三阴乳腺癌与基底细胞样乳腺癌病理形态和生物学特征探讨
王成鑫,黄萱,封华
(江大病理诊断所;江汉大学医学院病理学与病理生理学教研室,湖北武汉430056)
李培林
(加州大学旧金山分校医学院医学系,旧金山CA94121)
三阴乳腺癌与基底细胞样乳腺癌病理形态和生物学特征探讨
王成鑫,黄萱,封华
(江大病理诊断所;江汉大学医学院病理学与病理生理学教研室,湖北武汉430056)
目的探讨三阴乳腺癌(triple-negative breast cancer,TNBC)与基底细胞样乳腺癌(basal-like breast cancer,BLBC)及非三阴乳腺癌(non triple-negative breast cancer,NTNBC)的关系及其形态、生物学特征。方法应用免疫组织化学(immunohistochemistry,IHC)方法对96例乳腺癌标本进行HER2、ER、PR蛋白的检查;应用FISH(fluorescent in situ hybridization)方法对3例HER2 IHC 3+及5例HER2 IHC 2+标本进行HER2基因扩增的检查;对22例TNBC进行了CK5/6或EGFR的检查。按照检查结果,将其分为TNBC、NTN⁃BC和BLBC,比较三者的病理形态及生物学特征。结果NTNBC占72.92%(70/96),其组织学Ⅰ、Ⅱ及Ⅲ级的病例分别为28.57%(20/70)、57.14%(40/70)和14.29%(10/70),淋巴结转移率为44.44%(16/36);TN⁃BC占乳腺癌的27.08%(26/96),无组织学Ⅰ级病例,组织学Ⅱ及Ⅲ级的病例分别为53.85%,(14/26)及46.15%,(12/26)例,淋巴结转移率为61.11%(11/18);BLBC占TNBC的63.64%(14/22),同TNBC一样,无组织学Ⅰ级病例,Ⅱ、Ⅲ级的病例分别为57.14%(8/14)及42.86%(6/14),淋巴结转移率为55.56%(5/9)。TN⁃BC与BLBC低分化病例的比例以及淋巴结的转移率均高于NTNBC。3例HER2 IHC 3+的病例FISH检查结果同IHC,5例HER 2 IHC 2+标本FISH检查1例基因扩增,3例阴性,1例结果不确定。结论TNBC与BLBC占乳腺癌1/4的比例,组织学多为中、低分化,浸润性生长,易发生淋巴结转移和复发,临床预后较差。虽然BLBC与TNBC大部分有重叠,但其具有独自的特异性,应成为独立的组织病理学类型。CK5/6或EGFR可用作从TNBC中筛选BLBC的指标。IHC 2+病例要做FISH检查,以正确指导治疗。
三阴乳腺癌;基底细胞样乳腺癌;病理形态学;荧光原位杂交
乳腺癌是异质性明显的恶性肿瘤,为女性最常见的恶性肿瘤之一,占女性死因的首位。在传统分类上,将乳腺癌分为激素受体(ER和/或PR)阳性或阴性肿瘤[1-2]。近年来,根据基因表达谱及基因分型,将乳腺癌分为4种亚型[2-3]:①基底细胞样型(basal-like subtype,ER、PR、HER2均阴性);②HER2高表达型(ER、PR、阴性,HER2阳性);③管腔型(1uminal subtype),此型又按照有无HER2的过表达分为:Luminal A(ER和/或PR阳性,HER2阴性);④Luminal B(ER和/或PR阳性,HER2阳性)。也有分为5型及其他亚型的[1,4],即多一型正常乳腺样肿瘤(Normal breast-like)。管腔型以ER及其相关基因高表达为特征,预后较好;基底细胞样型乳腺癌(BLBC)是指具有基底细胞基因表型并不同程度地表达基底细胞角蛋白和肌上皮标记物的乳腺癌,占全部乳腺癌的15%,与早已发现的免疫组化三联阴乳腺癌(TNBC)在免疫表型及临床预后等方面存在相似之处,特别是在组织学上多为高级别肿瘤。更因为BLBC占TNBC的85%[5],有人将BLBC与TNBC相提并论,并视为完全相同的乳腺癌亚型[6],但目前诸多研究显示,BLBC与TNBC是不同范畴的两类乳腺癌[2,5,7],BLBC与TNBC两型之间至少有30%以上存在不一致性,基因分型、免疫表型及组织学类型也不能完全对应。
TNBC指雌激素受体(ER)、孕激素受体(PR)和HER2均无表达的乳腺癌,被认为是一个单独的组织学类型,占全部乳腺癌的10%~17%,其中任何一项阳性者即定义为NTNBC[8-11]。本研究目的在于分析TNBC、BLBC及NTNBC间的关系及其病理形态特点及生物学特征。
1 资料和方法
1.1 临床资料
选取2008年1月至2012年12月间江大病理诊断所收检的乳腺癌手术标本96例,进行临床病理资料分析,包括年龄、淋巴结转移、病理类型、组织学分级等。所有患者均为女性,年龄23~86岁,平均年龄51.12岁。
1.2 病理资料
所有标本均为浸润性乳腺癌,90%以上为浸润性导管癌,少数为黏液癌、小叶癌及混合性乳腺癌。按照癌组织的分化程度的不同,将其分为三级:GⅠ、GⅡ、GⅢ。有淋巴结清扫的病例,每例检查淋巴结均在12枚以上。
1.3 方法与试剂
标本经40 g/L缓冲甲醛固定,常规石蜡包埋切片,切片厚3~4 μm,分别作常规HE及应用免疫组织化学S-P法检查HER2、ER、PR蛋白在乳腺癌组织中的表达,对22例TNBC进行了CK5/6或EGFR的检查,二者中任意一项阳性即为BLBC。应用FISH方法对3例HER2 IHC 3+及5例IHC 2+HER2标本进行HER2基因扩增的检查。试剂购自福州迈新公司(产品编号:ER:MAB-0349;PR:MAB-0236;C-erbB-2(HER2):MAB-0198;CK5/6:MAB-0276、EGFR:RMA-0554;HER2双色探针试剂盒:Z2020-5)。染色步骤按试剂盒说明进行。已知阳性组织切片作阳性对照,PBS液代替一抗作阴性对照。
1.4 IHC及FISH结果判定
HER2免疫组织化学及FISH检测结果判定按照ASCO/CAP指南[7]推荐标准判定;ER、PR结果判定:采用文献[12]介绍的评分方法,即将肿瘤细胞核着色数量、着色程度分别评分,两者相加,3分及以上为阳性。根据IHC及FISH检查结果,将其分为3组:TNBC、NTNBC和BLBC组。TNBC最大年龄85岁,最小年龄23岁,平均年龄48.32岁;NTNBC最大年龄86岁,最小年龄26岁,平均年龄52.68岁;BLBC最大年龄77岁,最小年龄39岁,平均年龄51.5岁。
1.5 统计学方法
应用SPSS 13.0软件进行统计学处理,比较用非参数检验。P<0.05为差异有统计学意义。
