Seroprevalence of syphilis in patients attending a tertiary care hospital in Southern India
Sadia Khan, Godfred Antony Menezes, Rahul Dhodapkar, Belgode Narasimha Harish
1Department of Microbiology, Amrita Institute of Medical Sciences, Ponekara, Kochii-682041, Kerala, India
2College of Applied Medical Sciences, Ha’il University, Ha’il, Kingdom of Saudi Arabia
3Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
Seroprevalence of syphilis in patients attending a tertiary care hospital in Southern India
Sadia Khan1*, Godfred Antony Menezes2, Rahul Dhodapkar3, Belgode Narasimha Harish3
1Department of Microbiology, Amrita Institute of Medical Sciences, Ponekara, Kochii-682041, Kerala, India
2College of Applied Medical Sciences, Ha’il University, Ha’il, Kingdom of Saudi Arabia
3Department of Microbiology, Jawaharlal Institute of Postgraduate Medical Education and Research, Pondicherry, India
ARTICLE INFO
Article history:
Received 23 Sep 2014
Received in revised form 26 Sep 2014
Accepted 16 Oct 2014
Available online 22 Oct 2014
Syphilis seroprevalence
Objective:To report our experience with two tests, anti-cardiolipin antibody test [venereal disease reasearch laboratory (VDRL) test] and specific treponemal test (Treponema pallidumhemagglutination assay), used for screening antenatal, high risk cases and cases from sexually transmitted infection in a tertiary care hospital from January 2006 till December 2008.
1. Introduction
Syphilis, caused byTreponema pallidumis a classical example of a sexually transmitted disease (STD) that can be successfully controlled by effective public health measures due to the availability of a sound diagnostic test and effective and economical treatment options. The World Health Organization estimates that 10-12 million new infections of syphilis occur every year[1]. Infection rates show extreme variation between countries of the same region as well as various subcategories of populations studied[2-5]. Indian data on syphilis seroprevalence is meagre,with incidence rates ranging from 5.4 per 100 persons each year in a sexually transmitted infection clinic to prevalence of 21.9% in convenience samples of long distance truck drivers[6-8]. The present study was aimed at understanding the occurrence of syphilis among various patient groups attending a tertiary care hospital and studying the trends over a period of three years.
2. Materials and methods
The study was conducted in a tertiary care teaching hospital in Southern India from January 2006 till December 2008. A retrospective analysis of laboratory log book maintained for syphilis tests was performed for this period. A total of 14 639 samples were received from various patient groups including antenatal cases, patients attending STD clinic, blood donors and HIV positive patients.
Screening for syphilis was performed by venereal diseasereasearch laboratory (VDRL) test. Serum samples from all patients were tested by qualitative VDRL using standard procedures. Samples positive for VDRL were subjected to a quantitative VDRL test using serum dilutions from 1 in 2 upto 1 in 64. A specific treponemal test,Treponema pallidumhemagglutination assay (TPHA) was peformed on samples positive in the quantitative VDRL. Samples positive in both tests were designated as seropositive for syphilis.
Statistical analysis of data was done by using SPSS version 16. Results were summarized using descriptive statistics. Pearson’sChi-square test was used to evaluate differences between proportions.Chi-square for linear trends was calculated.
The study was approved by institute ethics committee.Patient information obtained during the study was kept confidential.
3. Results
Among the 14 639 samples collected, 103 were positive by VDRL test. Of these 89 were positive by quantitative VDRL and TPHA. The year wise distribution of these cases is shown in Table 1. The cumulative seroprevalence over three years was found to be 0.61% in this study. The syphilis seroprevalence reduced from 0.88% in 2006 to 0.40% in 2008, which was statistically significant (χ2=9.16,P=0.010 3).
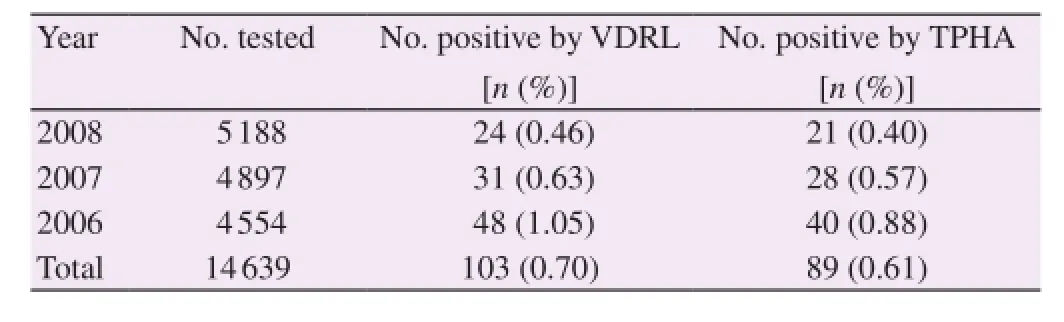
Table 1 Seroprevalence of syphilis infection from the study period January 2006 till December 2008.
