床突旁动脉瘤的手术策略及疗效
束旭俊,孙正辉,武 琛,王芙昱,王胜宝,薛 哲,王文鑫
解放军总医院 神经外科,北京 100853
床突旁动脉瘤的手术策略及疗效
束旭俊,孙正辉,武 琛,王芙昱,王胜宝,薛 哲,王文鑫
解放军总医院 神经外科,北京 100853
目的探讨床突旁动脉瘤的手术策略及疗效。方法回顾分析我院2010年1月- 2014年5月46例行手术治疗床突旁动脉瘤患者的临床资料,其中男性8例,女性38例,年龄22 ~ 72岁,平均50.15岁。17例动脉瘤破裂,9例罹患多发动脉瘤。眼动脉瘤22个、梭性动脉瘤10个、垂体上动脉瘤8个、窝动脉瘤3个、蛇形动脉瘤1个、假性动脉瘤5个。20个动脉瘤≤5 mm,15个5 ~ 15 mm,14个≥15 mm。手术策略包括直接夹闭、夹闭塑形、颅内外血管架桥、颈动脉结扎和动脉瘤包裹。根据格拉斯哥评分(Glasgow outcome scale,GOS)评估临床疗效。结果19个动脉瘤直接夹闭,21个夹闭塑形,颅内外架桥6个,颈动脉结扎2个,动脉瘤包裹1个。根据GOS评分,42例预后良好(GOS 4 ~ 5分),3例预后差(GOS 2 ~ 3分),1例死亡(GOS 1分)。结论根据床突旁动脉瘤的不同特征,采用相应的策略处理动脉瘤,能提高床突旁动脉瘤的临床疗效。
床突旁;颅内动脉瘤;外科治疗
发生于颅内颈内动脉(internal carotid artery,ICA)的动脉瘤通常根据相关分支血管来命名,如眼动脉瘤、垂体上动脉瘤、后交通动脉瘤等;也有根据动脉瘤与周围解剖结构的关系来命名,如海绵窦动脉瘤、床突旁动脉瘤、窝动脉瘤等[1]。1994年Batjer等[2]用床突旁动脉瘤(paraclinoidal carotid aneurysm,PCA)描述发生于海绵窦顶壁与后交通动脉起始部之间的颈内动脉(C5 ~ C6段ICA)上的动脉瘤。该处动脉瘤与前床突、颅底硬膜返折、脑神经关系密切,而且也是大型和巨大型动脉瘤的好发部位,给手术治疗带来了很大的挑战,而动脉瘤的手术策略也呈现多样性,本文总结了我院近4年来手术治疗床突旁动脉瘤的经验。
资料和方法
1 临床资料 自2010年4月- 2014年5月,我院神经外科手术治疗床突旁动脉瘤46例(共49个床突旁动脉瘤),男8例,女38例,年龄22 ~ 72岁,平均50.15岁。其中9例为多发动脉瘤,17例动脉瘤破裂。蛛网膜下腔出血患者Hunt-Hess分级:Ⅰ级4例,Ⅱ级7例,Ⅲ级2例,Ⅳ级4例。主要临床症状为剧烈头痛11例,意识障碍6例,视力、视野损伤15例,头部及眼部疼痛7例,短暂性脑缺血发作4例,动眼神经麻痹1例,体检偶然发现2例。动脉瘤位置:眼动脉瘤22个,颈动脉窝动脉瘤3个,垂体上动脉瘤8个,球形动脉瘤10个,蛇形动脉瘤1个,颈动脉背侧动脉瘤5个。动脉瘤直径大小:≤5 mm 20个,5 ~ 15 mm 15个,≥15 mm 14个。
2 手术方法 术前根据患者头颅CT、脑CT血管成像(computed tomography angiography,CTA)或脑血管造影(digital subtraction angiography,DSA)判断动脉瘤的特征及其与前床突的关系。若术中需磨除前床突,开颅前应显露颈部ICA以便临时阻断。手术入路包括常规翼点入路或扩大翼点入路。打开硬脑膜后,分离侧裂,开放颈动脉池,显露床突上段ICA和部分床突段ICA。若术中探查动脉瘤能完全显露,则直接夹闭;若动脉瘤被前床突阻挡,瘤颈无法完全显露,则需磨除前床突和视神经管上壁;若瘤颈较宽,移行至床突段ICA,则还需进一步打开远侧环,切开视神经鞘,显露床突段ICA。床突旁假性动脉瘤一般体积较小,瘤颈不明显,若无夹闭的可能,可行动脉瘤包裹术;对于突入海绵窦的巨大动脉瘤,可根据患者颅内血流代偿情况,选择行ICA单纯结扎或动脉瘤孤立联合颅内外架桥。选择单纯夹闭、夹闭塑形、动脉瘤包裹、颈动脉结扎还是颅内外血管架桥根据床突旁动脉瘤术前影像学特征和术中具体状况而定。
