Carotid Artery Stenting: 2016 and Beyond
Siddharth Wayangankar, MD*, Samir Kapadia, MD and Christopher Bajzer, MD
1Department of Cardiovascular Medicine, Cleveland Clinic, 9500 Euclid Ave, Cleveland, OH 44195, USA
Introduction
It has been over six decades since carotid stenosis was implicated in the pathophysiology of ischemic stroke[1]. Surgical options developed to treat carotid artery stenosis have evolved since then, and studies have shown superiority of carotid endarterectomy (CEA)compared to medical therapy [2]. Similarly, as endovascular therapy has evolved over the last two decades, studies reflecting safety, feasibility, and equivalence of carotid artery stenting (CAS) to CEA have been replicated in several studies for intermediate to high surgical risk patients [3, 4]. However, since its inception, the field of CAS has been mired in several controversies and has been subject to intense scrutiny from multiple stakeholders within the field of medicine. Despite this, CAS as a procedure continues to evolve. In this review, we discuss specific issues concerning CAS that are relevant in the current era.
Indications for Carotid Revascularization
Two aspects of traditional studies comparing surgical carotid revascularization and medical therapy have been flawed by the passage of time. First, medical therapy in most of these studies consisted only of aspirin. Current medical treatment consists of a potent cocktail of anti-platelet, anti-hypertensive and contemporary statin therapies. Hence, results from these traditional studies are difficult to extrapolate to the current era. Secondly, in retrospect,earlier studies were inadequate due to inaccurate post-procedural neurological assessments. In fact, a meta-analysis performed two decades ago showed that the choice of specialty evaluating the postprocedural neurological outcomes was the strongest predictor of 30-day adverse neurological outcomes[5]. It ranged from 7.7%, if evaluated by a neurologist, to 2.3% when evaluated by the operator surgeon. Despite the shortcomings of earlier studies,current guidelines recommend carotid revascularization if the risk of peri-procedural stroke and death is <6% in symptomatic patients and <3% in asymptomatic patients [6]. In general, CAS is preferred over CEA when patients have high surgical risks(Table 1).
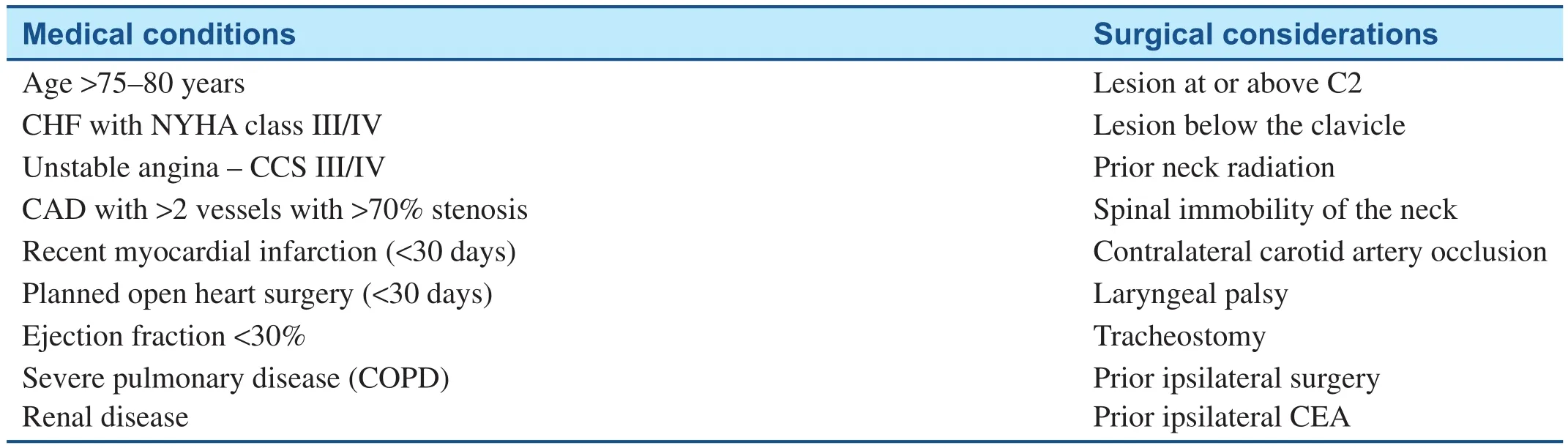
Table 1 High Surgical Risk Medical and Surgical Conditions.
Symptomatic High Surgical Risk Patients
One of the most important and well-designed studies to establish the equivalence of CAS with CEA was the Sapphire trial (Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy). In this study, both the operators (CAS and CEA) had comparable prior procedural experience. This study showed non-inferior 30-day (CAS,2.1% vs. CEA, 9.3%, P=0.95) and 1-year (CAS,16.3% vs. CEA, 20.0%, P=0.58) major adverse cardiac and cerebrovascular outcomes (MACCE)[4]. This equivalence was maintained at 3 years[8]. Currently, CAS coverage for reimbursement is limited to only those who have >70% stenosis and deemed to be high surgical risk patients,or if patients are enrolled in a US Food and Drug Administration (FDA) sanctioned clinical trial [7].
Symptomatic Average Surgical Risk Patient
Table 2 shows the serious shortcomings associated with early studies comparing CAS with CEA. Studies like EVA-3S, SPACE and ICSS had operators with almost negligible prior experience with CAS,and the use of an embolic protection device (EPD)was not mandatory. The latter being a standard of care in clinical practice in the US [13]. As noted in the table, some of the earlier studies had trainees perform CAS to accelerate enrollment. In light of the poor experience, rates of EPD deployment were low, leading to compromised procedural safety within the CAS cohort.
On the other hand, the CREST trial enrolled 1321 symptomatic patients and found no difference in 4-year composite cardiovascular and cerebrovascular outcomes. It was one of the best designed (comparable operator experience) and largest clinical trials comparing CAS and CEA (Table 2). Stroke rates remained similar between groups at 4 years[3]. Unlike the European trials, low volume operators within the CREST trial had a “vetted in” phase where they performed around 10–30 CAS. Based on the lead in phase, operators were selected to be part of the randomized clinical trial. Therefore, the trial compared operators (for CAS and CEA) with similar experience in each of the modalities, thereby bolstering the validity of trial results. Multi-societal guidelines recommend CAS over CEA for average surgical risk patients with the estimated peri-procedural stroke risk being <6% (Table 3).
Should Asymptomatic Patients be Treated?
Studies supporting carotid revascularization like ACAS (Asymptomatic Carotid Atherosclerosis Study) and ACST (Asymptomatic Carotid Sur-gery Trial) were performed in the pre-statin era.Given improvement in medical therapy since those studies were performed, the applicability of these study results is questionable. There are some observations that raise the question whether or not asymptomatic lesions need to be revascularized. Firstly, the 30-day MACCE for CAS(5.2%) and CEA (4.5%) within the CREST trial were historically low across all centers; and more importantly, improvements were seen both in CAS and CEA [3]. Secondly, two consecutive studies dealing with supra-aortic atherosclerotic disease have shown good outcomes with intensification of medical therapy (Table 4). The earlier WASID trial[16] compared warfarin to aspirin in symptomatic patients with intra-cranial disease. The 30-day and 1-year death/stroke outcomes are shown in Table 4. The subsequent SAMPRISS trial [17]compared stenting with intensive medical therapy(IMT) and IMT alone; again in patients with intracranial disease. When data from the patients in the IMT alone group were analyzed, they had outcomes at half the rate of those in the WASID trial,thereby underscoring the possible benefit afforded by IMT alone.
