electrophysiology. By the early 2000s, the same technology was utilized for percutaneous RDN in patients with resistant hypertension. The initial small size studies showed promising results and this procedure was met with a great deal of enthusiasm from the scientific community and industry. However, SYMPLICITY HTN-3, the largest randomized sham-controlled clinical trial, showed RDN was not more effective than medial therapy in treatment of severe resistant hypertension. Percutaneous RDN has therefore not yet received FDA approval in the United States and remains in clinical evaluation. Herein we review the Simplicity RDN trials with a focused analysis of the SYMPLICITY HTN-3 trial results and its impact on the design of the most recent trials, the SPYRAL HTN Global clinical trials. This review is focused principally on the SYMPLICITY catheter system(Medtronic CardioVascular Inc., Santa Rosa, CA,USA); however, there are several alternative RDN systems with proprietary catheter-based electrode designs, chemical, or ultrasound ablation energy delivery, in addition to external ultrasound. Table 1 summarizes several contemporary technologies. The application of RDN in patients with chronic kidney disease (CKD) or end stage renal disease (ESRD),a subset of patients who were excluded from major clinical trials, is also described. The role of RDN in the management of other disease processes such as congestive heart failure, cardiac arrhythmia, metabolic disease, and sleep apnea is also presented.
SYMPLICITY HTN 1 and 2 Clinical Trials
SYMPLICITY HTN-1 was a first-in-man, proofof-concept, catheter-based RDN trial which was launched in June 2007. It enrolled 50 patients at five Australian and European centers using the SYMPLICITY®Arch™ catheter by Ardian Inc(Palo Alto, CA, USA), which was later acquiredby Medtronic CardioVascular Inc (Santa Rosa,CA, USA). This study used the first generation SYMPLICITY catheter which applied low energy radiofrequency energy only at a single point, distal electrode tip. The catheter is advanced distally into the each renal artery and then as it is retracted proximally, RF energy is applied circumferentially to create at least 4 lesions in separate quadrants. This study demonstrated that the procedure was safe and effective. There were no RDN catheter related complications. One patient developed catheter-induced renal artery dissection prior to ablation that was treated with stent placement, and one patient developed a femoral artery pseudoaneurysm at the access site that was conservatively managed. The efficacy endpoints, change in mean office-based systolic and diastolic blood pressure, were reduced by 22 mmHg and 11 mmHg, respectively, at 6 months. In addition,24-h systolic ambulatory blood pressure monitoring(ABPM) demonstrated an 11 mmHg reduction in a subset of nine patients who had ABPM performed and were office BP responders, defined as reduction in office systolic blood pressure (SBP) of at least 10 mmHg [8].
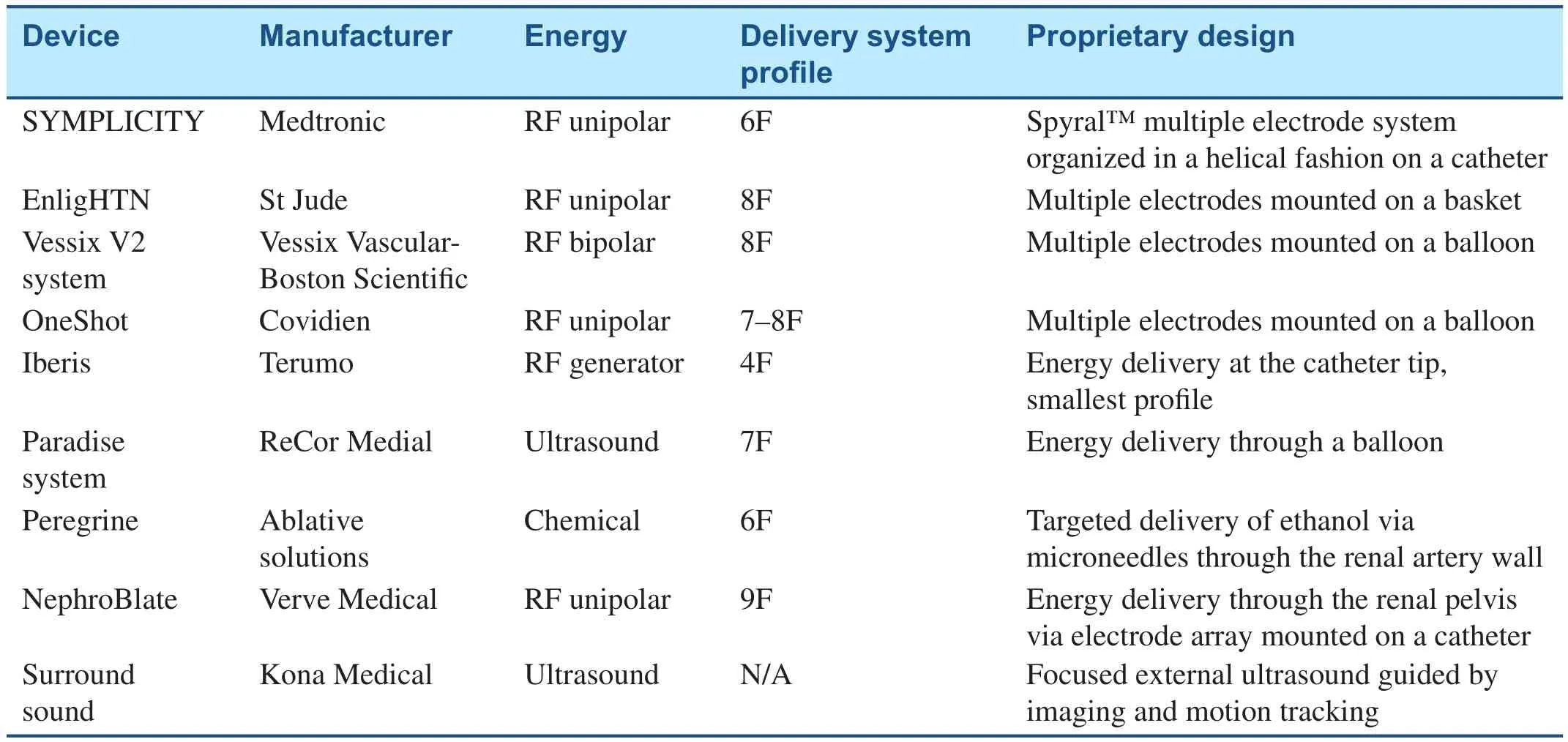
Table 1 Renal Denervation Devices.