3 随访和疗效评价 随访截止日期为2014年11月10日。随访内容包括影像学随访和患者术后神经功能状态随访。术后复查CTA或DSA评估动脉瘤有无残颈、复发或再出血;定期电话随访患者神经功能状态,根据格拉斯哥预后评分(Glasgow outcome scale,GOS)评价手术疗效:5分:预后良好,能正常生活;4分:轻度残疾,但可独立生活;3分:重度残疾,日常生活需照顾;2分:植物生存状态;1分:死亡。
结 果
1 手术情况 本组46例中行常规翼点开颅35次,扩大翼点开颅11次;34例开颅前显露颈部ICA,29例术中磨除前床突,共处理床突旁动脉瘤49个,其中19个动脉瘤行直接夹闭,21个行夹闭塑形,1个行包裹术,2个行颈部ICA结扎,6个行动脉瘤孤立联合颅内外血管架桥。
2 动脉瘤大小、形态与处理方式 当床突旁动脉瘤直径<15 mm时,约91.4%可行夹闭或夹闭塑形;当直径≥15 mm时,57.1%行夹闭塑形,35%需行颅内外血管架桥,7%行ICA结扎牺牲载瘤动脉,无一例能行单纯夹闭。眼动脉瘤、窝动脉瘤和垂体上动脉瘤全部能通过夹闭或夹闭塑形来处理;球形动脉瘤50%行血管架桥,40%行夹闭塑形,10%行颈部ICA结扎;床突段ICA背侧动脉瘤多为假性动脉瘤,40%成功夹闭,20%行夹闭塑形,20%行包裹,20%行血管架桥。1例蛇形动脉瘤累及ICA较长,行ICA结扎。见表1。
3 疗效及随访 1例术后突发脑疝,最终因呼吸衰竭死亡。该例系左侧垂体上动脉瘤患者,术前Hunt-Hess 3级,行左侧翼点入路开颅,动脉瘤夹闭成功,但术中见脑肿胀及血管痉挛明显。其余45例均获随访,随访6 ~ 54(21±4)个月。术后行CTA或DSA评估动脉瘤处理情况,45例均未复发或再出血,其中2例留有残颈,1例载瘤动脉狭窄,6例架桥均通畅。术后视力、视野障碍较术前比,好转5例,未变9例,变差2例;一过性动眼神经麻痹7例,永久性麻痹1例;术后脑积水2例,后期行脑室腹腔分流术;3例肢体活动障碍术后2例明显好转;2例意识障碍中1例术后好转,另1例转康复科后续治疗。GOS评分:预后良好35例(76.1%),轻度残疾7例(15.2%),重度残疾2例(4.3%),植物生存1例(2.2%),死亡1例(2.2%)。
4 典型病例 女性患者,53岁,突发头痛伴视物模糊入院(图1)。查体:神志清楚,颈项强直,左眼鼻侧视野缺损,右侧肢体肌力4级。头颅CT示蛛网膜下腔出血,主要集中在环池及左侧侧裂。DSA示左侧大型眼动脉瘤,指向上方。行左侧翼点开颅前显露颈部ICA,以备临时阻断。术中见动脉瘤被前床突阻挡,遂磨除前床突和视神经管上壁,开放视神经鞘,打开远侧环。充分显露动脉瘤近端瘤颈后,用3枚直角开窗动脉瘤夹对动脉瘤夹闭塑形。术后复查DSA未见动脉瘤显影,载瘤动脉通畅,远端血管显影好。患者术后未见新发神经功能障碍,左眼视力较术前好转。
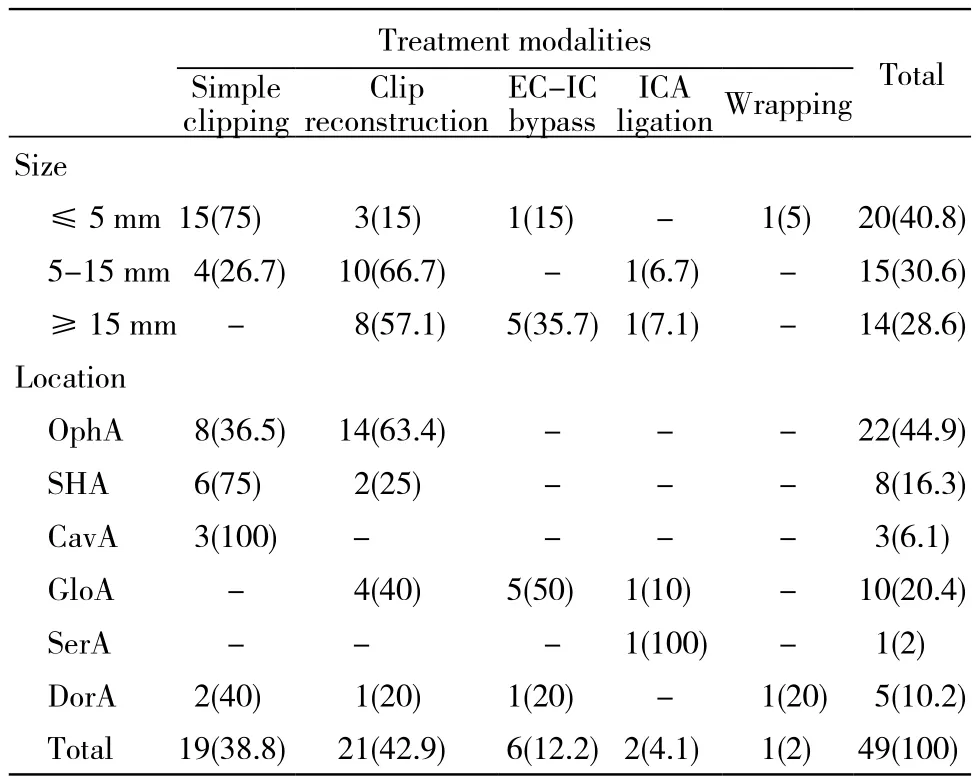
表1 床突旁脉瘤大小、位置和治疗模式Tab. 1 Sizes, location and treatment modalities of paraclinoid aneurysm (n, %)
讨 论