Thus, the medical community currently needs more definitive and contemporary evidence to determine if revascularization has added benefit in asymptomatic carotid artery stenosis in addition to intensive medical therapy. The CREST 2 trial( Figure 1) will randomize 2480 patients (1240 in each limb) to revascularization (CAS or CEA) with IMT vs. IMT alone in a parallel study design and will probably shed more light on this topic.
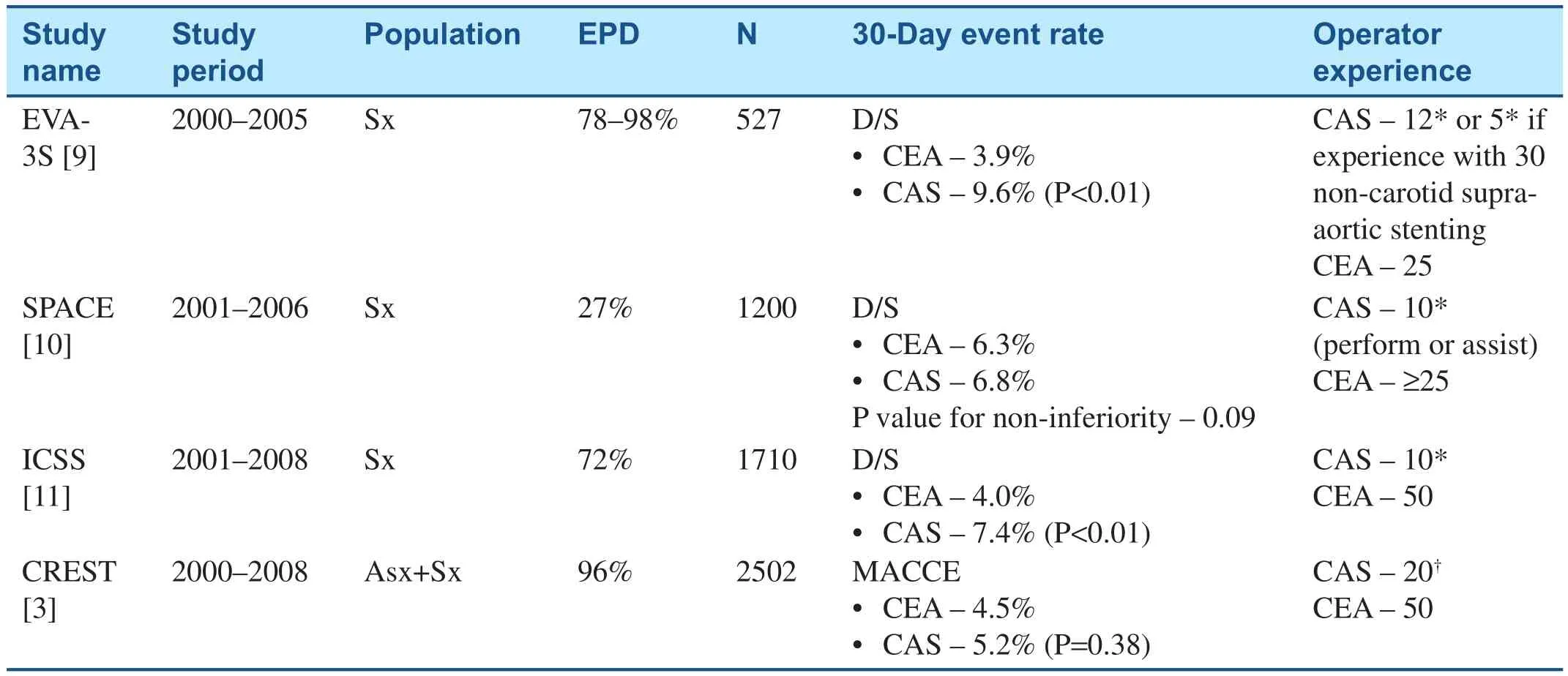
Table 2 Randomized Control Trials Suggesting the Existence of a Procedure-Related Learning Curve with CAS.
Current Data on Treating Asymptomatic Patients
A. High surgical risk patients– Though 30-day MACCE was similar between CEA and CAS within the SAPPHIRE trial [4] (CAS, 5.4% vs.CEA, 10.2%; P=0.20); CAS proved to have a significant edge over CEA with regards to 1-year(9.9% vs. 21.5%, P=0.02) MACCE outcomes. At 3 years, though the absolute number of MACCE events were lower in the CAS group, the differences were not statistically significant (CAS –24.6% vs. CEA – 26.9%, P>0.05) [8]. Refer to Table 3 for current multi-societal recommendations on treating such patients.
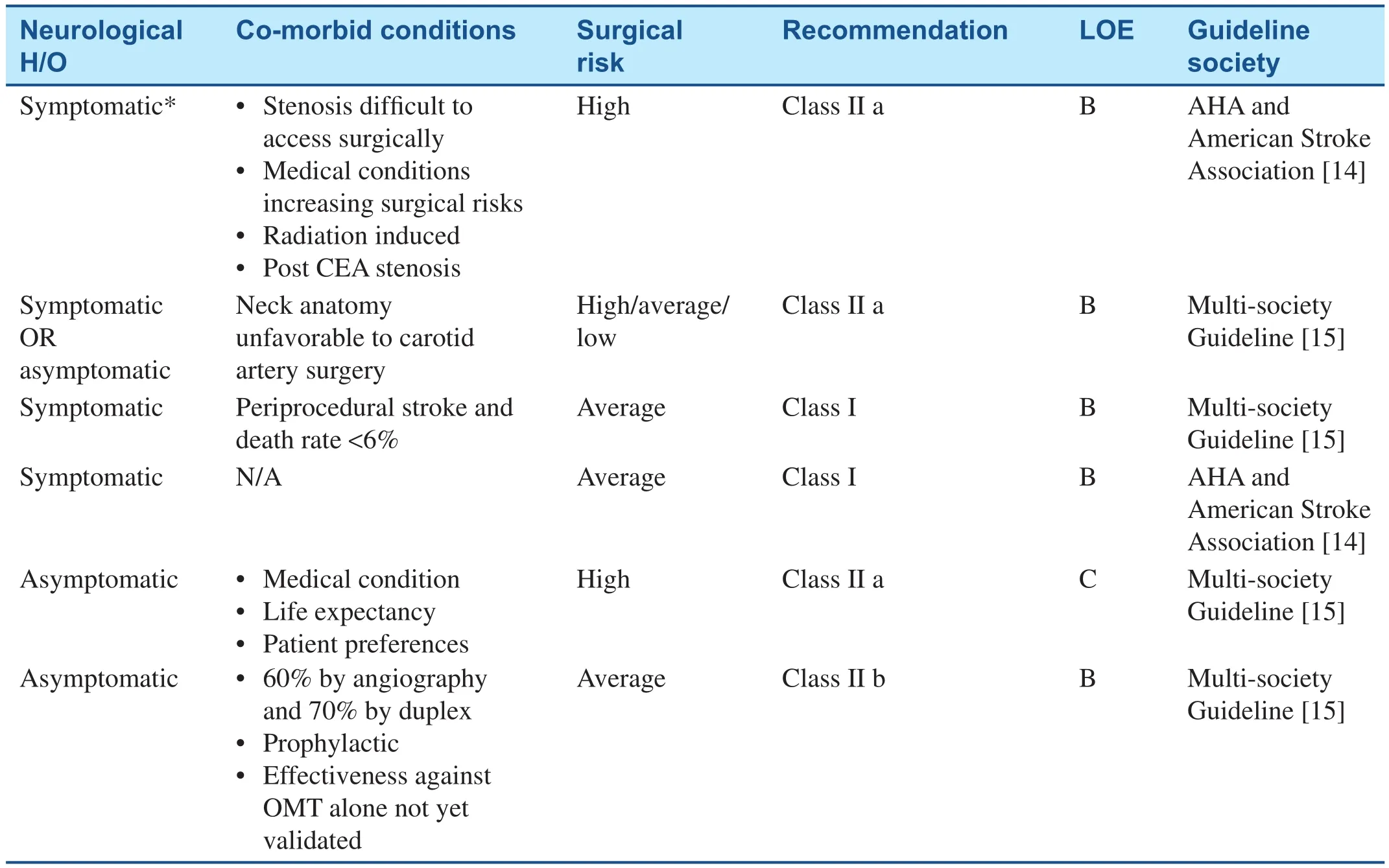
Table 3 Multidisciplinary Carotid Stent Guidelines.
