MRI对乳腺癌新辅助化疗后腋窝淋巴结的评估
李富,曾健△,李春燕,罗铭,孔震
MRI对乳腺癌新辅助化疗后腋窝淋巴结的评估
李富1,曾健1△,李春燕2,罗铭1,孔震1
摘要:目的探讨MRI对乳腺癌新辅助化疗后腋窝淋巴结(ALN)评估的价值。方法对44例乳腺癌患者进行新辅助化疗(NAC),比较患者NAC前和NAC4周期后MRI测量患侧ALN直径、肿瘤表观扩散系数(ADC)值变化及其间接相关性;比较MRI与病理对患侧腋窝阳性淋巴结的检测结果。结果所有患者均完成了4周期的NAC,有反应(CR+PR)率为72.73%(32/44),无反应(SD+PD)率为27.27%(12/44)。有反应组NAC前后的ALN最大直径由(1.37±1.06)cm缩短为(0.90±0.76)cm,NAC前后的ADC值由(0.91±0.28)×10-3mm2/s增加到(1.01±0.32)×10-3mm2/s (P<0.01);NAC前后的ADC值变化(△ADC)与腋窝淋巴结NAC前后最大直径的变化(△L)不相关(r=0.131,P= 0.413)。NAC后MRI评估ALN的敏感度100%,特异度62.5%,Kappa值0.68。结论MRI功能指标ADC值不能作为早期间接反映NAC后ALN的疗效的独立指标,但MRI仍是评估NAC后ALN状态的敏感指标。
关键词:乳腺肿瘤;化学疗法,辅助;磁共振成像;信号处理,计算机辅助;淋巴转移;治疗结果;新辅助化疗;表观扩散系数
乳腺癌位居女性恶性肿瘤第1位,每年新发病例约21万,其发病率、死亡率呈逐年上升趋势,治疗是以手术为主的综合治疗[1-2]。新辅助化疗(neoadju⁃vant chemotherapy,NAC)是对局部进展期乳腺癌(1ocally advanced breast cancer,LABC)患者术前进行的全身性辅助化疗,以缩小肿瘤,有效清除淋巴结及远处潜在的微转移病灶,使手术切除甚至保乳成为可能[1]。磁共振扩散加权成像(MRI-DWI)的功能参数肿瘤表观扩散系数(ADC)值能早期从分子水平反映肿瘤的新辅助化疗疗效[3]。腋窝淋巴结(axillary lymph node, ALN)疗效是NAC疗效评估不可或缺的一部分,ALN状态的评估是乳腺癌腋窝处理的关键,但NAC后肿瘤ADC值变化能否间接用于ALN化疗疗效的早期评估及MRI对ALN状态的评估与病理的等效性如何是一个值得探讨的临床问题。
1 资料与方法
1.1一般资料收集我院2011年1月—2013年12月收治的44例乳腺癌患者NAC前和NAC4个周期后MRI资料进行分析,所有患者均符合NAC标准并签署相关的检查治疗同意书。纳入标准:(1)经空芯针穿刺活检病理证实为乳腺癌。(2)均有完整病史、临床检查、双侧乳腺超声及MRI-DWI相关检查资料。(3)经肝脏B超、X线胸片和全身骨扫描排除远处转移。(4)MRI检查病灶直径≥2.5 cm且为单一病灶,增强后病灶表现为团块状强化。(5)行NAC前、NAC4个周期后接受2次乳腺MRI检查,每次检查参数不变。排除标准:原发炎性乳腺癌或乳腺出现转移性病灶。所有患者均经穿刺病理组织学确诊为乳腺癌并同意接受NAC,年龄26~62岁,平均年龄(49.3±12.4)岁,参考2010年NCCN指南(V.2.2010)的cTNM分期标准:T2期14例,T3期25例,T4 期5例。
1.2方法参考V.2.2010,根据患者病理结果选择相应的NAC方案,20例采用紫杉醇类联合铂类化疗方案。16例采用紫杉醇类联合蒽环类化疗,7例采用紫杉醇类联合卡培他滨化疗方案,1例采用紫杉醇类、铂类联合赫赛汀化疗方案。在出现骨髓抑制时予以升高白细胞的支持治疗。MRI检查:采用我院3.0T超导型磁共振仪和双侧乳腺表面线圈,造影剂为钆喷酸葡胺注射液。患者采取俯卧位,双侧乳腺自然悬垂于专用乳腺表面线圈内,使用加压器。所有研究对象均进行双侧乳腺常规MRI和动态增强成像(包括ADC值测定、时间-信号曲线)。
1.3腋窝淋巴结最大直径及ADC值以MRI三维重建图像中最大淋巴结直径代表淋巴结大小。△ADC=NAC 4个周期后肿瘤ADC值(ADC2)-NAC前肿瘤ADC值(ADC1);ALN最大直径变化(△L)=NAC前ALN最大直径(L1)-NAC 4个周期后ALN最大直径(L2)。
