Comparison of combined phacoemulsification-nonpenetrating deep sclerectomy and phacoemulsificationtrabeculectom y
Tamer Takmaz,Hale Elif Akmeȿe,Nihal Onursever
Department of Ophthalmology,Atatürk Training and Research Hospital,Ankara 06800,Turkey
Comparison of combined phacoemulsification-nonpenetrating deep sclerectomy and phacoemulsificationtrabeculectom y
Tamer Takmaz,Hale Elif Akmeȿe,Nihal Onursever
Department of Ophthalmology,Atatürk Training and Research Hospital,Ankara 06800,Turkey
Received:2014-07-09 Accepted:2014-08-29
·AIM:To compare the outcomes of combinedphacoemulsification and non - penetrating deepsclerectomy (P - DS) with combined phacoemulsificationand trabeculectomy (P- T) in patients who have cataractand moderate - to - severe primary open angle glaucoma(POAG) or pseudoexfoliative glaucoma (PXG).
cataract; deep sclerectomy; glaucoma;phacoemulsification; trabeculectomy
INTRODUCTION
Cataract and glaucoma are the most common leading causes of blindness in the world[1].Both diseases are seen mostly in elderly people.During the first diagnosis of glaucoma in elderly people,most of them has already cataract diagnosis or during the follow up of glaucoma patients cataract develops.In glaucoma patients as cataract progresses,disease also progresses.This progression is generally due to intraocular pressure(IOP)increase.Some studies have demonstrated that IOP decreases after cataract extraction[2-4]. The treatment protocol is different in patients with concomitant cataract and glaucoma.First glaucoma or cataract surgery is done or combined surgeries are preferred.Nowadays combined cataract and glaucoma surgeries are more popular in patients with concomitant cataract and glaucoma.Combined surgeries resulted in greater reduction of IOP contrary to phacoemulsification alone[5,6].Combining cataract extraction with an antiglaucomatous procedure is widely accepted as a suitable surgical intervention for coexisting uncontrolled glaucoma and visually significant cataract[5-13].
In the treatment of cataract,mainly used surgical technique is phacoemulsification.In the treatment of glaucoma, penetrating or non-penetrating filtering surgeries are performed.In non-penetrating filtering surgeries, postoperative complications such as hypotony,maculopathy, hyphema,flat anterior chamber,choroidal detachment, intraocular inflamation and endophthalmitis are seen less than penetrating filtering surgeries[14,15].Patients for whom such complications are of predictable concern may be good candidates for non penetrating surgeries.
In this study,we compared the effectiveness of combined phacodeep sclerectomy surgery with combined phacotrabeculectomy surgery in patients with visually significant cataract and moderate to severe glaucoma.There are studies comparing any combination of phacoemulsification,nonpenetrating filtration surgery and trabeculectomy for openangle glaucoma,but to our knowledge there is no other study comparing combined phacoemulsification and non-penetrating deep sclerectomy(P-DS)with phacoemulsification and trabeculectomy(P-T)in patients with moderate-to-severe glaucoma.
SUBJECTS AND METHODS
In this prospective randomized study,40 eyes of 40 patients with cataract and primary open angle glaucoma(POAG)or pseudoexfoliative glaucoma(PXG)underwent random ly, either combined P-DS or combined P-T operations.The randomization was performed as follows;the first patients with POAG and PXG diagnosis underwent P-T and the second patients underwent P-DS operations.The operations were performed in this way until there were 20 patients in each group.Patients with visually significant cataract and moderate to severe glaucoma with antiglaucomatous therapy were included in the study.Exclusion criteria were as follows; open angle glaucoma except POAG and PXG,posttraumatic, uveitic,neovascular and dysgenetic glaucomas,angle-closure glaucoma,history of previous ocular surgery,infection and uveitis,severe anterior and posterior segment pathology, intraocular tumors,serious systemic diseases and rheumatic disease.POAG diagnosis criteria was as follows;IOP was over 20 mm Hg without medication,anterior chamber angles were open with gonioscopy,optic nerve head examination and visual field analysis were compatible with glaucoma and retinal nerve fiber layer changes were seen either with optical coherence tomography(OCT)or Heidelberg retina tomograph (HRT).Patients were identified as PXG when they had the criteria as POAG and additionally they had pseudoexfoliative material observed with biomicroscopic examination.
