An unusual cause of optic neuritis: rickettsiosis disease
Loukil Hanen, Snoussi Mouna, Frikha Faten, Ben Salah Raida, Jallouli Moez, Chérif Yosra, El Aoud Sahar, Marzouk Sameh, Bahloul Zouhir
Department of Internal Medicine, Hédi Chaker University Hospital, Sfax, Tunisia
An unusual cause of optic neuritis: rickettsiosis disease
Loukil Hanen, Snoussi Mouna*, Frikha Faten, Ben Salah Raida, Jallouli Moez, Chérif Yosra, El Aoud Sahar, Marzouk Sameh, Bahloul Zouhir
Department of Internal Medicine, Hédi Chaker University Hospital, Sfax, Tunisia
ARTICLE INFO
Article history:
Received 12 Jul 2014
Received in revised form 10 Aug 2014
Accepted 27 Sep 2014
Available online 17 Oct 2014
Optic neuritis
Optic neuritis (ON) may be associated to a range of autoimmune or infectious diseases. We report herein a case of ON induced byRickettsia conorii. A 53-year-old woman presented with a recent decrease in visual acuity and headache. ON was diagnosed on the basis of ophthalmologic examination and flash visual evoked potentials. Etiological investigation made in our department eliminated first autoimmune disorders (vasculitis and connective tissue diseases). Rickettsial optic neuritis was confirmed by detection of specific antibodies in serum and the negativity of other serologic tests. An association between corticosteroids and cyclines was prescribed with improvement of visual acuity.
1. Introduction
Rickettsioses are caused by small intracellular Gram-negative bacteria belonging to the Rickettsiaceae family. They are transmitted by various arthropod species, which are either vectors or reservoirs for the bacteria[1].The clinical presentation of certain rickettsial infections is known for several centuries and symptoms may vary from mild to severe. Disseminated vasculitis is the basic pathogenetic mechanism of this infection and it may subsequently lead to multiple-organ involvement[2]. Violations eye during rickettsial infection are uncommon. We report a case of optic neuritis (ON) revealingRickettsia conorii(R. conorii) infection in a 53-year-old woman.
2. Case report
A 53-year-old woman presented with a 2-month historyof decreased vision in the left eye. The patient underwent an ophthalmologic consultation, which showed a low visual acuity (VA). Her VA was 4/10 with bilateral central scotoma. The anterior segment and the intraocular pressure were totally normal in both eyes. Dilated fundoscopy revealed a bilateral swelling of the optic disc and there were no retinal vessels abnormalities (Figure 1). A general and neurological examination was normal. Fluorescein angiography was performed showing bilateral papillitis and posterior scleritis without retinal vasculitis (Figure 2). Under the impression of ON, the patient was referred for an electrophysiology examination. Flash visual evoked potentials showed low amplitude in the right eye and delay in the P 100 latency in both eyes corresponding to inflammatory ON (Figure 3). Brain magnetic resonance imaging with intravenous contrast showed an abnormal high signal change in the periventricular and subcortical frontal white matter, interpreted as nonspecific abnormalities. Antinuclear antibodies test screening for autoimmune disorders was positif (titer: 1/640) with two subtypes (anti SSA and anti SSB). Other blood analysis revealing high erythrocyte sedimentation rate (40 mm/H1) and serum level of C-reactive protein was within the normal range. The diagnosis of bilateral ON with encephalitis related to primary Sjögren syndrome was evoked and the patient received corticosteroid therapy with high dose (1 mg/kg/d) preceded by intravenous methylprednisolone pulse. The patient reported partial improvement of visual disturbances and gradually worsening headaches. In June 2013, she was admitted to our Internal Medicine Department. She mentioned oral, ocular and nasal dryness. She also complained of permanent headache and blurred vision. There were no other significant findings on physical or neurological examination. An ophthalmologic examination was performed after 7 days of corticotherapy and showed a VA 4/10 in both eyes, while fundoscopy still showed swelling of the optic disc. Tear break-up time measurement with fluorescein and schirmer didn’t confirm dry eye syndrome. Blood results indicated a slight normochromic anemia, normal cell white and platelet count, aspartate aminotransferase 14 IU/L, alanine aminotrasferase 25 IU/ L, total bilirubin 7 µmol/L (direct bilirubin 2), alkaline phosphatase 45 IU/L, erythrocyte sedimentation rate 11 mm/H1, C-reactive protein 2 mg/L, calcemia 2.27 mmol/L, calciuria 6 mmol/24 h, serum albumin 35 g/L and polyclonal hyperimmunoglobulinemia 16 g/L. Urine microscopy showed no cells or casts. Proteinuria was negative and the renal function was normal. Immunological exams including complement fractions C3 and C4, rheumatoid factor, circulating immunocomplexes, antinuclear antibodies, antineutrophil cytoplasmic antibodies, antiphospholipid antibodies and cryoglobulinia were negative. Serologic tests for herpes simplex, herpes zoster, syphilis, Lyme disease, HIV and Toxoplasma were negative but positive for R. conorii (IgM 64 IU and IgG 128 IU). There was no lymphocytic infiltration of the labial salivary glands.