1.4效果判定采用影像学评估NAC疗效,根据2009年RECIST标准1.1版[4]:化疗4~6个周期后测量实体肿瘤最大径线。完全缓解(complete response,CR)所有目标病灶消失;部分缓解(partial response,PR):基线病灶长径总和缩小≥30%;疾病进展(progressive disease,PD):基线病灶长径总和增加≥20%或出现新病灶;疾病稳定(stable disease,SD):基线病灶长径总和有缩小但未达PR或有增加但未达PD。按照疗效将患者分为有反应(CR+PR)组和无反应(SD+PD)组。
1.5ALN阳性判定标准应用乳腺专用线圈,并以腋窝淋巴结>1 cm或者形态异常为淋巴结转移标准[5]。
1.6统计学方法采用SPSS 17.0进行统计学分析,计量资料以±s表示,采用配对t检验;计数资料以例(%)表示,用χ2检验;定性资料一致性分析采用Kappa检验。用Pearson相关分析评估NAC前后ALN最大直径变化与MRI功能指标△ADC值的相关性,以P<0.05为差异有统计学意义。
2 结果
2.1NAC疗效44例患者均完成了4个周期的NAC,患者有反应(CR+PR)率为72.73%(32/44),无反应(SD+PD)率为27.27%(12/44)。
2.2NAC前和NAC4个周期后ALN最大直径的变化与NAC前比较,有反应组淋巴结最大直径在NAC后缩短,差异有统计学意义(P<0.01);无反应组淋巴结最大直径在NAC后变化不明显,差异无统计学意义(P>0.05),见表1、图1。
Tab.1 The longest diameter changes of ALN before and after four cycles of NAC in two groups表1 NAC前和4个周期NAC后ALN最大直径的变化(cm,±s)

Tab.1 The longest diameter changes of ALN before and after four cycles of NAC in two groups表1 NAC前和4个周期NAC后ALN最大直径的变化(cm,±s)
**P<0.01
n t组别有反应组无反应组32 12 NAC前1.37±1.06 1.34±0.65 NAC后4个周期0.90±0.76 1.35±1.00 3.575**0.035
2.3NAC前和NAC4个周期后肿瘤ADC值的变化与NAC前比较,有反应组ADC值在NAC后显著增加,差异有统计学意义(P<0.01);无反应组ADC值在NAC后与NAC前比较,差异无统计学意义(P>0.05),见表2、图1。
Tab.2 The changes of tumor ADC value before NAC and after four cycles of NAC in two groups表2 NAC前和4个周期NAC后肿瘤ADC值的变化(×10-3mm2/s,±s)
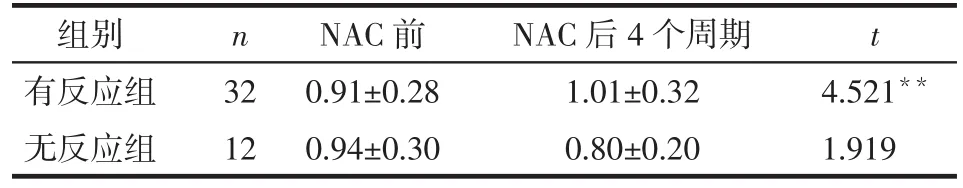
Tab.2 The changes of tumor ADC value before NAC and after four cycles of NAC in two groups表2 NAC前和4个周期NAC后肿瘤ADC值的变化(×10-3mm2/s,±s)
**P<0.01
n t组别有反应组无反应组32 12 NAC前0.91±0.28 0.94±0.30 NAC后4个周期1.01±0.32 0.80±0.20 4.521**1.919
2.4△ADC与△L的相关性有反应组△ADC与△L无相关关系(r=0.131,P=0.413)。
2.5NAC后MRI与病理对患侧ALN状态的评估NAC后病理对患侧ALN状态的评估为金标准,MRI评估患侧ALN状态的敏感度100%,特异度62.5%,Kappa值0.68,见表3。

Tab.3 Consistency analysis of pathology andmRI evaluation for ALN after NAC表3 病理和MRI对NAC后患侧ALN状态评估的一致性分析 (例)