Shortly after completion of this study,SYMPLICITY HTN-2 was launched in June 2009.In an unblinded fashion, 106 resistant hypertensive patients were randomized 1:1 to renal denervation with the SYMPLICITY®Arch catheter vs. medical therapy. This study showed office-based systolic and diastolic blood pressures were reduced by 32 mmHg and 12 mmHg, respectively, at 6 months in the RDN arm compared with no significant change in the medical treatment arm. Similar to the prior study, SYMPLICITY HTN-2 showed a clinically meaningful decline in 24-h systolic and diastolic ABPM of 11 mmHg and 7 mmHg, respectively in a subset of only 20 RDN patients who had ABPM performed. This study also confirmed the safety of renal denervation, with no device-related complications [9]. On the heels of these two studies SYMPLICITY HTN-3 pivotal clinical trial was designed and launched in the United States.
SYMPLICITY HTN-3
The SYMPLICITY HTN-3 trial was conducted between 2011 and 2013 in 88 sites in the United States. It was a prospective, single-blinded, randomized, sham-controlled trial of 535 patients with severe resistant hypertension who were randomly assigned in a 2:1 fashion to renal denervation with the second-generation SYMPLICITY Flex™ catheter or a sham renal angiography procedure alone.To be randomized in the trial, patients were initially screened in the office and were required by protocol to have an average of three SBP measurements in the office that were ≥160 mmHg. Patients must have received treatment with ≥3 anti-hypertensive medications at their maximum tolerated doses, including diuretic therapy, and had no medication changes in the previous 2 weeks. For the next 2 weeks, patients recorded their home BP and kept a diary of their medications. Then they were seen in the office again and if office SBP was still ≥160 mmHg, and adherence to home medications was confirmed, a 24-h ABPM was performed. Only if average ABPM SBP was ≥135 mmHg were the patients then included in the study. Following randomization, patients were mandated to maintain their anti-hypertensive regimen without change, notwithstanding medical necessity.
The primary endpoint of the trial was change in blood pressure at 6 months between patients randomized to RDN versus the sham control procedure.At 6 months, the RDN group had mean reduction in office SBP of 14.1 mmHg which was significant compared to the baseline but did not significantly differ from an 11.7 mmHg reduction in the sham group, a difference of only 2.4 mmHg (P-value=0.26 for superiority with a margin of 5 mmHg). There was also no significant change in 24-h ambulatory SBP between the two groups (6.8 mmHg in the RDN group vs. 4.8 mmHg in the sham-procedure group, P-value=0.98 for superiority with a margin of 2 mmHg). The study did, however, meet its prespecified safety endpoint.There were no significant difference in safety outcomes between the two groups [10].
To compare SYMPLICITY HTN-3 results to prior trials and registry data, SYMPLICITY HTN-1 showed a reduction in mean office SBP of 22 mmHg at 6 months and 24-h ambulatory SBP of 11 mmHg at least 30 days after the procedure [8]. SYMPLICITY HTN-2 showed 32 mmHg reduction in mean office SBP and 11 mmHg reduction in 24-h ambulatory SBP at 6 months which was significantly larger that the control group [9]. Further, in a study of 1000 patients from the global SYMPLICITY registry, a‘real world’ prospective registry, the mean office SBP was reduced 11.6 mmHg with a 6.6 mmHg reduction in 24-h ambulatory SBP 6 months following RDN [11].
Lessons Learned From SYMPLICITY HTN-3
Unlike prior RDN trials, why did SYMPLICITY HTN-3 not reproduce superior results with RDN?There are several potential explanations. One possibility would be to accept that RDN is not effective and to postulate why the positive results shown in previous trials were not replicated in SYMPLICITY HTN-3. There would be three major explanations:first, unlike prior trials, SYMPLICITY HTN-3 had a very effective blinding process. In the shamprocedure arm, every effort was made to blind the patients to the procedure by using conscious sedation, sensory isolation (for example, wearing blindfolds, headphones and playing background music,etc.), and similar to the treatment arm these patients were admitted for overnight observation and blindness was even tested in the study via a questionnaire and its effectiveness was confirmed [10, 12].In addition, the study staff who assessed blood pressure during follow-ups were also blinded. Therefore lack of blindness in prior trials could have been responsible for introduction of bias and skewing the results in favor of renal denervation. Secondly, in SYMPLICITY HTN-3 the sham-procedure group showed an unexpected and significant reduction in office-based SBP of 11.7 mmHg at 6 months compared to baseline. This observation implies good medical care, vigorous follow-up, and adherence to medications as part of participation in the trial could have been responsible for the BP response in the control group. This latter observation may relate to the “Hawthorne effect”, suggesting that individual behavior may be differing when patients are aware they are being followed in the context of a study. Third, the exaggerated office-based SBP reduction observed in RDN earlier trials or registries could be due to regression toward the mean phenomenon. This could be due to the fact that the office-based SBP was extreme on its first measurement and could also account for the fact that ambulatory BP showed a more modest response to RDN. Considering that ABPM represents a measure independent of variability associated with a single office assessment, this rationale would not however explain lack of 24-h ambulatory SBP response observed in SYMPLICITY HTN-3.