2 结果
2.1 组织形态学
在TNBC中非特殊型导管癌占了绝大部分,多为浸润性导管癌Ⅱ~Ⅲ级,少数为黏液及化生性癌。它们与NTNBC不同的形态学特点为:较低的组织学分级,无Ⅰ级病变,细胞具有明显的多形性,高的核浆比、较少腺管样结构、核分裂多见(图1,见封三),细胞凋亡现象明显,间质稀少以及推挤性边缘和中央地图样坏死(图2,见封三)或粉刺样坏死等,有时还可见梭形细胞及鳞状分化(图3,见封三),有中央区微血管增生和炎性细胞浸润。
2.2 ER、PR、HER2蛋白、CK5/6和EGFR及HER2基因的表达
ER、PR、HER2蛋白表达的情况如表1所示,96例患者中,ER:58例阳性;PR:41例阳性;HER2:31例阳性。TNBC 26例,占全部乳腺癌的27.08%(26/96),NTNBC 70例,占72.92%(70/96)。CK5/6和EGFR表达见图4(见封三)和图5(见封三)FISH结果:3例HER2 IHC 3+的病例有基因扩增(图6,见封三);5例HER2 IHC2+标本2例基因扩增,其中1例为导管内癌扩增,无实际意义,2例阴性(图7,见封三),1例结果不确定。22例TNBC中,14例CK5/6或EGFR阳性表达,为BLBC,占TNBC的63.64%(14/22),低于文献[5]中占85%的报道。
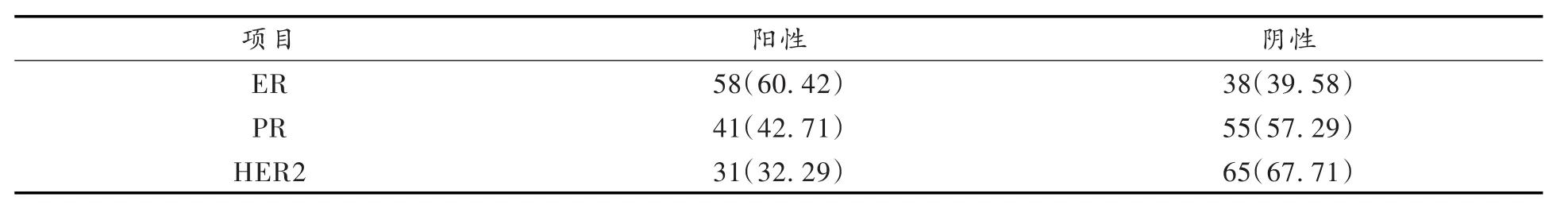
表1 ER、PR、HER-2蛋白表达的情况/例(%)Tab.1 Expression of ER,PR and HER2 in breast cancer
2.3 各组乳腺癌组织学分级及淋巴结转移率
乳腺癌组织学分级及淋巴结转移率如表2和表3所示,TNBC(包括BLBC)无组织学Ⅰ级病例,Ⅱ~Ⅲ级的病例分别为53.85%(14/26)及46.15%(12/26),本组有完整淋巴结资料的病例18例,11例有淋巴结转移,转移率为61.11%;NTNBC组70例,组织学Ⅰ、Ⅱ及Ⅲ级的病例分别为28.57%(20/70)、57.14%(40/70)和14.29%(10/70),有完整淋巴结资料的病例36例,16例有淋巴结转移,转移率为44.44%(16/36)。TNBC组织学高级别的比例远高于非三阴型组,差异有显著的统计学意义(P<0.001),淋巴结转移率三阴型组61.11%也高于非三阴型组的44.44%;BLBC组Ⅱ~Ⅲ级的病例分别为57.14%(8/14)及42.86%(6/14),本组有完整淋巴结检查资料的病例9例,5例有淋巴结转移,转移率为55.56%(5/9),同TNBC相比,在组织学分级上差别不大,淋巴结转移率高于NTNBC,而低于TNBC,可能和标本基数太少有关。
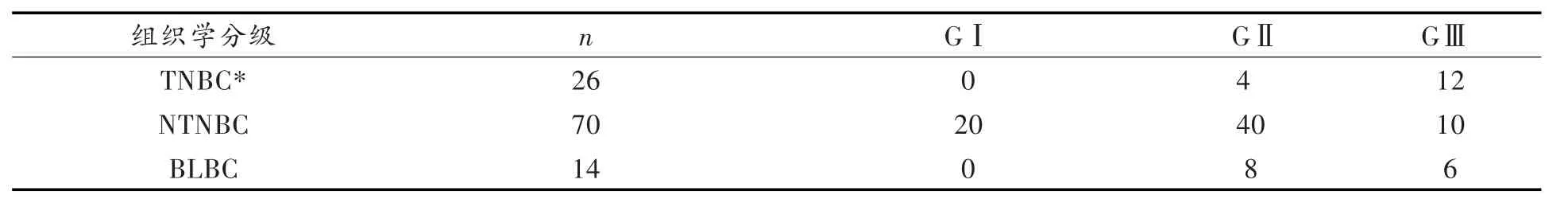
表2 三阴与非三阴型乳腺癌组织学分级/例Tab.2 Histological grade of triple-negative and non-triple-negative breast cancer
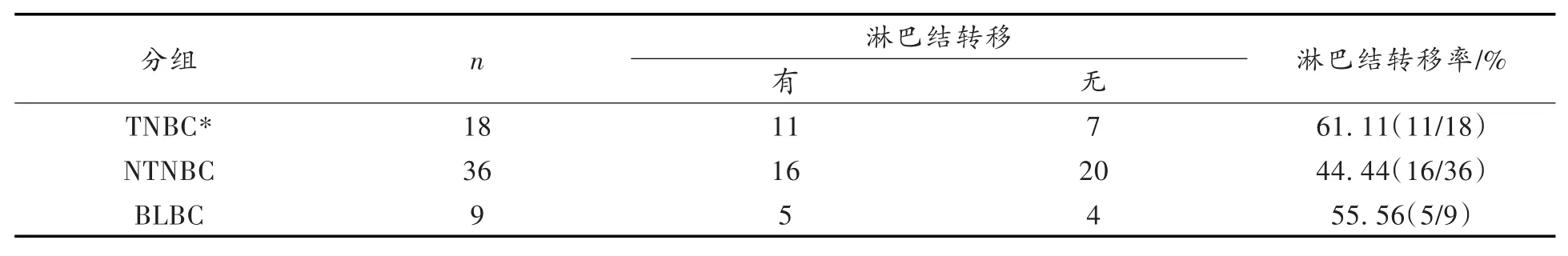
表3 三阴与非三阴型乳腺癌淋巴结转移率/例Tab.3 Rate of lymph node metastasis of triple-negative and non-triple-negative breast cancer
3 讨论
TNBC是早已广泛认识、具有特殊免疫表型的一类乳腺癌。激素受体阳性者往往对内分泌治疗有效,而具有HER2基因过表达的患者则对靶向治疗敏感,因此目前对乳腺癌患者常规进行激素受体和HER2基因表达的检测。TNBC则不适用于内分泌治疗及靶向治疗。TNBC占乳腺癌的10%~17%[2,9-11],但也有TNBC占乳腺癌比例较高的报道。袁中玉等[11]的研究TNBC占23.8%,也有TNBC占24.8%的报道,这和本研究TNBC占乳腺癌的27.08%比较接近,究其原因,可能是本研究严格按照ASCO/CAP指南推荐标准进行判定,27.08%应该是最实际的数据。实际工作中,TNBC是按照免疫组化结果判定的,不同的实验室对同一病例的判断也会必然不同。
BLBC由PEROU等在2000年时首次提出,对内分泌及靶向治疗均不敏感,容易复发及发生转移。ER、PR和HER2阴性与CK5/6和(或)EGFR阳性目前已经成为经典的BLBC诊断标准。本研究发现,BLBC与TNBC在形态、免疫表型及生物学特征上互有重叠。本研究结果BLBC占TNBC的63.64%(14/ 22),低于文献[5]中占85%的报道,这也可能是乳腺癌国内外发病与分型的差异。但须注意的是EGFR单独使用时的阳性率很低,CK5/6与EGFR联合应用优于单独使用,可以从TNBC中筛选出大部分的BLBC。
TNBC及BLBC其恶性度高,侵袭性强,容易复发及发生淋巴结转移,更倾向于经血道转移至脑或肺,其无病生存期及总体生存率均较NTNBC为低,是生物学行为及临床预后较差的乳腺癌亚型,大部分患者5年内死亡。本研究的三阴乳腺癌组无组织学Ⅰ级病例,其组织学Ⅱ及Ⅲ级的病例分别为14例(53.85%,14/26)及12例(46.15%,12/26),淋巴结转移率为61.11%(11/18);BLBC在组织学分级上基本同TNBC,淋巴结转移率为55.56%(5/9),高于非三阴乳腺癌,而低于TNBC;TNBC低分化病例的比例以及淋巴结的转移率均高于NTNBC,差异有统计学意义(P<0.001)。免疫组化HER2 IHC2+以下的病例,是否给予HER2靶向治疗,需要进行FISH或CISH(色素原位杂交)的检测,以确定该基因有无扩增。TNBC与BLBC发病均倾向于中、老年女性,临床表现、生物学行为相似,两者的预后与各自组织学类型的关系尚待进一步研究。
(References)
[1]CHOI J,KIM D H,JUNG W H,et al.Metabolic interaction between cancer cells and stromal cells according to breast can⁃cer molecular subtype[J].Breast Cancer Res,2013,15(5):R78.
[2]RAKHA E A,EL-SAYED M E,GREEN A R,et al.Prognostic markers in triple-negative breast cancer[J].Cancer,2007,109:25-32.
