经皮椎体成形术治疗新鲜骨质疏松性椎体压缩骨折
·临床研究·
经皮椎体成形术治疗新鲜骨质疏松性椎体压缩骨折
孟祥玉,吐尔洪江·阿布都热西提,谢江,田惠中,马原
作者单位:830002新疆维吾尔自治区,新疆医科大学第六附属医院微创脊柱外科
【摘要】目的探讨经皮椎体成形术(percutaneous vertebroplasty,PVP)治疗新鲜骨质疏松性椎体压缩骨折的疗效。方法2011年1月~2012年12月共治疗骨质疏松性单椎体压缩骨折38例,其中男7例,女31例;年龄55~80岁(平均65.1岁)。患者取俯卧位局麻下行单侧穿刺PVP。测量椎体高度的恢复情况和后凸角改善情况,视觉模拟量表(visual analogue scale, VAS)评分评价疼痛缓解程度,活动能力评分检测活动改善情况,并对并发症进行分析。结果所有手术均顺利完成,每个椎体平均填充骨水泥3.5 mL。随访时间均>12个月。椎体前壁高度由术前(19.2±5.7) mm改善至术后(20.0±5.7) mm,椎体中间高度由术前(19.2±5.1) mm改善至术后(20.2±5.0) mm,差异有统计学意义(P<0.05);椎体后壁高度和Cobb角术前与术后相比,差异无统计学意义(P>0.05);VAS评分术前8.3±1.1,术后12个月时为1.1±0.6,术前、术后差异有统计学意义(P<0.05)。活动能力评分术前3.1±0.9,术后12个月时为1.1±0.3,术前、术后差异有统计学意义(P<0.05)。骨水泥渗漏9例。结论PVP可有效治疗新鲜骨质疏松性椎体压缩骨折,创伤小,减轻疼痛,改善功能,无重大并发症。
【关键词】老年人; 胸椎; 腰椎; 骨质疏松; 脊柱骨折; 骨折,压缩性; 经皮椎体后凸成形术
作者简介:孟祥玉(1976—), 硕士,副主任医师
【中图分类号】R 683.2
DOI【】
收稿日期:(2014-07-22)
Percutaneous vertebroplasty for treatment of acute osteoporotic vertebral compression fracturesMENGXiang-yu,Turghunjan·Abdurxit,XIEJiang,TIANHui-zhong,MAYuan.DepartmentofMinimallyInvasiveSpinalSurgery,SixthAffiliatedHospitalofXinjiangMedicalUniversity, 830002Urumqi,XinjiangUygurAutonomousRegion,China
Abstract【】ObjectiveTo analyze the therapeutic effect of percutaneous vertebroplasty (PVP) for the treatment of acute osteoporotic vertebral compression fractures. MethodsFrom January 2011 to December 2012, 38 cases were treated with PVP for one-level osteoporotic compression fracture, which included 7 males and 31 females in the age range of 55-80 years with a mean age of 65.1 years old. All operations were finished successfully under local anesthesia on the surgical area with 1% lidocaine at prone position. Body height and kyphotic Cobb’s angle of vertebral bodies were measured before and after operation, pain levels and activity was evaluated by visual analogue scale(VAS) score and locomotor activity score at preoperative, postoperative 1 d, postoperative 1 week,postoperative 3 months and postoperative 12 months. Complications were also recorded. ResultsThe average operation time was 32 min(ranging 25-50 min). An average of 3.5 mL Polymethylmethacrylate(PMMA)were injected. Follow-up period was more than 12 months. Respective preoperative and postoperative, the anterior height of the vertebral body were (19.2±5.7) mm and (20.0±5.7) mm; the medium height of the vertebral body were (19.2±5.1) mm and (20.2±5.0) mm; the difference was statistically significant(P<0.05). There was no difference in the posterior vertebral height and the kyphotic Cobb’s angle correction rate at preoperative and postoperative. Pain relief and mobility improvement were observed after the operation. VAS score revealed a decrease from 8.3±1.1 to 1.1±0.6. Locomotor activity score decreased from 3.1±0.9 to 1.1±0.3. Cement leakage happened in 9 patients without neurological complications. ConclusionPVP can achieve satisfactory clinical outcomes in treating acute osteoporotic compression fractures.