An alternative assessment of the current data would suggest that based on the wealth of prior clinical and basic science evidence on RDN there may be reasonable explanations for its lack of effi-cacy in the largest and most rigorously designed RDN trial. Sub-group andpost hocanalyses have provided some insight into possible factors such as operator experience and procedural factors, patient characteristics, medication class interaction with RDN, medication compliance, and medication changes during the trial.
In apost hocanalysis of SYMPLICITY HTN-3 there was a statistically significant greater reduction in office and ambulatory BP with increased number of ablation attempts, and there was also a trend towards more reduction in BP with delivery of four-quadrant ablation although it did not reach statistical significance [13]. Notably, more than 50%of the operators in the SYMPLICITY HTN-3 trial had performed only one or two RDN procedures as part of the trial. This is in contrast to the global SYMPLICITY registry in which 82% of operators performed ≥6 procedures [11]. Nevertheless, a relationship between operator volume and outcome has not been firmly established.
An additional important technical factor may relate to the anatomic site of ablation. Since the results of SYMPLICITY HTN 3, recent pathological studies have shown that while there are fewer nerves surrounding the renal artery in distal segments, the mean distance from renal artery lumen to the nerves is least in distal segments (2.6 mm)compared to proximal segments (3.4 mm), and therefore RF ablation in distal renal artery segment may be more likely to achieve effective renal artery ablation [14]. The same concept has recently been examined in a swine animal model by two different groups. They have shown that distal renal artery ablation and ablation into renal artery branches was associated with significantly greater efficacy and less variability in renal denervation as measured by renal norepinephrine tissue content and renal cortical axon density [13, 15].
Despite these findings, major limitation to RDN therapy remains the lack of a practical biomarker of procedural efficacy [16]. In SYMPLICITY HTN-1 renal noradrenaline spillover was used as a surrogate for procedural effectiveness and there was on average 47% reduction but with wide variability in response (95% CI 28–65%) [8]. Parallel anecdotal evidence in a patient who underwent RDN and passed away 12 days later from aortic dissection,showed that ablation did not penetrate deeper than 2 mm from renal artery lumen and only achieved partial RDN [17]. In essence, a lack of BP response to RDN in some patients may be the result of procedural failure to achieve RDN and not necessarily conceptual failure of RDN.
Sub-group analyses of patient characteristics in SYMPLICITY HTN-3 also provide a potential explanation for the trial’s negative efficacy outcome. Sub-group analysis based on ethnicity showed that RDN had similar effects in African Americans and non-African Americans with a mean reduction in office-based SBP of about 15 mmHg;however, in the sham-procedure arm the African American group had an exaggerated and signifi-cant reduction in office-based SBP of 17.8 mmHg at 6 months compared to 8.6 mmHg in non-African Americans, which mitigated the effect of RDN in the African American subgroup. Analysis of patient medication regimen showed that a higher percentage of the African American subgroup were also receiving vasodilator therapy at baseline. The cause of the observed differential response in African Americans is unclear, but could be potentially due to genetic factors, medication class interaction with RDN, or medication compliance.
In another medication analysis of patients who underwent RDN, prescription of an aldosterone antagonist at baseline was a positive predictor of officebased and 24-h ambulatory SBP response to RDN at 6 months. Conversely, vasodilator prescription at baseline was found to be a negative predictor of officebased and 24-h ambulatory SBP response. This raises the question of whether or not there is a medication class interaction with RDN. These findings should be interpreted with caution and only taken as hypothesis generating as they arepost hocsubgroup analyses with limited number of patients in each group and could have happened by chance. Nonetheless, they highlight the importance of standardized medical therapy in future RDN trials [13]. One further important observation from SYMPLICITY HTN-3 was that despite an emphasis on keeping a stable medical regimen throughout the trial duration, 39% of patients changed their medical therapy between randomization and 6 months which also could have impacted trial results. Additionally, the only means to evaluate medication compliance in the SYMPLICITY HTN 3 trial was by patient verbal report rather than a more objective way to assess medication compliance by checking plasma or urine drug levels that are included in contemporary RDN trials.
SYMPLICITY HTN-3 enrolled an extreme subset of resistant hypertension patients with average baseline SBP of 180 mmHg, on an average of five antihypertensive medications of different classes, and with significant comorbidities (about 45% diabetes and 25% coronary artery disease). This patient population may introduce greater heterogeneity given variability in medical adherence and comorbidities.Also, it is likely that arterial remodeling and stiffness as a result of long-standing hypertension was also a major contributor to systolic hypertension in these patients and sympathetic overactivity, which is modulated with RDN, may have been a less significant mediator of hypertension [10].
