Com parison of sub-Tenon's anaesthesia in phacoemulsification w ith 3 and 5 m L lidocaine
Muge Coban-Karatas,Oya Yalcin Cok,Rana Altan-Yaycioglu
1Department of Ophthalmology,School of Medicine,Baskent University,Adana 01250,Turkey
2Department of Anesthesiology,School of Medicine,Baskent University,Adana 01250,Turkey
Com parison of sub-Tenon's anaesthesia in phacoemulsification w ith 3 and 5 m L lidocaine
Muge Coban-Karatas1,Oya Yalcin Cok2,Rana Altan-Yaycioglu1
1Department of Ophthalmology,School of Medicine,Baskent University,Adana 01250,Turkey
2Department of Anesthesiology,School of Medicine,Baskent University,Adana 01250,Turkey
Received:2015-02-02 Accepted:2015-05-23
·AIM:To compare the effect of sub- Tenon anesthesia3 mL and 5 mL lidocaine on intraocular pressure (IOP),analgesia and akinesia. Sub - Tenon's anaesthesia is acommon regional technique for cataract surgery byphacoemulsification. As a volume - based block, IOPoptimization along with analgesia and akinesia is aconcern for successful surgical course.
sub - Tenon's anaesthesia; intraocularpressure; phacoemulsification; akinesia; pain
INTRODUCTION
Cataract surgery is one of the most common outpatient procedures and can be safely performed with a regional nerve block.Sub-Tenon's anaesthesia is a valuable technique in modern intraocular surgery which involves using a blunt cannula,thereby c
onsiderably reducing the risks associated with the use of a sharp needle in the orbit[1-4].In this prospective randomized study,we evaluated the intraocular pressure(IOP)changes,analgesia and akinesia in two different volumes of local anesthetic in patients undergoing routine cataract surgery with sub-Tenon's anaesthesia.
SUBJECTS AND METHODS
This prospectively designed study enrolled patients with cataract scheduled for phacoemulsification with intraocular lens implantation.It was approved by Baskent University Institutional Review Board and Ethics Committee(Project nr: KA 14/34).A written informed consent was obtained from all participants.Total of 70 patients,with American Society of Anesthesiology(ASA)physical statusⅠ-Ⅲwere included. Exclusion criteria were allergy to lidocaine,history of previous retinal and strabismus surgery,and presence of glaucoma or high IOP.
All the patients received sub-Tenon's anaesthesia with 2% lidocaine.The block was performed using Corbin sub-Tenon's anaesthesia cannula smooth rounded tip,0.3 mm side port 23 gauge(Katena Instruments)through an inferonasal conjunctival incision 5-6 mm posterior to limbus into sub-Tenon's space posterior to the equator of the globe by the same surgeon(Coban-Karatas M).After administration of anaesthetic no ocular massage was performed.Patients were random ly enrolled to the study to receive sub-Tenon's block either with 3 mL(Group I)or 5 mL(Group II)lidocaine and were not informed at any stage which volume of anaesthetic they had received.Prior to the study,sealed envelopes from a computer-generated table was prepared by a nurse who was not associated with the study,and the envelopes were opened by the investigators just before the injection.
Table 1 Characteristics of the patients(n,±s)

Table 1 Characteristics of the patients(n,±s)
Parameters Group Ⅰ Group Ⅱ Age(a)62.9±9.3 67.4±8.2 Gender(F/M)10/22 13/21 Physicalstatus(ASAⅠ/Ⅱ/Ⅲ)9/12/11 13/10/11 Axial length(mm)23.4±1.3 23.5±1.1
Standard monitoring included electrocardiography,pulse oximetry and non-invasive blood pressure monitoring.No patients received any sedation during the procedure.
All IOP recordings and evaluation of analgesia and akinesia were performed by a masked physician(Altan-Yaycioglu R). IOP was measured by Icare Pro©(Icare,Tiolat Oy Helsinki, Finland)before and 10min after the block.The akinesia of the anaesthetic was evaluated 10min after the block.Akinesia was subjectively graded as 0-3(0:no eye movements in all fields of gaze,1:minor eye movements in one or two gazes, 2:moderate eye movements in more than 2 gazes,3:full eye movements in all gazes).At the end of the cataract procedure the patient was asked by the same masked physician about the level of pain and graded as 0-3(0:no pain,1:mild pain, 2:moderate pain,3:severe pain).Complications such as chemosis and subconjunctival hemorrhage were also noted.
Statistical AnalysisStatistical analysis was performed using the statistical package SPSS software(Statistical Package for the Social Sciences,version 17.0,SPSS Inc.,Chicago,III, USA).For each continuous variable,normality was checked by Kolmogorov-Smirnov test and by histograms.Comparisons between the groups were performed with Student's t-test for normally distributed data,and with Mann-Whitney U test for the data not normally distributed.The categorical variables were analyzed using Fisher exact and Chi-square tests where appropriate.Values of P less than 0.05 were considered statistically significant.
