Neuroanatomy and clinicalanalysis of the cervicalsympathetic trunk and longus colli
Zhaoyang Yin,Jian Yin,Jun Cai,Tao Sui,Xiaojian Cao
Department of Orthopedics,The First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China.
Neuroanatomy and clinicalanalysis of the cervicalsympathetic trunk and longus colli
Zhaoyang Yin△,Jian Yin△,Jun Cai,Tao Sui✉,Xiaojian Cao✉
Department of Orthopedics,The First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China.
Anteriorcervicalsurgery is commonly used forcervicalvertebralbody lesions.However,the structure ofblood vessels and nerve tissues along the route of anterior cervicalsurgery is complex.We aimed to measure the data of the longus colli,the sympathetic trunk and the cervicalsympathetic trunk(CST)ganglia in Chinese cadaverspecimens.A totalof 32 adultcadavers were studied.We delineated the surgicalanatomy ofthe CST.The superiorand inferior/cervicothoracic ganglia ofthe sympathetic trunk consistently appeared.The middle ganglion was observed in 28.1%ofthe specimensand there were 2 casesofunilateraldouble middle cervicalganglia.The inferiorganglion was observed in 25.0%of the specimens and the cervicothoracic ganglion was observed in the remaining specimens.The distance between the CST gradually decreased from the top to the bottom,and the distance between the medialedges ofthe longus colligradually broadened from the top down.The average angle between the bilateral CST and the midline of the vertebra was 11.2°±1.8°on the leftside and 10.3°±1.4°on the rightside.The average angle between the medialmargins of longus colliof both sides was 11.1°±1.9°.The CST is athigh risk when LC muscle is cuttransversely oris dragged heavily,especially atthe levels of C6 and C7.Awareness of the regionalanatomy of the CST could help surgeons to identify and preserve itduring anterior cervicalsurgeries.
cervicalsympathetic trunk,ganglion,Horner syndrome,longus colli,spinalsurgery
Introduction
Discectomy from the anterior cervical spine and interbody bone graft fusion was first reported by Robinson and Smith[1],which provided an effective surgical procedure for cervical and intervertebral disc disease.Since then,various methods forimproved surgery have been advanced.Anteriorcervicalsurgery for the treatmentofcervicalvertebralbody lesions,including tumor infection and trauma,has become very common.However,the structure of blood vessels and the nerve tissue along the route ofanteriorcervicalsurgery is complex,which increases surgical difficulty and risk.Sympathetic nerve injury,a complication of the surgery,has been studied[2-3].In our work,we also found postoperative symptoms of injury to the sympathetic trunk.Bertalanffy and Eggert reported that the incidence of Horner's syndrome was 1.1%in a cohort of 450 cases undergoing anterior cervical surgery[4], which is similar to that reported by Cuatico and Dohn[5-6],but lower than that reported(4%)by Bruneau etal.[7].Research into the cervicalsympathetictrunk(CST)was also reported[8-9],butthere have been no systemic anatomical studies of the sympathetic trunk and surrounding structures in Chinese subjects. This study aimed to measure the data of the longus colli(LC),sympathetic trunk and CST ganglia in Chinese subjects and to become more familiar with their anatomical characteristics,thereby providing a basis for avoiding injury in surgery.