SPYRAL HTN Global Clinical Trial
The SPYRAL HTN Global clinical trial has been designed to address design shortcomings of the prior SYMPLICITY Trials. It is composed of two simultaneous, randomized, blinded, sham-controlled trials conducted by experienced renal denervation operators at about 25 centers in the United States, Europe, Japan, and Australia: OFF-MED(NCT02439749) and ON-MED (NCT02439775)[18]. The randomization target for both studies is 100 patients, with up to 120 patients in the OFF-MED arm to account for attrition due to patients meeting escape criteria (if SBP ≥180 mmHg) to ensure safety of study subjects. The OFF-MED arm is essentially a proof-of-concept study, intending to assess RDN efficacy without anti-hypertensive medication in patients who are drug naive or after a drug washout period. The ON-MED arm studies the efficacy of RDN in patients on a stable and standardized antihypertensive regimen composed of a thiazide-type diuretic, dihydropyridine-type calcium-channel blocker, and an angiotensin- converting enzyme inhibitor or angiotensin receptor blocker, at dosages at least 50% of the maximal recommendation. Unlike SYMPLICITY HTN-3, SPYRAL HTN Global clinical trial includes patients with moderate uncontrolled hypertension by including those with office SBP of ≥150 mmHg, and 24-h ambulatory SBP of ≥140 mmHg to <170 mmHg, and eliminating the requirement of maximum doses of three anti-hypertensive therapies. It also requires a DBP of ≥90 mmHg to include those with combined systolic-diastolic hypertension that may be more sympathetically mediated. Both studies will use the third-generation SYMPLICITY Spyral™ renal denervation catheter, in which four radiofrequency electrodes are mounted approximately 5 mm apart and at 90° of separation from each other in a helical pattern, therefore providing automated four quadrant ablation treatments (Figure 1). Furthermore,urine and serum samples of the subjects will be analyzed several times by mass spectroscopy to test for medication compliance throughout the study period. The findings of these two trials will guide investigators design the future SPYRAL HTN pivotal study [18].
RDN and Chronic Kidney Disease
A subset of patients with high incidence of resistant hypertension, who would benefit greatly from better blood pressure control but have been excluded from major RDN trials are patients with CKD. Several studies have shown sympathetic overactivity in patients with CKD and ESRD [19–21]. Hering et al. carried out a two-center pilot study of RDN in 15 patients with moderate to severe CKD (mean estimated glomerular filtration rate of 31±9 mL/min per 1.73 m2) and demonstrated RDN did not cause further deterioration in renal function and lead to average reduction in office-based systolic and diastolic BP of 32/15 mmHg at 6 months and 33/19 mmHg at 12 months [22]. Other small size studies have produced similar results [23, 24]. One study demonstrated a small improvement in eGFR and reduced albuminuria using a standard electrophysiology ablation catheter for RDN [23]. The role of RDN in the setting of CKD and ESRD needs further investigation in larger populations and in a comparative and randomized fashion.
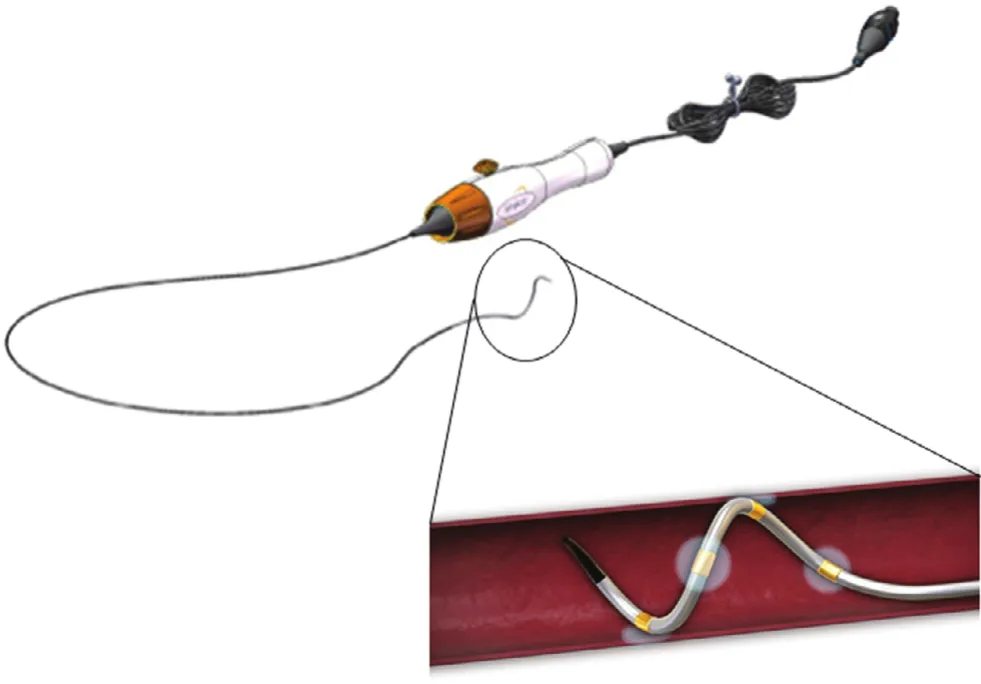
Figure 1 SYMPLICITY Spyral™ Renal Denervation Catheter.Photo adopted from http://www.medgadget.com and http://www.invasivecardiology.com/blog/transcatheter-renaldenervation.
