LVAS患者3D-FLAIR影像表现及其临床意义
刘颖曹代荣方哲明顾晰邢振
1福建医科大学附属第一医院影像科
2福建医科大学附属第一医院耳鼻咽喉头颈外科
·临床研究·
LVAS患者3D-FLAIR影像表现及其临床意义
刘颖1曹代荣1方哲明1顾晰2邢振1
1福建医科大学附属第一医院影像科
2福建医科大学附属第一医院耳鼻咽喉头颈外科
目的利用磁共振三维快速液体衰减反转恢复序列(3D-FLAIR)探讨大前庭导水管综合征(LVAS)内耳的影像特征及其临床意义。方法回顾性分析60只经水成像3D-TSE序列证实的LVAS患耳和20只正常对照耳的3.0T磁共振3D-FLAIR影像,参照水成像显示的迷路形态,观察迷路各结构的信号特征,测量患耳内淋巴囊、前庭和耳蜗的信号强度,分析其信号与患者年龄及听力损失分级的相关性。结果病变组中52只耳蜗和50只前庭3D-FLAIR序列显示高信号,对照组中20只正常耳均未见高信号;内耳高信号的存在与否和听力损失无相关(P=0.840);内淋巴囊分别与耳蜗(t=-1.2,P=0.233)和前庭(t=-1.807,P=0.074)之间的信号强度差异不具统计学意义;内淋巴囊信号强度与患者年龄呈正相关(r=0.510,P=0.000),与听力损失程度无相关(r=0.027,P=0.852)。结论3D-FLAIR序列可以观察到LVAS内耳信号的改变,与听力损失程度无关,与患者年龄相关。
水抑制成像;大前庭导水管综合征;磁共振成像
大前庭导水管综合征(Large Vestibular Aque⁃duct Syndrome LVAS)的认识最初得益于颞骨断层扫描的观察,并提出该病的最初诊断标准[1]。MRI内耳水成像作为LVAS诊断的重要手段,对于患耳迷路形态改变的认识已有许多报道[2-9],我们前期观察到LVAS患耳内淋巴囊体积与听力损失程度无相关[8],另提出骨性前庭导水管内存在疝出的外淋巴间隙的推测[9],然而这些研究限于形态学观察,无法阐述LVAS发病机制。对于能反应迷路内淋巴液成分的MR信号变化除Sugiura[6]个案报道外,尚无专题研究。我们利用对液体成份变化高度敏感的三维液体衰减反转恢复(three-dimensional fluid attenuated in⁃version recovery 3D-FLAIR)序列观察LVAS迷路信号变化,探讨LVAS迷路信号与患者年龄及听力损失的相关性。
1 资料与方法
1.1 病例资料
收集30例(60只耳)由CT确诊的大前庭导水管综合征,合并其他内耳畸形者(如Mondini畸形)剔除。男性20例,女性10例,中位年龄4岁(1-41岁)。20%LVAS患者具家族性[7],30例患者中12例分属4个家庭,18例散发病例。对照组10例共20只正常耳,男性6例,女性4例,中位年龄8岁(3-15岁);入选标准为无耳部自觉症状且听力学检查正常,内耳及颅脑MR正常;对照组源于因头痛来我院行颅脑MR检查的患儿,告知其父母情况,同意加做内耳MR及听力学检查者作为志愿者。受检者(未成年人由父母代签)均签署知情同意书。
1.2 听力检测
30名患者及10名对照组志愿者均在MR检查前后一周内在我院完成听力检查,其中15名不配合小儿行ABR检查,25名可配合者行纯音电测听检查,患者及对照组听力分级参照WHO[1]标准。
1.3 MR检查
3.0 T SIEMENS MAGNETOM VERIO MR扫描,16通道头线圈采集,重T2水成像及3D-FLAIR序列均采用 SPACE(Sampling Perfection with Applica⁃tion-optimized Contrast different flip angle Evolutions),重T2水成像用于解剖定位,参数:TR=1000ms,TE= 132ms,空间分辨率0.50 mm×0.50 mm×0.50 mm,采集时间4分50秒;3D-FLAIR序列用于信号分析,参数:TR=6000 ms,TE=388 ms,TI=2100 ms,采集时间5分 32秒,空间分辨率0.70 mm×0.70 mm×0.70 mm。
1.3 图像分析
