原发性甲状旁腺功能亢进症致高血钙危象诊断及治疗分析
田丹丹,王丽娜,蒋升
·临床诊疗提示·
原发性甲状旁腺功能亢进症致高血钙危象诊断及治疗分析
田丹丹,王丽娜,蒋升
目的探讨原发性甲状旁腺功能亢进症致高血钙危象的临床表现、实验室检查及影像学检查结果、治疗及转归。方法选取2005年1月—2015年1月新疆医科大学第一附属医院收治的10例原发性甲状旁腺功能亢进症致高血钙危象患者,入院时随机血钙水平均≥3.75 mmol/L。回顾性分析患者的临床表现、实验室检查及影像学检查结果、治疗及转归。结果10例患者血钙水平4.02~5.20 mmol/L,平均(4.48±0.42)mmol/L;8例患者血磷水平偏低(0.50~0.94 mmol/L),2例患者血磷水平处于参考范围低值。甲状旁腺素(PTH)水平305~2 500 ng/L,平均(1 369±682)ng/L;碱性磷酸酶水平68~1 445 U/L,平均(381±405)U/L。1例未行99Tcm-甲氧基异丁基异腈(MIBI)显像检查,1例99Tcm-MIBI显像阴性,但2例患者均有典型超声、实验室检查结果及临床表现,术后均证实为有功能腺瘤。其余患者99Tcm-MIBI显像均阳性。10例患者入院后均及时给予扩容、利尿、降钙等内科治疗,所有患者在每日补液量4 000~6 000 ml的基础上,根据病情给予利尿剂、降钙素及双磷酸盐等治疗,缓解患者高钙症状,在3~5 d内血钙水平维持在相对安全的范围内,且生命体征平稳后,在准确定位的基础上给予手术治疗。术后10例患者血清PTH水平均明显下降,全身疼痛、烦渴、恶心及呕吐等症状在1周内明显改善;8例患者血钙水平在术后3~7 d内恢复正常,余2例患者术后1~2 d内发生低钙血症,给予钙剂及活性维生素D3治疗,1周后血钙水平正常,低钙血症症状消失。结论原发性甲状旁腺功能亢进症致高血钙危象患者血钙水平升高,PTH水平亦升高,一旦诊断明确,若无手术禁忌证,应积极完善术前准备并尽早手术治疗。手术是其最有效治疗方法。
甲状旁腺功能亢进,原发性;高钙血症;诊断;治疗;治疗结果
田丹丹,王丽娜,蒋升.原发性甲状旁腺功能亢进症致高血钙危象诊断及治疗分析[J].中国全科医学,2015,18(36):4479-4482.[www.chinagp.net]
Tian DD,Wang LN,Jiang S.Analysis of the diagnosis and treatment of hypercalcemic crisis induced by primary hyperparathyroidism[J].Chinese General Practice,2015,18(36):4479-4482.
高血钙危象是指任何原因导致血清钙离子水平≥3.75 mmol/L而引起的临床综合征,主要表现为骨骼系统、泌尿系统、胃肠道、心血管及神经中枢的病变[1]。发病急剧,病情凶险,系内科急症,需紧急抢救和治疗。现将新疆医科大学第一附属医院近10年收治的10例原发性甲状旁腺功能亢进症致高血钙危象患者的病例资料进行分析,并结合文献分析,以期探讨和优化其术前准备及术后处理流程。
1资料与方法