RDN in Management of Systemic Diseases Other than Hypertension
The role of RDN in management of several systemic diseases other than hypertension such as congestive heart failure, arrhythmia, metabolic syndrome, and sleep apnea has been explored over the past several years. Prior studies have shown evidence of sympathetic overactivity in both heart failure with reduced[25–27] and preserved ejection fraction [28, 29]which has been linked to worse heart failure outcomes. In patients with heart failure and reduced ejection fraction, it has been well demonstrated that neuroendocrine antagonists, such as angiotensinconverting enzyme inhibitors, β-blockers, and aldosterone antagonists improve outcomes. Could modulation of the documented sympathetic overactivity allow RDN to play a role in the management of congestive heart failure? In a swine model of systolic heart failure in which heart failure was induced with rapid ventricular pacing, it has been shown that RDN improved cardiac function and attenuated left ventricular remodeling [30]. Small human studies have also shown improvement in systolic(increased ejection fraction) and diastolic measurements (reduction in E/E ratio and isovolemic relaxation time) and reduction in left ventricular mass after RDN [31]. There are several ongoing trials aiming to further elucidate the role of RDN in heart failure management including two multicenter trials SYMPLICITY HF and DIASTOLE.The SYMPLICITY HF trial (NCT01392196) is currently underway in Australia and Europe studying RDN in patients with combined systolic heart failure (EF<40%) and stage II or IIichronic kidney disease (GFR 30–75 mL/min/1.73 m2) with expected completion in 2017. DIASTOLE (Denervation of the renAl sympathetIc nerveS in hearT Failure With nOrmal Lv Ejection Fraction, NCT01583881) is a multi-center, prospective, randomized controlled trial which just finished recruitment. Its targeted sample of 60 patients with hypertension and heart failure with preserved ejection fraction were randomized in a 1:1 fashion to RDN in addition to anti-hypertensive treatment vs. anti-hypertensive treatment alone with the primary endpoint of E/E ratio at 12 months. There are a host of secondary endpoints including other echocardiographic parameters of diastolic dysfunction, MRI parameters(left ventricular mass, left ventricular volume, left atrial volume, left ventricular ejection fraction, and right ventricular ejection fraction), and invasive hemodynamic parameters of diastology by measuring left ventricular end diastolic pressure, left ventricular relaxation from pressure-volume loops, and functional parameters (6 min walk and Minnesota Living with Heart Failure Questionnaire). The results should be available in the near future [32].
Another area of potential application for RDN is metabolic syndrome. Patients with obesity and metabolic syndrome have elevated urinary noradrenaline levels, increased efferent muscle sympathetic nerve activity, and elevated rates of plasma noradrenaline spillover [33–35]. These findings have stimulated investigators to explore the potential role of RDN in the management of metabolic syndrome and diabetes. The literature on this topic has provided mixed results. A retrospective sub-analysis of 37 patients who underwent renal denervation in the SYMPLICITY HTN study showed significant decrease in fasting plasma glucose, insulin, C-peptide and 2-h post load glucose levels at 3-months follow-up while no metabolic improvements were reported in the control group who received medical therapy alone [36]. However the Denervation of the Renal Arteries in Metabolic Syndrome (DREAMS-study) assessed the effect of bilateral RDN with the SYMPLICITY Flex™ catheter in 29 patients with metabolic syndrome and did not show improvement in insulin sensitivity[37]. Further, mechanistic basic science research is needed to study the pathophysiologic role of renal nerve sympathetic activity in the complex pathophysiology of metabolic syndrome prior to embarking on further clinical trials.
Treatment of cardiac arrhythmias, both atrial and ventricular, is another area in which RDN has been studied. The sympathetic nervous system plays a crucial role in the pathogenesis and maintenance of atrial and ventricular arrhythmias [38]. Studies have shown that RDN makes it more difficult to induce atrial fibrillation in animal models and also lowers the ventricular rate [39, 40]. A subset study of 14 RDN responders (defined as a reduction in office SBP≥10 mmHg post RDN) from the EnligHTN I study, (which used the multi-electrode EnligHTN ablation catheter, St Jude Medical, St Paul, MN,USA), revealed RDN was associated with signifi-cant reduction in mean heart rate at 1 and 6 months,as well as reductions in the total number of premature supraventricular and ventricular contractions[41]. The “adjunctive renal sympathetic denervation to modify hypertension as upstream therapy in the treatment of atrial fibrillation” or H-FIB trial, (NCT01635998) is a large (300 patients),prospective, double-blind, randomized controlled trial, currently in progress to address the whether RDN in conjunction with atrial fibrillation ablation may enhance atrial fibrillation ablation success.This study uses the Boston Scientific Vessix renal denervation system [42]. Regarding ventricular arrhythmias, a case series of four patients with ventricular tachycardia storm despite prior ablation and maximized anti-arrhythmic therapy, reported RDN significantly reduced the number of ventricular tachycardia episodes [43]. More studies are needed to understand the linkage between renal sympathetic innervation and arrhythmogenesis to identify who would benefit from RDN for arrhythmia management.