【Key words】Aged; Thoracic vertebrae; Lumbar vertebrae; Osteoporosis; Spinal fractures; Fractures, compression; Percutaneous kyphoplasty
J Spinal Surg, 2015,13(3):135-139
随着社会的老龄化,骨质疏松的发生率逐渐增加,由于骨质疏松所导致的老年椎体压缩性骨折不断增多[1]。老年骨质疏松性椎体压缩性骨折常伴有较高的死亡率和致残率,引起慢性疼痛,身体功能受损,降低生活质量[2]。既往的非手术治疗包括卧床休息、药物、理疗和支具,治疗时间长、并发症多,患者较痛苦[3]。近年来,经皮椎体成形术(percutaneous vertebroplasty,PVP)广泛开展,取得了良好的治疗效果[4-5],但多用于非手术治疗无效的老年骨质疏松性压缩骨折[6],由于该手术的微创性和疗效,已有文献报道新鲜骨折患者疗效满意[7],本研究对本科治疗的患者资料进行回顾性分析,以明确该手术是否适合老年新鲜骨质疏松性压缩骨折。
1资料与方法
1.1一般资料
本组患者共38例,男7例,女31例;年龄55~80岁,平均65.1岁。均为影像学检查所证实。骨折原因:走路滑倒跌伤27例,坠落伤3例,其他原因8例。均为单椎体骨折。受伤至手术时间均<2周。伤椎部位:T81例,T101例,T114例,T1213例,L111例,L25例,L32例,L41例。采用Genant等[8]的方法对椎体骨折的类型和压缩程度进行分级。楔形骨折Ⅰ度12例,Ⅱ度7例,Ⅲ度3例;双凹型骨折Ⅰ度10例,Ⅱ度4例 ;粉碎性骨折Ⅰ度1例,Ⅱ度1例。
1.2手术方法
患者取俯卧位,常规心电监护,建立静脉通道,腰背部穿刺区域行常规皮肤消毒铺巾,在正位透视下选择穿刺点,穿刺点位于棘突旁2~3 cm处,穿刺针与人体矢状面成角15°~20°。术中正侧位双向透视证实穿刺方向,当侧位见穿刺针抵达椎体后缘骨皮质但未超过椎弓根前缘时,正位像针尖应位于椎弓根投影之内,然后将穿刺针穿刺至椎体前部的1/3处。透视证实穿刺针位置后开始调配骨水泥,于透视监控下将骨水泥于黏稠状态下注入,注射时间2~3 min,术中如发现有骨水泥渗漏便立即停止注射,注射结束后插入针芯,待骨水泥固化后拔出穿刺针。
1.3评价方法