[3]CAREY L A,PEROU C M,LIVASY C A,et al.Race,breast cancer subtypes,and survival in the Carolina breast can⁃cer study[J].JAMA,2006,295:2492e502.
[4]REDDY K B.Triple-negative breast cancers:an updated review on treatment options[J].Curr Oncol,2011,18(4):e173-179.
[5]BANER JEE S,REIS-FILHO J S,ASHLEY S,et al.Basal-like breast carcinomas:clinical outcome and response to che⁃motherapy[J].J Clin Pathol,2006,59(7):729-735.
[6]SIZIOPIKOU K P,COBLEIGH M.The basal subtype of breast carcinomas may represent the group of breast tumors that could benefit from EGFR-targeted therapies[J].Breast,2007,16(1):104-107.
[7]WOLFF A C,HAMMOND M E,HICKS D G,et al.Recommendations for human epidermal growth factor receptor 2 testing in breast cancer:American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update[J].J Clin Oncol,2013,31(31):3997-4013.
[8]BILICI A L,ARSLAN C,ALTUNDAG K.Promising therapeutic options in triple-negative breast cancer[J].J Buon,2012,17(2):209-222.
[9]RAKHA E A,ELLIS I O.Triple-negative/basal-like breast cancer:review[J].Pathology,2009,41(1):40-47.
[10]袁中玉,王树森,高岩,等.305例三阴乳腺癌患者的临床特征及预后因素分析[J].癌症,2008,27(6):561-565.
[11]王成鑫,刘丽江.乳腺少见疾病的病理诊断学[M].武汉:武汉出版社,2013:148-152.
[12]官静,陈莹,刘丽江.乳腺癌组织微阵列HER-2/neu,ER,PR相关性的研究[J].中国现代医学杂志,2004,14(6):50-53.
(责任编辑:范建凤)
Abstract:ObjectiveTo study whether exogenous HA can reduce macrophage-tropic(CCR5-dependent,R5) HIV infectivity.MethodsIn this study,first using TZM-bl cell and un-stimulated CD4+T cells assays to assess whether exogenous HA can reduce R5-HIV infectivity.Next treat the un-stimulated CD4+T cells with hyaluroni⁃dase to study endogenous HA impact on R5-HIV infectivity.At last measures both exogenous HA,and endoge⁃nous HA effect on R5-HIV binding on CD4+T cells.Results(1)100 μg of exogenous HA treatment can reduce R5-HIV infectivity on TZM-bl cells and un-stimualted CD4+T cells(P<0.001).(2)Hyaluronidase treatment can enhance HIV infectivity,by adding 100 μg of exogenous HA can reverse the function of hyaluronidase treatment(P<0.001).(3)100 μg of exogenous HA can reduce R5-HIV binding to CD4+T cells,while hyaluronidase treatment can enhance R5-HIV binding to CD4+T cells(P<0.001).ConclusionExogenous HA can reduce R5-HIV in⁃fectivity on un-stimulated CD4+T cells,while hyaluronidase treatment can enhance R5-HIV binding to CD4+T cells,and R5-HIV infectivity.
Keywords:hyaluronic acid(HA);R5-HIV;infectivity;CD4+T cell
李培林
(加州大学旧金山分校医学院医学系,旧金山CA94121)
摘要:目的探讨外源性透明质酸(HA)是否可以降低巨噬细胞嗜性(CCR5依赖,R5)人类免疫缺陷病毒(HIV)对CD4+T细胞的感染性。方法首先用TZM-bl细胞和未受刺激的CD4+T细胞检测,以评估外源性透明质酸(HA)能否降低R5-HIV的感染性。用透明质酸酶去处理未受刺激的CD4+T细胞,研究内源性HA对R5-HIV感染性的影响。最后,同时测量外源性和内源性透明质酸(HA)对R5-HIV对CD4+T细胞粘和力的影响。结果(1)100 μg外源性HA处理能够显著降低R5-HIV感染TZM-bl细胞和未受刺激的CD4+T细胞(P<0.001)。(2)透明质酸酶处理可增强HIV的感染性,但是如果加上100 μg外源性HA可以逆转透明质酸酶的处理(P<0.001)。(3)100 μg外源性HA可以减少R5-HIV对CD4+T细胞的粘和力,透明质酸酶处理可以提高R5-HIV对CD4+T细胞的粘和力(P<0.001)。结论外源性HA减少R5-HIV对未受刺激的CD4+T细胞的感染性,而透明质酸酶处理可以提高R5-HIV对CD4+T细胞的粘和力,能增强R5-HIV对CD4+T细胞的感染性。
关键词:透明质酸;R5-HIV;病毒感染;CD4+T细胞
0 Introduction
Prevention of HIV transmission is still the most direct way to stem the HIV/AIDS epidemic[1].However,to date,large-scale clinical trials of vaccines to produce an HIV-specific antibody or a T-cell response to pre⁃vent HIV infection have been disappointing[2-3].Since 80%of HIV infection occurs through sexual contact[4], there is intense interest in the prevention of HIV mucosal transmission,and CCR5-tropic viruses(R5 viruses) are preferentially transmitted.To design a better strategy to prevent mucosal transmission of HIV,it needs more fully understand the mechanism of HIV mucosal transmission[5].
Mucosal tissues are the front-line defense against pathogen invasion and greatly impede HIV transmis⁃sion.Studies using the simian immunodeficiency virus(SIV)rhesus macaque model demonstrate that the geni⁃tal tract mucosal barrier limits exposure of CD4+T cells,dendritic cells(DCs),and macrophages to the majority of the viral inoculum,and only a small number of infectious virions pass through the mucosal barrier to estab⁃lish the infected founder population[6-7].These findings are confirmed by clinical studies showing that a small number of infectious virions breach the mucosal barrier to infect resting CD4+T cells,generating a clonal or oli⁃goclonal founder population[5,8-9].
Mucosal integrity plays an important role in HIV transmission,and mucosal inflammation can increase HIV transmission[10-12].The mucosal tissues are composed of epithelial cells,extracellular matrix,interstitial cells and surface mucus.In addition to providing a full complement of host immune cells that variably facili⁃tate or impede HIV infection,the mucosal surface also serves as a physical barrier to mucosal HIV invasion. Mucosal mucus can trap HIV virions[13]and reduce virion movement[14].An acidic vaginal mucosal environment can decrease the rate of HIV sexual transmission[15].How these effects on mucosal HIV transmission are mediat⁃ed remains largely unknown[5,9].
The surface of the mucosal layer is a scaffold with extracellular matrix,a major component of the extracel⁃lular matrix is hyaluronic acid(HA,or hyaluronan).HA is a large glycosaminoglycan(GAG)that can be remod⁃eled and degraded by hyaluronidase.On the surface of the cells,HA polymers extend up to 25 μm in length, forming pericellular coats.HA interaction with its receptors can induce cellular signaling and is involved in mu⁃cosal tissue homeostasis and maintenance of tissue integrity[16-18].HA is also a regulator of immunity.HA inter⁃action with its main receptor,CD44,regulates recruitment and extravasation of T-cells into sites of inflamma⁃tion[19-20]and participates in the inflammatory process[16,21].HA interaction with CD44 can reduce cytokine pro⁃duction from macrophages in the setting of inflammation[22]and lowers PKCa activity to decrease histamine re⁃lease from leukemic cell lines[23].
In our lab,recently we observed that exogenous HA reduced HIV infectivity when both virions and CD4+T cells expressed CD44.Effects were seen on both early infection events like viral binding and probably later events through reduction of PKCa activation,while treatment with hyaluronidase reduced endogenous HA thick⁃ness and enhanced susceptibility of CD4+T cells to infection,but in that study the HIV was generated from NL4-3 plasmid,which is a T-cell-tropic(CXCR4-dependent,X4)[24].Clinical studies have found that CCR5-tropic viruses(R5 viruses)are preferentially transmitted[5].The main aim of this study was to assess the role of HA in CCR5-tropic HIV infection on un-stimulated CD4+T cells.We observed that exogenous HA re⁃duced both X4,and R5-HIV infectivity on un-stimulated CD4+T cells.Effects were seen on viral binding, while treatment with hyaluronidase reduced endogenous HA thickness and enhanced susceptibility of CD4+T cells to infection.