床突旁动脉瘤占颅内动脉瘤的5% ~ 11%,女性多见,也是大型或巨大动脉瘤,多发动脉瘤的好发部位[3]。本组46病例,男女比例约1∶5,30.4%为大型或巨大型动脉瘤。床突旁动脉瘤因位于颅底,与前床突、视神经、海绵窦等关系密切,手术显露动脉瘤存在一定风险,早期手术治疗床突旁动脉瘤的并发症发生率高达60%[4]。近年来,随着颅底外科技术的发展和手术器械的进步,手术安全性已明显提升,近5年文献报道死亡率为3.5% ~ 11%[5-8],本组手术死亡率为2.2%,较文献报道略低,原因可能为有一部分Hunt-Hess分级高的患者和高龄患者接受了治疗创伤小的介入治疗,而未行手术治疗。

图 1 女性患者,53岁,突发头痛伴左眼视物模糊入院A:颅脑CT示蛛网膜下腔出血;B: 3D-DSA示左侧大型眼动脉瘤;C: 动脉瘤术中景象;D: 磨除前床突,显露近端瘤颈;E: 动脉瘤夹闭塑形完成;F: 术后DSA(侧位)示动脉瘤夹闭完全,载瘤动脉通畅Fig. 1 A 53-year-old female patient who presented with sudden headache and visual impairment of left eye was transferred to our hospitalA: Head CT scan showed subarachnoid hemorrhage; B: Three dimensional DSA showed a large left ophthalmic aneurysm; C: Intraoperative view of the aneurysm; D: Intraoperative view after anterior clinoidectomy; E: Clip reconstruction of the aneurysm with 3 right-angled fenestrated clips; F: Postoperative DSA (lateral view) showed total obliteration of the aneurysm and great filling of the parent artery
床突旁动脉瘤的显露是手术的关键因素。部分动脉瘤被前床突阻挡而无法直接夹闭,因此切除前床突是显露该类动脉瘤的必要步骤。有学者[9-10]提倡从硬膜外磨除前床突,有学者[11-12]提倡硬膜下磨除前床突,Barami等[13]则采用联合硬膜内外的方法磨除前床突。我们提倡硬膜下磨除前床突,原因:1)直视下磨除前床突时,动脉瘤与前床突及周围硬膜关系一目了然,能有效减少对动脉瘤和视神经的骚扰;2)一旦动脉瘤发生破裂,能第一时间控制出血并辨别破裂状况,为下一步处理赢得了时间。不管采用哪种方式磨除前床突,最好在开颅前显露好颈部ICA,以便需要时行临时阻断。显露颈部ICA还便于在处理大型动脉瘤时行穿刺逆行回抽。有学者[6,14]认为,ICA穿刺逆行回抽是处理大型或巨大床突旁动脉瘤的一项有效措施,能降低手术相关并发症的发生率。Parkinson等[15]则通过介入方式用球囊和微导管行回抽减压,避免了颈部切口。本组有29例磨除前床突,34例显露颈部ICA,其中31例颈部临时阻断ICA,11例行ICA穿刺逆行回抽,7例动脉瘤发生术中破裂,均为成熟破裂。
床突旁动脉瘤的处理策略要视动脉瘤的特征和术中状况而定。当床突旁动脉瘤体积较小,瘤颈不宽时,单纯夹闭是最简单有效的方式。本组38.8%的动脉瘤行直接夹闭,其中75%的动脉瘤直径<5 mm。假性动脉瘤常见于床突旁颈内动脉,虽体积较小,但基底较宽,无明显瘤颈,单纯夹闭难以成功[16];有学者[17]建议用筋膜或棉纱包裹加固瘤壁;如果动脉瘤发生破裂,Yanaka等[18]建议尝试缝合破裂口;若以上方法均不可行,只能孤立动脉瘤并行颅内外架桥。本组4例假性动脉瘤中2例行夹闭,1例行架桥,1例行包裹。可见假性动脉瘤的处理很棘手,术前应准确判断并做好架桥预案。