止痛效果采用疼痛视觉模拟量表(visual analogue scale, VAS)评价[9],VAS评分卡范围:0(完全无痛) ~10(患者所经历的最严重的疼痛)。活动能力评分:①行动无明显困难,②行走困难(需帮助),③需使用轮椅或只能坐立,④被迫卧床。椎体高度压缩率和恢复率计算参照Lee 等[10]的方法,测量侧位X 线片上压缩骨折椎体前壁高度a0、中间高度m0和后壁高度p0,同时测量侧位X线片相应骨折椎体上、下前壁高度a1、a2、中间高度m1、m2和后壁高度p1、p2。压缩骨折椎体原始前壁高度A =(a1+a2)/2,中间高度M =(m1+m2)/2,后壁高度P =(p1+p2)/2。椎体前壁压缩率=(A-a0)/A×100%,中间压缩率=(M-m0)/M×100%,后壁压缩率=(P-p0)/P×100%,椎体高度恢复率= (术前压缩率-术后压缩率)/ 术前压缩率×100%。椎体后凸角度和恢复率参照脊柱Cobb角测量方法,侧位X线片上压缩骨折椎体上、下终板垂线交角即为椎体后凸角度,后凸角度恢复率=(术前后凸角度-术后后凸角度)/术前后凸角度×100%
1.4统计学处理

2结果
本组38例患者均顺利完成手术,手术时间25~50 min,平均32 min。每个椎体平均填充骨水泥3.5 mL。
患者术后VAS评分明显改善,从术后1 d至术后3个月疼痛呈逐渐减轻的趋势,3个月以后疼痛维持在一个比较稳定的状态。患者活动功能的改善以术后1 d最明显,此后稳定在一个较好的水平(见表1)。
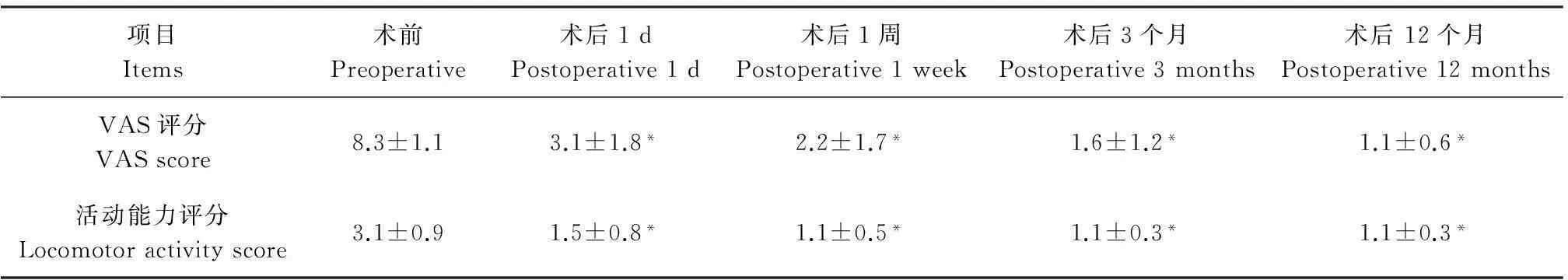
比较患者术前及术后X线片,发现患者椎体前壁高度和椎体中间高度均较术前改善明显;椎体后壁高度和后凸Cobb角度术前与术后比较无明显变化(见表2)。
9例患者出现骨水泥渗漏,其中4例渗漏至脊柱旁软组织,2例渗漏至椎旁静脉,2例渗漏至椎管内硬膜外,1例渗漏至邻近椎间隙。但均未出现神经症状,有3例患者出现邻椎骨折均再次行椎体成形术,未出现感染及硬膜外血肿等其他并发症。典型病例影像学资料见图1。
表1术前和术后随访VAS评分及活动能力评分
Tab.1VAS score and locomotor activity score at operation and follow-up
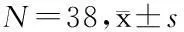
项目Items术前Preoperative术后1dPostoperative1d术后1周Postoperative1week术后3个月Postoperative3months术后12个月Postoperative12monthsVAS评分VASscore8.3±1.13.1±1.8*2.2±1.7*1.6±1.2*1.1±0.6*活动能力评分Locomotoractivityscore3.1±0.91.5±0.8*1.1±0.5*1.1±0.3*1.1±0.3*
注:*与术前比较P<0.05
Note:*Compared with preoperativeP<0.05
表2术前和术后椎体高度和后凸角度