RESULTS
A total of 70 eyes of 70 patients were included in the study. Two patients were excluded due to the patients' request for sedation during block administration.Data of 2 patients were excluded from the statistical analysis due to possible of deviation from the study blindness protocol.Therefore,a total of 66 patients completed the study.Patients' characteristics such as age,weight,height,axial length,ASA physical status were comparable between groups(Table 1).IOP revealed no statistically significant alteration in both groups before and 10min after the block(P<0.05)(Table 2). Akinesia and analgesia were significantly better in Group II in comparison to Group I.“No eye movement”was obtained in 13 patients(38.2%)in Group II whereas none of the patients had“no eye movement”in Group I(Figure 1). Eighteen(56.3%)patients had“no pain”and 14(43.7%)patients had“mild and moderate pain”in Group Ⅰ whereas“No pain”in 28 patients(82.4%)and“mild pain”in 6 patients(17.6%)were observed in Group Ⅱ(Figure 2). Complications were comparable between groups.
Table 2 Intraocular pressure measurements(±s)

Table 2 Intraocular pressure measurements(±s)
Intraocular pressure(mm Hg)Group Ⅰ Group Ⅱ Before the block 20.1±3.2 19.5±3.1 At 10min after the block 19.7±3.1 20.4±3.4

Figure 1 Akinesia in patientsaP=0.000.
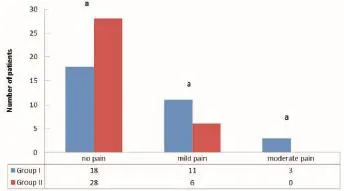
Figure 2 Pain in patientsaP=0.037.
DISCUSSION
The sub-Tenon block was introduced as a simple,effective and safer block for routine ophthalmic procedures[3,4].It provides effective anaesthesia to the orbit with a lower incidence of sight threatening complications than sharp needle techniques[1].The use of sub-Tenon's block appears to have increased rapidly in many countries.Sub-Tenon's block will reduce the incidence of serious complications that occur with traditional needle blocks[5,6].Common complications of sub-Tenon's anesthesia are mostly minor[7].These include pain upon injection,reflux of local anesthetic,chemosis, bleeding,and retained visual sensation[8,9].Major complications that can result from needle blocks include brainstem anaesthesia,retrobulber hemorrhage,globe penetration or perforation,optic nerve damage,damage to extraocular muscles and myotoxicity[8-16].
In our study,we compared the effects of the different doses of sub-Tenon's anaesthesia on IOP,akinesia and analgesia.IOP didn't reveal any significant change in both groups before and 10min after the block.However,akinesia and analgesia were significantly better in Group II(5 mL group).
Patton et al[17]showed in their study that the level of kinesia was greater in the 3 mL group compared to 5 mL group.In contrast to our findings,there was no significant difference in pain perception between two groups.Although there was great variation in IOP changes following sub-Tenon's anaesthetic, there was a trend for larger rise in mean IOP immediately after anaesthetic administration in 5 mL group compared to 3 mL group,but this didn't reach statistical significance.
In another prospective,randomised,controlled trial in which patients were randomly allocated to one of two groups.In group I,single injection of 5 mL of local anaesthetic was injected.In group II,3 mL of the same anaesthetic solution was injected followed by application of gentle orbital pressure for 2min.A further 2 mL of the same anaesthetic solution was injected through the same conjunctival incision.Measurement of movement in four quadrants of eye were done by the surgeon at 3 and 6min.IOP,chemosis,and subconjuctival haemorrhage were also measured.Single injection of local anaesthesia for sub-Tenon's block with mixture of lignocaine with adrenaline,bupivacaine and hyaluronidase was found to be superior to provide akinesia of ocular muscles compared to divided dose given by two injections.No difference in groups in terms of haemorrhage,chemosis,patient's satisfaction and IOP was found[18].
There are several studies comparing topical anaesthesia with sub-Tenon block for cataract surgery.Data indicate that more significant anaesthesia and analgesia was achieved with sub-Tenon's block,leading to more favorable surgical conditions and enhanced patient and surgeon satisfaction[19,20].
Along with the satisfaction of the surgeon with the akinesia providing superior operating conditions,the satisfaction of the patients mostly depend on the level of analgesia during the procedure.The pain that they will experience or they expect to suffer from is the only reality for the patients undergoing the surgery.Ensuring the high quality analgesia during the operation may limit clinicians' intention to decrease the dose of local anaesthetic and the volume of the drug for any reason.In our study,higher volume group had better pain relief and this result lead us to the question of“why should we decrease the volume if there is no difference between IOP but significant benefit with the akinesia and analgesia?”.