当动脉瘤体积较大,瘤颈较宽时,可用多枚瘤夹采用不同的组合方式来对动脉瘤夹闭塑形。夹闭塑形需要反复调整瘤夹位置以达到不留残颈的同时保持载瘤动脉也不狭窄的目的。Lee和Kim[19]报道了用开窗夹成功夹闭塑形10例大型床突旁动脉瘤,他们认为手术的关键是要显露出近端瘤颈。我们在处理大型床突旁动脉瘤时,会进一步分离近端载瘤动脉,切开视神经鞘,打开远侧环,游离床突段ICA,这样做的优点:1)能更好地显露床突旁动脉瘤的近端瘤颈;2)夹闭塑形时,有更好的视野和更多的空间调整瘤夹;3)能在床突段ICA放置临时阻断夹,使动脉瘤孤立更彻底。本组床突旁动脉瘤42.9%行夹闭塑形,其中85.7%的动脉瘤直径>5 mm,可见夹闭塑形是处理非小型动脉瘤的重要方式。球形动脉瘤和蛇形动脉瘤因累及ICA全周而没有瘤颈,此类动脉瘤往往不适合夹闭塑形,需要牺牲载瘤动脉并行颅内外血管架桥;对于对侧血流代偿好并能良好耐受一侧ICA闭塞的患者,可直接在颈部结扎ICA。本组10例球形动脉瘤5例行架桥;1例术前行DSA检查时Matas试验显示颅内血流代偿较好,能耐受ICA球囊闭塞试验,遂行颈部ICA结扎。
治疗床突旁动脉瘤时,若术中操作不当会引发术后视力、视野障碍、脑梗死、动眼神经麻痹等症状。Eliava等[6]报道约25%的患者因手术导致视力、视野损伤,这与动脉瘤压迫,术中过度牵拉,供血穿支动脉损伤,磨视神经管时热损伤有关。此外脑脊液漏、术后脑梗死也是较常见的等并发症。Li等[20]报道了术后脑缺血性卒中发生率为20%,主要原因为术中临时阻断载瘤动脉时间过长或损伤穿支动脉。本组术后视力、视野障碍较术前有所好转5例,未变9例,变差2例;术后缺血性卒中发生率为3例(6.5%),明显低于文献报道。减少手术操作所致的损伤至关重要,我们认为术中操作应注意:1)磨除前床突时要持续用0.9%氯化钠注射液灌洗,降低视神经的热损伤;2)切开视神经鞘时要避免损伤眼动脉;3)术中尽可能减少对脑组织和神经的牵拉;4)瘤颈尚未充分显露时,不应反复尝试夹闭动脉瘤;5)颈部穿刺回抽能使大型或巨大动脉瘤塌陷,为夹闭提供更多空间和更好的术野;6)分离床突段时ICA时在该段放置阻断夹能彻底孤立动脉瘤,为动脉瘤剖开取栓或血管吻合提供无血的操作环境;7)动脉瘤夹闭后,应取一块肌筋膜填塞前床突空缺,防止术后脑脊液漏。
1 Kobayashi S, Koike G, Orz Y, et al. Juxta-dural ring aneurysms of the internal carotid artery[J]. J Clin Neurosci, 1995, 2(4):345-349.
2 Batjer HH, Kopitnik TA, Giller CA, et al. Surgery for paraclinoidal carotid artery aneurysms[J]. J Neurosurg, 1994, 80(4): 650-658.
3 Javalkar V, Banerjee AD, Nanda A. Paraclinoid carotid aneurysms[J]. J Clin Neurosci, 2011, 18(1):13-22.
4 Sengupta RP, Gryspeerdt GL, Hankinson J. Carotid-ophthalmic aneurysms[J]. J Neurol Neurosurg Psychiatry, 1976, 39(9):837-853.
5 Sharma BS, Kasliwal MK, Suri A, et al. Outcome following surgery for ophthalmic segment aneurysms[J]. J Clin Neurosci, 2010, 17(1):38-42.