Tab.2Height of the vertebral body and Cobb’s angle at preoperative and postoperative
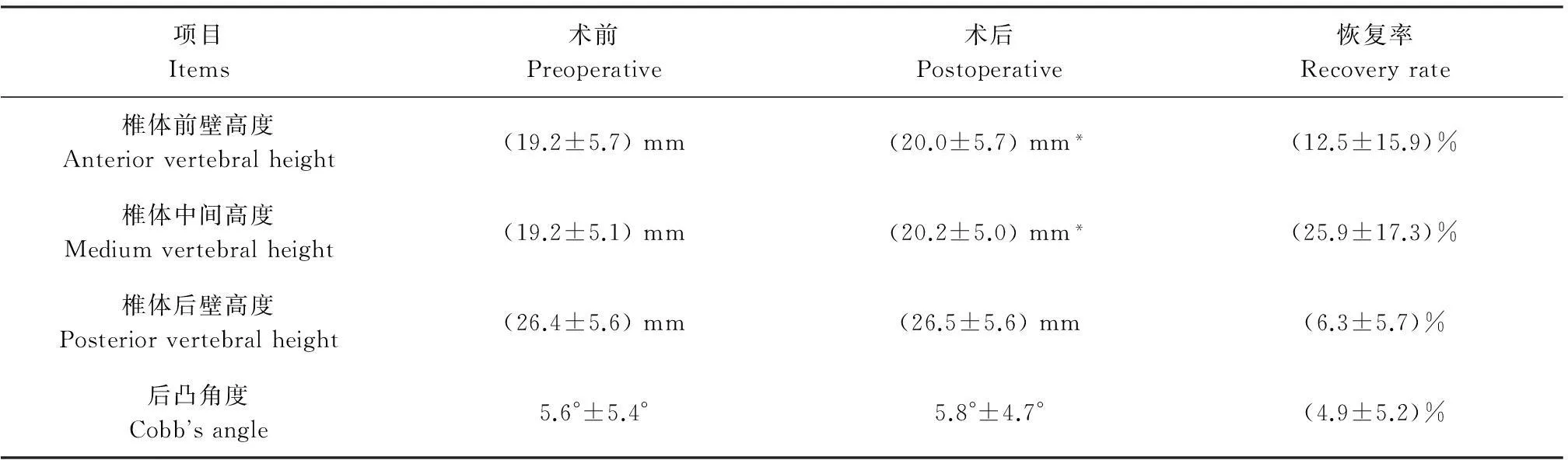
项目Items术前Preoperative术后Postoperative恢复率Recoveryrate椎体前壁高度Anteriorvertebralheight(19.2±5.7)mm(20.0±5.7)mm*(12.5±15.9)%椎体中间高度Mediumvertebralheight(19.2±5.1)mm(20.2±5.0)mm*(25.9±17.3)%椎体后壁高度Posteriorvertebralheight(26.4±5.6)mm(26.5±5.6)mm(6.3±5.7)%后凸角度Cobb‘sangle5.6°±5.4°5.8°±4.7°(4.9±5.2)%
注:*与术前比较P<0.05
Note:*Compared with preoperativeP<0.05
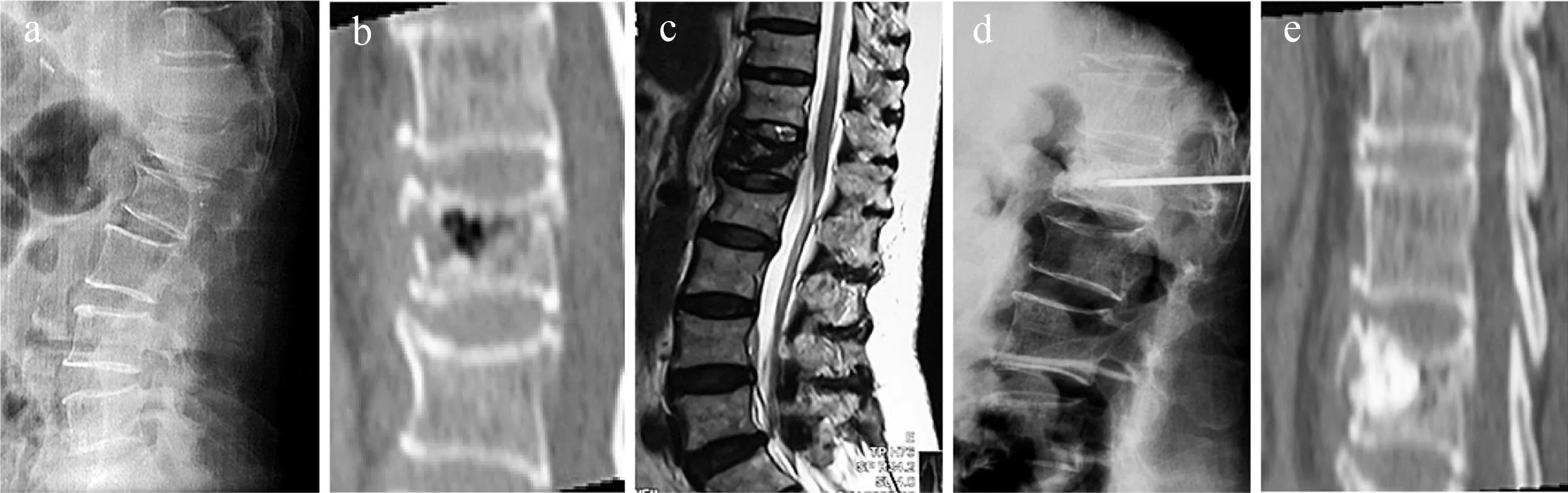
a:术前腰椎侧位X线片示L1椎体楔形压缩性骨折b:术前CT三维重建示L1椎体粉碎性骨折c:术前MRI示L1椎体T2加权像信号异常d:术中X线示穿刺针位置好,骨水泥充填好,椎体高度部分恢复e:术后CT三维重建示骨水泥充填好,无渗漏
a: Preoperative roentgenograph shows L1wedge type compression fractureb: Preoperative 3D-CT reconstruction shows L1crush type compression fracturec: Preoperative T2WI MRI shows L1fresh compression fractured: Intraoperative roentgenograph shows puncture needle position is good, bone cement is well filled and vertebral body height is recoveried partiallye: Postoperative 3D-CT reconstruction shows bone cement is well filled and no cement leakage happen
图1典型病例影像学资料
Fig.1Radiologic data of typical case
3讨论
