标准化指征下胸腔镜手术治疗新生儿先天性膈疝*
何秋明 钟 微 李 乐 余家康 胡 超 张文华 吕俊健 张 红 夏慧敏
(广州市妇女儿童医疗中心新生儿外科,广州 510623)
·临床研究·
标准化指征下胸腔镜手术治疗新生儿先天性膈疝*
何秋明 钟 微**李 乐 余家康 胡 超 张文华①吕俊健②张 红③夏慧敏
(广州市妇女儿童医疗中心新生儿外科,广州 510623)
目的 探讨胸腔镜手术治疗新生儿先天性膈疝(congenital diaphragmatic hernia,CDH)的疗效。 方法 2013年9月~2014年8月应用胸腔镜治疗新生儿先天性膈疝14例,观察孔位于肩胛下角第6肋间,置入5 mm trocar,操作孔2个,分别位于肩胛下角线与脊柱连线中点第5~7肋间和腋前线第5~7肋间,置入3 mm trocar;在6 mm Hg气压维持下,将疝内容物回纳,再降低压力至2~4 mm Hg,以不可吸收线完成膈肌修补。 结果 除1例因脾脏出血中转开腹外,其余13例均顺利完成胸腔镜手术。手术时间90~150 min(平均116 min)。术中监测血气,13例完成胸腔镜手术患儿术中PaCO238~66 mm Hg(平均48 mm Hg),pH 7.18~7.39(平均7.30),乳酸0.55~1.22 mmol/L(平均0.93 mmol/L)。术后呼吸机通气时间49~192 h(平均113 h)。14例随访2~13个月(平均7个月),14例患儿均存活,无复发,1例术后5个月左侧肺炎,1例术后9个月因粘连性肠梗阻行手术治疗,余患儿均无呼吸困难、呼吸道感染症状或肠梗阻发生,生长发育良好。 结论 胸腔镜手术治疗新生儿CDH疗效满意。
先天性膈疝; 新生儿; 胸腔镜
先天性膈疝(congenitial diaphragmatic hernia, CDH)是由于膈肌先天性发育不良而导致的畸形,腹腔脏器经膈肌缺损疝入胸腔,引起一系列病理生理变化,对心肺功能、全身状况均造成不同程度的影响,是新生儿急危重症之一。随着微创外科技术的不断发展,胸腔镜手术治疗新生儿CDH的优势突显,成功病例不断增多。然而国外最新的研究显示,胸腔镜手术加重术中的高碳酸血症及酸中毒,术后复发率较开放手术高,应严格掌握手术指征[1,2]。目前,胸腔镜治疗新生儿CDH的具体指征尚未统一。我院根据欧洲CDH协作组的建议[3]及手术经验制定胸腔镜手术标准化指征:①体重>2.0 kg;②无肝脏疝入;③无肠梗阻;④无肺动脉高压或严重心脏畸形;⑤无须高频振荡通气或体外膜肺治疗。手术时机:①平均动脉压正常水平;②吸入氧浓度<50%、血氧饱和度在85%~95%;③乳酸<3 mmol/L;④尿量>2 ml·kg-1·h-1。2013年9月~2014年8月我科在标准化指征下应用胸腔镜治疗新生儿CDH 14例,效果良好,现报道如下。
1 临床资料与方法
1.1 一般资料
本组14例,男9例,女5例。胎龄37.1~40.1周(平均39.0周)。出生体重2450~3620 g(平均2852 g)。主要临床表现为出生后呼吸困难、青紫等。入院后需机械通气12例。胸腹部X线检查提示左侧膈疝13例、右侧膈疝1例;胸、腹部超声检查提示左侧胸腔疝入物为肠管和脾脏6例,疝入物为肠管7例,右侧胸腔疝入物为肾脏和胃1例(因超声提示胃疝入而行上消化道造影,结果提示胃位置正常,位于左上腹,仅为肠管疝入);心脏彩超检查提示卵圆孔未闭6例,卵孔未闭及动脉导管未闭7例,卵圆孔未闭、动脉导管未闭及永存左上腔静脉1例。经禁食、胃肠减压、监测血气、纠正酸碱紊乱等处理后应用胸腔镜治疗。手术时体重2.50~3.58 kg(平均2.91 kg)。手术日龄2~6 d(平均3.4 d)。术前准备为1~4 d(平均2.4 d)。