The study protocol adhered to the tenets of the Declaration of Helsinki.Written informed consent was taken from all patients after explaining details about the surgical procedure, beneficial effects,complications and alternatives of the procedure.
Detailed ophthalmic examination and glaucoma tests were performed in all patients before surgical procedures.Bestcorrected visual acuity,biomicroscopy,IOP measurement with Goldmann applanation tonometry(IOP measurements were performed between 9.00-11.00 a.m.),gonioscopy and fundus examination were performed.Automated standard static threshold perimetry(24-2 Sita-Fast strategy)was performed with the Humphrey Field Analyzer(Humphrey Instruments,San Leandro,CA,USA).Retinal nerve fiber layer and optic disc analysis with HRT(HeidelbergEngineering,GmbH,Heidelberg,Germany)and/or OCT (RTVue,Optovue,Inc.Fremont,CA,USA)were also performed in possible conditions and number of glaucoma medications were recorded.Staging of the glaucoma as moderate-to-severe was defined according to Hodapp et al[16]glaucoma grading scale.
All separate-site combined P-T and P-DS procedures were performed under peribulbar anaesthesia by the same surgeon (Takmaz T).In P-DS group,procedure started with creation of a fornix-based conjunctival flap.First,a superficial,onethird partial thickness,5.0×5.0 mm scleral flap was dissected anteriorly 1.0 mm into the clear cornea,and than a second deep scleral flap 1.0 mm within the edges of the superficial flap was dissected nearly half way,until Schlemm's canal.At this time,the surgeon switched to phacoemulsification.After phacoemulsification,the second flap was dissected further,Schlemm's canal deroofed,the deep scleral flap was excised and juxtacanalicular meshwork was removed.The intrascleral space was filled with viscoelastic substance and any implant was not used.The superficial scleral flap was closed with 10-0 buried nylon sutures and the conjunctiva was sutured watertight.
In P-T group,procedure started with creation of a fornixbased conjunctival flap.A 1/3 to1/2 partial thickness scleral flap was dissected in 4.0×4.0 mm rectangular configuration. Then,the surgeon switched to phacoemulsification.After phacoemulsification,a posterior lip sclerectomy sized 1.0-1.5 mm was created with a punch and a peripheral iridectomy was performed in all cases,routinely.The scleral flap was closed with 10-0 buried nylon sutures and the conjunctiva was sutured watertight.
In both groups,standard torsional phacoemulsification with intraocular lens(IOL)implantation was performed through a 2.2 mm clear corneal incision.Following incisions,an ophthalmic viscoelastic device(OVD)was instilled in the anterior chamber and continuous curvilinear capsulorhexis, approximately 5.0 mm in diameter was created.After hydrodissection,torsional phacoemulsification was performed withInfiniti Vision Systems phaco unit(Alcon Laboratories, Inc.)and remaining cortical material was removed with bimanual infusion/aspiration cannulas.After removing the cortex,a foldable,aspheric,one-piece AcrivaUD 613 IOL (VSY Biotechnology,Istanbul,Turkey)was inserted into the capsular bag.Incisions were closed by stromal hydration and the phacoemulsification was completed.
Patients were hospitalized one day and after discharge from hospital,examined on 10d and in 1,3,6 and 12mo after surgery.Postoperatively,topical antibiotic,lomefloxacin 0.3%(Okacin;Novartis Pharma,Basel,Switzerland)twice daily was used for ten days and topical prednisolone acetate 1%(Pred Forte;Allergen,Westport Co.,Mayo,Ireland) eyedrops five times daily was used over 2 to 3mo on a tapering schedule.Complications were recorded.If the IOP level was over target IOP and thought to be high for the status of the optic nevre,antiglaucomatous medications were added.When needed Nd:YAG laser goniopuncture in P-DS group and needling in P-T group were performed.