自20世纪90年代中期以来,PVP逐渐成为骨质疏松性椎体压缩骨折的首选治疗方法,其适应证为颈椎、胸椎和腰椎>2周的骨质疏松性椎体压缩性骨折引起中至重度的疼痛并非手术治疗无效,其绝对禁忌证:①已愈合的骨质疏松性椎体压缩性骨折或骨折非手术治疗有效;②存在未治疗的凝血疾病;③存在椎间盘炎、骨髓炎或败血症。相对禁忌证:①骨折椎体后缘有骨块突入椎管;②骨折时间>1年;③骨折椎体压缩>80%[6]。临床上通常认为对于椎体压缩性骨折所导致的疼痛、活动受限以及降低生活质量有一定的自限行,随着时间的推移骨折逐渐愈合,在几周至几个月的时间内患者的症状会减轻,生活质量会随之改善。但Hasserius等[11]的研究显示椎体骨折后健康状况的恶化持续许多年,结局比其他类型的脆性骨折要差。Suzuki 等[12]报道1组病例,107例患者因骨质疏松性压缩性骨折就诊,给予患者药物治疗及制动和康复,观察患者疼痛、活动能力和生活质量等在3周,3、6、12个月的改善情况,发现骨折后1年患者的状况与腰椎椎间盘突出、中央型腰椎椎管狭窄及因腰颈部问题而完全不能工作的患者情况相同,与通常大多数人所认为的骨折后预后较好所不同,急性椎体骨折是骨折患者健康状况长期持续严重恶化的开始。
目前对于新鲜与陈旧性骨质疏松性压缩骨折尚无统一的定义。本研究采用较为通用的分期方法[13],将骨质疏松椎体骨折后2周内定义为新鲜骨折(急性期),>3个月为陈旧骨折,2周~3个月的骨折为亚急性骨折。本组38例患者均为新鲜骨折,发病至手术时间均<2周,未经过正规的非手术治疗而采取手术治疗,基于以下几点考虑:①急诊就诊的患者疼痛非常明显,活动受限,患者对早期药物治疗的满意度较低,迫切希望能较快的缓解疼痛,恢复活动。②患者均为老年人,长期卧床会导致一系列的相关并发症。③对既往非手术治疗效果欠佳患者手术治疗后效果比较肯定。④经济生活水平的提高使患者要求有更高的生活质量。⑤有文献报道对急性骨折行PVP的有效性[7]。
既往有研究证明单侧穿刺与双侧穿刺临床疗效无明显差异[14],注入骨水泥的量与临床疗效无明显差异[15],且一项关于骨水泥的生物力学研究证实3.5 mL的骨水泥就可以使骨折椎体及领近椎体达到正常的应力分布[16],单侧穿刺与双侧穿刺相比能明显减少手术操作的时间,患者的耐受性更好,故本组病例均采用单侧穿刺入路,注射的骨水泥量为3~4 mL。根据术前X线及CT影像,从压缩较重的一侧穿刺,如果压缩程度相同则从症状较重的一侧穿刺,如果压缩程度相同症状无明显区别则可根据医生的操作习惯选择。术中既要保证椎体有较好的充盈,又要减少骨水泥的渗漏。