1.2 方法
气管插管麻醉(无须单肺通气)。改良卧位:健侧卧位至最大限度的俯卧,垫高胸肋部,患侧上臂屈曲上抬、固定。术者站于患儿头侧,麻醉师及设备位于手术床右侧,护士站于手术床左侧,显示屏位于手术床尾(图1)。应用德国Storz公司腹腔镜。肩胛下角第6肋间直视下5 mm trocar作为腔镜孔,在腔镜观察下置入分别于肩胛下角线与脊柱连线中点第5~7肋间和腋前线第5~7肋间置入2个3 mm trocar作为操作孔。在6 mm Hg气压维持下,以操作钳缓慢轻柔将疝内容物回纳入腹,再降低压力至2~4 mm Hg,清楚暴露膈肌缺损,沿张力较小的缺损边缘开始以2-0或3-0带针不可吸收缝线进行间断缝合完成膈肌修补。对于缺损边缘张力大者,经皮穿刺进针,将膈肌边缘缝合悬吊固定在相邻肋骨上,于皮下完成打结。
术中监测血气,重点记录动脉血二氧化碳分压(PaCO2)、pH、乳酸。术后常规留置胸腔引流管(图2),记录机械通气时间。出院后门诊随访。
2 结果
除1例因脾脏出血中转开腹外,其余13例均顺利完成胸腔镜手术。镜下所见:左侧13例,均为后外侧膈疝,6例疝入内容物为肠管、脾脏,7例仅为肠管;右侧1例,存在疝囊,疝入物为肾脏;缺损面积3.4~12.0 cm2(平均8.9 cm2)。手术时间90~150 min(平均116 min)。术中监测血气,13例完成胸腔镜手术患儿术中PaCO238~66 mm Hg(平均48 mm Hg),pH 7.18~7.39(平均7.30),乳酸0.55~1.22 mmol/L(平均0.93 mmol/L)。术后呼吸机通气时间49~192 h(平均113 h)。复查胸片肺复张后拔除胸腔引流管,拔管时间2~14 d(平均7.3 d)。14例随访2~13个月(平均7个月),均存活,无复发,1例左侧膈疝术后5个月左侧肺炎(图3),1例(脾脏出血中转开腹)术后9个月因粘连性肠梗阻行手术治疗,其余患儿均无呼吸困难、呼吸道感染症状或肠梗阻发生,生长发育良好。
3 讨论
Schaarschmidt等[4]报道新生儿CDH应用胸腔镜比腹腔镜更容易回纳疝入的内容物。Shah等[5]总结微创技术治疗22例CDH的经验,认为对于婴幼儿应用腹腔镜、胸腔镜这2种微创方式均可进行修补,但对于新生儿则建议应用胸腔镜治疗,原因在于胸腔镜下疝内容物容易复位,复位后存在良好的操作空间等多个优点。国内外学者均有类似的经验[6,7]。然而,腔镜与开放术式治疗新生儿CDH效果对比的系统评价[8]表明,腔镜手术可增加危险因素(如气胸所致的高碳酸血症、酸中毒、操作时间更长等)、术后并发症较高(如复发率等),原因除有学习曲线、手术技巧等问题外,更重要的是胸腔镜手术治疗新生儿CDH应有适应证及合适的手术时机。
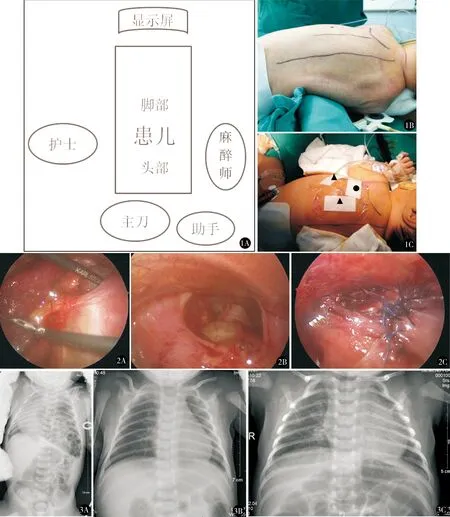
图1 A.胸腔镜治疗新生儿CDH的手术室布局;B.手术体位:垫高胸肋部;C.三孔法操作,●为腔镜孔,▲为操作孔 图2 A.回纳疝内容物;B.疝内容物复位后膈肌缺损;C.膈肌修补完成 图3 男,胸腔镜膈肌修补手术治疗前后的X线表现。A.患儿出生1 d(术前1 d)胸腹平片可见左侧胸腔肠管影,提示左侧膈疝;B.患儿在出生1个月(术后1个月)胸部平片未见膈疝复发;C.患儿出生5个月(术后5个月)胸片提示左侧肺炎,但未见膈疝复发征象
3.1 手术时机与术中并发症的关系