Most of the patients were considered to have advanced glaucoma,that's why complete and qualified success was defined accordingto the Advanced Glaucoma Intervention Study(AGIS)[17].Complete success was defined as an IOP of 18 mm Hg or lower without any additional medication and qualified success was defined as an IOP of 18 mm Hg or lower with antiglaucomatous medications.
Statistical analysis was performed using the SPSS 16.0 software package for Windows(SPSS Inc.).Mann-Whitney U test(Two-independent samples test)was used to compare means between groups.To evaluate the within group differences Wilcoxon signed-rank test was used.The Chisquare test was used for comparison of the categorical variables between the two groups.All P values were 2-sided and differences were considered significant if the P value was less than 0.05.
RESULTS
The age and sex distribution were similar in both groups(P>0.05)(Table 1).Number of POAG and PXG patients were not different(P>0.05)(Table 1).
There was no difference between groups in terms of preoperative visual acuity(VA),IOP,central corneal thickness,vertical cup/disc ratio,visual field results and number of medications(Table 1).
One year after the surgery VA,IOP,number of medications and success rates were similar in both groups(Table 2). When postoperative results were compared to preoperative values in each group,it was seen that visual acuity increased, IOP and number of medications decreased(P<0.01).These changes were also similar in both groups(P>0.05).
Postoperative IOPs were 15.0 and 14.5 mm Hg,with 0.8 and 0.5 medications in P-DS and P-T groups respectively. Although it is not statistically significant,postoperative both IOPs(P=0.472)and number of medications(P=0.307) were slightly lower in P-T group than in P-DS group.In all patients,IOP was 18 mm Hg or lower,with or without additional antiglaucomatous medication.Qualified success was 100%in both groups and complete success was slightly better in P-T group;60%vs 50%(P=0.530).
There was not any intraoperative complication in both groups. Nd:YAG laser goniopuncture was applied in 7 eyes(once in 5 eyes and twice in 2 eyes)in P-DS group.Needling was performed in 1 eye in P-T group.
Table 1 Preoperative demographic data and ocular measurements±s
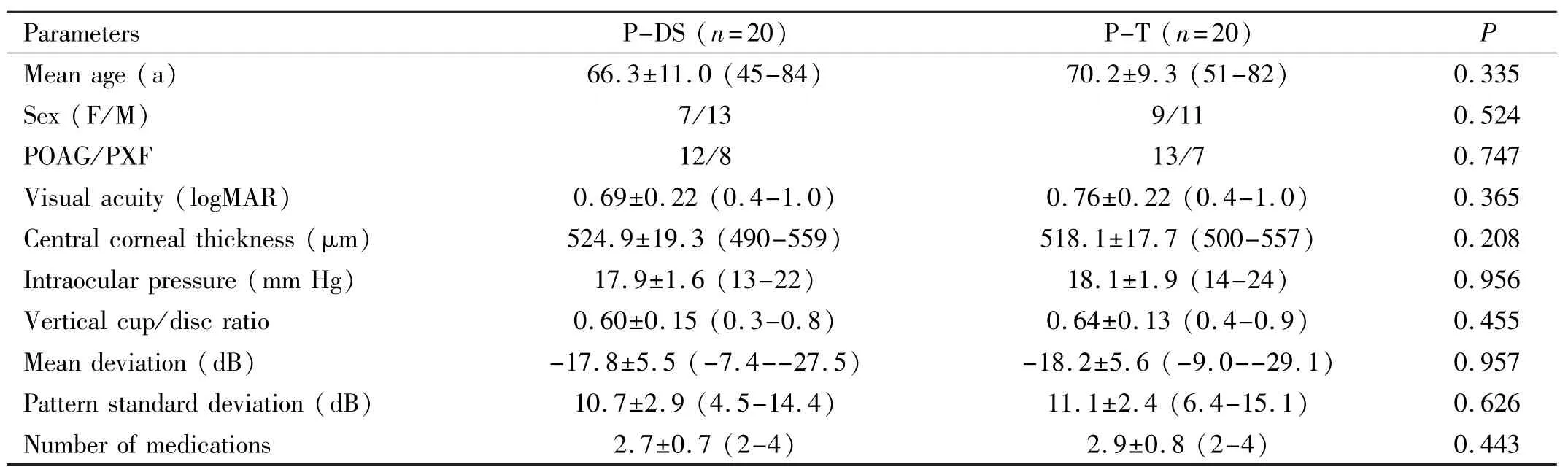
Table 1 Preoperative demographic data and ocular measurements±s
POAG:Primary open angle glaucoma;PXG:Pseudoexfoliative glaucoma.