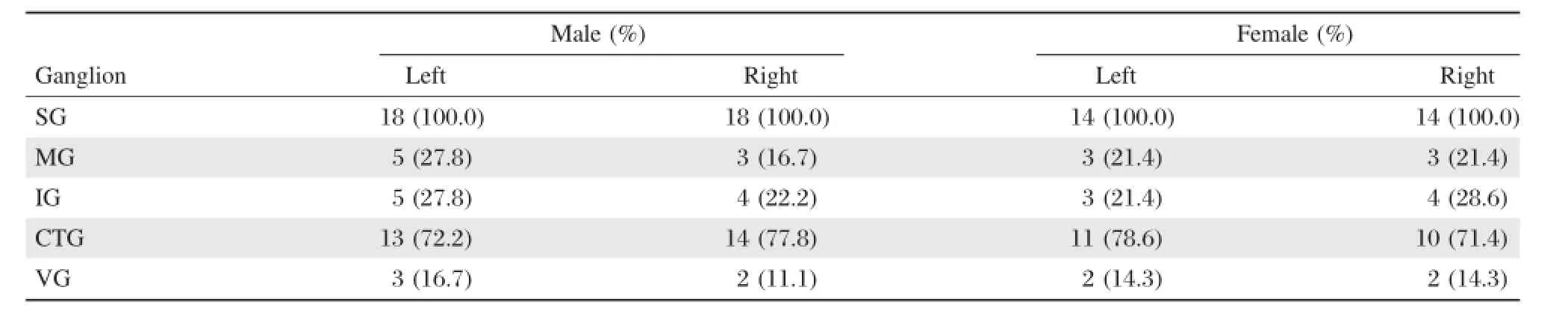
Table 1 The number of ganglia on the right and left side in men and women
Materials and methods
Cadavers
In our study,32 adult cadavers(18 men and 14 women)with a mean age of56 years old(ranged from 27 to 78 years)were obtained from the Departmentof Anatomy ofthe authors'affiliated institution.They were placed in the supine position and theirnecks in loose extension.Anterior skin and softtissues of the neck and platysma muscles were removed.Afterthe omohyoid muscle was transected,and the sternocleidomastoid muscle and the carotid sheath were retracted,the LC and the sympathetic trunk beneath the prevertebral fascia were exposed.Research was performed on the courseofthecervicalLCon both sidesofand on the sympathetic trunk,as wellas its corresponding relationship with thevertebralbody.Thestudy protocolwasapproved by the localinstitutionalreview board atthe authors' affiliated institution and the study was carried outin accordance with the institutionaland state guidelines regarding use ofhuman cadavers.
Measurements
Measurements were obtained,including the dimensions of the superior cervical ganglion,the middle cervicalganglion,the inferiorcervical/cervicothoracic ganglion and thevertebralganglion,thedistancebetween the ganglia,the medialpartofthe LC on both sides,the cervicaland thoracic vertebralanteriormidline,CST and cervicalspine anteriormidline,the angle between CST and cervicalspine longitudinalaxis,and the angle between the medialpartsofthe LC.The protractorused forangle measurementwas sensitive to 1°,and the verniercalipersused forlength measurementsweresensitive to 0.1 mm.We examined the measurementdata of both sidesusing a testand analysisofvariance,respectively.Statistical analysis
Data was expressed as x±s.Statisticalanalysis of distance between the two sides was performed using Student's t test,and the number of the ganglions between men and women was examined using x2test. P<0.05 was considered as significant.
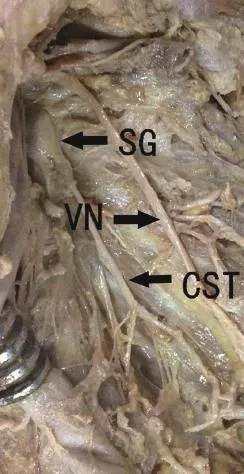
Fig.1 The position and adjacent tissue of the superior ganglion.SG:superior ganglion;CST:cervical sym-pathetic trunk; VN:nervi vagus.
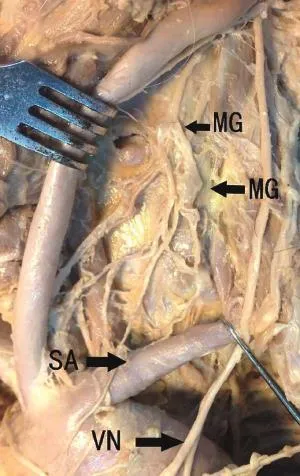
Fig.2The double middle cervical ganglia are observed.MG: middle ganglion;SA:subclavian artery;VN:nervi vagus.