In conlusion,we suggest that sub-Tenon's anaesthesia either with 3 or 5 mL 2%lidocaine had no effects on IOP;however, analgesia and akinesia were preferably better in patients who received 5 mL lidocaine for the block during cataract surgery by phacoemulsification.Sub-Tenon's anaesthesia with 5 mL local anaesthetic provides good analgesia and operating conditions,while avoiding the passage of a sharp needle into the orbit.
REFERENCES
1 Guise P.Sub-Tenon's anaesthesia:an update.Local Reg Anaesth2012;5:35-46
2 Gayer S,Kumar CM.Ophthalmic regional anesthesia techniques.Minerva Anestesiol2008;74(1-2):23-33
3 Jaichandran V.Ophthalmic regional anaesthesia:A review and update.Indian J Anaesth2013;57(1):7-13
4 Villafranca Barba A,Mouslim S,De la Gala Garcia FA,Reyes Fierro A.Sub-tenon block for ocular globe anesthesia:a review.Rev Esp Anestesiol Reanim2011;58(3):167-173
5 Kumar CM,Williamson S,Manickam B.A review of sub-Tenon's block:current practice and recent development.Eur J Anaesth2005;22 (8):567-577
6 Kumar CM,Eid H,Dodds C.Sub-Tenon's anaesthesia:complications and their prevention.Eye(Lond)2011;25(6):694-703
7 Kumar CM.Orbital regional anesthesia:Complications and prevention.Indian J Ophthalmol2006;54(2):77-84
8 Shahid E,Juzar UT,Afaq A,Sherwani B,Sharif-ul-Hasan K. Anaesthesia in various anterior segment complications of sub-Tenon surgeries.J Pak Med Assoc 2013;63(5):548-551
9 Aranda Calleja MA,Martínez Pueyo A,Bellido Cuellar S,García Ruiz P.Ⅲcranial nerve palsy and brainstem disfunction following retrobulbar anaesthesia.Neurologia 2011;26(9):563-564
10 George RB,Hackett J.Bilateral hearing loss following a retrobulbar block.Can J Anaesth 2005;52(10):1054-1057
11 Kumar CM,Dowd TC.Complications of ophthalmic regional blocks: their treatment and prevention.Ophthalmologica 2006;220(2):73-82
12 Schrader WF,Schargus M,Schneider E,Josifova T.Risks and sequelae of scleral perforation during peribulbar or retrobulbar anesthesia.J Cataract Refract Surg2010;36(6):885-889
13 Kallio H,Rosenberg PH.Advances in ophthalmic regional anesthesia.Best Pract Res Clin Anesthesiol2005;19(2):215-227
14 Vinerovsky A,Rath EZ,Rehany U,Rumelt S.Central retinal artery occlusion after peribulber anaesthesia.J Cataract Refract Surg2004;30 (4):913-915
15 Gross A,Cestari DM.Optic neuropathy following retrobulbar injection:a review.Semin Ophthalmol2014;29(5-6):434-439
16 Guyton DL.Strabismus complications from local anesthetics.Semin Ophthalmol2008;23(5):298-301
17 Patton N,Malik TY,Aslam TM,Vallance JH.Effect of volume used in sub-Tenon's anaesthesia on efficacy and intraocular pressure:a randomized clinical trial of 3 mL versus 5mL.Clin and Experiment Ophthalmol2004;32(5):488-491
18 Khan EI,Mustafa J,McAdoo J,Shorten G.Efficacy of sub-Tenon's block using an equal volume of local anaesthetic administered either as a single or as divided doses.A randomised clinical trial.BMC Anesthesiol 2009;9:2
19 Rodrigues PA,Vale PJ,Cruz LM,Carvalho RP,Ribeiro IM,Martins JL.Topical anesthesia versus sub-Tenon block for cataract surgery: surgical conditions and patient satisfaction.Eur J Ophthalmol 2008;18 (3):356-360
20 Rüschen H,Celaschi D,Bunce C,Carr C.Randomised controlled trial of sub-Tenon's block versus topical anaesthesia for cataract surgery:a comparison of patient satisfaction.Br J Ophthalmol 2005;89(3):291-293