3 讨论
进展期乳腺癌的新辅助化疗已经在临床上广泛开展,如何评估NAC后腋窝淋巴结状态是腋窝外科处理的关键。MRI是NAC前评估腋窝淋巴结状态[6-7]及NAC后评估肿瘤大小的有效方法[8-10]。NAC后早期评估腋窝淋巴结状态对于全面评估NAC疗效及决定腋窝淋巴结外科处理策略均有很强的现实意义。DWI功能参数ADC值可早期从细胞或分子水平上间接反映化疗的疗效,为乳腺癌NAC后疗效的评估提供了新的方法和途径。目前研究证实ADC值较肿瘤大小出现变化的时间要早且敏感度和特异度较高,提示其可以用于早期评估化疗效果[11-14]。临床实践中由于常规乳腺线圈的局限性和较小的腋窝淋巴结不能获得准确的腋窝淋巴结ADC值,不易直接评估NAC后腋窝淋巴结的状态。Belli等[15]认为肿瘤的ADC值与腋窝淋巴结转移等预后因素有关。本研究试图用肿瘤ADC值作为间接评估NAC后腋窝淋巴结状态的量化指标,探讨用肿瘤ADC值代替腋窝淋巴结ADC值早期间接评估NAC后腋窝淋巴结的状态,为全面评估乳腺癌NAC疗效提供新的途径。本研究中有反应组肿瘤ADC值的变化和腋窝淋巴结大小的变化不相关,说明肿瘤ADC值尚不能早期间接反映腋窝淋巴结大小变化,肿瘤ADC值还不能作为独立因素评估NAC后的腋窝淋巴结状态,与Belli等[15]的研究结果有所不同,可能与本研究的样本量较小及纳入新辅助化疗患者的标准不同有关。虽然本研究没有证实ADC值作为独立因素可以早期间接评估NAC后的腋窝淋巴结状态,但大量研究通过综合应用MRI多参数证实了MRI作为评估NAC后腋窝淋巴结状态的有效性[16-17],多为中度敏感[18]。本研究中患者NAC后腋窝淋巴结状态与术后病理结果比较一致,可能和患者的选取有关,在后续的研究中需要扩大样本量并采用计算机辅助探测[19]等新技术手段进行更深入的探讨。目前,前哨淋巴结活检(SLNB)在乳腺癌NAC后腋窝处理中的应用是国内外关注的热点问题,NAC后腋窝淋巴结的有效评估是开展SLNB的前提和保证[20-21]。基于国内外的共识和本研究的结论,笔者认为MRI是临床上评估NAC腋窝淋巴结状态的可靠方法,可以为NAC后腋窝淋巴结的外科处理提供准确的信息。
参考文献
[1] Chen JH,Feig BA,Hsiang DJ, et al.Impact ofmRI evaluates neoad⁃juvant chemotherapy response on change of surgical recommenda⁃tion in breast cancer[J].Ann Surg, 2009, 249(3):448- 454.doi: 10.1097/SLA.0b013e31819a6 e01.
[2] Untchm,harbeck N,huober J, et al.Primary therapy of patients with early breast cancer: evidence, controversies, consensus: opin⁃ions of german specialists to the 14th St.gallen international breast cancer conference 2015 (Vienna 2015) [J].Geburtshilfe Frauen⁃heilkd, 2015, 75(6):556-565.doi:10.1055 /s-0035-1546120.
[3] Galons JP,AltbachmI, Painemurrieta GD,et al.Early increases in breast tumor xenograft watermobility in response to paclitaxel thera⁃py detected by noninvasive difusionmagnetic resonance imaging[J].Neoplasia(New York), 1999, 1(2):113-117.