Results
The CST,which is located on both sides of the cervical spine and is covered by the prevertebralfascia, was composed of the superior cervical ganglion,the middle cervical ganglion,the inferior cervical/cervicothoracic ganglion,the vertebral ganglion,and the internode branch.We observed thatthe superiorcervical ganglion appeared in allcadavers,the middle cervical ganglion and inferior cervical/cervicoth oracic ganglion were asymmetrically absent in some cadavers,and the middle cervical ganglion appeared on the leftside in 8(25%)cases and on the right side in 6(18.8%)cases of 32 specimens at different times. The cervicothoracic ganglion or stellate ganglion, which is combined with cervicalganglion and the first thoracic ganglion,consistently appeared on both sides (with 8 cases on the left side and 8 cases of 32 specimens on the leftside)in the absence ofthe inferiorcervicalganglion atdifferenttimes.The appearance rate ofa vertebralganglion was nothigh.A vertebralganglion appeared asymmetrically on the left side in 5(15.6%)cases and on the right side in 4(12.5%) cases of 32 specimens(Table 1).
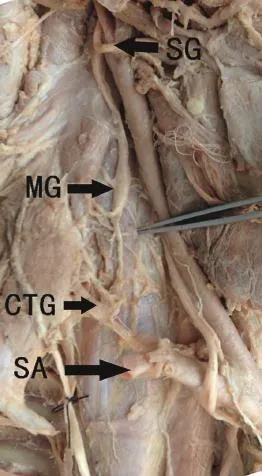
Fig.3 The position and adjacent tissue of the sympathetic trunk.SG:superior ganglion;MG:middle ganglion;CTG: cervicothoracic ganglion;SA:subclavian artery.
Superior cervical ganglion
The superiorcervicalganglion was detected in all32 specimens on both sides,in the frontof the transverse process at C2-C3.The average length of the superior cervical ganglion was 31.9±5.3 mm and 32.2±5.0 mm on the left and rightside,respectively.The average width was 7.0±1.2 mm and 7.2±1.1 mm on the leftand rightside,respectively.The average thickness was 2.7±0.3 mm and 2.7±0.3 mm on the left and rightside,respectively.No significantdifferences were found between the left and right side(P>0.05) (Fig.1).
Middle cervical ganglion
We observed that the middle cervicalganglion was on the leftin 8 casesand on the rightin 6 cases,among which 5 cases ofbilateralsymmetry appeared(Fig.2). The middle cervicalganglion was located in the front of C6 transverse process;the average length was 6.6±1.5 mm and 6.3±1.5 mm on the leftand right side,respectively.The average width was 3.9±0.8 mm and 3.8±0.8 mm on the leftand rightside,respectively.The average thickness was 2.0±0.5 mm and1.7±0.3 mm on the left and right side,respectively. No significantdifferences were found between the left and rightside(P>0.05)(Fig.3).
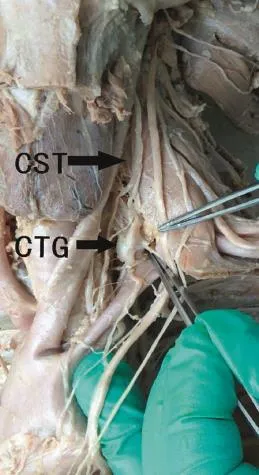
Fig.4 The position and adjacent tissue of the sympathetic trunk.CTG:cervicothoracic ganglion;CST:cervicalsympathetic trunk.
Inferior cervical ganglion
The inferior cervical ganglion,which is located in C7 transverse process forward,was found in 8 cadavers on the leftside and in 8 cadavers on the rightside. There were 7 cases ofbilateralsymmetry.The average length of the inferior cervical ganglion was 8.6±1.6 mm and 8.2±1.5 mm on the leftand rightside,respectively.The average width was 4.5±0.6 mm and 4.4±0.5 mm on the left and right side,respectively. The average thic k ness wa s 4.4±0.5 mm and 3.9±0.3 mm on the left and right side,respectively. No significant differences were found between the left and right side(P>0.05).