6 Eliava SS, Filatov YM, Yakovlev SB, et al.Resultsof microsurgical treatment of large and giant ICA aneurysms using the retrograde suction decompression (RSD) technique: series of 92 patients[J]. World Neurosurg, 2010, 73(6): 683-687.
7 Nanda A, Javalkar V. Microneurosurgical management of ophthalmic segment of the internal carotid artery aneurysms: single-surgeon operative experience from Louisiana State University, Shreveport[J]. Neurosurgery, 2011, 68(2): 355-370.
8 Colli BO, Carlotti J, Assirati J, et al.Resultsof microsurgical treatment of paraclinoid carotid aneurysms[J]. Neurosurg Rev,2013, 36(1): 99-114.
9 Froelich SC, Aziz KM, Levine NB, et al. Refinement of the extradural anterior clinoidectomy: surgical anatomy of the orbitotemporal periosteal fold[J]. Neurosurgery, 2007, 61(5 Suppl 2): 179-185.
10 Kim JS, Lee SI, Jeon KD, et al. The pterional approach and extradural anterior clinoidectomy to clip paraclinoid aneurysms[J]. J Cerebrovasc Endovasc Neurosurg, 2013, 15(3):260-266.
11 Sai Kiran NA, Furtado SV, Hegde AS. How I do it : anterior clinoidectomy and optic canal unroofing for microneurosurgical management of ophthalmic segment aneurysms[J]. Acta Neurochir(Wien), 2013, 155(6): 1025-1029.
12 Gross BA, Du R. Microsurgical treatment of ophthalmic segment aneurysms[J]. J Clin Neurosci, 2013, 20(8):1145-1148.
13 Barami K, Hernandez VS, Diaz FG, et al. Paraclinoid carotid aneurysms: surgical management, complications, and outcome based on a new classification scheme[J]. Skull Base, 2003, 13(1):31-41.