Parameters P-DS(n=20)P-T(n=20)P Mean age(a)66.3±11.0(45-84)70.2±9.3(51-82) 0.443 0.335 Sex(F/M)7/13 9/11 0.524 POAG/PXF 12/8 13/7 0.747 Visual acuity(logMAR)0.69±0.22(0.4-1.0)0.76±0.22(0.4-1.0)0.365 Central corneal thickness(μm)524.9±19.3(490-559)518.1±17.7(500-557)0.208 Intraocular pressure(mm Hg)17.9±1.6(13-22)18.1±1.9(14-24)0.956 Vertical cup/disc ratio 0.60±0.15(0.3-0.8)0.64±0.13(0.4-0.9)0.455 Mean deviation(dB)-17.8±5.5(-7.4--27.5)-18.2±5.6(-9.0--29.1)0.957 Pattern standard deviation(dB)10.7±2.9(4.5-14.4)11.1±2.4(6.4-15.1)0.626 Number of medications 2.7±0.7(2-4)2.9±0.8(2-4)
Table 2 Ocular measurements and success rate one year after the surgery±s

Table 2 Ocular measurements and success rate one year after the surgery±s
Parameters P-DS(n=20)P-T(n=20)P Visual acuity(logMAR)0.19±0.20(0.0-0.7)0.16±0.16(0.0-0.5)0.784 Post op intraocular pressure(mm Hg) 10d 13.2±1.5(11-16)12.2±1.2(11-15)0.058 1mo 14.8±1.2(12-18)15.3±1.3(13-19)0.192 3mo 15.2±1.4(12-19)14.8±1.1(13-17)0.183 6mo 14.5±1.8(11-17)13.9±1.6(11-16)0.211 1y 15.0±1.7(13-18)14.5±1.6(11-17)0.472 Number of medications 0.8±0.9(0-2)0.5±0.7(0-2)0.307 Success(complete/qualified)10/10 12/8 0.530
DISCUSSION
Combined surgeries in patients with cataract and glaucoma are widely used procedures nowadays[5-13].This is generally due to frequent coincidence of cataract and glaucoma in the elderly population and frequent occurence of cataract progression after glaucoma surgery[9,10,18-20].The main advantages of combined surgeries are to reduce the number of surgical procedure and to reduce the bleb failure risk after cataract surgery alone.
Combined surgeries in glaucoma,especially in severe cases, is one of the controversial subjects in ophthalmology.In these patients first glaucoma or cataract surgery or combined surgeries may be performed.In our study,the average IOPs before the operations seemed within normal limits,but in most patients IOP was over 18 mm Hg with 3 or more medications and some patients had progression.Although phacoemulsification alone may reduce IOP and these glaucoma interventions may result in some serious complications we planned and performed combined glaucoma and cataract surgeries in these patients because the disease was progressive and according to AGIS the IOP should be under 18 mm Hg in these patients[17].
There are many different glaucoma surgical procedures and either penetrating or non penetrating filtration surgeries may be performed during combined surgeries.With regards to success rate of glaucoma procedures,same success rates are observed in both kinds of procedures but complication rates are lower in non penetrating surgeries[8,14].So,is there any superiority of non penetrating surgeries to the penetrating surgeries,if the same success rates are observed?This is widely discussed question nowadays.Non penetrating deep sclerectomy has been more widely used glaucoma procedure because of its intraoperative safety,fewer early postoperative complications and IOP lowering effect that is comparable to trabeculectomy[21-24].The advantage of nonpenetrating glaucoma procedures is lowering the IOP in a controlled manner so that VA results are better than penetrating surgeries,infection rate is lower than penetrating surgeries. On the other hand,trabeculectomy has been known as gold standard technique in glaucoma in spite of higher complication rates compared to non penetrating filtration surgeries.Better IOP decrease,lower number of medications necessary after surgery are the main advantages of penetrating filtration surgery.Although trabeculectomy is accepted as gold standard surgical procedure in glaucoma,in non penetrating filtering surgeries,some postoperative serious complications such as hypotony,maculopathy,flat anterior chamber,choroidal detachment and endophthalmitis are seen less than trabeculectomy[14,15].Because our patients had moderate-to-severe glaucoma,we applied more safe non-penetrating surgery in some of the patients although it's known to end up with less IOP lowering effect unlike conventional treatment and compared the results.