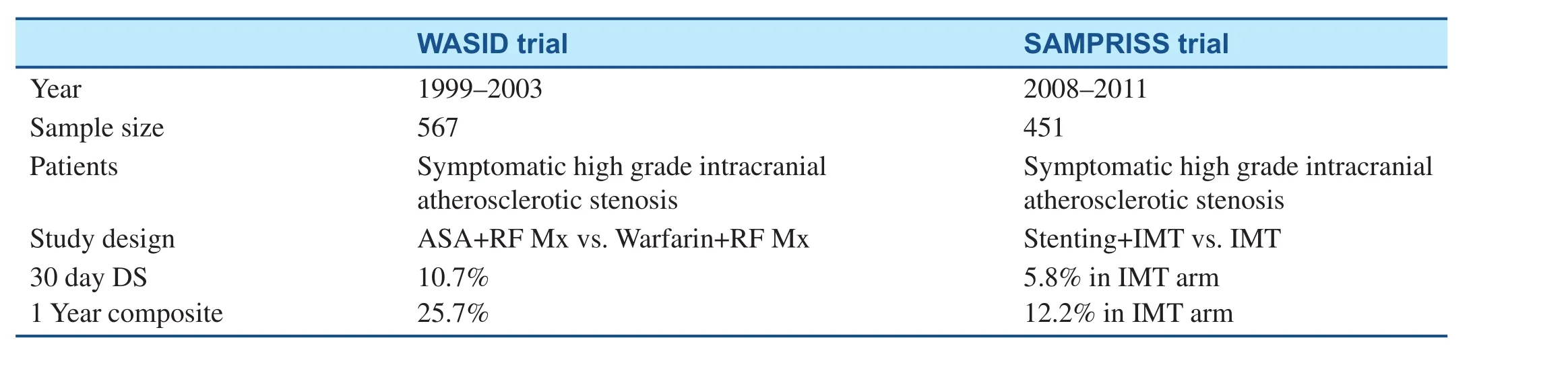
Table 4 Studies on Medical Therapy in Intra-Cranial Atherosclerotic Disease.
B. Average surgical risk patients– The CREST trial showed that in these patient groups, CAS was comparable to CEA with respect to a composite endpoint of MACCE (CAS, 5.6±1.0% vs.CEA, 4.9±1.0%; P=0.56 and rates of stroke up to 4 years (CAS, 4.5±0.9% vs. CEA, 2.7±0.8%;P=0.07) [3]. Refer to Table 3 for current multisocietal recommendations on treating such patients.
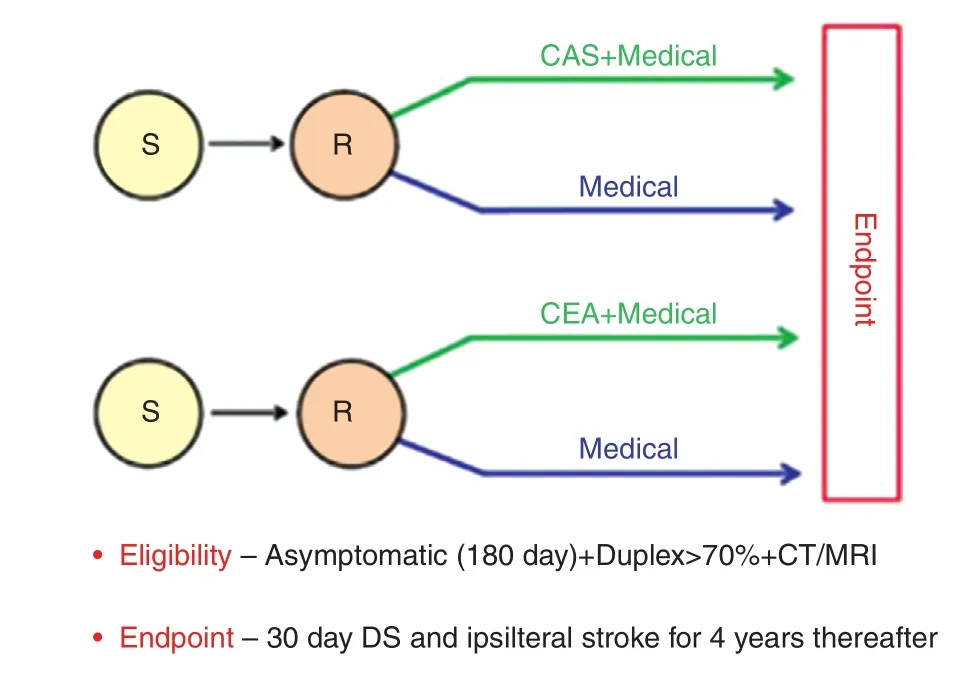
Figure 1 CREST-2 Parallel Study Design.S, Screening; R, randomization, CAS, carotid artery stenting;CEA, carotid end-arterectomy.Adapted from Brott et al. [18].
Procedural Risk Assessment
While the CREST trial showed a composite clinical equivalence of CAS and CEA with regards to the MACCE outcomes, the individual risks associated with each revascularization modality were slightly different. The CAS cohort had slightly higher minor strokes, while the CEA cohort had higher cranial nerve palsies and myocardial infarction [3]. Hence,risk stratification for CAS would help individualize carotid revascularization options and hopefully translate to best outcomes.