14 Chen SF, Kato Y, Subramanian B, et al. Retrograde suction decompression assisted clipping of large and giant cerebral aneurysms: our experience[J]. Minim Invasive Neurosurg, 2011,54(1):1-4.
15 Parkinson RJ, Bendok BR, Getch CC, et al. Retrograde suction decompression of giant paraclinoid aneurysms using a No. 7 French balloon-containing guide catheter. Technical note[J]. J Neurosurg,2006, 105(3): 479-481.
16 Meling TR, Sorteberg A, Bakke SJ, et al. Blood blister-like aneurysms of the internal carotid artery trunk causing subarachnoid hemorrhage: treatment and outcome[J]. J Neurosurg, 2008, 108(4): 662-671.
17 Joo SP, Kim TS, Moon KS, et al. Arterial suturing followed by clip reinforcement with circumferential wrapping for blister-like aneurysms of the internal carotid artery[J]. Surg Neurol, 2006, 66(4): 424-428.
18 Yanaka K, Meguro K, Nose T. Repair of a tear at the base of a blister-like aneurysm with suturing and an encircling clip: technical note[J]. Neurosurgery, 2002, 50(1): 218-221.
19 Lee SK, Kim JM. Internal carotid artery Reconstruction using multiple fenestrated clips for complete occlusion of large paraclinoid aneurysms[J]. J Korean Neurosurg Soc, 2013, 54(6): 477-483.
20 Li J, Lan ZG, Liu Y, et al. Large and giant ventral paraclinoid carotid aneurysms: Surgical techniques, complications and outcomes[J]. Clin Neurol Neurosurg, 2012, 114(7): 907-913.
Surgical strategies and efficacy of paraclinoid aneurysms
SHU Xujun, SUN Zhenghui, WU Chen, WANG Fuyu, WANG Shengbao, XUE Zhe, WANG Wenxin
Department of Neurosurgery, Chinese PLA General Hospital, Beijing 100853, China
SUN Zhenghui. Email: szh301@sina.com
ObjectiveTo investigate the surgical strategies of paraclinoid aneurysms and analyze its clinical outcomes. Methods Clinical data about 46 patients with paraclinoid aneurysm who were surgically treated in our hospital from January 2010 to May 2014 were retrospectively analyzed. Of the 46 patients with total 49 aneurysms, 8 were males, 38 were females with the mean age of 50.15 years (range: 22-72). 17 patients had ruptured aneurysm and 9 patients had multiple aneurysms. There were 22 ophthalmic aneurysms, 10 globe aneurysms, 8 superior hypophyseal aneurysms, 3 carotid cave aneurysms, 1 serpentine aneurysm and 5 pseudoaneurysms. The diameters of 20 aneurysms were smaller than 5 mm, 15 were between 5 mm and 15 mm, and 14 aneurysms were larger than 15 mm. Surgical strategies included simple clipping, clip reconstruction, extracranial-to-intracranial (EC-IC) bypass, cervical ICA ligation and aneurysm wrapping. Clinical outcome was evaluated by Glasgow outcome scale (GOS).Results19 aneurysms were clipped, 21 aneurysms were treated by clip reconstruction, 6 aneurysms were treated by EC-IC bypass, 2 aneurysms were treated by cervical ICA ligation, and 1 aneurysm was treated by wrapping. According to the GOS, 42 patients had good outcomes (GOS 4, 5), 3 had poor outcomes (GOS 2, 3) and 1 was dead (GOS 1).ConclusionAccording to the individual characteristics of paraclinoid aneurysm, appropriate surgical strategies for patients are applied, which can improve the clinical outcomes.
paraclinoidal; intracranial aneurysm; surgical therapy
R 651.1
A
2095-5227(2015)06-0536-05
10.3969/j.issn.2095-5227.2015.06.004
时间:2015-03-10 09:49
http://www.cnki.net/kcms/detail/11.3275.R.20150310.0949.007.html
2014-12-03
北京市科学委员会基金(Z141107002514052)
Supported by Beijing Municipal Science and Technology Commission(Z14 1107002514052)
束旭俊,男,在读硕士。研究方向:脑血管病。Email: 15652797823@163.com
孙正辉,男,博士,出站博士后,副教授,副主任。
Email: szh301@sina.com