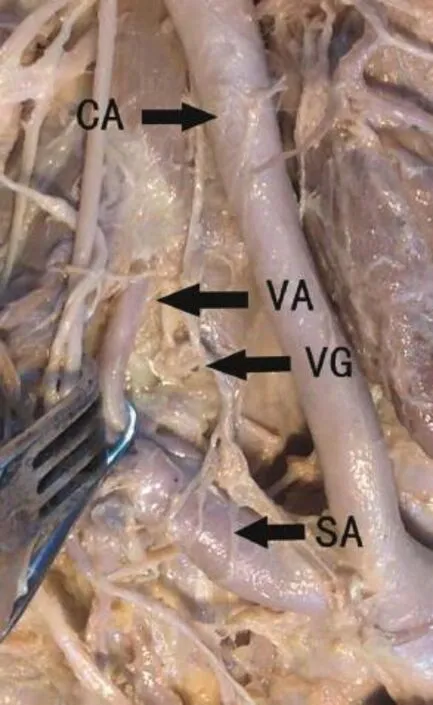
Fig.5 The position and adjacent tissue of the vertebral ganglion.VG:vertebral ganglion;CA:cephalic artery;VA:vertebral artery;SA:subclavian artery.
Cervicothoracic ganglion
The cervicothoracic ganglion,which lies in frontof the first rib neck,was detected on the left side in 32 specimens of 24 cases,and in 24 cases,itwas located on the right side,but there was no symmetry.There were 23 cases of bilateral symmetry.The averagelength of the cervicothoracic ganglion was 18.7±2.0 mm and 18.9±1.6 mm on the left and right side, respectively.The average width was 7.0±1.0 mm and 6.7±0.9 mm on the left and right side,respectively.The average thickness was 2.5±0.4 mm and 2.3±0.3 mm on the leftand right side,respectively. No significantdifferences were found between the left and rightside(P>0.05)(Fig.4).
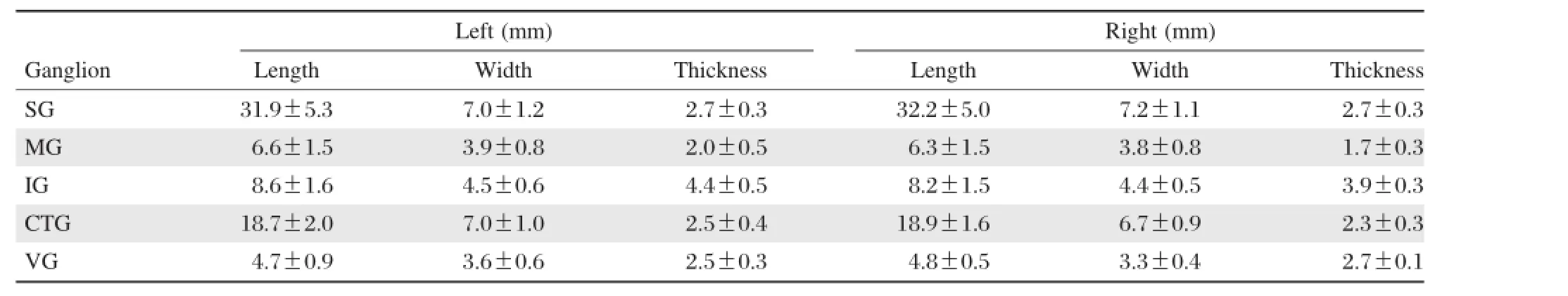
Table 2 The sizes of ganglia
Vertebral ganglion
Bilaterally symmetrical vertebral ganglia were detected in 4 casesof32 specimens,and 1 case wasunilateral(Fig.5).The average length of the vertebral ganglion was4.7±0.9 mm and 4.8±0.5 mm on the left and rightside,respectively.The average width was 3.6±0.6 mm and 3.3±0.4 mm on the leftand right side,respectively.The average thickness was 2.5±0.3 mm and 2.7±0.1 mm on the leftand rightside,respectively.No significantdifferences were found between the leftand rightside(P>0.05)(Table 2).