由2名熟悉内耳MR的医师(分别具备6年、21年影像诊断经历)以脑脊液为参照,分别评估前庭及耳蜗3D-FLAIR信号,高于脑脊液信号者记录为高信号;2名医师评估结果的一致性行组内相关系数分析,信度良好则Pearson’s chi-squared检验分析前庭及耳蜗高信号的存在与否与听力损失程度的相关性。2名医师进一步分别测量前庭、耳蜗及同一层面的内淋巴囊信号强度后取平均值(图1A/C),独立样本t检验比较前庭与内淋巴囊、耳蜗与内淋巴囊的信号强度差异。3D-FLAIR感兴趣区(ROI)的放置参照水成像定位(图1)。水成像显示:部分LVAS患者内淋巴囊可见高低信号分界(图1B/D)(研究[9]显示水成像高信号部分为外淋巴液疝入骨性前庭导水管及岩骨后缘,并非真正的内淋巴囊),因此测量3D-FLAIR高信号部分代表真正的内淋巴囊,信号分析参照文献[10]的半定量法,选取同层面小脑半球为参照(图1 A/C),计算内淋巴囊/小脑信号强度比,Spearman’s rank-correlation coefficient分析内淋巴囊/小脑信号强度比与患者年龄、听力损失程度的相关性。所有统计应用SPSS19.0统计学软件(ver19.0;Chicago,IL,USA)分析数据,P<0.05设为差异有统计学意义。
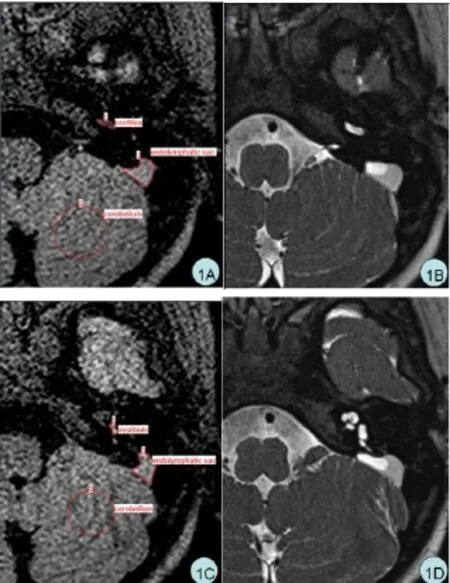
图1 LVAS内耳信号强度的测量方法:ROI以水成像图像(图1B/D)为参照,3D-FLAIR序列上选取中心层面手动圈出耳蜗(1A)、前庭(1C)及内淋巴囊(1A,1C)高信号区域,并圈出同层面同侧3cm2大小的小脑半球,测量其信号强度(图1A/C)。Fig.1 The measurement of the signal intensity of LVAS inner ear.Placed the ROI on 3D-fluid-attenuated inversion recovery (3D-FLAIR)images(Fig1A,1C)with referenced to the heavily T2-weighted images at the same level(Fig 1B,1D).We focused on the cochlea(Fig 1A),vestibule(Fig 1C)and endolymphatic sac(Fig 1A,1C),we placed ROI in the high signal area on 3D-FLAIR(Fig 1A,1C).The signal of the cerebellum at the same level as the endolymphatic sac was used as an internal reference(Fig 1A,1C).
2 结果
3D-FLAIR序列显示:20只正常耳均无高信号(图2A),60只LVAS患耳52只耳蜗(图2B)、50只前庭(图2C)存在高信号,60只患耳中有43只耳蜗及前庭同时存在高信号。LVAS患者内淋巴囊与前庭(t=-1.807,P=0.074)、内淋巴囊与耳蜗(t=-1.200,P= 0.233)之间信号强度差异均无统计学意义。
60只患耳年龄介于1-41岁,中位年龄4岁;患耳内淋巴囊与小脑信号强度比平均值为0.92±0.30,该信号强度比与患者年龄线性正相关(r=0.510,P=0.000)。
60只患耳中,轻度听力下降(26-40 dB HL)3只,中度听力下降(41-60 dB HL)3只,重度听力下降(61-80 dB HL)2只,极重度听力下降(>80dB HL)52只。内淋巴囊信号强度比与患者听力损失程度无相关性(r=0.027,P=0.852);前庭或耳蜗中高信号存在与否与患者的听力损失程度无相关(P=0.840)。
60只LVAS患耳中16只耳3D-FLAIR序列上内淋巴囊仅见高信号影(图3A),44只耳低信号区以前庭导水管开口为中心向远端延伸,后缘始终有高信号区,分界清楚,弧形膨隆(图3B)。无1例仅见低信号。无1只耳3D-FLAIR序列上内淋巴囊仅见低信号。
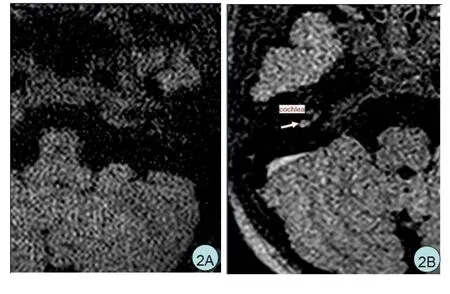

图2 LVAS及志愿者正常耳3D-FLAIR迷路信号特点:10岁志愿者,内耳无高信号影(图2A);5岁LVAS女孩,右侧耳蜗及内淋巴囊见高信号影(图2B);6岁LVAS男孩,左侧前庭见高信号影。(图2C)。Fig.2 The signal intensity feature of inner ear in the healthy control and LVAS on 3D-FLAIR images.No high signal was present in the inner ear of a 10-year-old healthy control(Fig 2A).High signal intensity was identified in the cochlea of a 5-year-old girl with LVAS(Fig 2B).High signal intensity was identified in the vestibule of a 6-year-old boy with LVAS(Fig 2C).