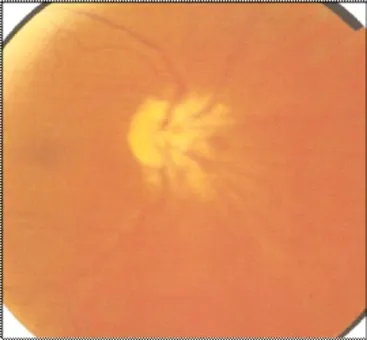
Figure 1.Fundoscopy showing swelling of the optic disc.
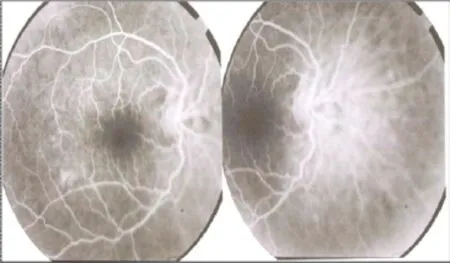
Figure 2.Fluorescein angiography showing bilateral papillitis and posterior scleritis without retinal vasculitis.
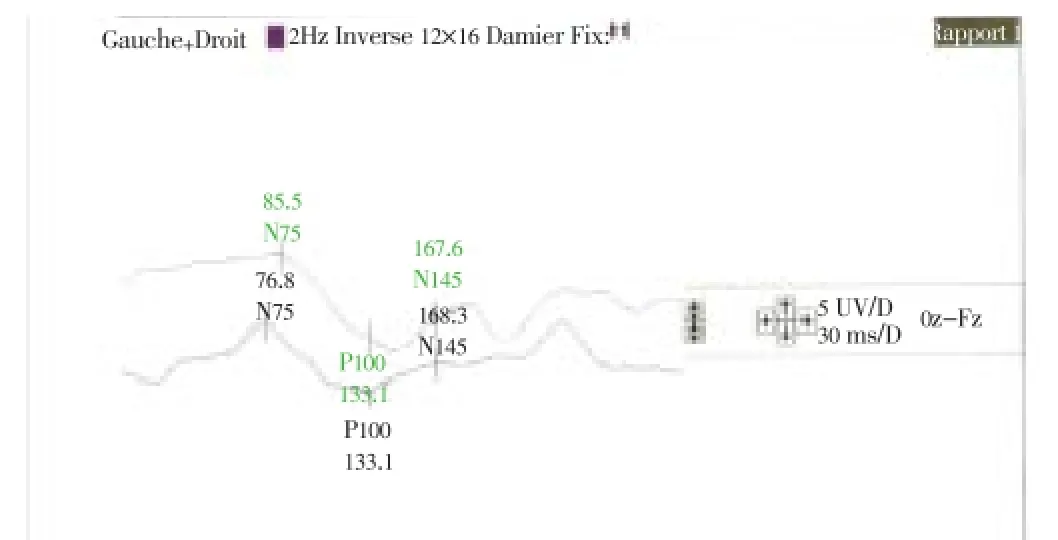
Figure 3.Flash visual evoked potentials showing low amplitude in the right eye and delay in the P100 latency in both eyes corresponding to inflammatory optic neuritis.
A diagnosis of ON and scleritis related to rickettial infection was made on the basis of clinical, immunological and serological findings and the patient reported also an eschar on the scalp one month ago. The patient was treated with oral doxycycline (200 mg/d) for 15 d and corticosteroids (1 mg/kg/d) for 4 weeks in a tapering regimen. Two weeks after the initiation of treatment, the patient reported a marked improvement of vision which was confirmed by ophthalmologic examination (VA 8/10 in the left eye and 5/10 in the right eye). Dilated fundoscopy revealed a swollen right optic disc. At the last follow-up in March 2014, ophthalmologic examination showed the same VA values and atrophic right papillae.