Among the various sub-populations study, patients attending the sexually transmitted infection clinic showed a seroprevalence of 2.62% (Table 2). The seroprevalence decreased significantly from 4% in 2006 to 1.39% in 2008 (χ2=12.543 3,P=0.001 9). The antenatal group showed a seroprevalence of 0.12% (χ2=1.07,P=0.58) whereas congenital syphilis was seen in 0.61% of pediatric age group tested. Among the HIV positive individuals screened for syphilis, 6.5% were positive for treponemal antibodies (Table 3). None of the blood donors were positive for syphilis. Miscellaneous groups of patients admitted to other broad specialities with features suggestive of secondary or tertiary syphilis were also screened. The seropositivity in this group was 2.11%.
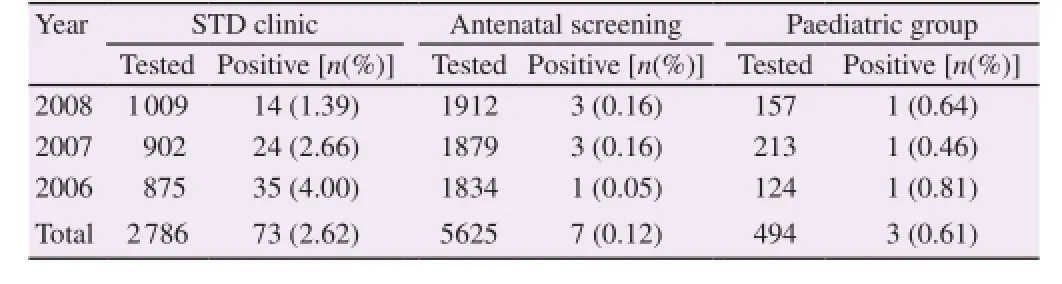
Table 2 Seroprevalence of syphilis among patients attending STD clinic, antenatal screening and pediatric age group.
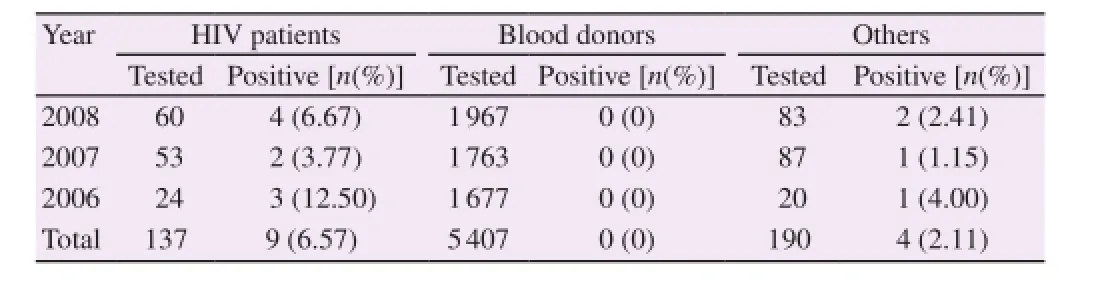
Table 3 Seroprevalence of syphilis among HIV patients screened, blood donors and other patients screened for syphilis.
4. Discussion
The present study was determined the seroprevalence of syphilis in patients attending a tertiary care centre and studied short term trends in changing rates of syphilis in various subgroups of patients. Various studies from India have shown varied rates of syphilis depending upon the population study. Studies from STD clinics have shown seroprevalence ranging from 5.4% to 8.2%[8,9]. Our study showed a statistically significant declining rate of syphilis in STD clinics as well as the overall seroprevalence. These findings could be interpreted as indicators of improved programmes for prevention and management of STDs as well as availability of treatment in STD clinics[9].
Indian studies on syphilis from antenatal groups has shown a seroprevalence of 0.84% to 0.98%[10,11]. Low seroprevalence of 0.12% was also seen in the current study. However, as syphilis can cause adverse outcomes of pregnancy in 80% of the cases, including stillbirths, abortions, perinatal death and neonatal infections in a significant number of cases, the importance of screening antenatal women for syphilis should always be highlighted[12].