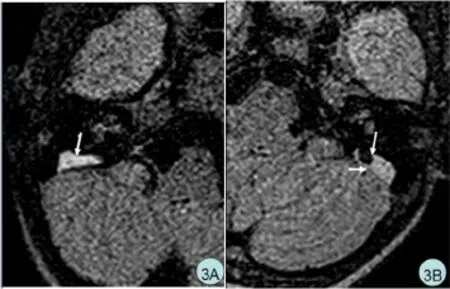
图3 LVAS患者扩大内淋巴囊的信号特点:4岁LVAS男孩,内淋巴囊内仅见高信号影(图3A);6岁LVAS男孩,内淋巴囊除有高信号区外,还有和脑脊液相似的低信号区,低信号区后缘有高信号区,分界清楚,呈弧形膨隆。(图3B)。Fig.3 The signal characteristics of the endolymphatic sac in LVAS.Only hyperintense signal was observed in the endolymphatic sac of a 4-year-old boy with LVAS(Fig 3A).High-signal area co-occurred with a low-signal area was observed in the endolymphatic sac with clear boundary and in curved bulge of a 3-year-old girl with LVAS(Fig 3B).
3 讨论
三维液体衰减反转恢复(three-dimensional fluid attenuated inversion recovery 3D-FLAIR)序列可抑制自由水信号,对液体成份变化的敏感性明显优于水成像[11-13]。水成像序列内、外淋巴液均为高信号,无法区别;由于3D-FLAIR序列对液体成分变化的高敏感性,同时内淋巴液蛋白含量远高于外淋巴液,浓度约1000~3000mg/100ml[14],因此内淋巴液呈高信号,外淋巴液呈低信号。正常人耳蜗、前庭及半规管以外淋巴液为主,外淋巴液总量是内淋巴液总量的28.4倍[15],因此正常人耳蜗、前庭3D-FLAIR呈低信号;内淋巴囊仅含内淋巴液,LVAS患者内淋巴囊3D-FLAIR呈高信号。
本组病例3D-FLAIR显示:LVAS组耳蜗及前庭见高信号,且信号强度与内淋巴囊信号呈正相关,而无症状对照组无高信号。LVAS患者前庭和耳蜗3D-FLAIR显示高信号提示其蛋白含量增高,考虑这些区域有较多内淋巴液,从影像学上支持多数学者提出的内淋巴倒流理论,即LVAS患者外伤等引起脑脊液压力的突然波动,压迫淋巴囊周围的硬脑膜,有可能使淋巴循环从高渗的内淋巴囊倒流,迫使内淋巴囊的高渗液通过宽大的内淋巴管逆流,并经扩大了的水管进入淋巴循环,经连合管流入耳蜗,引起毛细胞退变导致患者感音神经性聋[16-20]。
另外观察到LVAS患者内淋巴囊信号与年龄呈正相关,提示扩大的内淋巴囊中蛋白成分随年龄增长而升高,这支持Pyle[20-21]报道的前庭水管随年龄增长可出现动态变化;内淋巴囊组织学研究[22]表明:内淋巴囊结构呈囊样,存在吞噬细菌、细胞碎屑和其他小颗粒的功能异常,可引起内淋巴囊内容液的浓缩,因此内淋巴囊3D-FLAIR序列信号随年龄增长而升高。
进一步分析LVAS患者迷路信号与听力损失程度的相关性,发现前庭、耳蜗高信号的存在与否和听力损失程度无相关,而且内淋巴囊信号强度与听力损失程度亦无相关,可能是本组患者以重度聋为主而影响了结果。
由于本组患者以重度聋为主,无一例在听力下降过程中行MR观察,无法及时了解MR信号改变与患者听力动态变化的相关性。听障儿童的语言功能发展呈现出年龄差异,干预年龄越早,听障儿童的语言功能发展越快[23],因此及早得通过MR信号及听力情况了解并干预LVAS患儿的治疗,对于未来语言发展及听力保护具重要作用,这方面有待影像及耳科医师进一步研究探讨。
4 结论
LVAS患者的前庭和耳蜗与内淋巴囊的3D-FLAIR序列信号强度相关,且内淋巴囊信号强度随LVAS患者年龄的增长而升高,预示着内淋巴囊高渗液倒流及内淋巴囊内液体蛋白含量随病程进展而升高。
1 WHO:Report of the first informal consultation on future program de⁃velopments for the prevention of deafness and hearing impairment. Geneva:Word Health Organization,1997:23-24.