1.1一般资料选取2005年1月—2015年1月新疆医科大学第一附属医院收治的10例原发性甲状旁腺功能亢进症致高血钙危象[2]患者,入院时随机血钙水平均≥3.75 mmol/L。其中男1例,女9例;年龄23~60岁;病程2~10年;以骨痛、骨质疏松、病理性骨折为首发症状3例,以多饮、多尿、血尿及泌尿系结石为首发症状3例,以厌食、恶心、消瘦为首发症状2例,混合型表现2例。
1.2方法回顾性分析10例患者的临床表现、实验室检查及影像学检查结果、治疗及转归。
2结果
2.1临床表现及诊断10例患者中有3例全身疼痛进行性加重,活动受限,并存在不同程度的病理性骨折;3例入院前烦渴、多饮表现逐渐加重,尿量逐渐减少,甚至无尿;余4例均有恶心、呕吐、精神萎靡,严重脱水等表现。10例患者根据多次血液生化、血钙及甲状旁腺素(PTH)等检查结果,明确诊断为原发性甲状旁腺功能亢进症致高血钙危象,且据甲状旁腺超声、99Tcm-甲氧基异丁基异腈(MIBI)显像等影像学检查进一步定位病变位置。
2.2实验室检验10例患者血钙水平4.02~5.20 mmol/L,平均(4.48±0.42)mmol/L;8例患者血磷水平偏低(0.50~0.94 mmol/L),2例患者血磷水平处于参考范围低值。PTH水平305~2 500 ng/L,平均(1 369±682)ng/L;碱性磷酸酶水平68~1 445 U/L,平均(381±405)U/L。患者术前及术后1周实验室检查结果见表1。
2.3影像学检查本组患者1例未行99Tcm-MIBI显像检查,1例99Tcm-MIBI显像检查阴性,但2例患者均有典型超声、实验室检查结果及临床表现,术后均证实为有功能腺瘤。其余患者99Tcm-MIBI显像检查均阳性(见表2)。
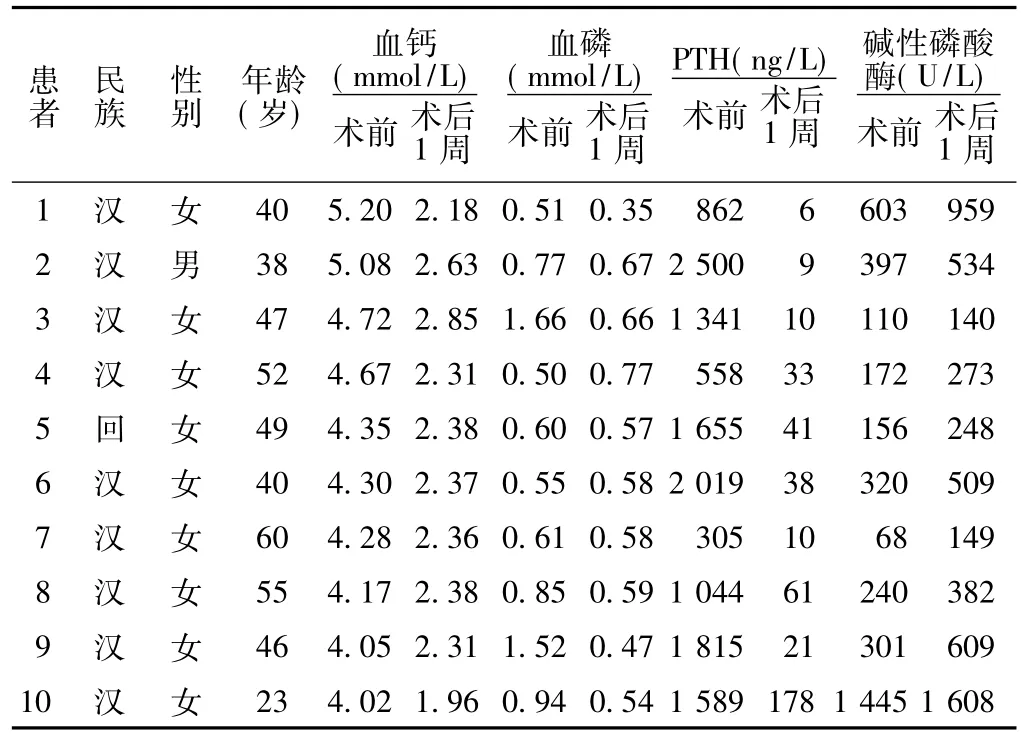
表1 10例原发性甲状旁腺功能亢进症致高血钙危象患者术前及术后1周实验室检查结果Table 1 Laboratory test results of the 10 patientswho have been diagnosed with hypercalcemia crisis induced by primary hyperparathyroidism before surgery and 1 week after surgery
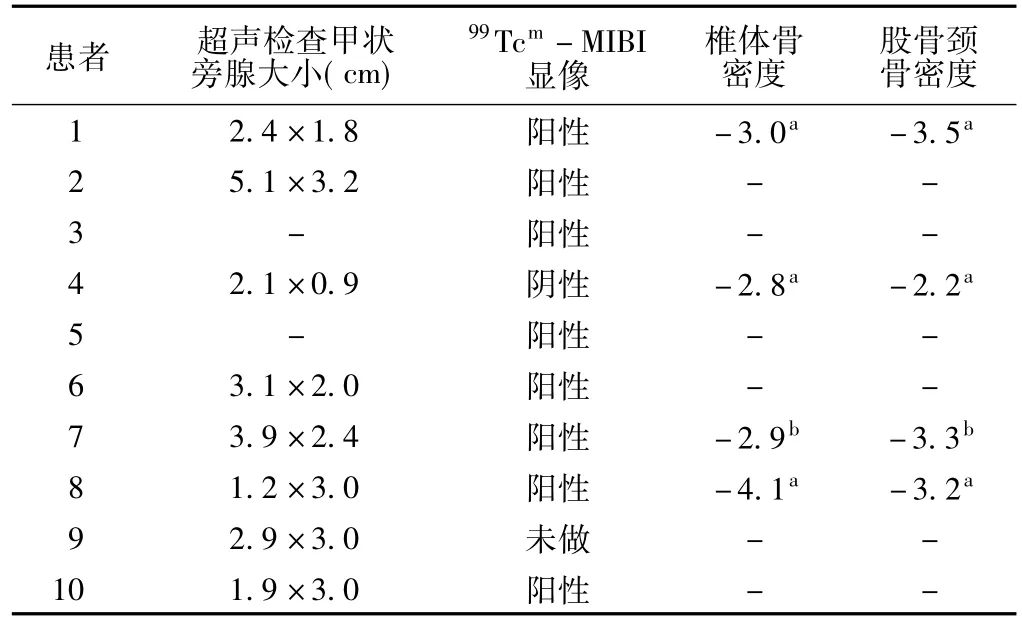
表2 10例原发性甲状旁腺功能亢进症致高血钙危象患者影像学检查结果Table 2 Imageological examination results of 10 patients with hypercalcemic crisis induced by primary hyperparathyroidism
2.4治疗与转归10例患者入院后,首先明确定性诊断,即原发性甲状旁腺功能亢进症致高血钙危象,后均积极给予补液、使用利尿剂、抑制骨吸收、骨破坏及减少PTH的合成与释放等内科治疗,控制高血钙,缓解危象,入院72 h内,每日补液量4 000~6 000ml,口服与静脉滴注相结合。在补液的基础上,均给予利尿剂(呋塞米40~80 mg/d),促使尿钙排出。7例患者联合使用鲑鱼降钙素,10 U/kg静脉滴注,连用3 d后血钙水平降至3.00 mmol/L以下;3例患者在使用降钙素的基础上联合应用帕米膦酸钠注射液,60 mg/d静脉滴注,第5天血钙水平降至3.00 mmol/L以下。