Distance among the superior,middle,and inferior cervical ganglia
Distance between the superior and middle cervical ganglia on the same side corresponded to the lower edge of the superior cervical ganglion and the upper edge of the midd le cervical gang lion.Distance between the middle cervical ganglion and inferior cervical/cervicothoracic ganglion on the ipsilateral side corresponded to the lower edge of the middle cervical ganglion and upper edge of the inferior cervical/cervicothoracic ganglion.Distance between the superior cervicalganglion and the cervical/cervicothoracic ganglion on the ipsilateralside corresponded to the loweredge ofthe superiorcervicalganglion and upperedge ofthe cervical/cervicothoracic ganglion.In ourstudy,there were 2 cases ofdouble middle cervical ganglia.Distance between the superior and middle cervicalganglia corresponded to the lower edge ofthe superior cervical ganglion and upper edge of the double middle cervical ganglion.Distance between the middle double cervicalganglion and inferiorcervical/cervicothoracic ganglion on the ipsilateral side corresponded to the lower edge of the double middle cervicalganglion and upperedge of the inferior cervical/cervicothoracic ganglion.On the leftside,the average distance between the superiorand middle ganglia was 44.2±4.9 mm,while on the rightside,the average was46.8±4.6 mm,and no significantdifferences were found between the leftand right side.The mean distance on the leftside between the middle cervicalganglion and inferiorcervical/cervicothoracic ganglion was 18.9±2.9 mm,and on the right side,18.0±1.5 mm, and no significant differences were found between the left and rightside.The average distance on the left side between the superior cervical ganglion and cervical/cervicothoracic ganglion was 71.5±6.0 mm, and on the rightside,73.1±5.3 mm,and no significant differences were found between the leftand rightside (Table 3).
Sympathetic trunk
The average angle between CST and midline ofthe vertebralbody on the leftand rightside was 11.2°± 1.8°and 10.3°±1.4°,respectively.No significantdifferences were found between the left and rightsides (P>0.05).The average distance between the medial margin of CST and midline of the vertebralbody on the leftside was 26.7±2.6 mm at C3,25.5±2.3 mm at C4,24.1±2.1 mm at C5,22.5±1.9 mm at C6 and 20.8±1.6 mm at C7;on the rightside,itwas 26.5± 2.7 mm at C3,25.0±2.4 mm at C4,23.5±2.0 mm at C5,22.1±1.8 mm atC6 and 20.4±1.5 mm atC7.
In addition,22 cases of 32 cadavers(68.8%)had white tendon tissues under the thoracic spine,and 10 cases of 32 cadavers(31.2%)had muscle tissues or a mixture of muscle and tendon tissues to inside of the anterior longitudinalligament.
The LC from the cephalic end to caudalend has a tendency to converge.The average angle between the medialmargins of LC on both sides was 11.1°±1.9°. Distance between the medial margin of LC and the anterior midline of the cervicothoracic spine from the top to the bottom gradually broadened.The average distance on the leftwas 4.0±0.6 mm atC3,4.8±0.8 mm at C4,5.9±0.9 mm at C5,6.9±0.9 mm at C6,7.8±0.8 mm at C7,8.9±0.9 mm at T1 and 10.5±1.3 mm at T2;and on the right,itwas 4.1±0.6 mm at C3, 5.0±0.7 mm at C4,6.0±0.7 mm at C5,7.1±0.8 mm at C6,8.0±0.8 mm at C7,9.2±1.0 mm at T1, 10.6±1.2 mm at T2(Table 4).
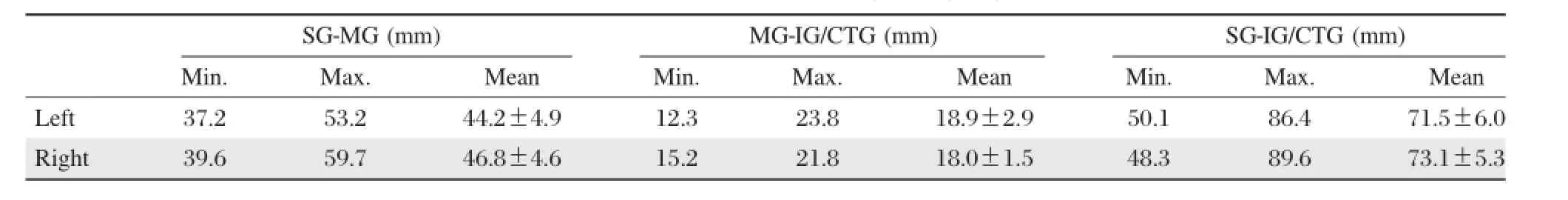