Table 5 shows the medical, anatomic, and procedural related variables contributing to procedural risk.
Recent publications provide risk models to assess procedural risk for mortality or stroke [19–21].These models encompass multiple variables known to increase risk of CAS-associated adverse outcomes and provide a summary risk score of death or stroke. Similar risk scores have been used effectively in various fields of medicine (e.g., CHADS2 score), and the development of an effective CAS score may help physicians with shared decision making with respect to the best modality of carotid revascularization. The NCDR CAS score [19] is a recently published score that assesses risk of periprocedural death and stroke from pre-procedural variables (before angiography). This score, developed by Hawkins et al., utilized the NCDR CARE registry database of 11,122 CAS procedures,asymptomatic and symptomatic, with low, average and high surgical risks. Figure 2 demonstrates the use of the CAS score for estimation of in-hospital stroke or death following carotid artery stenting.
Finally, despite development of risk models and predictors, clinicians should keep in mind that any anatomic or technical feature that prolongs instrumentation within the supra-aortic vasculature, or makes delivery of embolic protection device diffi-cult, would be best reserved for the surgical mode of revascularization. Other issues such as vascular access, chronic kidney dysfunction or contrast allergy should also be considered before deciding on a plan of care [7].
CAS – The Procedure
A. Patient selectionis the most important foundation on which a new CAS program should develop. A recently published executive consensus document (ECD) on CAS training and Credentialing [13] highlights the tenets on which a program needs to be designed and executed. In general, operators and institutions should self-evaluate themselves on the spectrum of annual CAS volume. This will help them select appropriate patients for their CAS program. Low volume operators and institutions should start with low risk CAS procedures and keep the complicated ones for proctoring. Also, patients inherently at high surgical risk and/or symptomatic may be the target candidates that a new program should enroll initially [7].
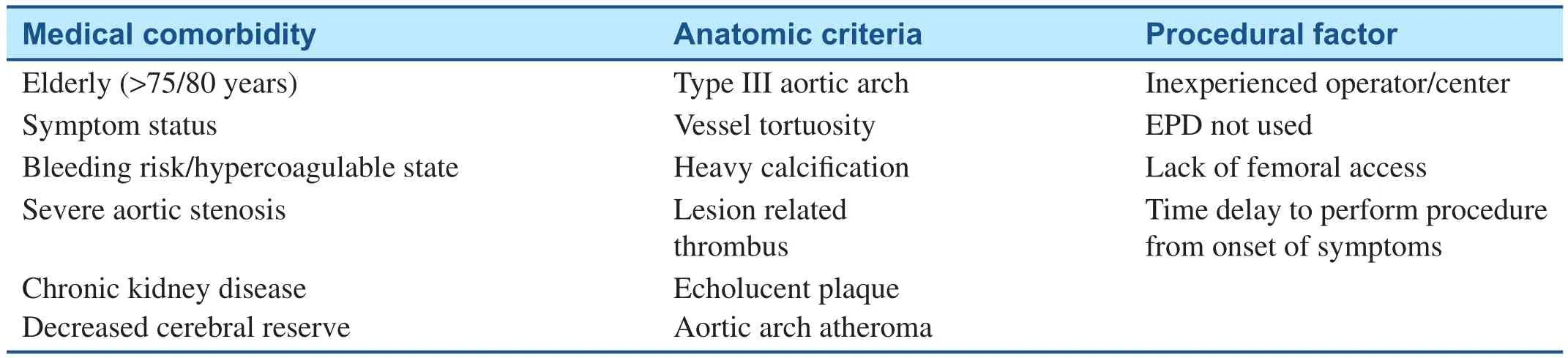
Table 5 Features Suggesting Increased Risk of Carotid Stent Procedures.
B. Access – Though performed via the transfemoral route traditionally, the newer generation of interventional operators have adopted to radial access for CAS. A recent randomized controlled trial comparing the two access sites showed no difference in MACCE or access related complications [23]. This study established the safety and feasibility of performing CAS via the trans-radial route, albeit with some shortcomings of higher access turn-over rates and higher radiation compared to femoral access routes. On the other hand, the trans-radial approach provided the benefit of a shorter hospital stay [23]. In general, radial access provides greater and prompt post-procedural ambulation which may sometimes be important to circumvent post- procedural hemodynamic issues. Also trans-radial can make some anatomical variants(Right carotid intervention via right radial artery in type III arch, Bovine left carotid artery via right radial artery etc.) more amenable to intervention compared to the trans-femoral route.
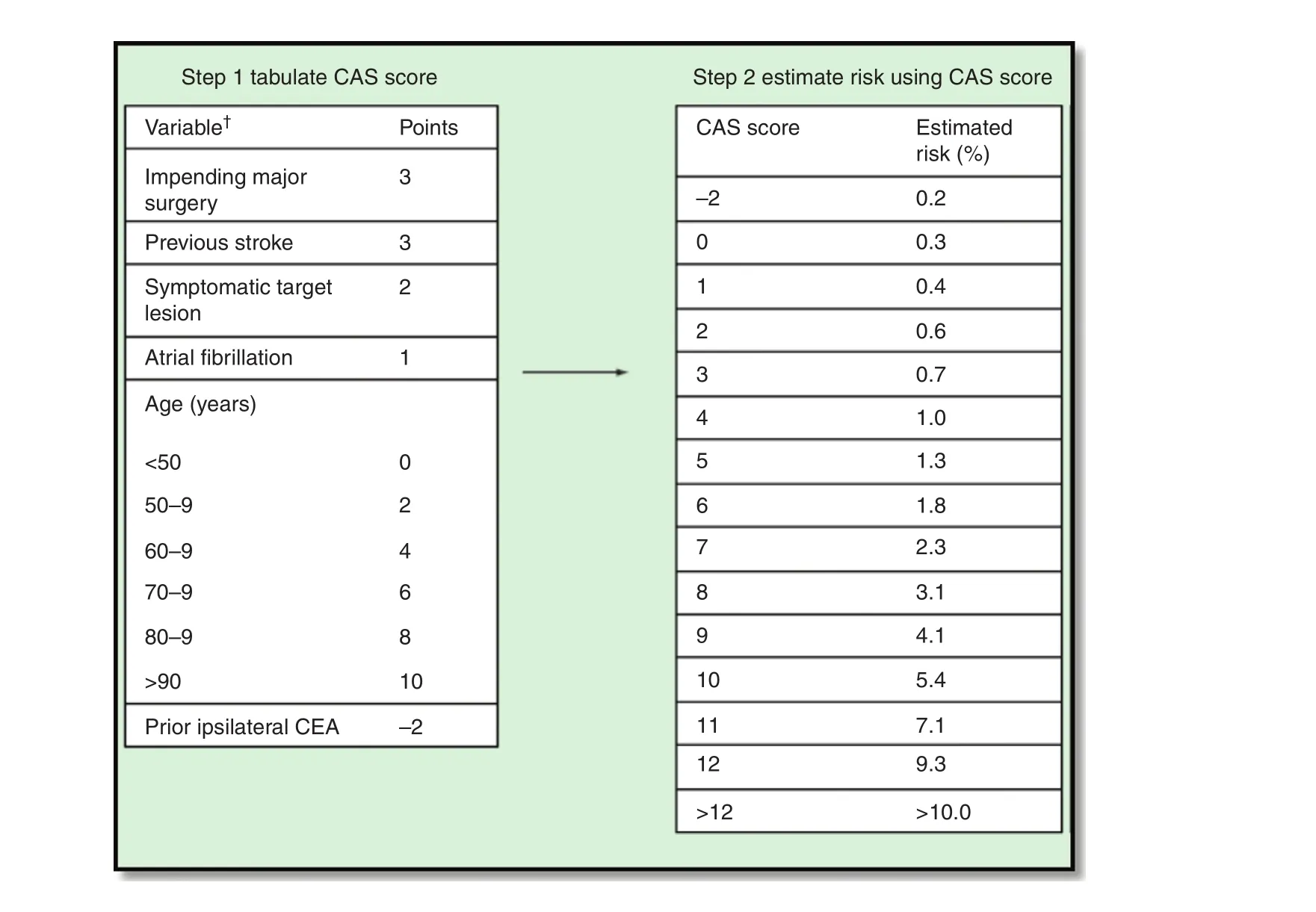
Figure 2 The NCDR CAS Score.Reproduced with permission from Hawkins et al. [22].