在新生儿腔镜手术中,使用的CO2容易导致新生儿低体温及酸中毒,而CDH患儿往往合并有肺发育不良,CO2建立的气胸或气腹均可能加重肺损伤[9,10]。McHoney等[11]报道传统开放术式平均PaCO2为73 mm Hg,胸腔镜手术平均PaCO2为75 mm Hg;开放、胸腔镜手术中平均pH分别为7.20、7.21,差异均无统计学意义。但最近的临床随机对照研究[12]显示,开放、胸腔镜手术中平均PaCO2分别为68、96 mm Hg,平均pH值分别为7.21、7.08,胸腔镜手术明显加重了患儿术中的高碳酸血症及酸中毒。我科根据欧洲CDH协作组的建议[3]制定胸腔镜手术的时机为:①平均动脉压正常;②吸入氧浓度<50%、血氧饱和度在85%~95%;③乳酸<3 mmol/L;④尿量>2 ml·kg-1·h-1。符合此四项条件者提示血流动力学稳定,可耐受手术。本组13例完成胸腔镜操作术中平均PaCO248 mm Hg,平均pH 7.30,平均乳酸0.93 mmol/L,高碳酸血症及酸中毒情况似乎较上述国外文献报道的好。
3.2 手术适应证
Tsao等[13]对微创治疗CDH进行系统评价,结果显示胸腔镜术后有更高的复发率,并且体外膜肺、需要补片等因素均影响CDH的临床预后。此外,一些较大宗(>20例)胸腔镜手术治疗新生儿CDH的回顾分析结果显示,中转开胸或开腹率高达25%以上,主要原因有缺损大、疝内容物难回纳(如肝疝入)、损伤疝内容物(如脾脏、肠管、胃血管)等[14~16],因此,需要掌握胸腔镜手术适应证。我科制定的胸腔镜手术适应证:①体重>2.0 kg。体重过小者,存在体格较小、手术操作空间不够的可能[17]。Gourlay等[18]曾尝试对1.9 kg的新生儿CDH采用胸腔镜治疗而失败。在较大宗胸腔镜手术治疗新生儿CDH的病例报告中,患儿体重均>2.0 kg[19~22]。②无肝脏疝入。当存在肝脏疝入,尤其是右侧膈疝时,往往提示可能膈肌缺损大,需要应用补片修补,或难以复位,进而导致中转开放手术[17,20,23]。③无肠梗阻。胸腔镜无法解决合并肠旋转不全等消化道畸形,因此,应用胸腔镜治疗前在临床上需要观察胃液性状及有无大便排出,或者行消化道造影以排除有无肠梗阻的可能。④无肺动脉高压或严重心脏畸形。存在严重心血管系统畸形者,提示将不能耐受腔镜手术中可能出现的高碳酸血症[19,24]。⑤无须高频振荡通气或体外膜肺治疗,这是因为应用体外膜肺时难以转运患儿至手术室,而高频振荡通气影响手术操作[23]。
本组均为新生儿患者,除1例由于脾脏较大且出血而中转开腹外,余13例均顺利完成胸腔镜操作。成功的经验在于,病例经标准化指征筛选后,在胸腔镜操作过程中,患儿心肺功能稳定,由于胸腔存在自然空腔,并且新生儿CDH常合并同侧肺发育不良、肺处于萎陷状态,将疝内容物回纳入腹后,操作空间明显增加,易于膈肌修补。本组所有病例术后均存活,术后随访2~13个月,未见复发或膈膨升;1例左侧膈疝术后5个月左侧肺炎;1例术后9个月因粘连性肠梗阻行手术治疗,其余患儿均无呼吸困难、呼吸道感染症状或肠梗阻出现。
因此,在开展胸腔镜治疗新生儿CDH的初期,建议应严格掌握手术适应证及时机、筛选合适患儿应用胸腔镜技术。随着微创技术的提高、适宜器械的开发、手术经验的积累,将打破更多限制,更好地应用微创技术治疗新生儿CDH,但其预后仍需前瞻性、多中心、长期随访的研究进一步明确。
1 Bishay M, Giacomello L, Retrosi G, et al. Hypercapnia and acidosis during open and thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia: results of a pilot randomized controlled trial. Ann Surg,2013,258(6): 895-900.