2 Kouichirou O,Jusuke I,Tetsuya F,et al.Large vestibular aqueduct syndrome with high CT density and high MR signal intensity.AJNR 1997;18:482–484.
3 Dahlen R,Harnsberger R,Gray S,et al.Overlapping thin-section fast spin-echo MR of the large vestibular aqueduct syndrome.AJNR 1997;18:67–75.
4 Naganawa S,Koshikawa T,Iwayama E,et al.MR imaging of the en⁃larged endolymphatic duct and sac syndrome by use of a 3D fast asymmetric spin-echo sequence:volume and signal-intensity mea⁃surement of the endolymphatic duct and sac and area measurement of the cochlear modiolus.Am J Neuroradiol,2000;21(9):1664-1669.
5 Naganawa S,Koshikawa T,Fukatsu H,et al.Serial MR imaging stud⁃ies in enlarged endolymphatic duct and sac syndrome.Eur Radiol 2002;12 Suppl 3:114-117.
6 Sugiura M,Naganawa S,Sato E,et al.Visualization of a high protein concentration in the cochlea of a patient with a large endolymphatic duct an d sac,using three-dimensional fluid-attenuated inversion re⁃covery magnetic resonance imaging.The journal of Laryngolo⁃gy&Otology 2006;120:1084-1086.
7 Tong K,Harnsberger H,Dahlen R.Large vestibular aqueduct syn⁃drome:a genetic disease?AJR Am J Roentgenol 1997;168: 1097-1101.
8 方哲明,娄昕,兰兰,等.大前庭导水管综合征内淋巴囊体积与听力损伤相关性分析.中华耳科学,2010,8(2):153-156.
Fang ZM,Lou,X,Lan L,et al.Relationship of the endolymphatic sac volume and hearing loss in patient with large vestibular aqueduct syndrome.[J].Chinese Journal of Otology,2010,8(2):153-156.
9 方哲明,娄昕,兰兰,等.大前庭导水管综合征内淋巴囊和前庭导水管MRI信号特征及其临床意义.中华放射学杂志,2012,46(1):9-12.
Fang ZM,Lou,X,Lan L,et al.MR imaging features and clinical value of aqueduct and endolymphatic sac in patients with large vestibu⁃lar aqueduct syndrome Chinese Journal of Radiology,2012,46(1): 9-12.
10 Naganawa S,Ishihara S,Iwano S,et al.Estimation of gadolinium in⁃duced T1-shortening with measurement of simple signal intensity ra⁃tio between the cochlea and brain parenchyma on 3D-FLAIR:corre⁃lation with T1 measurement by TI scout sequence.Magn Reson Med Sci 2010;9:17-22.
11 Lee IH,Kim HJ,Chung WH,et al.Signal intensity change of the labyrinth in patients with surgically confirmed or radiologically diag⁃nosed vestibular schwannoma on isotropic 3D fluid-attenuated in⁃version recovery MR imaging at 3T.Eur Radiol 2010;20:949-957.
12 Yoshida T,Sugiura M,Naganawa S,et al.Three-dimensional flu⁃id-attenuated inversion recovery magnetic resonance imaging find⁃ings and prognosis in sudden sensorineural hearing loss.Laryngo⁃scope 2008;118:1433–1437.