Table 3 The distances among the ganglia
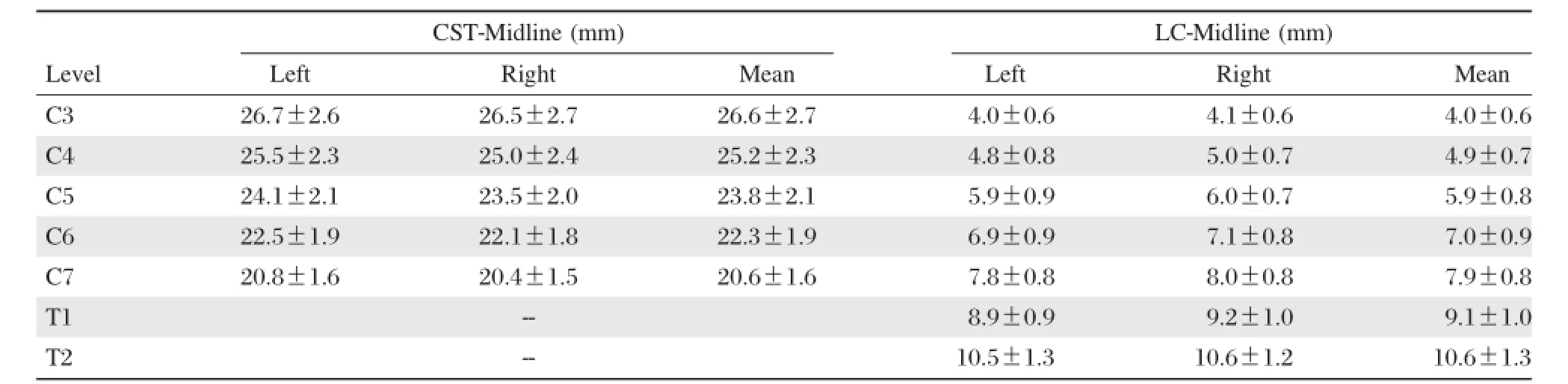
Table4 The distances between the CST and the midline and the distances between the LC and the midline at the level of the vertebrae
Discussion
Horner's syndrome was first reported in 1929 by Swiss ophthalmologist Johann-Friedirch-Horne.The diagnostic criteria of the World Health Organization are listed as follows:decreased vision,miosis,endophthalmos,no sweat,and vascular dilatation at the lesion site[10].Horner's syndrome can occur after CST injury. Diagnosis can be made according to clinical signs and laboratory results.
Under normal circumstances,CST contains 3-4 ganglia,including the superior,middle(double),inferior cervical/cervicothoracic and vertebral ganglia.In the 32 specimens in our study,the inferior and cervical/cervicothoracic ganglia consistently appeared,and their locations were relatively fixed in general. The lower rate of the middle cervical ganglion was approximately 28.1%.Two of the specimens had unilateral appearance of two cervical middle ganglia. Our study showed that the superior ganglion was the largest ganglion of the sympathetic trunk.The length and width of the superior ganglion were 12.5±1.5 and 5.3±0.6 mm,respectively,which was located at the C4 vertebrallevelin the study of Civelek etal.[11]. However,in our study,the length and width of the superior ganglion were 32.1±5.1 and 7.1±1.2 mm, respectively,which was located atthe C2-3 vertebral level.Tubbs etal.indicated thatthe superior ganglion was approximately located at the C2-3 vertebral level and in the rear of the internalcarotid artery[12],which is consistentwith our study.This disagreementmight depend on if the specimens were soaked in formalin, as wellas the soaking time.However,the likelihood ofinjury to the superiorganglia ofthe sympathetic trunk is very small.The anterior tubercle of the transverse process of the lower cervicalspine at C6 is an important anatomicallandmark.Our study found thatthe middle cervicalganglion was mostly in C6 transverse process level,and in 28%ofthe specimens,we observed 2 cases of double ganglia.The length and width of the middle ganglion were 6.5±1.5 and 3.9±0.8 mm,respectively. In some samples,in the absence ofthe middle ganglion, the diameter of the CST was 2.5±0.3 mm on the left side,and 2.3±0.3 mm on the rightside.Our measurements corresponded to those in Kray et al.'s report[8], in which the diameter of the CST was 2.2±0.7 mm. The inferior cervical ganglion and the first thoracic ganglion fused into the cervicothoracic ganglion in most cases.If the inferior ganglion appeared,itwas close to the first thoracic ganglion,and the distance was 5.5±1.6 mm on the left side,and 5.1±1.0 mm on the rightside.The two ganglia sometimes intertwined. Moststudies have indicated that the CST runs along the prevertebralfascia posteriorly and along LC anteriorly.However,Lyons et al.found that in 16.7%of the specimens,the CST ran along the posterior wallof the carotid sheath,which indicated the possibility of damaging the sympathetic trunk by stretching the carotid sheath during anteriorcervicalsurgery[13].The anatomical characteristics are very important for surgery of the lower cervical or anterior cervical thoracic spine. Surgeons should avoid excessive stretching of the carotid sheath during surgery.