According to our study,IOP decrease after surgery was similar in both groups.Similarly,Gianoli et al[8]observed no statistical difference between phaco-DS and phaco-trab in IOP lowering effect.On the other hand,they reported more complication rates in phacotrab group compared to phaco DS. In our study,the results were also similar but we didn't observe any severe complication in both groups.Shingleton et al[5]performed combined P-T in eyes with pseudoexfoliation glaucoma and stated that uneventful surgeries resulted in significant long-term reduction in IOP and glaucoma medication requirements.Cabarga-Nozal et al[25]evaluated and compared the results and complications after uneventful phaco-deep sclerectomy in one eye with intended phaco-deep sclerectomy converted to phaco-trabeculectomy in the fellow eye.They found no differences in VA or IOP control between uneventful phaco-deep sclerectomy and phaco-deep sclerectomy converted to phaco-trabeculectomy.However, they indicated that fewer drugs were needed to successfully control IOP and the rate of complications was lower if phacodeep sclerectomy was completed uneventfully and 24mo after the surgeries the IOPs were 13.31 and 14.44 in P-DS and P-T, respectively.Cillino et al[11]also compared the efficacy of PDS without implant with punch trabeculectomy,and evaluated the effect of simultaneous temporal approach phacoemulsification on both techniques.Twenty-four months after the procedures the IOPs were 16.5 and 17.3 mm Hg in P-DS and P-T respectiveley,but at the endpoint they were 15.7 and 13.8 mm Hg.As a result,they indicated that both techniques controlled IOP efficaciously,phacoemulsification combined with penetrating and non-penetrating procedures did not seem to interfere with final results but when a lower target IOP and probability of success over time were considered,punch trabeculectomy,single or combined, exhibited a better trend.
We performed laser goniopuncture in 7 eyes in deep sclerectomy group.In some studies,high rate of Nd:YAG laser goniopunctures were reported[26].Nd:YAG laser goniopuncture is a simple technique that is necessary if the percolation through the trabeculodescemet membrane is insufficient.By this procedure nonpenetrating surgery is turned to penetrating surgery but complications of penetrating surgery are not seen because of IOP decrease in a controlled manner.
Which glaucoma surgery technique should be preferred when we decide to perform combined surgery?As same IOP could not be targeted to all glaucoma patients,same surgical technique could not be applied to all glaucoma patients.The treatment protocol changes individually because of different target IOP for each patient depending on glaucomatous effect on each eye.According to the AGIS complete success was defined as an IOP of 18 mm Hg or lower without any additional medication and qualified success was defined as an IOP of 18 mm Hg or lower with antiglaucomatous medications[17].In our study,one year after the surgery IOP, number of medications and success rates were similar in both groups.In all patients,IOP was 18 mm Hg or lower,with or without additional antiglaucomatous medication.Qualified success was 100%in both groups and complete success was slightly better in P-T group;60%vs 50%.Complete success rate seems low in both groups and we think that the main cause of this result is,our patients had moderate-to-severe glaucoma in both groups and the preoperative number of medications were also high.
While we didn't observe any complication in both groups, generally complication rates are higher in penetrating glaucoma surgeries.According to some literatures,nonpenetrating glaucoma surgeries are more suitable for patients with high hyperopias,maculopathy,diabetes and hemorrhagic risk because of higher complication rates in penetrating glaucoma surgeries[11,27].