在患者补液充分的前提下,转外科手术治疗。本组患者从诊断原发性甲状旁腺功能亢进症致高血钙危象到手术时间为3~7 d,平均5 d。患者在术前准确定位下,均行单纯甲状旁腺切除术及同侧探查,见甲状旁腺包膜完整;术中冷冻切片示:均为甲状旁腺腺瘤,与B超及99Tcm-MIBI显像检查结果相符,术中出血较少,无并发症发生;术后24 h内9例患者血清PTH水平恢复到参考范围内,1例仍高于参考范围;3~7 d内血钙水平逐渐恢复正常,术后无声音嘶哑、饮水呛咳;所有患者术后常规给予葡萄糖酸钙注射液,20 ml/d,预防低钙血症,但仍有2例患者术后发生低钙血症,1例未见明显口唇麻木及手足抽搐,1例口唇麻木、手足抽搐均阳性,均给予钙剂及活性维生素D3治疗,1周后复查血钙水平恢复正常,无口唇麻木、手足抽搐等。
3讨论
3.1临床表现及诊断高血钙危象是内科临床的急症之一,其原因常见于原发性甲状旁腺功能亢进症和肿瘤性高钙血症;占90%以上[3],两者中,前者更为常见,本研究中,10例患者均为原发性甲状旁腺功能亢进症所致,与文献报道较一致[4]。当血钙水平≥3.75 mmol/L时,患者高钙血症表现会明显加重,常伴有明显脱水表现,如出现少尿、无尿,氮质血症等;另外可出现恶心、呕吐、意识障碍、心律失常甚至心搏骤停等消化系统、神经系统及心血管系统表现。本组患者中3例全身骨痛进行性加重,活动受限;3例尿量逐渐减少,出现少尿、无尿伴恶心、呕吐;余4例均有恶心、呕吐、表情淡漠、严重脱水表现。高钙血症患者一般多饮多尿,当出现恶心、呕吐、少尿、无尿、严重失水时,提示危象的开始,临床上应提高警惕,一旦发现,立即给予及时处理,切勿单纯依赖血钙的水平判断病情。
原发性甲状旁腺功能亢进症致高血钙危象的定性诊断主要根据临床表现和实验室检查判断,诊断高血钙危象的标准是:血清钙水平≥3.75 mmol/L,如同时伴PTH水平升高,则定性诊断明确[2]。定位诊断,一般选用甲状旁腺超声、放射性核素显像及CT。国外报道99Tcm-MIBI显像检查对甲状旁腺病变定位的灵敏度为82%~100%[5],国内的报道为91.4%[6]。国内外均有报道B超和99Tcm-MIBI显像检查联合应用可提高定位诊断的准确性[6-7]。本组患者颈部超声阳性率为100.0% (8/8),99Tcm-MIBI显像检查阳性率为88.9%(8/9),两者联合灵敏度达100.0%。
3.2治疗高血钙危象一旦明确诊断需及时采取有效的内科治疗,降低血钙水平、缓解症状,为后续定位诊断及治疗争取时间。(1)扩容、利尿纠正脱水:高血钙危象一般有严重的脱水,这是威胁患者生命的最主要原因,也是治疗的关键和基础,快速补液可迅速纠正脱水。在补液的基础上,给予利尿剂,促使尿钙排出,但噻嗪类利尿剂禁用。(2)降钙素及双磷酸盐:可抑制骨吸收,能有效降低血钙水平。前者起效快,作用时间短,存在脱逸现象;后者起效较慢,持续时间较长,故使用降钙素除了有效降低血钙水平外,同时也为双磷酸盐起效争取时间,临床上二者常联合应用[8-9]。本组患者3例采用降钙素与双磷酸盐联合应用,降钙效果确切。对于原发甲状旁腺功能亢进症致高血钙危象,联合使用可快速降低血钙水平,缓解危象。(3)透析及糖皮质激素治疗:也能快速有效地降低血钙水平,但临床很少使用。本组患者均未采用透析及使用糖皮质激素治疗。