2 Chan E, Wayne C, Nasr A. Minimally invasive versus open repair of Bochdalek hernia: a meta-analysis. J Pediatr Surg,2014,49(5): 694-699.
3 Reiss I, Schaible T, van den Hout L, et al. CDH EURO Consortium. Standardized postnatal management of infants with congenital diaphragmatic hernia in Europe: the CDH EURO Consortium consensus. Neonatology,2010, 98(4): 354-364.
4 Schaarschmidt K, Strauss J, Kolberg-Schwerdt A, et al. Thoracoscopic repair of congenital diaphragmatic hernia by inflation-assisted bowel reduction, in a resuscitated neonate: a better access? Pediatr Surg Int,2005,21(10): 806-808.
5 Shah SR, Wishnew J, Barsness K, et al. Minimally invasive congenital diaphragmatic hernia repair: a 7-year review of one institution’s experience. Surg Endosc, 2009, 23(6):1265-1271.
6 Gomes Ferreira C, Reinberg O, Becmeur F, et al. Neonatal minimally invasive surgery for congenital diaphragmatic hernias: a multicenter study using thoracoscopy or laparoscopy. Surg Endosc,2009, 23(7): 1650-1659.
7 黄金狮, 陈 快, 戴康临, 等.经胸腔镜手术治疗先天性膈疝的体会.中华小儿外科杂志,2012, 33(5): 340-343.
8 Lansdale N, Alam S, Losty PD, et al. Neonatal endosurgical congenital diaphragmatic hernia repair: a systematic review and meta-analysis. Ann Surg,2010,252(1): 20-26.
9 Wung JT, Sahni R, Moffitt ST, et al. Congenital diaphragmatic hernia: survival treated with very delayed surgery, spontaneous respiration, and no chest tube. J Pediatr Surg,1995,30(3): 406-409.
10 Tobias JD. Anesthetic considerations for laparoscopy in children. Semin Laparosc Surg,1998,5(1): 60-66.
11 McHoney M, Giacomello L, Nah SA, et al. Thoracoscopic repair of congenital diaphragmatic hernia:intraoperative ventilation and recurrence. J Pediatr Surg,2010,45(2):355-359.
12 Bishay M, Giacomello L, Retrosi G, et al. Hypercapnia and acidosis during open and thoracoscopic repair of congenital diaphragmatic hernia and esophageal atresia: results of a pilot randomized controlled trial. Ann Surg,2013, 258(6):895-900.
13 Tsao K, Lally PA, Lally KP. Congenital Diaphragmatic Hernia Study Group. Minimally invasive repair of congenital diaphragmatic hernia. J Pediatr Surg,2011,46(6):1158-1164.
14 Keijzer R, van de Ven C, Vlot J, et al. Thoracoscopic repair in congenital diaphragmatic hernia: patching is safe and reduces the recurrence rate. J Pediatr Surg,2010,45(5):953-957.
15 Gander JW, Fisher JC, Gross ER, et al. Early recurrence of congenital diaphragmatic hernia is higher after thoracoscopic than open repair: a single institutional study. J Pediatr Surg,2011,46(7): 1303-1308.
16 Szavay PO, Obermayr F, Maas C, et al. Perioperative outcome of patients with congenital diaphragmatic hernia undergoing open versus minimally invasive surgery. J Laparoendosc Adv Surg Tech A,2012,22(3):285-289.
17 Gomes Ferreira C, Reinberg O, Becmeur F, et al. Neonatal minimally invasive surgery for congenital diaphragmatic hernias: a multicenter study using thoracoscopy or laparoscopy. Surg Endosc,2009, 23(7):1650-1659.