1 Material and Methods
1.1 Material
Hyaluronic acid(HA)(Sigma,St.Louis,MO),hyaluronidase(Hase)(Sigma,St.Louis,MO),Phytomeagglu⁃tinin-M(PHA-M)(Roche,Indianapolis IN),human-Interleukin 2(hIL-2)(Roche,Indianapolis,IN),MDEM and PRMI(Life Technologies,Carlsbad,CA),anti-HIV-1-p24 antibody(Santa Cruz Biotechnology,Dallas, Texas),Alexa Fluor647(Life Technologies,Carlsbad,CA),cell membrane staining(Life Technologies,Carls⁃bad,CA),stained nuclei with DAPI(Life Technologies,Carlsbad,CA),anit-CD4-PE(R&D System),EasySep Human CD4+T cell Enrichment kit(STEMCell,Vancouver,BC),HIV-1p24 ELISA kit(PerkinElmer, Waltham,MA).Beta-Glo®assay system(Promega,Madison WI).
1.2 Methods
1.2.1 Isolation of CD4+T cells from healthy donorsCD4+T cells were isolated from healthy donors PBMCs using the EasySep Human CD4+T cell Enrichment kit(STEMCell,Vancouver,BC)according to the manufac⁃turer′s instructions.
1.2.2 Generation of X4(NL4-3)and R5(YK-JRCSF)HIV virus stock from PBMCIsolated PBMCs were stimulated with 3 μg/mL of phytomeagglutinin-M(PHA-M)(Roche,Indianapolis IN);and 20 unit/mL of hu⁃man-Interleukin 2(hIL-2)(Roche,Indianapolis,IN)for 3 days,X4 and R5 HIV viral supernatant from trans⁃fection of 293T cells was used to infect pooled mixed stimulated PBMCs prepared from 2 healthy donors.The supernatant from HIV infected PBMCs was harvested at day 7 and day 11.Viral titers were determined by HIV-1p24 ELISA(PerkinElmer,Waltham,MA).
1.2.3 Reduction of HA from cell surface1x106/mL of unstimulated CD4+T cells were washed 3 times in RPMI without FCS and incubated in RPMI with 12 unit/mL of hyaluronidase(Hase)(Sigma,St.Louis,MO)for 60 min,followed by removal of supernatant and three washes with RPMI without FCS.
1.2.4 Staining HIV-p24 on unstimulated CD4+T cellsHIV staining:Unstimulated CD4+T cells were incu⁃bated with R5-HIV for 5 hours,fixed with 2%formaldehyde,and incubated with mouse anti-HIV-1 p24 anti⁃body at 4℃overnight,then stained with donkey anti-mouse IgG antibody conjugated with Alexa Fluor647 (Life Technologies,Carlsbad,CA)for 2 hours.HIV-p24 staining was measured by 2 methods:laser scanning microscopy(LSM),and flow cytometry(FACS).For LSM analysis:the cells were further stained with anit-CD4-PE(R&D System),cell membranes with cell membrane staining(Life Technologies,Carlsbad,CA), and stained nuclei with DAPI(Life Technologies,Carlsbad,CA),and LSM510 META laser scanning micro⁃scope(Carl Zeiss Microimaging Inc.Thornwood,NY,USA)was used to scan the cells with Z-stack projections. For FACS analysis:50 000 HIV-p24 stained cells were analyzed by EasyCyte6HT-2L(Millipore,MA).
1.2.5 Assays for HIV Infection(1)TZM-bl cells(NIH AIDS Research and Reference Reagent Program):3× 104cells plated into 96 well plate for overnight,then removed supernatant and cells were washed with complete DMEM without FCS,then treated with study reagents,inoculated with 100pg HIV-p24 of HIV/well for 5 hours, washed 3 times with complete DMEM,and cultured in complete DMEM.HIV infectivity was measured by us⁃ing Beta-Glo®assay system(Promega,Madison WI)and measured with a plate reader(VICTOR3)(PerkinEl⁃mer)at 3 days post-infection[25].The luciferase activity is presented as relative light units(RLU).(2)Unstimulat⁃ed CD4+T cells:1×106healthy donor unstimulated cells were washed with RPMI without FCS,treated with dif⁃ferent reagents,inoculated with 1 000 pg HIV-p24 of HIV for 5 hours,washed 3 times with complete RPMI,re⁃suspended in complete RPMI with 5 μg of PHA-M and 20 unit of hIL-2 for 24 hours,washed 3 times with com⁃pleted RPMI,and finally resuspended in completed RPMI with 20 unit of hIL-2.HIV infectivity was measured by HIV-1 p24 production in supernatant at day 7 post-infection by using HIV-1p24 ELISA kit(PerkinElmer, Waltham,MA).
1.3 Statistical analysis
TZM cell assay was run in triplicate and repeated at least 3 times.Experiments with primary CD4+T cells were run in duplicate and repeated with at least 3 different donors.Data averages and standard deviations(SD)were calculated in Microsoft Excel 2008 and presented as means±standard deviation(x±s).Significance was assessed by a t-test,with P<0.05 considered significant.
2 Results
2.1 Exogenous HA reduces both X4 and R5-HIV infectivity on TZM-bl cells line,and unstimulated CD4+T cells
Earlier studies reported that exogenous HA could interrupt T cell rolling and impede extravasation of T cells into an inflamed site through interactions with CD44[19].To study whether exogenous HA can impact HIV infectivity,TZM-bl cells[25]were treated with exogenous HA for 1 hour,then inoculated with X4(NL4-3)or R5 (YK-JRCSF)produced from PBMCs cells and normalized by p24.HIV infectivity was measured at day 3 post infection by luciferase activity[25]as relative light units(RLU).Exogenous HA reduced infectivity of both X4 (NL4-3)and R5(YK-JRCSF)HIV significantly(Fig.1A).
In vivo studies of acute HIV and SIV infection demonstrate that virus initially targets resting CD4+T cells and establishes an infected founder population during mucosal transmission[5,8-9].To study whether exogenous HA treatment can reduce infectivity of both R5(YK-JRCSF)and X4(NL4-3)HIV on CD4+T cells,primary unstimulated CD4+T cells from healthy donors were treated with exogenous HA,and then inoculated with vi⁃ral stocks of both X4(NL4-3)or R5(YK-JRCSF)HIV normalized by p24,then stimulated with PHA and IL-2 for 24 hours.HIV infectivity was assessed by measurement of supernatant HIV-1 p24 7 days post-infection. Exogenous HA treatment significantly reduced HIV-1 p24 production during both X4(NL4-3)and R5 (YK-JRCSF)infection(Fig.1B).