3. Discussion
ON is closely linked to multiple sclerosis. However, it may be associated to a range of autoimmune or infectious diseases. ON due to infectious diseases is rare, since neuroretinitis is considered as the most ocular manifestation in eye infections[3]. Ocular involvement in rickettsial disease is uncommon and usually underdiagnosed. Rickettsial organisms are transmitted to peopleby insects (ticks and mites) and cause diseases such as typhus, the spotted fevers, and scrub typhus[2]. Rickettsiae are small, non flagellate, Gram-negative coccobacilli adapted to obligate intracellular parasitism[4]. Depending on the type of disease, four Rickettsiaceae groups are distinguished: scrub typhus (Orientia tsutsugamushi), spotted fever (Rickettsia rickettsii,Rickettsia akari, andR. conorii), typhus group (Rickettsia prowazekii, Rickettsia typhi) and miscellaneous (Ehrlichia,Anaplasma,Rickettsia slovaca)[4]. After entering human host, these microorganisms invade their target cells which are vascular endothelium and reticuloendothelial causing vasculitis which is responsible for skin rash, microvascular leakage, edema, tissue hypoperfusion and end-organ ischemic injury. Formation of thrombi can lead to tissue infarction and hemorrhagic necrosis[4]. Spotted fever group rickettsioses induce systemic infection, its symptomatology usually nonspecific and mimic other etiologies like viral or autoimmune diseases, making diagnosis more difficult, as in our patient. Fever, headache, neurological disturbances, and skin rash are the major symptoms[2]. The rickettsial infection may involve any parts of the eye mainly the back segment: retinitis with or without mild or moderate vitritis is the most common clinical finding. Typically, it presents in the form of white retinal lesions adjacent to retinal vessels and variable in number, size and location. In this situation, other infectious entities should be considered in differential diagnosis as toxoplasmosis[5]. Retinal vascular lesions in rickettsial disease may also include focal or diffuse vascular sheathing, vascular leakage, retinal hemorrhages, and retinal vascular occlusions, including branch retinal artery occlusion and branch retinal vein occlusion or subocclusion, leading to retinal neovascularization and vitreous hemorrhage[6]. Optic nerve involvement has been observed including optic disc edema, optic disc staining on fluorescein angiography, and optic neuritis with reversible visual loss[7]. Cystoid macular oedema, serous retinal detachment, hypofluorescent choroidal spots, conjunctival hemorrhage, and uveitis, have also been reported in affected individuals[6].
Diagnosis of rickettsial infection is usually based on serology in conjunction with the clinical presentation and epidemiological data (history of possible exposure to ticks, travel in endemic area, symptoms during summer months). Doxycycline has been recommended as the antibiotics of choice in rickettsial diseases[1]. In ocular involvement including severe retinitis, vitritis, retinal vascular occlusion or optic nerve systemic steroids, in association with doxycycline should be prescribed[5].
Our case report illustrates the difficulties in diagnosing the exact cause of optic neuritis when it is associated with multiple clinical and immunological disorders. The diagnosis of optic neuritis associated with primary Sjögren syndrome was evoked first, but ruled out by negative antinuclear antibody control and the absence of lymphocytic infiltration in the labial salivary glands. Other diagnosis including viral and bacterial infections having tropism for ocular involvement and autoimmune inflammatory vasculitis were also eliminated. The positive rickettsial serology, the epidemiologic context and the negativity of all investigations established the diagnosis of rickettsial infection. An association between corticosteroids and cyclines was prescribed with a partial improvement of visual acuity.
Rickettsioses should be considered in the diagnosis of acute optic neuritis in areas where Mediterranean spotted fever is endemic. Diagnosis must be also early to have a better response to treatment combining doxycycline and corticosteroids.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] Renvoisé A, Raoult D. [An update on rickettsiosis].Med Mal Infect2009;39(2): 71-81. French.
[2] Wood H, Artsob H. Spotted fever group rickettsiae: a brief review and a Canadian perspective.Zoonoses Public Health2012;59(Suppl 2): 65-79.
[3] de Seze J. Atypical forms of optic neuritis.Rev Neurol (Paris)2012;168(10): 697-701.
[4] Rathi N, Rathi A. Rickettsial infections: Indian perspective.Indian Pediatr2010;47(2): 157-164.
[5] El Matri L. Ocular manifestations of rickettsiosis: 2. Retinal involvement and treatment.Int J Med Sci2009;6(3): 128.
[6] Khairallah M, Kahloun R, Yahia SB, Jelliti B, Messaoud R. New infectious etiologies for posterior uveitis.Ophthalmic Res2013;49(2): 66-72.
[7] Khairallah M, Jelliti B, Jenzeri S. Emergent infectious uveitis.Middle East Afr J Ophtalmol2009;16(4): 225-238.
10.12980/APJTB.4.2014APJTB-2014-0359
*Corresponding author: Snoussi Mouna, Department of Internal Medicine, Hédi Chaker University Hospital, 3029 Sfax, Tunisia.
Tel: (+216) 99 27 47 43
E-mail: mounasnoussi23@yahoo.fr
Rickettsia conorii
Mediterranean spotted fever
Ocular involvement
 Asian Pacific Journal of Tropical Biomedicine2014年12期
Asian Pacific Journal of Tropical Biomedicine2014年12期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- Changing trends of cardiovascular risk factors among Indians: a review of emerging risks
- Seroprevalence of syphilis in patients attending a tertiary care hospital in Southern India
- Histopathological and molecular study of Neospora caninum infection in bovine aborted fetuses
- Genetic polymorphisms of GSTM1, GSTP1 and GSTT1 genes and lung cancer susceptibility in the Bangladeshi population
- Expression of p-PPARγ in the aging thoracic aorta of spontaneously hypertensive rat and inhibitory effect of rosiglitazone
- In vitro germination and propagation of a threatened medicinal orchid, Cymbidium aloifolium (L.) Sw. through artificial seed