针对原发性甲状旁腺功能亢进症致高血钙危象,手术切除病灶是唯一有确切效果的措施[10-11]。尽早手术治疗可避免不可逆性的肾功能不全、骨骼畸形、骨质疏松等严重结果[11]。本组患者长期疗效仍在随访中。定位明确者手术治愈率可达96%[12]。如瘤体术前定位明确,可行单侧探查,否则行双侧探查[13]。本组患者均定性、定位明确,在积极内科治疗改善内环境、血钙水平下降到相对安全水平的前提下,积极采取手术治疗,临床疗效显著。
此类患者,临床常见,定性比较容易,定位常存在难度,近年来随着影像学的进步,病变部位的定位越来越精准,本组患者术前采用颈部超声及99Tcm-MIBI显像检查,结果均为单侧腺瘤,治疗均采用颈部单侧探查和单纯腺瘤切除术,冷冻切片示:均为甲状旁腺腺瘤,与颈部超声及99Tcm-MIBI显像检查结果相符,术后无并发症发生;术后常规给予葡萄糖酸钙注射液,预防低钙血症,但仍有2例患者术后1~2 d内发生低钙血症,给予钙剂及活性维生素D3治疗,1周后复查血钙水平恢复正常,口唇麻木、手足抽搐消失。结合本组患者术后低钙血症发生率,提倡术后常规给予钙剂预防低钙血症,由于本研究样本量偏低,具体剂量需扩大样本量进一步研究。本组患者术后监测PTH水平,9例患者术后24 h PTH水平下降至参考范围,1例仍高于参考范围,但其值下降至术前最高值的12%,术后1周恢复正常,且骨痛、烦渴、多饮症状明显缓解。本组患者PTH水平术后24 h内90%(9/10)恢复到参考范围内,1周内均恢复正常;血钙水平在3~7 d内均恢复正常,骨痛、关节疼痛、烦渴、多饮、多尿及胃肠道症状在1周内明显改善;精神状况明显好转。
总之,原发性甲状旁腺功能亢进症致高血钙危象是内分泌急症之一,临床表现包含高钙血症的表现及高血钙危象的特点,常涉及多个系统,早期常无特异性表现,但若不及时处理可能危及生命,其唯一根治方法为手术治疗,故原发性甲状旁腺功能亢进症致高血钙危象的患者,临床应对时,应采用综合手段积极内科处理,缓解危象,改善内环境,为下一步手术治疗创造条件和争取时间。如能顺利手术治疗,多数患者短期及远期疗效均显著。
[1]Li SL,Huang ZM,Wei GH,et al.Clinical analysis for 51 cases of primary hyperparathyroidism[J].Chinese Journal of General Practitioners,2011,10(12):876-879.(in Chinese)李硕良,黄知敏,卫国红,等.原发性甲状旁腺功能亢进症51例临床分析[J].中华全科医师杂志,2011,10(12):876-879.
[2]Gong LL,Zhang SH,Feng ZP.Hypercalcemia crisisone one case and review of literature[J].Chongqing Medical,2009,38(18): 2282-2283.(in Chinese)龚莉琳,张素华,冯正平.高钙危象1例并文献复习[J].重庆医学,2009,38(18):2282-2283.