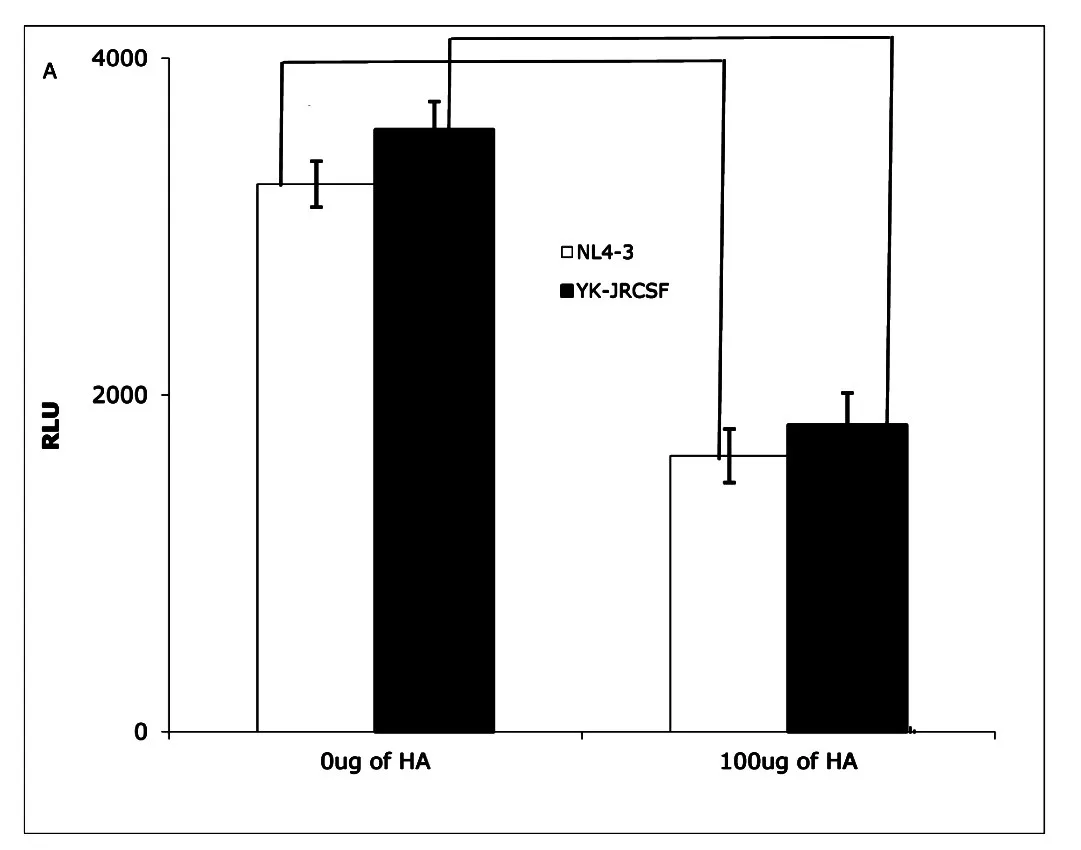
Fig.1ATZM-bl cells assay:Exogenous HA(Sigma,St. Louis,MO)reduced infectivity of both NL4-3(X4)(open bar)and YK-JRCSF(R5)HIV(filled bar).(Data are mean±SEM of triplicate samples and represent 3 independent experiments)
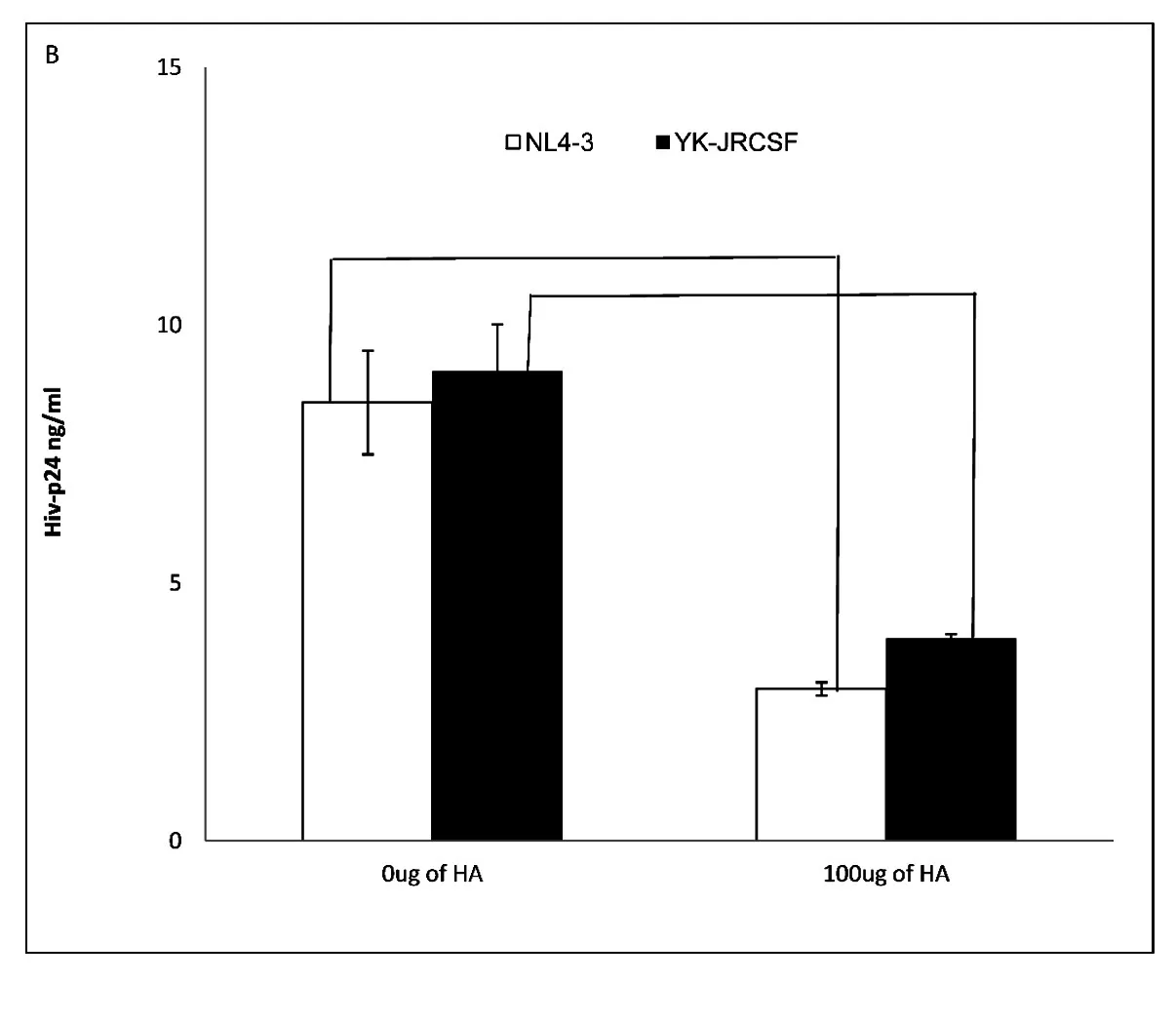
Fig.1BUn-stimulated CD4+T cells assay:Exogenous HA decreased infectivity of both NL4-3(X4)(open bar) and YK-JRCSF(R5)on primary un-stimulated CD4+T cells.(Data are mean±SEM of duplicate samples and representative of 3 donors)
2.2 Hyaluronidase treatment can enhance both X4 and R5-HIV infectivity on unstimulated CD4+T cells
Endogenous HA has been observed to form a cushion on the cell surface,to play an anti-adhesive role[18]and to impede ligand access to cell-surface receptors[26].Hyaluronidase treatment can reduce endogenous HA from the cell surface,thus promoting cell-cell contact[17].Hyaluronidase is highly activated during sexual inter⁃course as well as inflammation[16-18].Our initial experiments showed that exogenous HA reduced both X4 (NL4-3)and R5(YK-JRCSF)HIV infection of unstimulated CD4+T cells.Thus,we studied the impact of hyal⁃uronidase treatment on HIV infection of primary unstimulated CD4+T cells.Healthy donor,unstimulated primaryCD4+T cells were treated with hyaluronidase prior to inoculation with an equivalent input(by p24)of either X4 (NL4-3)or R5(YK-JRCSF),then stimulated with PHA and IL-2 for 24 hours.At day 7 post-infection,infec⁃tivity was assessed by measurement of HIV-1 p24 in culture supernatants.Consistent with the ability of endog⁃enous HA to inhibit HIV infection,hyaluronidase treatment significantly increased both X4(NL4-3)and R5( YK-JRCSF)infection of unstimulated CD4+T cells,but this enhancement could be completely reversed by ad⁃dition of exogenous HA(Fig.2).
These results indicate that hyaluronidase treatment renders unstimulated CD4+T cells more susceptible to HIVCD44infection,possibly through reduction of cell surface HA.