Despite technological advancement, technique refinement and contemporary studies showing equivalence of CAS and CEA with regards to MACCE, the trans-femoral CAS (TF-CAS) is associated with a higher number of peri-procedural cerebrovascular events, especially within the 24 hour post-procedure period [24, 25]. This has been attributed to unprotected catheterization (Pre-EPD) of carotid arteries through diseased and difficult aortic arches [26]. Consequently, the concept of CAS via direct carotid access has gained some leverage. The safety and feasibility of this approach was demonstrated in the ROADSTER trial [24]. This was a prospective, single-arm, multicenter clinical trial that evaluated the use of the ENROUTE Transcarotid neuroprotection system (NPS; Silk Road Medical Inc., Sunnyvale, CA, USA) during CAS pro-cedures performed in patients considered high risk for complications from carotid endarterectomy. Essentially this entailed a hybrid approach where the common carotid artery (CCA) is occluded proximally via surgical means, and the NPS is delivered distal to the surgical occlusion. This equipment allows flow reversal (CCA to femoral vein) while also allowing CAS via carotid access distal to the occlusion. This trial showed an excellent 30-day stroke rate of 1.4%,the lowest observed in any kind of prospective studies. This technique may also have significant advantages over traditional CEA in light of its lower cranial nerve injury and oro-pharyngeal dysfunction rates.
C. Procedural anti-coagulation– As an extension to the hemorrhagic benefit observed with bivalirudin in the coronary era, several operators had started using bivalirudin based on limited singlecen
ter retrospective feasibility studies [27–29].However, large scale real world data were limited until the study by Wayangankar et al. [30] which used the national registry of CAS (NCDR-CARE Registry) to compare CAS procedures with bivalirudin (n=3555) with unfractionated heparin(UFH, n=3555) in a propensity matched fashion.This study showed that bivalirudin was associated with lower rates of hemorrhagic outcomes compared with UFH during the index hospitalization for carotid artery stenting. In-hospital and 30-day ischemic events were similar between the two groups (Table 6). Until the results of ENDOMAX trial (ENDOvascular interventions with angioMAX, n=4000) are published, this is the largest real world study we have to draw inferences from. However, operators should keep in mind that variables other than bleeding(cost, presence of heparin induced thrombocytopenia, and lack of antidote with bivalirudin)may be instrumental in choosing the type of anticoagulant.
Embolic Protection Device
Data on neuro-protection relies on summary data in the form of meta-analysis or systematic reviews.This is because the rates of clinical cerebrovascular events are small and designing a randomized control trial would be technically and financially difficult. One such study was by Garg et al. [31] that reviewed data from procedures done between 1995 and 2007 and assessed the association of 30-day peri-procedural stroke. Using pooled analysis of 134 articles (n>23,000), the authors showed that compared to procedures without embolic protection devices, patients with neuro-protection did better with respect to post-procedural stroke at 30 days(RR – 0.62, 95% CI – 0.54–0.72, P<0.01) [31]. A similar benefit was observed in a pooled analysis by Touze et al. which showed a stroke and death benefit in favor of neuro-protection (RR – 0.57, 95%CI – 0.43–0.76, P<0.01) [32].
Embolic protection can be of the following three types
•Distal non-occlusive system– Distal embolic protection filters. This preserves blood flow but prevents distal embolization. Table 7 shows the current available distal EPD filters in practice.
•Distal Occlusive system– GuardWire Protection System (PercuSurge, Sunnyvale, CA, USA)occludes distally, and an aspiration catheter Export (Medtronic) provides suction. This technique relies on prevention of distal embolization by preventing both blood flow and embolic debris.
•Proximal protection devicesrely on flow reversal after occluding CCA and ECA flow either by direct aspiration (Mo.Ma; Medtronic,Minneapolis, MN, USA) or via a filter into the venous system (GORE Flow reversal system,WL Gore and Associates, Flagstaff, AZ, USA).The biggest advantage of this concept is that the EPD does not cross the lesion and hence decreases the chance of manipulation induced distal embolization. The MICHI neuro-protection system (Silk Road Medical Inc., Sunnyvale, CA, USA) is similar to the GORE system with the difference that it is used with direct carotid access – obviating the need to deal with hostile arches [33].
One of the first randomized control trials comparing the two strategies (proximal vs. distal protection) showed that new ipsilateral cerebral lesions with diffusion weighted imaging lesions were lesser with proximal protection device MoMa (Invatec/Medtronic Vascular Inc., Santa Rosa, CA, USA)compared to distal protection device – Angioguard(Cordis Corporation, Bridgewater, NJ, USA)[34]. Another single center study (n=140 patients)showed no difference in 30-day clinical outcomes when the two strategies were compared [35]. A recent publication from the NCDRs CARE registry (n=10,246) also showed no clinical differences within the two strategies [36]. Since large scale randomized studies would not be feasible to answer this question, with the current base of evidence, it can be safely concluded that either type of neuroprotection would be equally beneficial as long as it is used consistently and precisely.
D. Intra-cerebral angiography– These should be performed before and after carotid intervention. A pre-stenting intra-cerebral angiographyprovides good information about vascular anatomy (patency, presence of collaterals, Circle of Willis, dominance, isolated hemisphere) that not only helps with patient selection but also helps to maintain a template of pre-intervention status should complications occur [7]. Likewise,intra-cerebral angiography post-stenting helps to detect any kind of distal embolization in the form of intra-cerebral vascular “cut off.” Ideally two orthogonal views (AP and lateral) are recommended.