Lastly, treatment of obstructive sleep apnea has also been targeted with RDN as sympathetic overactivity is believed to play a critical role in the pathophysiology of this disorder [44, 45]. A small single center experience with RDN in ten patients with refractory hypertension and obstructive sleep
apnea not only resulted in better blood pressure control, but also improvement in gluc
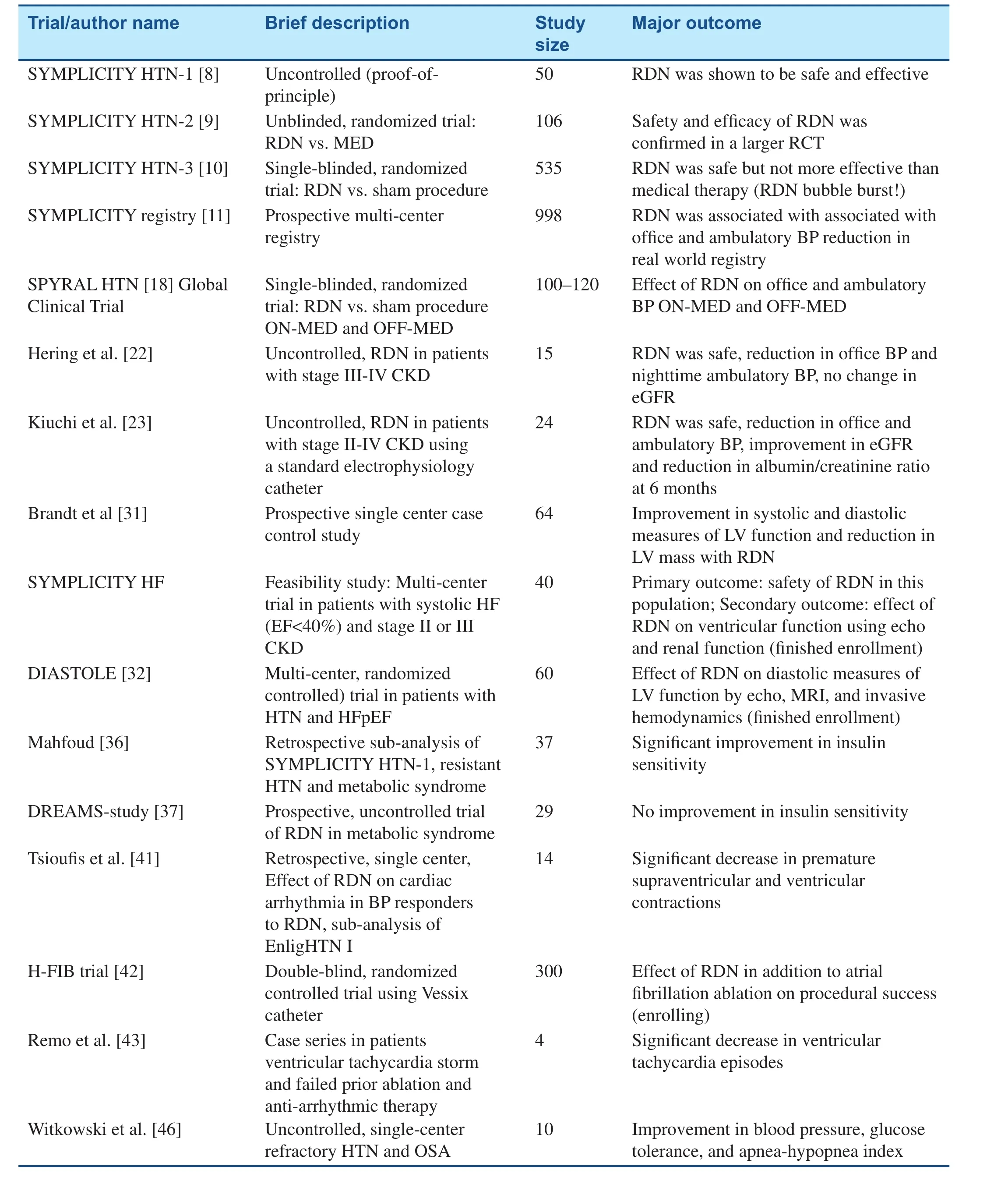
Table 2 Summary of the Studies Discussed in the Present Review.
ose tolerance,and apnea-hypopnea index in follow-up. This suggests that RDN may potentially have a role in the management of patients with comorbid refractory hypertension, glucose intolerance, and obstructive sleep apnea [46]. Table 2 provides a summary of the studies discussed in this review.
Conclusion
Despite the disappointing resu
l
ts of SYMPLICITY HTN-3, the field of RDN is still alive and is being actively investigated. SYMPLICITY HTN-3 carried a very important message that for this technology to be approved there should be a vigorously designed sham-controlled, blinded, randomized clinical trial. Important lessons were learned frompost hocand subgroup analyses of its data which contributed to the design of SPYRAL HTN Global ON-MED and OFF-MED clinical trials. The future of RDN evolves around refinement of its technology to obtain predictable and sustainable renal denervation via a trans-catheter approach that results in reduction of renal sympathetic output. If efficacy is demonstrated, predictors of treatment effect will be an important focus of investigation. A major limitation of the current RDN technology is the absence of a clinical, laboratory, or imaging test to assess its immediate procedural success. Another key issue with RDN is the identification of appropriate candidates. After the SYMPLICITY HTN-3 results,design of the SPYRAL HTN Global ON-MED clinical trial led the investigators to target a less severe hypertensive population but who have both systolic and diastolic hypertension. Patients will be treated with only very experienced operators and with careful attention to procedural method. In the past decade there has been a significant increase in RDN devices with proprietary design using various energy sources, and as investigators strive to discover the role of RDN in the management of hypertension, there is a future need for direct comparative study between these technologies to identify the safest and most effective device.
Conflict of Interest
Dr. Kandzari receives research/grant support from Medtronic CardioVascular and Boston Scientific,and also consulting honoraria from Medtronic CardioVascular and Boston Scientific.
REFERENCES
1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, et al. Joint National Committee on Prevention DE, Treatment of High Blood Pressure. National Heart L, Blood I and National High Blood Pressure Education Program Coordinating C. Seventh report of the Joint National Committee on Prevention, Detection,Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206–52.
2. Xie X, Atkins E, Lv J, Bennett A,Neal B, Ninomiya T, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes:updated systematic review and metaanalysis. Lancet 2016;387:435–43.
3. Group SR, Wright JT Jr., Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard bloodpressure control. N Engl J Med 2015;373:2103–16.
4. Sarafidis PA, Georgianos P, Bakris GL. Resistant hypertension--its identification and epidemiology.Nat Rev Nephrol 2013;9:51–8.