18 Gourlay DM, Cassidy LD, Sato TT, et al. Beyond feasibility: a comparison of newborns undergoing thoracoscopic and open repair of congenital diaphragmatic hernias. J Pediatr Surg,2009,44(9): 1702-1707.
19 Yang EY, Allmendinger N, Johnson SM, et al. Neonatal thoracoscopic repair of congenital diaphragmatic hernia: selection criteria for successful outcome. J Pediatr Surg,2005,40(9): 1369-1375.
20 Cho SD, Krishnaswami S, Mckee JC, et al. Analysis of 29 consecutive thoracoscopic repairs of congenital diaphragmatic hernia in neonates compared to historical controls. J Pediatr Surg,2009,44(1): 80-86.
21 Okazaki T, Nishimura K, Takahashi T, et al. Indications for thoracoscopic repair of congenital diaphragmatic hernia in neonates. Pediatr Surg Int,2011,27(1): 35-38.
22 Nam SH, Cho MJ, Kim DY, et al. Shifting from laparotomy to thoracoscopic repair of congenital diaphragmatic hernia in neonates: early experience. World J Surg,2013,37(11): 2711-2716.
23 Kim AC, Bryner BS, Akay B, et al. Thoracoscopic repair of congenital diaphragmatic hernia in neonates: lessons learned. J Laparoendosc Adv Surg Tech A,2009,19(4): 575-580.
24 Tobias JD. Anesthetic considerations for laparoscopy in children. Semin Laparosc Surg,1998,5(1): 60-66.
(修回日期:2015-06-29)
(责任编辑:李贺琼)
Outcomes of Thoracoscopic Repair of Congenital Diaphragmatic Hernia in Neonates Under Standardized Indications
HeQiuming,ZhongWei,LiLe,etal.
DepartmentofNeonatalSurgery,GuangzhouWomenandChildren’sMedicalCenter,Guangzhou510623,China
Correspondingauthor:ZhongWei,E-mail:zhongwei71@hotmail.com
Objective To analyze clinical outcomes of thoracoscopic repair of neonatal congenital diaphragmatic hernia (CDH). Methods Clinical data of 14 patients with CDH receiving thoracoscopic repair from September 2013 to August 2014 were retrospectively analyzed. Thoracoscopic observation port was placed at the site of subscapular angle on the sixth intercostal space for a 5 mm trocar. The two operational ports were located at the medium between scapular line and vertebral line on the level of fifth-seventh intercostal space and at the posterior axillary line on the level of fifth-seventh intercostal space, respectively, for 3 mm trocars. The CO2pressure decreased to 2-4 mm Hg after reduction of herniated organ. The diaphragmatic defect was identified and repaired with prolene or polyester fiber interrupted sutures. Results Primary diaphragmatic repair was successfully accomplished under thoracoscope in 13 neonates without perioperative complications, while one patient underwent conversion to open surgery because of spleen bleeding. In the 13 thoracoscopic cases, the intraoperative PaCO2was 38-66 mm Hg (average, 48 mm Hg), the pH value was 7.18-7.39 (average, 7.30), the lactate level was 0.55-1.22 mmol/L (average, 0.93 mmol/L), and the postoperative mechanical ventilation time was 49-192 h(average, 113 h). All the cases were followed up for 2-13 months (average, 7 months). One patient required reoperation for adhesive intestinal obstruction at 9 months after operation and one case suffered pneumonia at 5 months after repair. There were no other long-term complications. Conclusion Strictly following surgical indications for thoracoscopic repair of CDH in neonates could achieve satisfactory efficacy.
Congenital diaphragmatic hernia; Neonate; Thoracoscope
* 广东省自然科学基金项目(项目编号:S201302002738)
R726.1
A
1009-6604(2015)08-0707-04
10.3969/j.issn.1009-6604.2015.08.011
2014-12-22)
** 通讯作者,E-mail:zhongwei71@hotmail.com
① (广州市妇女儿童医疗中心麻醉科,广州 510623)
② (广州市妇女儿童医疗中心新生儿外科重症监护室,广州 510623)
③ (广州医科大学在读研究生,广州 511436)