3mL和5mL利多卡因眼球筋膜囊下麻醉在超声乳化手术中的比较研究
Muge Coban-Karatas1,Oya Yalcin Cok2,Rana Altan-Yaycioglu1
(作者单位:1土耳其,亚达那01250,Baskent大学,医学院,眼科;2土耳其,亚达那01250,Baskent大学,医学院,麻醉科)
Muge Coban-Karatas.bkaratas99@hotmail.com
目的:分析比较3mL和5mL利多卡因眼球筋膜囊下麻醉对白内障超声乳化手术中眼压,镇痛效果和眼外肌失运动能力的作用效果。眼球筋膜囊下麻醉是白内障超声乳化术中常用的局麻方式。作为一种剂量依赖型的阻滞方式,良好的眼压、镇痛效果以及眼外肌失运动是手术成功需要考虑的重要因素。方法:在获得伦理批准和患者的知情同意后,随机纳入70例患者作为研究对象,分别给予3mL利多卡因(组一)和5mL利多卡因(组二)作眼球筋膜囊下麻醉。麻醉前测量眼压,麻醉后10min评估眼压,镇痛效果和眼外肌失运动能力,并记录球结膜水肿和结膜下出血等并发症。结果:在麻醉管理期间,由于两名患者要求镇静,故从本研究中排除。比较组内及组间患者在麻醉前、后的基本特征,如年龄、体质量、身高、眼轴长度以及ASA生理状态,均无明显差异。与组一相比,组二患者眼外肌失运动能力及镇痛效果均明显较好。组二中有13例患者(38.2%)可达到眼球完全不运动,而组一没有患者可达到该程度。组一中有18例患者(56.3%)术中完全无痛觉,14例患者(43.7%)存在轻微痛觉,组二中有28例患者(82.4%)无痛觉,6例患者(17.6%)术中有轻微痛觉。此外,两组患者在麻醉前与麻醉后10min,其眼压的变化均无统计学差异(P<0.05)。两组患者并发症发生情况无明显差异。结论:3mL利多卡因和5mL利多卡因作眼球筋膜囊下麻醉对眼压均无影响,但在白内障超声乳化手术中给予5mL利多卡因作麻醉,在镇痛及眼外肌失运动能方面效果更好。
眼球筋膜囊下麻醉;眼压;超声乳化;失运动能;痛觉
Muge Coban-Karatas.Department of Ophthalmology,Baskent University Faculty of Medicine, Adana Education and Research Center,Dadaloglu Mah.39 sk.No:6 Yüregir 01250 Adana,Turkey.bkaratas99@ hotmail.com
10.3980/j.issn.1672-5123.2015.11.03
:Coban-Karatas M,Cok OY,Altan-Yaycioglu R. Comparison of sub-Tenon's anaesthesia in phacoemulsification with 3 and 5 mL lidocaine.Guoji Yanke Zazhi(Int Eye Sci)2015;15(11): 1847-1850
引用:Coban-Karatas M,Cok OY,Altan-Yaycioglu R.3mL和5mL利多卡因眼球筋膜囊下麻醉在超声乳化手术中的比较研究.国际眼科杂志2015;15(11):1847-1850
·METHODS: After obtaining ethics approval andinformed consent of patients, 70 patients were randomlyenrolled to the study to receive sub - Tenon's block witheither 3 mL (Group I) or 5 mL (Group II) lidocaine. IOPwas measured before the block. IOP, analgesia andakinesia were evaluated at 10min after the block.Complications such as chemosis and subconjunctivalhemorrhage were also noted.
·RESULTS:Two patients were excluded from the studydue to the patients' request for sedation during blockadministration. Patients' characteristics such as age,weight, height, axial length, American Society ofAnesthesiology (ASA) physical status were comparablein - group before and after block measurement andbetween groups. Akinesia and analgesia weresignificantly better in Group II in comparison to Group I.“No eye movement” was obtained in 13 patients (38. 2% )in Group II whereas none of the patients had “ no eyemovement” in Group I. Eighteen (56. 3% ) patients had“no pain” and 14 (43. 7% ) patients had “mild pain” inGroup I whereas “No pain” in 28 patients (82. 4% ) and“mild pain” in 6 patients (17. 6% ) was observed in GroupII. On the other hand, IOP revealed no statisticallysignificant alteration in both groups before and 10minafter the block (P<0. 05). Complications were comparablebetween groups.
·CONCLUSION:Sub - Tenon's anaesthesia either with 3or 5 mL lidocaine had no effects on IOP; on the otherhand, analgesia and akinesia were preferably better inpatients who received 5 mL lidocaine for the block duringcataract surgery by phacoemulsification.
- 国际眼科杂志的其它文章
- LASEK for the correction of hyperopia with mitomycin C using SCHWIND AMARIS excimer laser:one-year follow-up
- Hospitalised ocular injuries in Osogbo,Nigeria
- Comparison of combined phacoemulsification-nonpenetrating deep sclerectomy and phacoemulsificationtrabeculectom y
- 豚鼠早期实验性近视眼视网膜色素上皮细胞bFGF表达变化的研究
- 小鼠眼眶成纤维细胞TLR4基因静默对甲状腺眼病的效应研究
- 小鼠视网膜电图随生长发育的变化特点