E. Balloon dilatations– Traditionally, the CAS procedure consisted of an embolic protection device placement, pre-stent balloon dilatation with a <4 mm balloon at nominal pressures, followed by placement of a self-expanding stent,and eventually ending with a post-stent balloon inflation (≤5 mm balloon). While the prestent balloon inflation helps to allow the stent to pass, more importantly it provides a glimpse of hemodynamic response the patient may have with stent and post-dilatation. This step helps re-adjust medications and fluids before proceeding and stenting in a more controlled manner. Alternatively, some studies have alluded to the drawbacks of routine post-dilatations,mainly stemming from increased microscopic emboli (Doppler signals in intra-cranial imaging). The practice of post-dilatation doesn’t improve restenosis rates, and self-expanding stents eventually expand to their nominal diameters post stenting.
F. Carotid stent– Contemporary carotid stents are self-expanding by design, self-tapering or with a manufactured taper to deal with the discordant sizes of the internal carotid artery and common carotid artery. Though studies [37] have found no difference between closed and open cell types,operators are inclined to use the more conformable open cell type stents in more angulated lesions, whereas a higher surface area afforded by closed cell stents may be best suited for straighter lesions. Table 8 shows current available stents.
G. Treatment of ostial common carotid artery– Most trials comparing CAS and CEA evaluate the two modalities with respect to internal carotid artery interventions. A special subset of patient to consider is the ostial common carotid artery. Surgical treatment for such lesions is usually a carotid-subclavian bypass which is often limited by higher than average peri-procedural stroke outcomes [38, 39]. There exists limited data on how to treat such patients via CAS since these lesions are rare, and when present pose technical challenge to engage, cross, deliver and deploy interventional equipment [40]. Cam et al.report a single center experience with 17 such patients who underwent CAS from 2005 to 2011[40]. Most of the lesions involved the left CCA.Though various techniques have been described by the authors, the one that stands out is the one that they used in all the latter cases. This involved using a modified AL-1 catheter to deliver long 300 cm 014 wires (one of them being the filter wire) across the lesion, pre-dilatation followed by delivery of the stent mounted on both wires to provide good support for delivery and deployment of the stent. The authors report excellent short and long-term outcomes with this technique [40]. EPD is removed first followed by the buddy wire.
H. Patients with significant coronary artery disease– Around 10% of patients undergoing open heart surgery (OHS) have severe carotid artery disease (stenosis >80%) [41]. Due to lack of randomized data, clinical practice revolves around three strategies based on local practice patterns – staged CEA-OHS; combine CEAOHS; and staged CAS-CEA. Shishehbor et al.evaluated 350 such patients from 1997 to 2009 at the Cleveland Clinic. The authors found that despite CAS-OHS group being a higher risk group (higher pre-procedural stroke rates) and undergoing more complex OHS, they ended up with similar peri-procedural composite outcomes (1 year death, stroke, MI) compared to combined CEA-OHS and significantly better outcomes when compared to staged CEA-OHS[42]. When outcomes were evaluated after one year, the staged CAS-OHS strategy outscored both combined CEA-OHS and staged CEA-OHS. While the staged strategies were associated with higher inter-stage myocardial infarctions, the combined strategy was asso-ciated with more peri-procedural stroke [42].The lower late composite outcomes associated with staged CAS-OHS were driven by lower mortality; underscoring the importance of this strategy in this high risk group of patients.Until prospective randomized data becomes available, this study may provide some guidance to clinicians to provide best individualized treatment to this high risk sub-group of patients. Finally, hybrid approaches of combined CAS-OHS still needs to be explored and evaluated.
Learning Curve
Carotid artery stenting is a technically demanding procedure with a significant learning curve associated. Importantly, this learning curve is associated with technical success and peri-procedural outcomes [43]. There are two components of the learning curve – operator and institutional. Multiple studies have shown that as the operator gained more CAS volume, rates of peri-procedural complications declined [28, 44–46]. Similarly, institutions with higher volume fared better than lowervolume ones [43, 46–49]. Availability of technical mentoring, peer-to-peer feedback on patient and device selection provides an ideal milieu to ensure patient safety even with novices. Wayangankar et al. [43] summarized operator and learning curve thresholds to attain acceptable per- procedural death/stroke outcomes (Tables 9 and 10). Prior consensus statements by various societies on credentialing and training operators for CAS have been non-uniform and probably unrealistic in the contemporary setting. While the Italian SPREAD joint committee consensus document [50] recommends >75 cases (at least 50 as primary operator)to achieve competency and 50 per year to maintain, the prior 2007 US document (SCAI/SVM/SVS) was a bit liberal and stated that 25 supervised operators (half as primary operator) need to be performed to achieve competency. It did not provide thresholds for maintaining competency. The recently published 2015 SCAI/SVM CAS training and credentialing document [12] underscores the importance of annual CAS volume. “Maintenance”volume is important since studies have shown that increased time interval between consecutive CAS procedures is associated with greater risk of death, MI or stroke at 30 days [51]. With declining volumes, multiple competing sub-specialties,and issues with re-imbursement within the US,applicability of aggressive European CAS guidelines (on operator thresholds) would be difficult and prohibitive. The newer 2015 SCAI/SVM competency statement [12] recognizes this dilemma,and for the first time, has recommended a more realistic maintenance volume of 10–15 cases/year(threshold for achieving competency being 25 cases). Additionally, the document recommends double scrubbing, proctoring, and simulation as tools to complement clinical exposure for low volume operators.
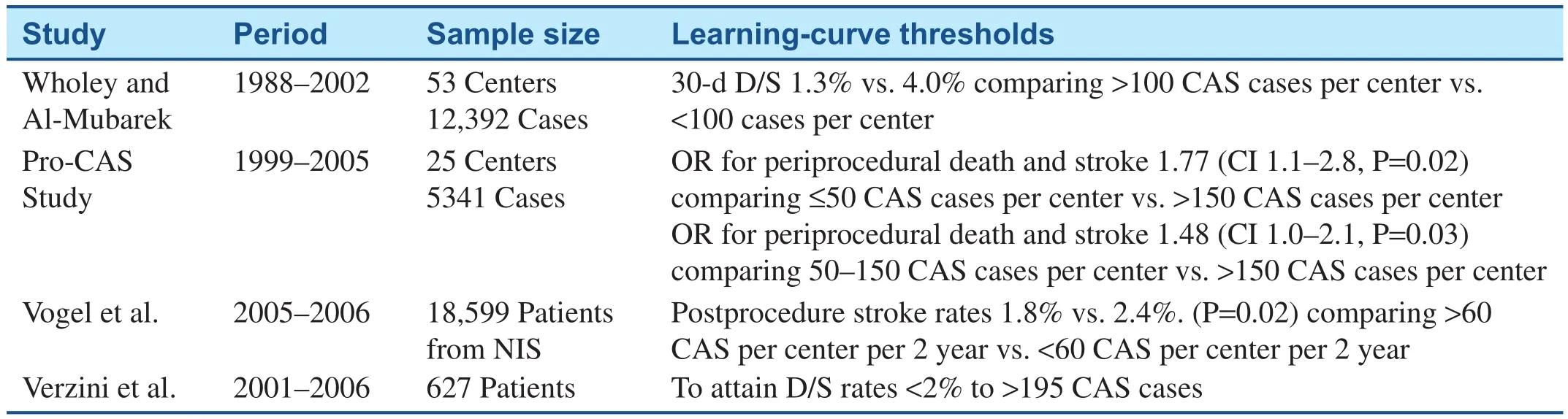
Table 10 Data on Learning Curve Thresholds for Institutions.