Omidi-Kashani等[17]报道了对单一椎体的压缩性骨折行PVP与椎体后凸成形术(percutaneous kyphoplasty, PKP)的疗效对比, PVP组28例,PKP组29例,观察患者的疼痛评分以及SF-36评分,随访6个月发现2组患者的临床疗效相同,而且并发症无显著差异,相比PKP比较昂贵的价格,作者推荐行PVP治疗。本组病例选择PVP而非PKP考虑以下因素:对于新鲜椎体骨质疏松性压缩性骨折,PVP的骨水泥能很好的填充至骨折的裂隙,在椎体内形成较好的骨水泥分布,而PKP需要用球囊对椎体进行撑开造成椎体骨小梁的压缩,虽然能较好地恢复椎体的高度,但骨水泥的分布较差,不能与椎体骨质很好的结合,由于PKP较高的费用及临床疗效与PVP相比并无明显优势故选择后者。
PVP治疗骨质疏松性椎体压缩性骨折的并发症发生率为1%~10%[6]。大多数都是一过性的和轻微的。包括:出血,肋骨或椎体后方结构骨折,由于骨水泥聚合反应产生的术后几小时一过性发热和疼痛加重,神经根的刺激,骨水泥通过椎旁静脉丛引起的肺栓塞,气胸和感染,需要减压手术去除渗漏的骨水泥和修复骨折的椎弓根的发生率<1%。本组共9例发生骨水泥渗漏,发生率为23.7%,考虑与新鲜骨折有关,但未出现血肿、肺栓塞、气胸和感染等其他并发症,可能与手术病例较少有关,但应密切防范,有3例病患者分别于术后1个月、5个月及10个月出现再骨折,均行椎体成形术后恢复,有1例患者术后1年死于其他疾病。
本组病例的临床结果说明PVP可以有效治疗新鲜的老年骨质疏松性压缩骨折,患者的疼痛明显缓解,活动能力改善,但椎体高度恢复不明显,后凸角度改善不明显,并发症的发生率没有明显的提高[18-19]。但本研究病例数较少,没有对照组且为回顾性研究,有一定的研究缺陷,需要随机对照试验来证实结论的可靠性。
参 考 文 献
[1] Lin JT, Lane JM.Osteoporosis: a review[J].Clin Orthop Relat Res, 2004, 425:126-134.
[2] Gold DT.The nonskeletal consequences of osteoporotic fractures. Psychologic and social outcomes[J].Rheum Dis Clin North Am, 2001, 27(1):255-262.
[3] Tamayo-Orozco J, Arzac-Palumbo P, Peón-Vidales H, et al.Vertebral fractures associated with osteoporosis: patient management[J].Am J Med, 1997, 103(2A):44S-48S.
[4] 郝定均, 刘鹏, 贺宝荣, 等.陈旧性与新鲜性压缩骨折行椎体成形术的临床对比研究[J].脊柱外科杂志, 2012, 10(2):83-86.