The LC is made of muscle and tendon tissues and is located in frontofthecervicaland upperthoracicvertebral body,including externaland internalparts.The external partbegins atthe C3-6 transverse process and stops at the anteriortubercle ofthe atlas.The internalpartbegins atthe C5-7 and T1-3 vertebralbodies and stops atthe anteriortubercleoftransverseprocessatT2-4 and C5-7,which is similarto Lu etal.'sreports[14-15].
The distance between the medialedge of LC and the anterior midline of the lower cervical spine gradually broadened from the top down.The nearest point of the sympathetic trunk on both sides was located at the C6-7 level;therefore,surgeons should keep deviating from the centerline as far as possible during surgery and minimize the stripping of LC,especially at the C6-7 level.LC is formed by muscle and tendon tissues, and the demarcation pointis located atthe cervicothoracic junction.In front of the lower cervical spine were mostly muscle tissues,and in frontofthe thoracic spine were mostly tendon tissues.This pointcould be used as a marker for intraoperative positioning.
CST injury is mostly caused by excessive exposure ofthe outersurface ofthe bone in frontofthe lowercervical vertebralbody,the hook vertebraljointor the transverse foramen,cutting off the CST in operation or stripping or excessively stretching the LC.Among the reasons above,exposure ofthe cervicalanteriorlateralpart or the transverse foramen and consequent excessive stretching ofthe LCwere the main reason that the CST was injured.Lu etal.indicated thatany injury of the CST in frontof the lower cervicalspine could cause Horner syndrome.Therefore,during anterior lowercervicaloperations,hooks should notbe placed above the LC,and there isno need to expose the sympathetic trunk;a little blunt dissection below the inner edge of the LC,placing the retractor under the LC and pulling carefully for the sake of avoiding sympathetic trunk injury,issufficient.Sometimes,the position of the middle cervicalganglion mustbe identified during surgery.However,in ourstudy,the middle cervical ganglion was absentin some samples.Identifying the stellate ganglion was important in such cases.This ganglion is consistently and generally located in front ofthe firstrib neck.Understanding ofthese anatomical featuresishelpfulforavoiding injury to the sympathetic trunk.
In conclusion,Horner's syndrome in cervicothoracic spine anterior surgicalcomplications is notrare,causing some adverse effects in patients.The distance between the medial margin of the CST and midline of the vertebral body is nearest at the levels of C6 and C7,and the CST is athigh risk when LC muscle is cuttransversely orisdragged heavily,especially during operation ofexposing the outersurface ofthe bone in frontof the lower cervicalvertebralbody,the hook vertebral joint or the transverse foramen.Familiarity with the anatomical characteristics of the LC and CST could contribute to identifying the sympathetic trunk correctly during surgery and reducing the occurrence of surgicalcomplications.
Acknowledgements
This work was supported by National Natural Science Foundation of China(Grant 81171694, 81371968,81401791),and a project funded by the Priority Academic Program Development of Jiangsu Higher Education institution.The cadavers used in our study were provided by the Department of Anatomy, Nanjing Medical University.We gratefully acknowledge the supportand assistance from allthe teachers of the Departmentof Anatomy.
[1]Robinson RA,Smith GW.Anterolateral cervical disc remo v al an d interb o dy fusio n for cerv ical d isc syndrome[J].Bull Johns Hopkins Med Soc,1955,96(1): 223-224.