5. Egan BM, Li J, Hutchison FN,Ferdinand KC. Hypertension in the United States, 1999 to 2012: progress toward healthy people 2020 goals. Circulation 2014;130:1692–9.
6. Papademetriou V, Rashidi AA,Tsioufis C, Doumas M. Renal nerve ablation for resistant hypertension:how did we get here, present status,and future directions. Circulation 2014;129:1440–51.
7. Smithwick RH, Thompson JE.Splanchnicectomy for essential hypertension; results in 1,266 cases.J Am Med Assoc 1953;152:1501–4.8. Krum H, Schlaich M, Whitbourn R, Sobotka PA, Sadowski J, Bartus K, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 2009;373:1275–81.
9. SYMPLICITY HTN I, Esler MD,Krum H, Sobotka PA, Schlaich MP,Schmieder RE, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension(The SYMPLICITY HTN-2 Trial):a randomised controlled trial.Lancet 2010;376:1903–9.
10. Bhatt DL, Kandzari DE, O’Neill WW, D’Agostino R, Flack JM,Katzen BT, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 2014;370:1393–401.
11. Bohm M, Mahfoud F, Ukena C, Hoppe UC, Narkiewicz K,Negoita M, et al. First report of the Global SYMPLICITY Registry on the effect of renal artery denervation in patients with uncontrolled hypertension. Hypertension 2015;65:766–74.
12. Kandzari DE, Bhatt DL, Sobotka PA, O’Neill WW, Esler M, Flack JM, et al. Catheter-based renal denervation for resistant hypertension: rationale and design of the SYMPLICITY HTN-3 Trial. Clin Cardiol 2012;35:528–35.
13. Mahfoud F, Tunev S, Ewen S,Cremers B, Ruwart J, Schulz-Jander D, et al. Impact of lesion placement on efficacy and safety of catheter-based radiofrequency renal denervation. J Am Coll Cardiol 2015;66:1766–75.
14. Sakakura K, Ladich E, Cheng Q, Otsuka F, Yahagi K, Fowler DR, et al. Anatomic assessment of sympathetic peri-arterial renal nerves in man. J Am Coll Cardiol 2014;64:635–43.
15. Henegar JR, Zhang Y, Hata C,Narciso I, Hall ME, Hall JE.Catheter-based radiofrequency renal denervation: location effects on renal norepinephrine. Am J Hypertens 2015;28:909–14.
16. Esler M. Illusions of truths in the SYMPLICITY HTN-3 trial:generic design strengths but neuroscience failings. J Am Soc Hypertens 2014;8:593–8.
17. Vink EE, Goldschmeding R,Vink A, Weggemans C, Bleijs RL, Blankestijn PJ. Limited destruction of renal nerves after catheter-based renal denervation: results of a human case study. Nephrol Dial Transplant 2014;29:1608–10.
18. Kandzari DE, Kario K, Mahfoud F, Cohen SA, Pilcher G, Pocock S, et al. The SPYRAL HTN global clinical trial program: rationale and design for studies of renal denervation in the absence (SPYRAL HTN OFF-MED) and presence(SPYRAL HTN ON-MED) of antihypertensive medications. Am Heart J 2016;171:82–91.
19. Converse RL Jr, Jacobsen TN,Toto RD, Jost CM, Cosentino F,Fouad-Tarazi F, et al. Sympathetic overactivity in patients with chronic renal failure. N Engl J Med 1992;327:1912–8.
20. Hausberg M, Kosch M, Harmelink P, Barenbrock M, Hohage H,Kisters K, et al. Sympathetic nerve activity in end-stage renal disease.Circulation 2002;106:1974–9.
21. Ligtenberg G, Blankestijn PJ,Oey PL, Klein IH, Dijkhorst-Oei LT, Boomsma F, et al. Reduction of sympathetic hyperactivity by enalapril in patients with chronic renal failure. N Engl J Med 1999;340:1321–8.
22. Hering D, Mahfoud F, Walton AS,Krum H, Lambert GW, Lambert EA, et al. Renal denervation in moderate to severe CKD. J Am Soc Nephrol 2012;23:1250–7.
23. Kiuchi MG, Maia GL, de Queiroz Carreira MA, Kiuchi T, Chen S,Andrea BR, et al. Effects of renal denervation with a standard irrigated cardiac ablation catheter on blood pressure and renal function in patients with chronic kidney disease and resistant hypertension.Eur Heart J 2013;34:2114–21.
24. Schlaich MP, Bart B, Hering D,Walton A, Marusic P, Mahfoud F,et al. Feasibility of catheter-based renal nerve ablation and effects on sympathetic nerve activity and blood pressure in patients with endstage renal disease. Int J Cardiol 2013;168:2214–20.
25. Cohn JN, Levine TB, Olivari MT,Garberg V, Lura D, Francis GS,et al. Plasma norepinephrine as a guide to prognosis in patients with chronic congestive heart failure. N Engl J Med 1984;311:819–23.
26. Floras JS. Sympathetic nervous system activation in human heart failure: clinical implications of an updated model. J Am Coll Cardiol 2009;54:375–85.
27. Hasking GJ, Esler MD, Jennings GL, Burton D, Johns JA, Korner PI. Norepinephrine spillover to plasma in patients with congestive heart failure: evidence of increased overall and cardiorenal sympathetic nervous activity. Circulation 1986;73:615–21.
28. Grassi G, Seravalle G, Cattaneo BM, Lanfranchi A, Vailati S,Giannattasio C, et al. Sympathetic activation and loss of reflex sympathetic control in mild congestive heart failure. Circulation 1995;92:3206–11.