In conclusion,in patients with coexisting cataract and moderate-to-severe glaucoma,both combined P-DS and PT may be performed safely.In our study,reliability and efficacy were similar in both groups.After penetrating glaucoma surgeries,severe complications threatening the vision may occur especially in moderate-to-severe glaucoma patients,that's why non-penetrating glaucoma surgeries may be performed in order to protect the patient from probable intraoperative and postoperative complications.But follow-up of P-DS patients should be done cautiously because IOP might rise after the surgery and when necessary laser goniopuncture should be performed.
REFERENCES
1 Resnikoff S,Pascolini D,Etya'ale D,Kocur I,Pararajasegaram R, Pokharel GP,Mariotti SP.Global data on visual impairment in the year 2002.Bull World Health Organ 2004;82(11);844-851
2 Merkur A,Dam ji KF,Mintsioulis G,Hodge WG.Intraocular pressure decrease after phacoemulsification in patients with pseudoexfoliation syndrome.J Cataract Refract Surg2001;27(4):528-532
3 Shingleton BJ,Laul A,Nagao K,Wolff B,O'Donoghue M,Eagan E, Flattem N,Desai-Bartoli S.Effect of phacoemulsification on intraocular pressure in eyes with pseudoexfoliation:single-surgeon series.J Cataract Refract Surg2008;34(11):1834-1841
4 Shrivastava A,Singh K.The impact of cataract surgery on glaucoma care.Curr Opin Ophthalmol 2014;25(1):19-25
5 Shingleton BJ,Wooler KB,Bourne CI,O'Donoghue MW.Combined cataract and trabeculectomy surgery in eyes with pseudoexfoliation glaucoma.J Cataract Refract Surg2011;37(11):1961-1970
6 Budenz DL,Gedde SJ.New options for combined cataract and glaucoma surgery.Curr Opin Ophthalmol2014;25(2):141-147
7 Lüke C,Dietlein TS,Lüke M,Konen W,Krieglstein GK.A prospective trial of phacotrabeculotomy combined with deep sclerectomy versus phaco-trabeculectomy.Graefes Arch Clin Exp Ophthalmol2008; 246(8):1163-1168
8 Gianoli F,Schnyder CC,Bovey E,Mermoud A.Combined surgery for cataract and glaucoma:phacoemulsification and deep sclerectomy compared with phacoemulsification and trabeculectomy.J Cataract Refract Surg1999;25(3):340-346
9 Rosdahl JA,Chen TC.Combined cataract and glaucoma surgeries: traditional and new combinations.Int Ophthalmol Clin2010;50(1):95-106
10 Casson RJ,Salmon JF.Combined surgery in the treatment of patients with cataract and primary open-angle glaucoma.J Cataract Refract Surg2001;27(11):1854-1863
11 Cillino S,Di Pace F,Casuccio A,Calvaruso L,Morreale D,Vadala M,Lodato G.Deep sclerectomy versus punch trabeculectomy with or without phacoemulsification:a randomized clinical trial.J Glaucoma 2004;13(6):500-506
12 Gindroz F,Roy S,Mermoud A,Schnyder CC.Combined Ex-PRESS LR-50/IOL implantation in modified deep sclerectomy plus phacoemulsification for glaucoma associated with cataract.Eur J Ophthalmol 2011;21(1):12-19
13 Yuen NS.Early results of modified nonpenetrating deep sclerectomy and phacoemulsification in the treatment of open angle glaucoma and cataract.Eur J Ophthalmol 2009;19(1):72-79