[2]An HS,Vaccaro A,Cotler JM.Spinaldisorders atthe cervicothoracic junction[J].Spine,1994,19(22):2557-2564.
[3]Johnston FG,Crockard A.One-stage internalfixation and anterior fusion in complex cervical spinal disorders[J]. J Neurosurg,1995,82(2):234-238.
[4]Bertalanffy H,Eggert HR.Complications of anterior cervical discectomy without fusion in 450 consecutive patients[J].Acta Neurochir(Wien),1989,99(1-2):41-50.
[5]Cuatico W.Anterior cervical discectomy without interbody fusion:an analysis of 81 cases[J].Acta Neurochir (Wien),1981,57(3-4):269-274.
[6]Dohn DF.Anterior interbody fusion for treatment of cervical disc conditions[J].JAMA,1966,197(11):897-900.
[7]Bruneau M,Cornelius JF,George B.Microsurgicalcervical n erv e ro o t d eco mp ressio n b y an tero lateral approach[J].Neurosurgery,2006,58(1 Suppl):ONS108-ONS113.
[8]Kiray A,Arman C,Naderi S,et al.Surgical Anatomy of the Cervical Sympathetic Trunk[J].Clin Anat,2005,18(3): 179-185.
[9]Saylam CY,Ozgiray E,Orhan M,etal.Neuroanatomy of Cervical Sympathetic Trunk:A Candaveic Study[J].Clin Anat,2009,22(3):324-330.
[10]Wlaton KA,Buono LM.Horner syndrome[J].Curr Opin Ophthalmol,2003,14(6):357.
[11]Civelek E,Karasu A,Cansever T,etal.Surgicalanatomy of the cervical sympathetic trunk during anterolateral approach to cervical spine[J].Eur Spine J,2008,17(8): 991-995.
[12]Tubbs RS,Salter EG,Oakes WJ.Anatomic landmarks for nerves of the neck:a Vade Mecum for neurosurgeons[J]. Oper Neurosurg,2005,2(56):256-260.
[13]Lyons AJ,Mills CC.Anatomical variants of the cervical sy mpath etic ch ain to b e co n sidered durin g neck dissection[J].Br J Oral Maxillofac Surg,1998,36(3): 180-182.
[14]Golffinos JG,Dickman CA.Repair of vertebralartery during anterior cervical decompression[J].J Spine,1994, 19(22):2552-2556.
[15]Lu J,Ebraheim NA,Nadim Y,et al.Anterior approach to the cervical spine:Surgical anatomy[J].Orthopedics, 2000,23(8):841-845.
△Zhaoyang Yin and Jian Yin contributed equally to this work.
✉Corresponding author:Dr.Xiaojian Cao,Department of Orthopedics, the First Affiliated Hospital of Nanjing Medical University,Nanjing, Jiangsu 210029,China.Tel:+86-013002505801,E-mail:xiaojiancao001@ 163.com;Dr.Tao Sui,Department of Orthopedics,the First Affiliated Hospital of Nanjing Medical University,Nanjing,Jiangsu 210029,China.Tel:+86-013913833209,E-mail:nydsuitao@163.com.
Received 13 March 2015,Revised 01 July 2015,Accepted 09 September 2015,Epub 30 October2015
R323.1,Document code:A
The authors reported no conflict of interests.
©2015 by the Journal of Biomedical Research.All rights reserved.
10.7555/JBR.29.20150047
 THE JOURNAL OF BIOMEDICAL RESEARCH2015年6期
THE JOURNAL OF BIOMEDICAL RESEARCH2015年6期
- THE JOURNAL OF BIOMEDICAL RESEARCH的其它文章
- The evolving concept of physiologicalischemia training vs. ischemia preconditioning
- PCSK9 and triglyceride-rich lipoprotein metabolism
- Generation of monoclonalantibodies against n-3 fatty acid desaturase
- Dominant-negative inhibition of glucose-dependent insulinotropic polypeptide impairs function ofβcells in transgenic pigs
- Waldenstrom′s macroglobulinemia associated with Hodgkin′s lymphoma: a case report
- A susceptibility locus rs7099208 is associated with non-obstructive azoospermia via reduction in the expression of FAM160B1