[5] Anselmetti GC, Corrao G, Monica PD, et al.Pain relief following percutaneous vertebroplasty: results of a series of 283 consecutive patients treated in a single institution[J].Cardiovasc Intervent Radiol, 2007, 30(3):441-447.
[6] Hulme PA, Krebs J, Ferguson SJ, et al.Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies[J].Spine (Phila Pa 1976), 2006, 31(17):1983-2001.
[7] Klazen CA, Lohle PN, de Vries J, et al.Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial[J].Lancet, 2010, 376(9746):1085-1092.
[8] Genant HK, Wu CY, van Kuijk C, et al.Vertebral fracture assessment using a semiquantitative technique[J].J Bone Miner Res, 1993, 8(9):1137-1148.
[9] Huskisson EC.Measurement of pain[J].Lancet, 1974, 2(7889):1127-1131. JT, Lane JM.Osteoporosis: a review[J].Clin Orthop Relat Res, 2004, 425:126-134.
[2] Gold DT.The nonskeletal consequences of osteoporotic fractures. Psychologic and social outcomes[J].Rheum Dis Clin North Am, 2001, 27(1):255-262.
[3] Tamayo-Orozco J, Arzac-Palumbo P, Peón-Vidales H, et al.Vertebral fractures associated with osteoporosis: patient management[J].Am J Med, 1997, 103(2A):44S-48S.
[4] 郝定均, 刘鹏, 贺宝荣, 等.陈旧性与新鲜性压缩骨折行椎体成形术的临床对比研究[J].脊柱外科杂志, 2012, 10(2):83-86.
[5] Anselmetti GC, Corrao G, Monica PD, et al.Pain relief following percutaneous vertebroplasty: results of a series of 283 consecutive patients treated in a single institution[J].Cardiovasc Intervent Radiol, 2007, 30(3):441-447.
[6] Hulme PA, Krebs J, Ferguson SJ, et al.Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies[J].Spine (Phila Pa 1976), 2006, 31(17):1983-2001.
[7] Klazen CA, Lohle PN, de Vries J, et al.Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial[J].Lancet, 2010, 376(9746):1085-1092.
[8] Genant HK, Wu CY, van Kuijk C, et al.Vertebral fracture assessment using a semiquantitative technique[J].J Bone Miner Res, 1993, 8(9):1137-1148.
[9] Huskisson EC.Measurement of pain[J].Lancet, 1974, 2(7889):1127-1131.
[10]Lee ST, Chen JF.Closed reduction vertebroplasty for the treatment of osteoporotic vertebral compression fractures. Technical note[J].J Neurosurg, 2004, 100(4 Suppl Spine):392-396.
[11]Hasserius R, Karlsson MK, Jónsson B, et al.Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly-a 12-and 22-year follow-up of 257 patients[J].Calcif Tissue Int, 2005, 76(4):235-242.
[12]Suzuki N, Ogikubo O, Hansson T.The course of the acute vertebral body fragility fracture: its effect on pain, disability and quality of life during 12 months[J].Eur Spine J, 2008, 17(10):1380-1390.
[13]Yu CW, Hsieh MK, Chen LH, et al.Percutaneous balloon kyphoplasty for the treatment of vertebral compression fractures[J].BMC Surg, 2014, 14:3.
[14]Song BK, Eun JP, Oh YM.Clinical and radiological comparison of unipedicular versus bipedicular balloon kyphoplasty for the treatment of vertebral compression fractures[J].Osteoporos Int, 2009, 20(10):1717-1723.
[15]Chen JF, Lee ST, Lui TN, et al.Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: a preliminary report[J].Chang Gung Med J, 2002, 25(5):306-314.
[16]Luo J, Daines L, Charalambous A, et al. Vertebroplasty: only small cement volumes are required to normalize stress distributions on the vertebral bodies[J].Spine (Phila Pa 1976), 2009, 34(26):2865-2873.
[17]Omidi-Kashani F, Samini F, Hasankhani EG, et al.Does percutaneous kyphoplasty have better functional outcome than vertebroplasty in single level osteoporotic compression fractures? A comparative prospective study[J].J Osteoporos, 2013:690329.