14 Mermoud A,Schnyder CC,Sickenberg M,Chiou AG,Hediguer SE, Faggioni R.Comparison of deep sclerectomy with collagen implant and trabeculectomy in open-angle glaucoma.J Cataract Refract Surg 1999; 25(3):323-331
15 Ang GS,Varga Z,Shaarawy T.Postoperative infection in penetrating versus non-penetratingglaucoma surgery.Br J Ophthalmol 2010;94 (12):1571-1576
16 Hodapp E,Parrish RK II,Anderson DR.Clinical decisions in
glaucoma.St.Louis:CV Mosby-Year Book Medical Publishers;1993: 52-61
17 The Advanced Glaucoma Intervention Study(AGIS):7.The relationship between control of intraocular pressure and visual field deterioration.The AGIS Investigators.Am J Ophthalmol2000;130(4): 429-440
18 Verges C,Cazal J,Lavin C.Surgical strategies in patients with cataract and glaucoma.Curr Opin Ophthalmol2005;16(1):44-52
19 Mathew RG,Murdoch IE.The silent enemy:a review of cataract in relation to glaucoma and trabeculectomy surgery.Br J Ophthalmol2011; 95(10):1350-1354
20 Patel HY,Danesh-Meyer HV.Incidence and management of cataract after glaucoma surgery.Curr Opin Ophthalmol2013;24(1):15-20
21 El Sayyad F,Helal M,El-Kholify H,Khalil M,El-Maghraby A. Nonpenetrating deep sclerectomy versus trabeculectomy in bilateral primary open-angle glaucoma.Ophthalmology2000;107(9): 1671-1674
22 Shaarawy T,Karlen M,Schnyder C,Achache F,Sanchez E, Mermoud A.Five year results of deep sclerectomy with collagen implant. J Cataract Refract Surg 2001;27(11):1770-1778
23 Ambresin A,Shaarawy T,Mermoud A.Deep sclerectomy with collagen implant in one eye compared with trabeculectomy in the other eye of the same patient.J Glaucoma 2002;11(3):214-220
24 Guedes RA,Guedes VM.Nonpenetrating deep sclerectomyin Brazil: a 3-year retrospective study.J Fr Ophthalmol 2005;28(2):191-196
25 Cabarga-Nozal C,Arnalich-Montiel F,Fernandez-Buenaga R, Hurtado-Cena FJ,Munoz-Negrete FJ.Comparison between phaco-deep sclerectomy and phaco-deep sclerectomy reconverted into phacotrabeculectomy:series of fellow eyes.Graefes Arch Clin Exp Ophthalmol 2010;248(5):703-708
26 Sanchez E,Schnyder CC,Sickenberg M,Chiou AG,Hediguer SE, Mermoud A.Deep sclerectomy:results with and without collagen implant.Int Ophthalmol 1996-1997;20(1-3):157-162
27 Mermoud A,Schnyder CC.Nonpenetrating filtering surgery in glaucoma.Curr Opin Ophthalmol2000;11(2):151-157
白内障超声乳化术联合非穿透性深层巩膜切除术与联合小梁切除术的疗效比较
Tamer Takmaz,Hale Elif Akmeȿe,Nihal Onursever
(作者单位:土耳其,安卡拉06800,阿塔蒂尔克教育与研究医院,眼科)
Tamer Takmaz.ttakmaz@gmail.com
目的:比较白内障超声乳化术联合非穿透性深层巩膜切除术(P-DS)和白内障超声乳化术联合小梁切除术(P-T)在白内障合并中度至重度原发性开角型青光眼(POAG)或假性剥脱性青光眼(PXG)患者中的疗效。方法:前瞻随机性研究。选取40例(40眼)白内障合并POAG或PXG患者,所有患者均接受全面眼部检查和青光眼测试。每组20眼,分别在局部麻醉下行P-DS或P-T。术前,术后10d,1、3、6、12mo记录视力、眼压及青光眼用药量。并对P-DS组行激光前房角穿刺、P-T组行普通穿刺的术后并发症记录。结果:两组患者年龄(P-DS组:66.3±11.0;P-T组:70.2± 9.3岁)和性别(P-DS组:女7,男13;P-T组:女9,男11)分布相似(P>0.05)。POAG和PXG患者在两组(P-DS组,P-T组)中分别为12例和8例,13和7例(P>0.05)。两组在术前视力(P-DS组:0.69±0.22 logMAR;P-T组: 0.76±0.22 logMAR)、眼压(P-DS组:17.9±1.6 mm Hg;P-T组:18.1±1.9 mm Hg)及用药量(P-DS组:2.7±0.7;P-T组:2.9±0.8)差异均无统计学意义(P>0.05)。与术前相比,两组术后均出现视力提高,眼压和用药量减少的现象(P<0.01)。术后两组(P-DS组,P-T组)眼压分别为15.0±1.7mm Hg和14.5±1.6 mm Hg(P=0.472)。术后P-T组(0.5±0.7)的用药量略少于P-DS组(0.8± 0.9)(P=0.307)。两组中均无并发症。P-DS组中7眼(5眼一次;2眼两次)行激光前房角穿刺;P-T组中1眼行普通穿刺。结论:同时患有白内障和青光眼的患者行联合P-DS与PT具有一定安全性。两组的可靠性与疗效相当。对P-DS组应进行密切随访,如果有必要应行激光前房角穿刺。