29. Grassi G, Seravalle G, Quarti–Trevano F, Dell’Oro R, Arenare F,Spaziani D, et al. Sympathetic and baroreflex cardiovascular control in hypertension-related left ventricular dysfunction. Hypertension 2009;53:205–9.
30. Xie Y, Liu Q, Xu Y, Gao J, Yan P,Zhang W, et al. Effect of catheterbased renal sympathetic denervation in pigs with rapid pacing induced heart failure. Zhonghua Xin Xue Guan Bing Za Zhi 2014;42:48–52.
31. Brandt MC, Mahfoud F, Reda S,Schirmer SH, Erdmann E, Bohm M, et al. Renal sympathetic denervation reduces left ventricular hypertrophy and improves cardiac function in patients with resistant hypertension. J Am Coll Cardiol 2012;59:901–9.
32. Verloop WL, Beeftink MM,Nap A, Bots ML, Velthuis BK,Appelman YE, et al. Renal denervation in heart failure with normal left ventricular ejection fraction. Rationale and design of the DIASTOLE (DenervatIon of the renAl Sympathetic nerves in hearT failure with nOrmal Lv Ejection fraction) trial. Eur J Heart Fail 2013;15:1429–37.
33. Grassi G, Dell’Oro R, Quarti-Trevano F, Scopelliti F, Seravalle G, Paleari F, et al. Neuroadrenergic and reflex abnormalities in patients with metabolic syndrome.Diabetologia 2005;48:1359–65.
34. Lee ZS, Critchley JA, Tomlinson B,Young RP, Thomas GN, Cockram CS, et al. Urinary epinephrine and norepinephrine interrelations with obesity, insulin, and the metabolic syndrome in Hong Kong Chinese.Metabolism 2001;50:135–43.
35. Schlaich M, Straznicky N, Lambert E, Lambert G. Metabolic syndrome: a sympathetic disease?Lancet Diabetes Endocrinol 2015;3:148–57.
36. Mahfoud F, Schlaich M,Kindermann I, Ukena C, Cremers B, Brandt MC, et al. Effect of renal sympathetic denervation on glucose metabolism in patients with resistant hypertension: a pilot study.Circulation 2011;123:1940–6.
37. Verloop WL, Spiering W, Vink EE, Beeftink MM, Blankestijn PJ,Doevendans PA, et al. Denervation of the renal arteries in metabolic syndrome: the DREAMS-study.Hypertension 2015;65:751–7.
38. Doumas M, Faselis C, Tsioufis C,Papademetriou V. Carotid baroreceptor activation for the treatment of resistant hypertension and heart failure. Curr Hypertens Rep 2012;14:238–46.
39. Linz D, Mahfoud F, Schotten U, Ukena C, Neuberger HR,Wirth K, et al. Renal sympathetic denervation suppresses postapneic blood pressure rises and atrial fibrillation in a model for sleep apnea.Hypertension 2012;60:172–8.
40. Zhao Q, Yu S, Zou M, Dai Z, Wang X, Xiao J, et al. Effect of renal sympathetic denervation on the inducibility of atrial fibrillation during rapid atrial pacing. J Interv Card Electrophysiol 2012;35:119–25.
41. Tsioufis C, Papademetriou V,Tsiachris D, Dimitriadis K,Kasiakogias A, Kordalis A, et al.Drug-resistant hypertensive patients responding to multielectrode renal denervation exhibit improved heart rate dynamics and reduced arrhythmia burden. J Hum Hypertens 2014;28:587–93.
42. Ahmed H, Miller MA, Dukkipati SR, Cammack S, Koruth JS,Gangireddy S, et al. Adjunctive renal sympathetic denervation to modify hypertension as upstream therapy in the treatment of atrial fibrillation (H-FIB) study: clinical background and study design.J Cardiovasc Electrophysiol 2013;24:503–9.
43. Remo BF, Preminger M, Bradfield J, Mittal S, Boyle N, Gupta A,et al. Safety and efficacy of renal denervation as a novel treatment of ventricular tachycardia storm in patients with cardiomyopathy.Heart Rhythm 2014;11:541–6.
44. Fisher JP, Young CN, Fadel PJ.Central sympathetic overactivity:maladies and mechanisms. Auton Neurosci 2009;148:5–15.
45. Prabhakar NR, Kumar GK.Mechanisms of sympathetic activation and blood pressure elevation by intermittent hypoxia.Respir Physiol Neurobiol 2010;174:156–61.
46. Witkowski A, Prejbisz A, Florczak E, Kadziela J, Sliwinski P, Bielen P,et al. Effects of renal sympathetic denervation on blood pressure,sleep apnea course, and glycemic control in patients with resistant hypertension and sleep apnea.Hypertension 2011;58:559–65.
 Cardiovascular Innovations and Applications2016年2期
Cardiovascular Innovations and Applications2016年2期
- Cardiovascular Innovations and Applications的其它文章
- Transient Pulmonary Atelectasis after Ketamine Sedation during Cardiac Catheterization in Spontaneously Breathing Children with Congenital Heart Disease
- Identification and Management of Iatrogenic Aortocoronary Dissection
- Cardiovascular Abnormalities Among Patients with Spontaneous Subarachnoid Hemorrhage.A Single Center Experience
- Coronary Artery Chronic Total Occlusion
- Carotid Artery Stenting: 2016 and Beyond
- The Transradial Approach for Cardiac Catheterization and Percutaneous Coronary Intervention: A Review