Challenges for Budding Operators
• The role of carotid revascularization is recently being challenged in asymptomatic patients. The CREST2 trial may offer some insights on the best strategy to manage such patients, and may have future implications on CAS procedural volume.
• In the US, the Centers for Medicare Services(CMS) has not yet revised the current national coverage determination (NCD) to correspond with the FDA approval of CAS devices with indications. Moreover there is a marked disconnect between CMS coverage and current guidelines. Current NCD limit a patient’s access to CAS who could have possible benefit. Hence,uncertainties in reimbursements will further worsen the CAS volume.
• Such an atmosphere may force patients and physicians into poor patient selection that may ultimately lead to worse clinical outcomes.
• Finally, this decline in CAS volume and the complexity of decision-making would magnify the current challenges in training and in maintaining competent CAS operators.
Conflict of Interest
The authors declare no conflict of interest.
REFERENCES
1. Fisher M. Occlusion of the internal carotid artery. AMA Arch Neurol Psychiatry 1951;65:346–77.
2. Mayberg MR, Wilson SE, Yatsu F, Weiss DG, Messina L, Hershey LA, et al. Carotid endarterectomy and prevention of cerebral ischemia in symptomatic carotid stenosis. Veterans affairs cooperative studies program 309 trialist group. J Am Med Assoc 1991;266:3289–94.
3. Brott TG, Hobson RW 2nd, Howard G, Roubin GS, Clark WM,Brooks W, et al. Stenting versus endarterectomy for treatment of carotid-artery stenosis. N Engl J Med 2010;363:11–23.
4. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med 2004;351:1493–501.
5. Rothwell PM, Slattery J, Warlow CP. A systematic review of the risks of stroke and death due to endarterectomy for symptomatic carotid stenosis. Stroke 1996;27:260–5.
6. Biller J, Feinberg WM, Castaldo JE, Whittemore AD, Harbaugh RE,Dempsey RJ, et al. Guidelines for carotid endarterectomy: a statement for healthcare professionals from a special writing group of the stroke council, american heart association. Stroke 1998;29:554–62.
7. White CJ. Carotid artery stenting. J Am Coll Cardiol 2014;64:722–31.
8. Gurm HS, Yadav JS, Fayad P,Katzen BT, Mishkel GJ, Bajwa TK,et al. Long-term results of carotid stenting versus endarterectomy in high-risk patients. N Engl J Med 2008;358:1572–9.
9. Mas JL, Chatellier G, Beyssen B,Branchereau A, Moulin T, Becquemin JP, et al. Endarterectomy versus stenting in patients with symptomatic severe carotid stenosis. N Engl J Med 2006;355:1660–71.
10. Ringleb PA, Allenberg J, Bruckmann H, Eckstein HH, Fraedrich G, Hartmann M, et al. 30 day results from the space trial of stent-protected angioplasty versus carotid endarterectomy in symptomatic patients: a randomised non-inferiority trial. Lancet 2006;368:1239–47.
11. Ederle J, Dobson J, Featherstone RL, Bonati LH, van der Worp HB,de Borst GJ, et al. Carotid artery stenting compared with endarterectomy in patients with symptomatic carotid stenosis (international carotid stenting study): an interim analysis of a randomised controlled trial. Lancet 2010;375:985–97.
12. Aronow HD, Collins TJ, Gray WA,Jaff MR, Kluck BW, Patel RA,et al. SCAI/SVM expert consensus statement on carotid stenting: training and credentialing for carotid stenting. Catheter Cardiovasc Interv 2016;87(2):188–99.
13. Roffi M, Cremonesi A. Carotid artery stenting versus endarterectomy for carotid stenosis. Lancet 2010;376:327; author reply 327–8.14. Furie KL, Kasner SE, Adams RJ,Albers GW, Bush RL, Fagan SC,et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the American heart association/American stroke association.Stroke 2011;42:227–76.
15. Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL, et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines,and the American Stroke Association, American Association of Neuroscience Nurses, American Association of Neurological Surgeons,American College of Radiology,American Society of Neuroradiology, Congress of Neurological Surgeons, Society of Atherosclerosis Imaging and Prevention, Society for Cardiovascular Angiography and Interventions, Society of Interventional Radiology, Society of NeuroInterventional Surgery,Society for Vascular Medicine, and Society for Vascular Medicine. J Am Coll Cardiol 2011;57:1002–44.
16. Kasner SE, Lynn MJ, Chimowitz MI, Frankel MR, Howlett-Smith H, Hertzberg VS, et al. Warfarin vs aspirin for symptomatic intracranial stenosis: subgroup analyses from wasid. Neurology 2006;67:1275–8.
17. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 2011;365:993–1003.
18. Brott TG. SVIN: update on crest-2 trial. Baltimore, MD, USA: Mayo Clinic; 2013.
19. Hawkins BM, Kennedy KF, Giri J,Saltzman AJ, Rosenfield K, Drachman DE, et al. Pre-procedural risk quantification for carotid stenting using the cas score: a report from the NCDR care registry. J Am Coll Cardiol 2012;60:1617–22.
20. Wimmer NJ, Yeh RW, Cutlip DE, Mauri L. Risk prediction for adverse events after carotid artery stenting in higher surgical risk patients. Stroke 2012;43:3218–24.
21. Touze E, Trinquart L, Felgueiras R, Rerkasem K, Bonati LH,Meliksetyan G, et al. A clinical rule(sex, contralateral occlusion, age,and restenosis) to select patients for stenting versus carotid endarterectomy: systematic review of observational studies with validation in randomized trials. Stroke 2013;44:3394–400.
22. Hawkins BM, Abu-Fadel MS,Rosenfield K. Risk assessment for carotid artery stenting. Expert Rev Cardiovasc Ther 2014;12:565–72.
23. Ruzsa Z, Nemes B, Pinter L, Berta B, Toth K, Teleki B, et al. A ran-domised comparison of transradial and transfemoral approach for carotid artery stenting: RADCAR(radial access for carotid artery stenting) study. EuroIntervention 2014;10:381–91.
24. Kwolek CJ, Jaff MR, Leal JI,Hopkins LN, Shah RM, Hanover TM, et al. Results of the roadster multicenter trial of transcarotid stenting with dynamic flow reversal. J Vasc Surg 2015;62:1227–34 e1221.
25. Murad MH, Coto-Yglesias F,Zumaeta-Garcia M, Elamin MB, Duggirala MK, Erwin PJ,et al. A systematic review and meta- analysis of the treatments of varicose veins. J Vasc Surg 2011;53:49S–65S.
26. Gupta N, Corriere MA, Dodson TF,Chaikof EL, Beaulieu RJ, Reeves JG, et al. The incidence of microemboli to the brain is less with endarterectomy than with percutaneous revascularization with distal filters or flow reversal. J Vasc Surg 2011;53:316–22.