13 Yamazaki M,Naganawa S.Increased signal intensity of the cochlea on pre-and post-contrast enhanced 3D-FLAIR in patients with ves⁃tibular schwannoma.Neuroradiology 2009;51:855–863.
14 Okamoto K,Ito J,Furusawa T,et al.MRI of enlarged endolymphatic sacs in the large vestibular aqueduct syndrome.Neuroradiology 1998;40:167–172.
15 王艳.内耳淋巴液的来源、性质和成分.生物学通报,2006,41:23.Wang Y.The origin,property and composition of inner ear lymph.. Bulletin,2006,41:23.
16 Berrettini S,Forli F,Bogazzi F,et al.Large vestibular aqueduct syn⁃drome:audiological,radiological,clinical,and genetic features.Ameri⁃can Journal of Otolaryngology-Head and Neck Medicine and Sur⁃gery 2005;26:363-371.
17 Gopen Q,Zhou GW,Whittemore K.Enlarged Vestibular Aqueduct: Review of Controversial Aspects.Laryngoscope 2011;121:1971– 1978.
18 Hirai S,Cureoglu S,Patricia A,et al.Large vestibular aqueduct syn⁃drome:a human tmporal bone study.Laryngoscope 2006;116: 2007-2011.
19 Levenson MJ,Parisier SC,Jacobs M,et al.The large vestibular aque⁃duct syndrome in children:a review of 12 cases and the description of a new clinical entity.Arch Otolaryngol Head Neck Surg 1989; 115:54-58.
20 刘铤.内耳病.北京:人民卫生出版社,2006,532.
Liu T.The inner ear disease.Beijing:People’s Medical Publishing House,2006,532.
21 Pyle GM.Embryological development and large vestibular aqueduct. Laryngoscope 2000;110:1837–1842.
22 Gussen R.Histological evidence of specialized microcirculation of the endolymphatic sac.Arch Otorhinolaryngol 1980;228:7–16.
23 王丽燕,杨影,孙喜斌.3-6岁听障儿童语言功能发展特点的研究.中华耳科学,2015,13(4):592-597.
Wang LY,Yang Y,Sun XB.Development of language function in hearing-impaired Children.Aged from 3 to 6 years.[J].Chinese Jour⁃nal of Otology,2015,13(4):592-597.
3D-FLAIR MRI Findings and Its Clinical significance in Patients with Large VestibularAqueduct Syndrome
LIU Ying1,CAO Dairong1,FANG Zheming1,GU Xi2,XING Zhen1
1 Departments of Radiology,
2 Departments of Otolaryngology-Head and Neck Surgery,The First Affiliated Hospital of Fujian Medical University
Subject To study characteristics of inner ears imaging with 3D-fluid-attenuated inversion recovery (3D-FLAIR)and its clinical significance in patients with large vestibular aqueduct syndrome(LVAS).MethodsStudy subjects included 30 patients(60 ears)with bilateral LVAS confirmed by water imaging with 3D-TSE sequence and 10 normal volunteers(20 ears).3D-FLAIR sequence was performed using a 3-Tesla MR scanner.With comparison to labyrinth morphology on routine inner ear water imaging,characteristics of labyrinth signals were examined.Signal intensities(SI)in the endolymphatic sac,vestibule and cochlea was measured,and their correlation to the degree of hearing loss and patient age analyzed.Correlation between the SI ratio(SIRs)of the endolymphatic sac and patient age(degree of hearing loss)was investigated.ResultsOn 3D-FLAIR,high signal was present in 52 cochleae and 50 vestibules among the 60 ears with LVAS, and in none of the 20 normal ears.There was no significant difference between endolymphatic sac SI and that of the vestibule(t=-1.807,P=0.074)or cochlea(t=-1.2,P=0.233).There was no correlation between high SI in inner ear and hearing loss(P=0.840).A positive linear correlation,however,was found between SIR and patient age(r=0.510,P=0.000),but not between SIR and hearing loss(r=0.027,P=0.852).Conclusion Signal variation in inner ear seen on 3D-FLAIR sequences does not correlate with the degree of hearing loss,but with patient age in LVAS.
Fluid Attenuated Inversion Recovery;Enlarged Vestibular Aqueduct Syndrome;Magnetic Resonance Imaging
R764
A
1672-2922(2016)06-783-5
2016-05-17审核人:娄昕)
10.3969/j.issn.1672-2922.2016.06.016
刘颖,硕士,主治医师,研究方向:头颈部影像诊断
方哲明,Email:409016093@qq.com