[4] Eisenhauer EA, Therasse P, Bogaerts J, et al.New response evalua⁃tion criteria in solid tumours: revised RECIST guideline (version 1.1) [J].Eur J Cancer, 2009, 45(2):228- 247.doi: 10.1016/j.ej⁃ca.2008.10.026.
[5] Yin ZX, Shen KW, Li YF, et al.The accuracy of preoperatively pre⁃dicting axillary lymph node status in breast cancer patients by ultra⁃sonography andmRI[J].Chin J Gen Surg, 28(4):259-262.[殷正昕,沈坤炜,李亚芬,等.术前乳腺B超及MRI检查对乳腺癌患者腋窝淋巴结状态评估的准确性[J].中华普通外科杂志, 2013, 28(4): 259-262].
[6]he N, Xie C, Wei W, et al.A new, preoperative,mRI-based scor⁃ing system for diagnosingmalignant axillary lymph nodes in women evaluated for breast cancer[J].Eur J Radiol, 2012, 81(10):2602-2612.doi: 10.1016/j.ejrad.2012.03.019.
[7] Scaranelo AM,Eiada R,Jacks LM,et al.Accuracy of unenhancedmR imaging in the detection of axillary lymph nodemetastasis:study of reproducibility and reliability[J].Radiology, 2012, 262(2): 425-434.doi: 10.1148/radiol.11110639.
[8] Rouzier R,mathieumC, Sideris L, et al.Breast-conserving surgery after neoadjuvant anthracycline- based chemotherapy for large breast tumors[J].Cancer, 2004, 101(5): 918- 925.doi: 10.1002/cncr.20491.
[9] Yeh E, Slanetz P, Kopans DB, et al.Prospective comparison ofmam⁃mography, sonography, andmRI in patients undergoing neoadju⁃vant chemotherapy for palpable breast cancer[J].Am J Roentgenol, 2005, 184(3): 868-877.doi:10.2214/ajr.184.3.01840868.
[10] Yin B, Liu L, Zhang BY, et al.The value ofmRI in evaluation of re⁃sidual tumor to neoadjuvant chemotherapy for breast cancer[J].Jour⁃nal of Pratical Radiology, 2013, 29(9): 1441-1444.[尹波,刘莉,张碧云,等.MRI在乳腺癌新辅助化疗残留病灶评价中的价值[J].实用放射学杂志, 2013, 29(9): 1441-1444].
[11] Lee KC,moffat BA, Schott AF, et al.Prospective early response im⁃ aging biomarker for neoadjuvant breast cancer chemotherapy[J].Clin Cancer Res, 2007, 13(1/2): 443-450.doi: 10.1158/1078-0432.CCR-06-1888.
[12] ThoenyhC, Ross BD.Predicting andmonitoring cancer treatment response with diffusion-weightedmRI[J].Jmagn Reson Imaging, 2010, 32(1): 2-16.doi: 10.1002/jmri.22167.
[13] Sharme U, Danishad KK, Seenu V, et al.Longitudinal study of the assessment bymRI and diffusion weighted imaging of tumor re⁃sponse in patients with locally advanced breastcancer undergoing neoadjuvant chemotherapy[J].NMR Biomed, 2009, 22(1):104-l13.doi: 10.1002/nbm.1245.
[14] Richard R, Thomassin I, Chapellierm, et al.Diffusion-weightedmRI in pretreatment prediction of response to neoadjuvant chemo⁃therapy in patients with breast cancer[J].Eur Radiol, 2013, 23(9): 2420-2431.doi: 10.1007/s00330-013-2850-x.
[15] Belli P, Costantinim, Bufi E, et al.Diffusionmagnetic resonance imaging in breast cancer characterisation: correlations between the apparent diffusion coefficient andmajor prognostic factors[J].Radi⁃olmed, 2015, 120(3): 268-276.doi: 10.1007/s11547-014-0442-8.
[16] Ramirez SI, Schollem, Buckmaster J, et al.Breast cancer tumor size assessment withmammography, ultrasonography, andmagnetic resonance imaging at a community basedmultidisciplinary breast center [J].Am Surg, 2012, 78(4):440-446.
[17] Luciani A, Dao TH, Lapeyrem, et al.Simultaneous bilateral breast andhigh- resolution axillarymRI of patients with breast cancer: preliminary results[J].AJR Am J Roentgenol, 2004,182(4): 1059-1067.doi: 10.2214/ajr.182.4.1821059.