[3]Khalil PN,Hallfeldt K.Diagnosis and therapy of primary hyperparathyreoidism[J].MMW Fortschr Med,2008,150 (45):39-41.
[4]Schoretsanitis G,Daskalakis M,Melissas J,et al.Parathyroid carcinonla:clinical presentation and management[J].Am J Otolaryngol,2009,30(4):277-280.
[5]Farley DR.Technetium-99m 2-methoxyisobutyl isonitrilescintigraphy:preoperative and intraoperative guidance for primary hyperparathyroidism[J].World J Surg,2004,28(12):1207-1211.
[6]Zhang WJ,Zheng LC,Zhang XM,et al.Applicatation value of double-phase99Tcm-MIBI imaging in the localization diagnosis of primary hyperparathyroidism[J].Chinese General Practice,2012,15(30):3559-3560,3564.(in Chinese)张文军,郑立春,张晓明,等.99m锝-甲氧基异丁基异腈双时相显像在原发性甲状旁腺功能亢进症定位诊断中的应用价值分析[J].中国全科医学,2012,15(30):3559-3560,3564.
[7]Moure D,Larrañaga E,Dominguez-Gadea L,et al.99MTcsestamibias sole technique in selection of primary hyperparathyroidism patients for unilateral neck exploration[J].Surgery,2008,144 (3):454-459.
[8]Liu WX,Liu WY,Lin HM,et al.Clinical study of severe acute pancreatitis complicated with hypercalcemia crisis in hyperparathyroidism[J].Journal of China Medical University,2012,41(5):446-447.(in Chinese)刘维新,刘威羽,蔺虹名,等.重症急性胰腺炎合并甲状旁腺功能亢进高钙危象的临床分析[J].中国医科大学学报,2012,41 (5):446-447.
[9]Xia FD,Liang HW,Li JD,et al.Clinical analysis of parathyroid tumors:a report of 45 cases[J].Chinese Journal of General Surgery,2013,22(5):613-617.(in Chinese)夏发达,梁慧文,李劲东,等.45例甲状旁腺肿瘤临床分析[J].中国普通外科杂志,2013,22(5):613-617.