[18]胡英江, 马永东, 常琴.不同时限行经皮椎体成形术的临床分析[J].脊柱外科杂志, 2013, 11(4):230-232.
[19]Nussbaum DA, Gailloud P, Murphy K.A review of complications associated with vertebroplasty and kyphoplasty as reported to the Food and Drug Administration medical device related web site[J].J Vasc Interv Radiol, 2004, 15(11):1185-1192. ST, Chen JF.Closed reduction vertebroplasty for the treatment of osteoporotic vertebral compression fractures. Technical note[J].J Neurosurg, 2004, 100(4 Suppl Spine):392-396.
[11]Hasserius R, Karlsson MK, Jónsson B, et al.Long-term morbidity and mortality after a clinically diagnosed vertebral fracture in the elderly-a 12-and 22-year follow-up of 257 patients[J].Calcif Tissue Int, 2005, 76(4):235-242.
[12]Suzuki N, Ogikubo O, Hansson T.The course of the acute vertebral body fragility fracture: its effect on pain, disability and quality of life during 12 months[J].Eur Spine J, 2008, 17(10):1380-1390.
[13]Yu CW, Hsieh MK, Chen LH, et al.Percutaneous balloon kyphoplasty for the treatment of vertebral compression fractures[J].BMC Surg, 2014, 14:3.
[14]Song BK, Eun JP, Oh YM.Clinical and radiological comparison of unipedicular versus bipedicular balloon kyphoplasty for the treatment of vertebral compression fractures[J].Osteoporos Int, 2009, 20(10):1717-1723.
[15]Chen JF, Lee ST, Lui TN, et al.Percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures: a preliminary report[J].Chang Gung Med J, 2002, 25(5):306-314.
[16]Luo J, Daines L, Charalambous A, et al. Vertebroplasty: only small cement volumes are required to normalize stress distributions on the vertebral bodies[J].Spine (Phila Pa 1976), 2009, 34(26):2865-2873.
[17]Omidi-Kashani F, Samini F, Hasankhani EG, et al.Does percutaneous kyphoplasty have better functional outcome than vertebroplasty in single level osteoporotic compression fractures? A comparative prospective study[J].J Osteoporos, 2013:690329.
[18]胡英江, 马永东, 常琴.不同时限行经皮椎体成形术的临床分析[J].脊柱外科杂志, 2013, 11(4):230-232.
[19]Nussbaum DA, Gailloud P, Murphy K.A review of complications associated with vertebroplasty and kyphoplasty as reported to the Food and Drug Administration medical device related web site[J].J Vasc Interv Radiol, 2004, 15(11):1185-1192.
(本文编辑于倩)
·消息·
“第九届脊柱脊髓复合型损伤治疗新进展学习班”通知
上海市第六人民医院骨科(脊柱外科)在连续成功举办八届国家级继续教育项目“脊柱脊髓复合型损伤治疗新进展学习班”基础上,将于2015年8月14~ 16日举办“第九届脊柱脊髓复合型损伤治疗新进展学习班”。学习班邀请了国内著名脊柱外科、创伤骨科、神经外科、胸外科、腹部外科、麻醉科以及护理等领域专家授课,采用理论讲授、模型操作以及病例讨论形式,尽最大可能提高学员理论及实践操作能力,结业时授予国家级继续教育Ⅰ类学分10分。热忱欢迎全国骨科同道前来上海市第六人民医院骨科参加此次学习班!
学习班地址: 上海市宜山路600号,上海交通大学附属第六人民医院骨科多功能学术报告厅
学习班费用: 800元/人,食宿以及来往交通费自理
报名邮箱: 15083130254@163.com; yangerzhu2012@163.com
联系地址: 上海交通大学附属第六人民医院骨科, 邮编 200233
联系人: 曹亮亮手机 15000037030; Email 15083130254@163.com
杨二柱手机 13918527551; Email yangerzhu2012@163.com