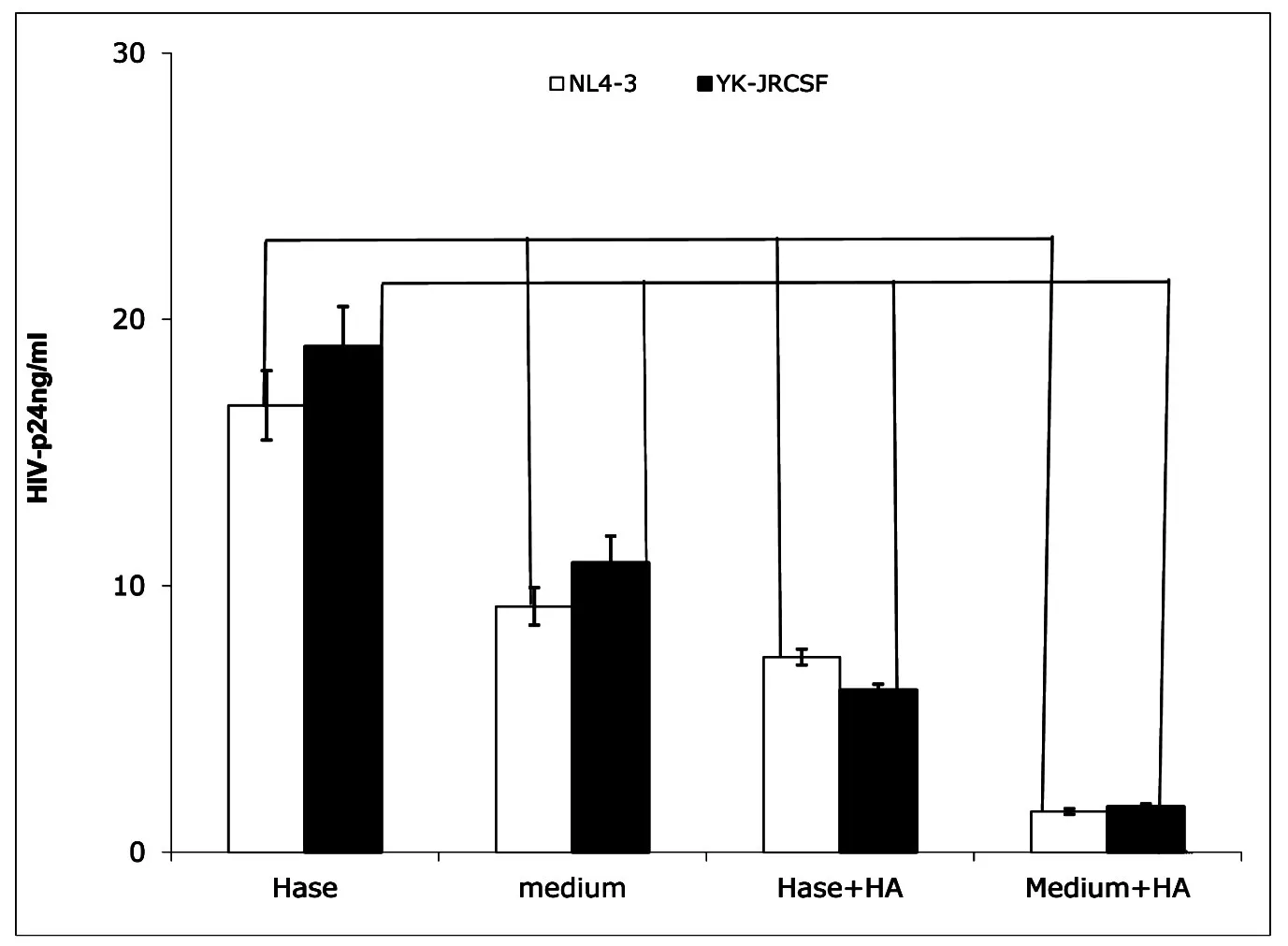
Fig.2Hyaluronidase treatment enhanced HIV infection of unstimulated CD4+T cells.Hase(Hyaluronidase treatment) (Sigma,St.Louis,MO);medium(medium treatment);Hase+HA:(Hyaluronidase treatment with 100 μg of exogenous HA(Sigma,St.Louis,MO));Medium+HA:(medium treatment with100 μg of exogenous HA).Treatment of healthy donor unstimulated CD4+T cells by hyaluronidase(Hase)boosted both X4(open bar)and R5(filled bar)HIV infection, and exogenous HA reduced this enhancement(Hase+HA).(All data are mean±SEM from duplicate samples and representative of at least 3 donors)
2.3 Hyaluronidase treatment enhances R5-HIV binding on unstimulated CD4+T cells
Next,we investigated how hyaluronidase treatment impacts HIV binding HA on the surface of unstimulated CD4+T cells.Our early results shown that hyaluronidase treatment can reduce endogenous HA thickness on surface of the un-stimulated CD4+T cells[24].Because the thickness of endogenous HA has been postulated to prevent ligand binding to cognate receptors on the surface of T-cells[27]and hyaluronidase treatment enhanced infectivity of both X4(NL4-3)and R5(YK-JRCSF),we hypothesized that hyaluronidase-mediated reduction of HA on the cell surface may enhance HIV binding.To test this hypothesis,unstimulated,primary CD4+T cells were treated by hyaluronidase and then incubated with R5(YK-JRCSF)in the presence 10 μg/mL of the peptide fusion inhibitor T-20[25]for 5 hours.Cells were washed 5 times to remove unbound HIV,stained with anti-HIV-1 p24 antibody,and studied by laser scanning microscopy.Hyaluronidase treatment significantly in⁃creases HIV binding on surface of the unstimulated,primary CD4+T cells(Fig.3A,B,C,D,E).
3 Discussion
Devising more effective interventions to prevent mucosal HIV transmission will require a deeper under⁃standing of the interplay between virus and target cells in the mucosal environment.Studies of both human and rhesus macaque models indicate that mucosal tissues provide multiple mechanisms to prevent HIV and SIV in⁃fection,including physical barriers and innate and adaptive immune responses[5,9].However,a small amount of HIV-1 and SIV can penetrate the mucosal barrier,gaining access to the sub-mucosa and the initial recipient cell targets,which appear to be predominantly resting CD4+T cells[8].Details of the interaction of HIV and SIVwith resting CD4+T cells in the sub-mucosa are not fully understood,but CCR5-tropic viruses(R5-HIV)are preferentially transmitted[5,9].In this study,we show that endogenous HA on unstimulated CD4+T cells is an ob⁃stacle for HIV infection and that hyaluronidase treatment can increase binding of HIV particles,and enhance HIV infectivity.Furthermore,addition of exogenous HA at 100 μg/mL,the concentration of HA in human epi⁃dermis[28],reduces HIV infectivity on unstimulated CD4+T cells.These data collectively argue that HA inter⁃feres with HIV infection during early stage,perhaps by directly impacting the interactions between CD44 andother molecules,or altering the distribution and/or activation status of local CD4+T cells,thus reducing targets which are needed for efficient transmission.
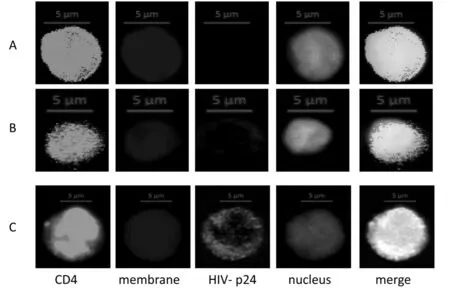
Fig.3(A,B,C)LSM510 META laser scanning microscope(Carl Zeiss Microimaging Inc.Thornwood,NY,USA)was used to scan the cells.Images are 40x;CD4+T cells were stained with mouse anti-HIV-1p24(Santa Cruz Biotech)and donkey anti-mouse IgG antibody with AlexaFluor@680(Life Technologies,Carlsbad,CA).CD4-PE(R&D Sytem),cell membrane staining(Life Technologies,Carlsbad,CA);and nuclear staining-DAPI(Life Technologies,Carlsbad,CA). (A)CD4+T cells treated with 100 μg of exogenous HA;(B)CD4+T cells treated with medium;(C)CD4+T cells treated with hyaluronidase
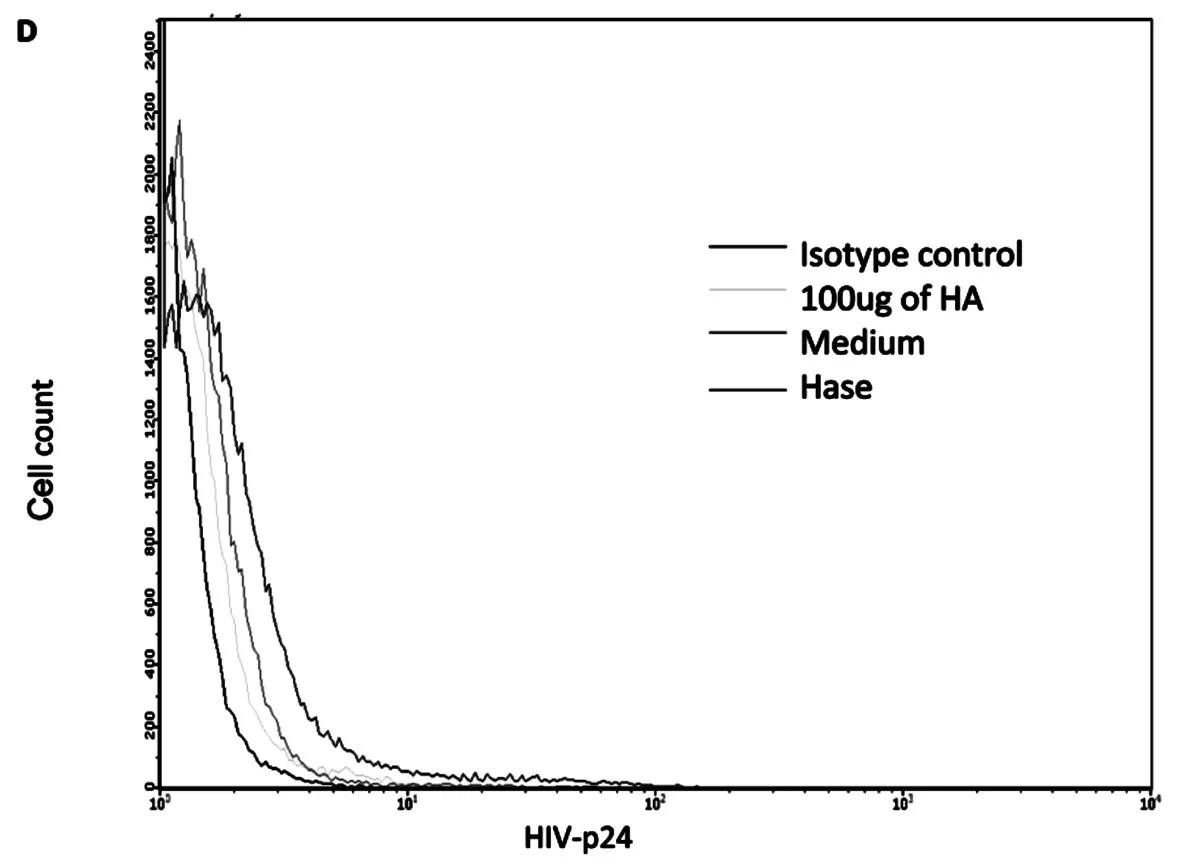
Fig.3 DFACS results:cells with isotype control,cells treated with 100 μg of HA,cells treated with medium and cells treated with hyaluronidase
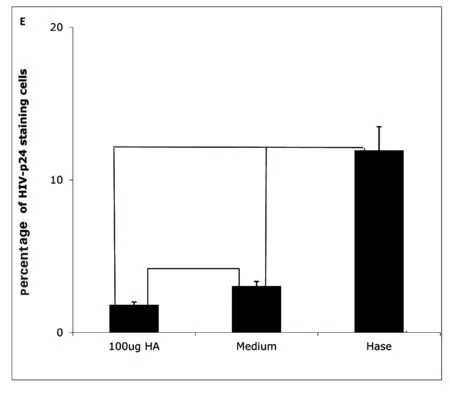
Fig.3EPercentage of HIV-1-p24 positive cells treated with hyaluronidase(Hase)or with medium(Medium)or with 100 μg of HA(100 μg HA).(All data are mean± SEM from duplicate experiments representative of at least 3 donors)
HA is the main component of the extra cellular matrix(ECM)in the mucosal tissue.The main receptor for HA,CD44,is highly expressed in all cells,including CD4+T cells,in mucosal tissues,especially those along the reproductive tract[18,29].HA interactions with CD44 are involved in mucosal immunity and participate in mu⁃cosal inflammation[16,21].It has been reported that exogenous HA can interfere with interaction of endogenous HA with CD44,limiting recruitment of T cells by reducing T cell adhesion[30],preventing T cell rolling,and in⁃hibiting T cell extravasation into an inflamed site[19-20].Other studies identify the recruitment of T cells into sub⁃mucosa as important and necessary for mucosal HIV transmission[5,9].