[10]Harrison BJ,Triponez F.Intraoperative adjuncts in surgery for primary hyperparathyroidism[J].Langenbecks Arch Surg,2009,394(5):799-809.
[11]Kearney T,Dang C.Diabetic and endocrine emergencies[J].Postqrad Med J,2007,83(976):79-86.
[12]Hessman O,Stålberg P,Sundin A,et al.High success rate of parathyroid reoperation may be achieved with improved localization diagnosis[J].World JSurg,2008,32(5):774-781.
[13]Henry JF.Reoperation for primary hyperparathyroidism:tips and tricks[J].Langenbecks Arch Surg,2010,395(2):103-109.
Analysis of the Diagnosis and Treatment of Hypercalcem ic Crisis Induced by Primary Hyperparathyroidism
TIANDan-dan,WANG Li-na,JIANG Sheng.Department of Endocrinology and Metabolism,the First Affiliated Hospital of Xinjiang Medical University,Urumqi830054,China
ObjectiveTo investigate the clinical manifestations,laboratory examination results,imageological examination results,treatment and outcomes of patients with primary hyperparathyroidism.M ethods Enrolled 10 patients with hypercalcemic crisis induced by primary hyperparathyroidism who were admitted into the First Affiliated Hospital of Xinjiang Medical University from January 2005 to January 2015.At admission,the blood calcium was randomly measured as≥3.75 mmol/L.Retrospective analysis was made on the clinical manifestations,laboratory examination results,imageological examination results,treatment and outcomes of the patients.Results The blood calcium level of 10 patients was 4.02-5.20 mmol/L,averagely(4.48±0.42)mmol/L;8 patients had low blood phosphorus levelwhich was(0.50-0.94mmol/L)and 2 patients had low blood phosphorus level in the reference range.The parathyroid hormone levelwas305-2 500 ng/L,averagely (1 369±682)ng/L;the alkaline phosphatase level was 68-1 445 U/L,averagely(381±405)U/L.One patient didn't receive99Tcm-MIBIexamination,and one patient had negative result in99Tcm-MIBIscaning,while the 2 patients had typical ultrasound results,laboratory examination results and clinicalmanifestations,and functioning pituitary adenomaswere confirmed in both two patients after surgery.The rest patients all showed positive in99Tcm-MIBI scaning.All patients were given the treatment of fluid expansion,dieresis and reduction of calcium;on the basis of a daily fluid injection of 4 000-6 000 ml,all patients were given the treatment of diuretics,calcitonin and double phosphate to relieve the symptoms of high calcium;After blood calcium was kept at a relatively safe level for 3 to 5 days,and vital signs became stabilized,operative treatmentwas given when accurate positioning was made.After operation,the serum PTH level obviously decreased in the 10 patients,and the symptoms ofwhole body ache,polydipsia,nausea and vomit improved significantly within one week;the blood calcium returned to normalwithin 3 to7 daysafter surgery;the other2 patients had hypocalcemiawithin 1 to2 day after operation,and were given treatment of calcium supplementation and vitamin D3,after which blood calcium returned to normal within one week and the symptoms of low calcium disappeared.Conclusion Patients with hypercalcemic crisis induced by primary hyperparathyroidism usually have elevated blood calcium level and PTH level.Once the definite diagnosis ismade and no surgery contraindications exist,preoperative preparation should be activelymade and surgery should be undertaken as soon as possible.Surgery is themost effectivemethod to treat the disease.
Hyperparathyroidism,primary;Hypercalcemia;Diagnosis;Therapy;Treatment outcome
R 582.1
B
10.3969/j.issn.1007-9572.2015.36.016
2015-06-18;
2015-10-27)
(本文编辑:陈素芳)
830054新疆乌鲁木齐市,新疆医科大学第一附属医院内分泌科
蒋升,830054新疆乌鲁木齐市,新疆医科大学第一附属医院内分泌科;E-mail:xjjsh@126.com