[18] Javid S, Segara D, Lotfi P, et al.Can breastmRI predict axillary lymph nodemetastasis in women undergoing neoadjuvant chemo⁃therapy[J]? Ann Surg Oncol, 2010, 17(7): 1841-1846.doi: 10.1245/s10434-010-0934-2.
[19] Kimh, KimhH, Park JS, et al.Prediction of pathological complete response of breast cancer patients undergoing neoadjuvant chemo⁃therapy: usefulness of breastmRI computer-aided detection[J].Br J Radiol, 2014, 87(1043): 20140142.doi: 10.1259/bjr.20140142.
[20] Liu G, Qiu PF, Wang YS, et al.Sentinel lymph node biopsy in clini⁃cally node- negative breast cancer patients after neoadjuvant che⁃motherapy[J].Chin J Endocr Surg, 2013, 7(2):111-114.[刘广,邱鹏飞,王永胜,等.新辅助化疗后腋窝淋巴结转阴乳腺癌患者前哨淋巴结活检研究[J].中华内分泌外科杂志, 2013, 7(2): 111-114].
[21] Tan VK,Goh BK,Fook-Chong S,et al.The feasibility and accuracy of sentinel lymph node biopsy in clinically node-negative patients after neoadju -vant chemotherapy for breast cancer-a systematic re⁃view andmeta-analysis [J].J Surg Oncol,2011,104(1):97-103.doi: 10.1002/jso.21911.
(2015-06-08收稿2015-08-18修回)
(本文编辑魏杰)
Evaluation ofmRI for axillary lymph node in breast cancer after neoadjuvant chemotherapy
LI Fu1, ZENG Jian1△, LI Chunyan2, LUOming1, KONG Zhen1
1 Department of Gastrointestine and Gland Surgery, 2 Department of Radiology, the First Affiliatedhospital, Guangximedical University, Nanning 530021, China△Corresponding Author E-mail: zengjian125@hotmail.com
Abstract:Objective To explore and evaluate the clinical value ofmRI for status of axillary lymph node after neoadju⁃vant chemotherapy (NAC) in patients with breast cancer.Methods Forty-four patients with 1ocally advanced breast cancer (LABC) were underwent NAC for four cycles.The longest diameter of axillary lymph node (ALN)measured bymRI scan.Val⁃ue of apparent diffusion coefficient (ADC) and their correlation were compared before NAC and four cycles after NAC.Re⁃sults ofmRI and pathological data for ALN were compared between two groups of patients.Results All patients finished four cycles of NAC.The total response rate (CR+PR) was 72.7% (32/44), and the total non-response rate (SD+PD) was 27.3% (12/44).The longest diameter of ALN was significantly shortened in response group.The longest diameter was (1.37± 1.06) cm before NAC and (0.90±0.76) cm after NAC (P<0.01).The ADC value of the tumor was significantly increased in re⁃sponse group [(0.91±0.28)×10-3mm2/s before NAC and (1.01±0.32)×10-3mm2/s after NAC, P<0.01)].There was no signifi⁃cant correlation between ADC value change (△ADC) and the longest diameter change of ALN (△L, r=0.131, P=0.413).The sensitivity, specificity and Kappa value of ALN evaluation after NAC were 100%, 62.5% and 0.68measured bymRI.Con⁃clusionThe change of tumor longest diameter reflects the effect of chemotherapy directly.The tumor ADC value ofmRI can not be used as an independent indicator of chemotherapy effect of ALN, eventhouthmRI was the sensitive index for eval⁃uating the status of axillary lymph node after neoadjuvant chemotherapy for breast cancer.
Key words:breast neoplasms; chemotherapy, adjuvant;magnetic resonance imaging; signal processing, computer-as⁃sisted; lymphaticmetastasis; treatment outcome; neoadjuvant chemotherapy; apparent diffusion coefficient
通讯作者△E-mail:zengjian125@hotmail.com
作者简介:李富(1979),男,主治医师,硕士,主要从事乳腺癌基础与临床研究
基金项目:广西壮族自治区卫生厅自筹经费科研课题(Z2011328)
中图分类号:R445.2,R737.9
文献标志码:A
DOI:10.11958/59011
作者单位:1广西医科大学第一附属医院胃肠腺体外科(邮编530021),2放射科