Our study demonstrates that exogenous HA reduces both X4 and R5 HIV infection of unstimulated CD4+T cells.Others have reported that the endogenous HA coat on the surface of cells can prevent extraneous or in⁃discriminant ligand binding[18]and can prevent infection with newcastle disease virus(NDV),vesicular stomati⁃tis virus(VSV),and rubella virus(RV).Reducing the thickness of HA on the cell surface by hyaluronidase treatment can make target cells more susceptible to NDV,VSV,and RV infection[31].We also observed that treatment of unstimulated CD4+T cells with hyaluronidase reduced the thickness of endogenous HA on the cell surface[24],allowing more HIV particles to bind(Fig.3),an effect that could be reversed by the addition of exoge⁃nous HA(Fig.2).While these experimental results suggest that the inhibitory effects of HA on HIV infection occur at least in part at an early stage of the viral life cycle,including effects localizable to viral binding, further work is needed.
It is notable that HA,and hyaluronidase are all highly expressed and play important roles in maintaining the integrity and function of the mucosal tissue along the reproductive tract.Hyaluronidase is also a major con⁃stituent of semen[29].Both HA and hyaluronidase are highly up-regulated during sexual intercourse as well as in⁃flammation[18].The processes of reproductive fertilization and HIV transmission intersect at many levels anatom⁃ically and functionally.Both involve the reproductive tract and permissiveness of mucosal tissue and surface barriers.Clinical studies have demonstrated that inflammation in the mucosal tissue can facilitate HIV trans⁃mission[32],and that transmission rates are higher for HIV in semen compared to blood[33].The identification of topical agents that can be applied to mucosal surfaces to prevent mucosal HIV transmission has been identified as a priority area for research and development in the effort to control the HIV/AIDS epidemic[34].
In summary,HA present on the surface of unstimulated CD4+T cells can influence both X4 and R5-HIV infection.Both HA and hyaluronidase have well described roles in reproductive and inflammatory processes. Our data now show that the status of the HA coat may play an important role in the initial interaction of X4 and R5-HIV virions with resting CD4+T cells,a feature that may be particularly relevant for mucosal HIV transmis⁃sion.Intriguingly,exogenous HA appears to block HIV engagement and infection of target cells.HA is a non-immunogenic natural biopolymer that has been used in a variety of clinical applications.These findings should be further explored in vivo and,if confirmed,could lead to the development of novel interventions to re⁃duce HIV mucosal transmission.
Conflict of Interest
The authors declare that they have no conflict of interest.
Acknowledgments
This work was supported by the National Institutes of Health[grants 1R21AI104445-01A1(PL)].
参考文献(References)
[1]PADIAN N S,MCCOY S I,KARIM S S,et al.HIV prevention transformed:the new prevention research agenda[J].Lancet, 2011,378:269-278.
[2]PITISUTTITHUM P,GILBERT P,GURWITH M,et al.Randomized,double-blind,placebo-controlled efficacy trial of a bi⁃valent recombinant glycoprotein 120 HIV-1 vaccine among injection drug users in Bangkok,Thailand[J].J Infect Dis,2006,194:1661-1671.
[3]WATKINS D I,BURTON D R,KALLAS E G,et al.Nonhuman primate models and the failure of the Merck HIV-1 vaccine in humans[J].Nat Med,2008,14:617-621.
[4]UNAIDS.(Global report 2013.Geneva)[EB/OL].[2013]http://www.unaids.org/globalreport/global_report.htm.
[5]SHAW G M,HUNTER E.HIV transmission[J].Cold Spring Harb Perspect Med,2012,2:1-23.
[6]MILLER C J,LI Q,ABEL K,et al.Propagation and dissemination of infection after vaginal transmission of simian immunode⁃ficiency virus[J].J Virol,2005,79:9217-9227.
[7]LI Q,ESTES J D,SCHLIEVERT P M,et al.Glycerol monolaurate prevents mucosal SIV transmission[J].Nature,2009,458:1034-1038.
[8]ZHANG Z,SCHULER T,ZUPANCIC M,et al.Sexual transmission and propagation of SIV and HIV in resting and activated CD4+T cells[J].Science,1999,286:1353-1357.
[9]HAASE A T.Early events in sexual transmission of HIV and SIV and opportunities for interventions[J].Annu Rev Med,2011,62:127-139.
[10]GIAVEDONI L D,CHEN H L,Hodara V L,et al.Impact of mucosal inflammation on oral simian immunodeficiency virus transmission[J].J Virol,2013,87:1750-1758.
[11]LAJOIE J,JUNO J,BURGENER A,et al.A distinct cytokine and chemokine profile at the genital mucosa is associated with HIV-1 protection among HIV-exposed seronegative commercial sex workers[J].Mucosal Immunol,2012,5:277-287.