白内障;深层巩膜切除术;青光眼;白内障超声乳化术;小梁切除术
Tamer Takmaz.Umit Mah.2449, Sokak,Kardelen Sitesi A Blok No:7/35 Umitkoy Ankara 06800,Turkey.ttakmaz@gmail.com
10.3980/j.issn.1672-5123.2015.11.04
:Takmaz T, Akmeȿe HA, Onursever N. Comparison ofcombined phacoemulsification - non - penetrating deep sclerectomyand phacoemulsification-trabeculectomy. Guoji Yanke Zazhi(Int EyeSci) 2015;15(11):1851-1856
引用:Takmaz T,Akmeȿe HA,Onursever N.白内障超声乳化术联合非穿透性深层巩膜切除术与联合小梁切除术的疗效比较.国际眼科杂志2015;15(11):1851-1856
·METHODS:In this prospective randomized study 40eyes of 40 patients with cataract and POAG or PXG wereevaluated. Complete eye examination and glaucoma testswere performed in all patients. Combined P-DS and P- Twere performed under local anesthesia in 20 eyes in eachgroup. Visual acuity ( VA ), intraocular pressure ( IOP )and number of glaucoma medications were all recordedpreoperatively and postoperative on 10d, 1, 3, 6 and12mo. Complications, laser goniopuncture in P-DS groupand needling in P-T group were also recorded.
·RESULTS:The age (P-DS, 66. 3 ± 11. 0 and P- T, 70. 2 ±9. 3y) and sex distribution (P-DS, 7 female and 13 male,P-T, 9 female and 11 male) were similar in both groups(P> 0. 05). Number of POAG and PXG patients were 12and 8, and 13 and 7 in P-DS and P-T groups, respectively(P > 0. 05 ). There was no difference between groups interms of preoperative VA (P-DS, 0. 69±0. 22 and P-T, 0. 76±0. 22 logMAR), IOP (P-DS, 17. 9±1. 6 and P-T, 18. 1±1. 9mm Hg) and number of medications (P-DS: 2. 7±0. 7 andP-T: 2. 9±0. 8), (P>0. 05). VA increased, IOP and numberof medications decreased in both groups postoperatively(P< 0. 01). Postoperative IOPs were 15. 0±1. 7 and 14. 5±1. 6 mm Hg in P - DS and P - T groups respectively (P =0. 472 ). Postoperative number of medications wereslightly better in P-T group (0. 5±0. 7) than in P-DS group(0. 8± 0. 9) (P = 0. 307). There were no complications inboth groups. Laser goniopuncture was applied in 7 eyes(once in 5 eyes and twice in 2 eyes) in P - DS group.Needling was performed in 1 eye in P-T group.
·CONCLUSION: In patients with coexisting cataract andglaucoma, both combined P - DS and P - T may beperformed safely. Reliability and efficacy were similar inboth groups. Follow - up of P - DS should be donecautiously and when necessary laser goniopunctureshould be performed.
- 国际眼科杂志的其它文章
- LASEK for the correction of hyperopia with mitomycin C using SCHWIND AMARIS excimer laser:one-year follow-up
- Hospitalised ocular injuries in Osogbo,Nigeria
- Com parison of sub-Tenon's anaesthesia in phacoemulsification w ith 3 and 5 m L lidocaine
- 豚鼠早期实验性近视眼视网膜色素上皮细胞bFGF表达变化的研究
- 小鼠眼眶成纤维细胞TLR4基因静默对甲状腺眼病的效应研究
- 小鼠视网膜电图随生长发育的变化特点