27. Stabile E, Sorropago G, Tesorio T,Popusoi G, Ambrosini V, Mottola MT, et al. Heparin versus bivalirudin for carotid artery stenting using proximal endovascular clamping for neuroprotection: results from a prospective randomized study. J Vasc Surg 2010;52:1505–10.
28. Lin PH, Bush RL, Peden EK, Zhou W, Guerrero M, Henao EA, et al.Carotid artery stenting with neuroprotection: assessing the learning curve and treatment outcome. Am J Surg 2005;190:850–7.
29. Cogar BD, Wayangankar SA, Abu-Fadel M, Hennebry TA, Ghani MK, Kipperman RM, et al. Clinical safety of bivalirudin in patients undergoing carotid stenting. J Invasive Cardiol 2012;24:202–5.
30. Wayangankar SA, Abu-Fadel MS,Aronow HD, Kennedy KF, Gupta R, Yeh RW, et al. Hemorrhagic and ischemic outcomes after bivalirudin versus unfractionated heparin during carotid artery stenting:a propensity score analysis from the NCDR. Circ Cardiovasc Interv 2013;6:131–8.
31. Garg N, Karagiorgos N, Pisimisis GT, Sohal DP, Longo GM, Johanning JM, et al. Cerebral protection devices reduce periprocedural strokes during carotid angioplasty and stenting: a systematic review of the current literature. J Endovasc Ther 2009;16:412–27.
32. Touze E, Trinquart L, Chatellier G, Mas JL. Systematic review of the perioperative risks of stroke or death after carotid angioplasty and stenting. Stroke 2009;40:e683–93.
33. Morr S, Lin N, Siddiqui AH.Carotid artery stenting: current and emerging options. Med Devices(Auckl) 2014;7:343–55.
34. Cano MN, Kambara AM, de Cano SJ, Pezzi Portela LA, Paes AT,Costa JR Jr, et al. Randomized comparison of distal and proximal cerebral protection during carotid artery stenting. JACC Cardiovasc Interv 2013;6:1203–9.
35. Mokin M, Dumont TM, Chi JM,Mangan CJ, Kass-Hout T, Sorkin GC, et al. Proximal versus distal protection during carotid artery stenting: analysis of the two treatment approaches and associated clinical outcomes. World Neurosurg 2014;81:543–8.
36. Giri J, Parikh SA, Kennedy KF,Weinberg I, Donaldson C, Hawkins BM, et al. Proximal versus distal embolic protection for carotid artery stenting: a national cardiovascular data registry analysis. JACC Cardiovasc Interv 2015;8:609–15.
37. Timaran CH, Rosero EB, Higuera A, Ilarraza A, Modrall JG, Clagett GP. Randomized clinical trial of open-cell vs closed-cell stents for carotid stenting and effects of stent design on cerebral embolization. J Vasc Surg 2011;54:1310–6.e1311;discussion 1316.
38. Payne DA, Hayes PD, Bolia A,Fishwick G, Bell PR, Naylor AR.Cerebral protection during open retrograde angioplasty/stenting of common carotid and innominate artery stenoses. Br J Surg 2006;93:187–90.
39. Berguer R, Morasch MD, Kline RA, Kazmers A, Friedland MS.Cervical reconstruction of the supra-aortic trunks: a 16-year experience. J Vasc Surg. 1999;29:239–46; discussion 246–8.
40. Cam A, Muhammad KI, Shishehbor MH, Bajzer CT, Kapadia SR.Technique and outcome of ostial common carotid artery stenting: a single centre experience. EuroIntervention 2012;7:1210–5.
41. Schwartz LB, Bridgman AH, Kieffer RW, Wilcox RA, McCann RL, Tawil MP, et al. Asymptomatic carotid artery stenosis and stroke in patients undergoing cardiopulmonary bypass. J Vasc Surg 1995;21:146–53.
42. Shishehbor MH, Venkatachalam S, Sun Z, Rajeswaran J, Kapadia SR, Bajzer C, et al. A direct comparison of early and late outcomes with three approaches to carotid revascularization and open heart surgery. J Am Coll Cardiol 2013;62:1948–56.
43. Wayangankar SA, Aronow HD.Carotid artery stenting. Interv Cardiol Clin 2013;3:91–103.
44. Ahmadi R, Willfort A, Lang W,Schillinger M, Alt E, Gschwandtner ME, et al. Carotid artery stenting: effect of learning curve and intermediate-term morphological outcome. J Endovasc Ther 2001;8:539–46.
45. Nallamothu BK, Gurm HS, Ting HH, Goodney PP, Rogers MA,Curtis JP, et al. Operator experience and carotid stenting outcomes in medicare beneficiaries. J Am Med Assoc 2011;306:1338–43.
46. Gray WA, Rosenfield KA, Jaff MR, Chaturvedi S, Peng L, Verta P. Influence of site and operator characteristics on carotid artery stent outcomes: analysis of the capture 2 (carotid acculink/accunet post approval trial to uncover rare events) clinical study. JACC Cardiovasc Interv 2011;4:235–46.
47. Verzini F, Cao P, De Rango P,Parlani G, Maselli A, Romano L,et al. Appropriateness of learning curve for carotid artery stenting: an analysis of periprocedural complications. J Vasc Surg 2006;44:1205–11; discussion 1211–2.
48. Staubach S, Hein-Rothweiler R,Hochadel M, Segerer M, Zahn R,Jung J, et al. The role of endovascular expertise in carotid artery stenting: results from the alkk-casregistry in 5,535 patients. Clin Res Cardiol 2012;101:929–37.
49. Theiss W, Hermanek P, Mathias K,Bruckmann H, Dembski J, Hoffmann FJ, et al. Predictors of death and stroke after carotid angioplasty and stenting: a subgroup analysis of the pro-cas data. Stroke 2008;39:2325–30.
50. Cremonesi A, Setaccic, Bignamini A, Bolognese L, Briganti F,Di Sciascio G, et al. Carotid artery stenting: first consensus document of the iccs-spread joint committee.Stroke 2006;37:2400–9.
51. Calvet D, Mas JL, Algra A, Becquemin JP, Bonati LH, Dobson J, et al. Carotid stenting: is there an operator effect? A pooled analysis from the carotid stenting trialists’ collaboration. Stroke 2014;45:527–32.
 Cardiovascular Innovations and Applications2016年2期
Cardiovascular Innovations and Applications2016年2期
- Cardiovascular Innovations and Applications的其它文章
- Transient Pulmonary Atelectasis after Ketamine Sedation during Cardiac Catheterization in Spontaneously Breathing Children with Congenital Heart Disease
- Identification and Management of Iatrogenic Aortocoronary Dissection
- Cardiovascular Abnormalities Among Patients with Spontaneous Subarachnoid Hemorrhage.A Single Center Experience
- Coronary Artery Chronic Total Occlusion
- The Transradial Approach for Cardiac Catheterization and Percutaneous Coronary Intervention: A Review
- The Future of Transcatheter Therapy for Mitral Valve Disease