[12]HAALAND R E,HAWKINS P A,SALAZAR-GONZALEZ J,et al.Inflammatory genital infections mitigate a severe genet⁃ic bottleneck in heterosexual transmission of subtype A and C HIV-1[J].PLoS Pathog,2009,5:e1000274.
[13]MAHER D,WU X,SCHACKER T,et al.HIV binding,penetration,and primary infection in human cervicovaginal tissue[J]. Proc Natl Acad Sci U S A,2005,102:11504-11509.
[14]SHUKAIRS A,ALLENSA,CIANCI GC,et al.Human cervicovaginal mucus contains an activity that hinders HIV-1movement[J].Mucosal Immunol,2013,6:427-434.
[15]LAI S K,HIDA K,SHUKAIR S,et al.Human immunodeficiency virus type 1 is trapped by acidic but not by neutralized human cervicovaginal mucus[J].J Virol,2009,83:11196-11200.
[16]TOOLEB P.Hyaluronan:from extracellular glue to pericellular cue[J].Nat Rev Cancer,2004,4:528-539.
[17]GIRISHK S,KEMPARAJU K.The magic glue hyaluronan and its eraser hyaluronidase:a biological overview[J].Life Sci,2007,80:1921-1943.
[18]EVANKO S P,TAMMi M I,TAMMI R H,et al.Hyaluronan-dependent pericellular matrix[J].Adv Drug Deliv Rev,2007,59:1351-1365.
[19]DE GRENDELE H C,ESTESS P,SIEGELMAN M H.Requirement for CD44 in activated T cell extravasation into an in⁃flammatory site[J].Science,1997,278:672-675.
[20]SIEGELMAN M H,DE GRENDELE H C,ESTESS P.Activation and interaction of CD44 and hyaluronan in immunologi⁃cal systems[J].J Leukoc Biol,1999,66:315-321.
[21]JIANG D,LIANG J,NOBLEP W.Hyaluronan as an immune regulator in human diseases[J].Physiol Rev,2011,91: 221-264.
[22]MUTO J,YAMASAKI K,TAYLOR K R,et al.Engagement of CD44 by hyaluronan suppresses TLR4 signaling and the sep⁃tic response to LPS[J].Mol Immunol,2009,47:449-456.
[23]KIM Y,LEE Y S,HAHN J H,et al.Hyaluronic acid targets CD44 and inhibits FcepsilonRI signaling involving PKCdelta, Rac1,ROS,and MAPK to exert anti-allergic effect[J].Mol Immunol,2008,45:2537-2547.
[24]LI P,FUJIMOTO K,BOURGUINGNON L,et al.Exogenous and endogenous hyaluronic acid reduces HIV infection of CD4+T cells[J].Immunol Cell Biol,2014,Jun 24,doi:10.1038.
[25]DERDEYN C A,DECKER J M,SFAKIANOS J N,et al.Sensitivity of human immunodeficiency virus type 1 to the fusion inhibitor T-20 is modulated by coreceptor specificity defined by the V3 loop of gp120[J].J Virol,2000,74:8358-8367.
[26]ZHANG L S,MA H W,GREYNER H J,et al.Inhibition of cell proliferation by CD44:Akt is inactivated and EGR-1 is down-regulated[J].Cell Prolif,2010,43:385-395.
[27]MCBRIDE W H,BARD J B.Hyaluronidase-sensitive halos around adherent cells.Their role in blocking lymphocyte-me⁃diated cytolysis[J].J Exp Med,1979,149:507-515.
[28]VOLPI N 1,SCHILLER J,STERN R,et al.Role,metabolism,chemical modifications and applications of hyaluronan[J]. Curr Med Chem,2009,16:1718-1745.
[29]RODRIGUEZ HURTADO I,STEWART A J,WOLFE D F,et al.Immunolocalization of the hyaluronan receptor CD44 in the reproductive tract of the mare[J].Theriogenology,2010,75:276-286.
[30]MOHAMADZADEH M,DEGRENDELE H,ARIZPE H,et al.Proinflammatory stimuli regulate endothelial hyaluronan ex⁃pression and CD44/HA-dependent primary adhesion[J].J Clin Invest,1998,101:97-108.
[31]PATTERSON R L,PETERSON D A,DEINHARDT F,et al.Rubella and rheumatoid arthritis:hyaluronic acid and suscep⁃tibility of cultured rheumatoid synovial cells to viruses.(resistant to virus)[J].Proc Soc Exp Biol Med,1975,149:594-598.
[32]GALVIN S R,COHEN M S.The role of sexually transmitted diseases in HIV transmission[J].Nat Rev Microbiol,2004,2: 33-42.
[33]PILCHER C D,TIEN H C,ERON J J Jr,et al.Duke-UNC-Emory Acute HIV Consortium.Brief but efficient:acute HIV infection and the sexual transmission of HIV[J].J Infect Dis,2004,189:1785-1792.
[34]HLADIK F,DONCEL G F.Preventing mucosal HIV transmission with topical microbicides:challenges and opportunities[J]. Antiviral Res,2010,88S:S3-9.
(责任编辑:陈旷)
Investigation of Pathomorphology and Biologic Characteristics of Triple-Negative Breast Cancer and Basal-Like Breast Cancer
WANG Chengxin,HUANG Xuan,FENG Hua
(Jiangda Pathologic Diaglostic Institute;Department of Pathology&Pathophysiology,School of Medicine,Jianghan University, Wuhan 430056,Hubei,China)
ObjectiveTo investigate the pathomorphology,biologic characteristics and the relation⁃ships oftriple-negative breast cancer(TNBC),non triple-negative breast cancer(NTNBC)andbas⁃al-like breast cancer(BLBC).MethodsHER2,ER,PR,CK5/6 or EGFR protein were deter⁃mined with immunohistochemistry(IHC)in breast cancer,3 cases of HER2 IHC 3+and 5 cases of HER2 IHC 2+were analysed for HER2 gene amplification with fluorescent in situ hybridization(FISH).CK5/6 or EGFR were checked in 22 cases of TNBC.The cases were divided into the TNBC,NTNBC and BLBC groups according to the examination results.The pathomorphology and bi⁃ologic characteristics of the three groups were compared.ResultsOf the 96 cases,27.08%(26/96)were confirmed to be TNBC in which gradeⅡandⅢcases were 53.85%(14/26)and 46.15%(12/ 26)respectively,lymph nodes metastasis rate was 61.11%(11/18);BLBC accounted for 63.64%(14/ 22)of TNBC,in which gradeⅡandⅢcases were 57.14%(8/14)and 42.86%(6/14)respective⁃ly,lymph nodes metastasis rate was 55.56%(5/9);There were no gradeⅠcases in TNBC and BLBC.72.92%(70/96)were confirmed to be NTNBC in which gradeⅠ,ⅡandⅢcases were 28.57%(20/70),57.14%(40/70)and14.29%(10/70)respectively,lymph nodes metastasis rate was 44.44%(16/ 36).The percentage of poorly differentiated cases and lymph nodes metastasis rate were higher in the TNBC and BLBC group than those in NTNBC,besides there was no gradeⅠcases in TNBC and BLBC group.Of the 5 HER2 IHC 2+cases,one case there was gene amplification,one equivocal and three negative and of 3 HER2 IHC 3+cases,the FISH result was consistent with IHC.Conclu⁃sionMore than 1/4 of breast cancer are TNBC or BLBC in our study.Compared with NTNBC,even though TNBC and BLBC share a great deal of overlap and have a poor differentiation with aggressive behavior and increased local recurrence or distant metastasis,indicating a poor prognosis,they may be independent histopathologic entity.CK5/6 or EGFR can be used to differentiate the BLBC from TNBC.IHC 2+cases should be examined with FISH in order to avoid misleading treatment.
triple-negative breast cancer;basal-like breast cancer;pathomorphology;FISH
Exogenous Hyaluronic Acid Reduces R5-HIV Infection of CD4+T Cells
LI Peilin
(Department of Medicine,University of California San Francisco(UCSF),San Francisco CA 94121,USA)
外源性透明质酸减少R5-HIV对CD4+T细胞感染的研究
2014-08-13
1R21AI104445-01A1(PL)
R737.902
A文章编号:1673-0143(2014)06-0057-05
R512.91文献标志码:A
1673-0143(2014)06-0062-09
2014-09-29
王成鑫(1954—),男,教授,主任医师,硕士生导师,研究方向:肿瘤病理。
Biography:LI Peilin(1958—),male,associate professor,majors in molecular immunology.