Co-infection rates of syphilis and HIV have been showing a worrisome trend in several countries, with urban outbreaks in men who have sex with men showing rates of 20%-73%[13]. In India, variable syphilis-HIV coinfection rates have been described[14]. Eventhough our study shows that 6.5% of diagnosed HIV patients were positive for syphilis, the results have to be interpreted with caution. The HIV positive individuals included in our study were symptomatic individuals who had presented to clinic for antiretroviral treatment. Therefore, all HIV positive individuals were not screened in the study unlike other studies which have screened large HIV positive cohorts. Syphilis and HIV co-infection presents a complex interaction. The increased incidence of HIV in homosexual and heterosexual individuals afflicted with STD, including syphilis is epidemiologically documented in numerous studies[15,16]. HIV alters the course of syphilis as well as the response to treatment. Incidence of neurosyphilis in HIV infected individuals is high even when treated with recommended dosage[17]. Altered serological responses in HIV positive patients also underlines the need for treponemal tests in this patient group. The need for further studies in this areashould be overemphasized.
Our study had several limitations. Its retrospective nature limited evaluation of several parameters like risk evaluation of particular groups such as men who have sex with men, rural and urban population,etc. Secondly, it was a hospital based study and population-based community studies are likely to show different results. Finally, the study looked into short term trends ranging over a period of 3 years. Long term evaluation of these trends will undoubtedly yield more epidemiological data. Nevertheless, findings of this study can help us understand the disease trends at a larger scale.
Eventhough the prevalence of syphilis is on the decline, screen of high risk populations should be continued to avoid the complications of undiagnosed and untreated syphilis.
Conflict of interest statement
We declare that we have no conflict of interest.
[1] World Health Organization, Department of HIV/AIDS.Global prevalence and incidence of selected curable sexually transmitted diseases: overview and estimates. Geneva: World Health Organization; 2001.
[2] Olokoba AB, Olokoba LB, Salawu FK, Danburam A, Desalu OO, Badung LH, et al. Syphilis in voluntary blood donors in Northeastern Nigeria.Eur J Sci Res2009;31(3): 335-340.
[3] Baião AM, Kupek E, Petry A. Syphilis seroprevalence estimates of Santa Catarina blood donors in 2010.Rev Soc Bras Med Trop2014;47(2): 179-185.
[4] Eyaufe AA, Osagie RN, Isibor JO, Okwu GI, Oriakhi RE, Turay AA. Performance of syphilis serology in students of Ambrose Alli University, Ekpoma, Nigeria.Int J Med Med Sci2009;1(4): 138-139.
[5] Tankhiwale SS, Naikwade SR. Seroprevalence of syphilis and biologically false positive cases in a tertiary care center.Indian J Dermatol Venereol Leprol2014;80(4): 340-341.
[6] Gawande AV, Vasudeo ND, Zodpey SP, Khandait DW. Sexually transmitted infections in long distance truck drivers.J Commun Dis2000;32(3): 212-215.
[7] Bala M, Singh V, Muralidhar S, Ramesh V. Assessment of reactivity of three treponemal tests in non-treponemal non-reactive cases from sexually transmitted diseases clinic, antenatal clinic, integrated counselling and testing centre, other different outdoor patient departments/indoor patients of a tertiary care centre and peripheral health clinic attendees.Indian J Med Microbiol2013;31(3): 275-279.
[8] Schneider JA, Lakshmi V, Dandona R, Kumar GA, Sudha T, Dandona L. Population-based seroprevalence of HSV-2 and syphilis in Andhra Pradesh State of India.BMC Infect Dis2010; 10: 59.
[9] Maity S, Bhunia SC, Biswas S, Saha MK. Syphilis seroprevalence among patients attending a sexually transmitted disease clinic in West Bengal, India.Jpn J Infect Dis2011;64(6): 506-508.
[10] Archana BR, Prasad SR, Beena PM, Okade R, Sheela SR, Beeregowda YC. Maternal and congenital syphilis in Karnataka, India.Southeast Asian J Trop Med Public Health2014;45(2): 430-434.
[11] Mehta KD, Antala S, Mistry M, Goswami Y. Seropositivity of hepatitis B, hepatitis C, syphilis, and HIV in antenatal women in India.J Infect Dev Ctries2013;7(11): 832-837.
[12] World Health Organization, Department of Reproductive Health and Research.The global elimination of congenital syphilis: rationale and strategy for action. Geneva: World Health Organization; 2007.
[13] Patton ME, Su JR, Nelson R, Weinstock H, Centers for Disease Control and Prevention (CDC). Primary and secondary syphilis-United States, 2005-2013.MMWR Morb Mortal Wkly Rep2014;63(18): 402-406.
[14] Shaw SY, Deering KN, Reza-Paul S, Isac S, Ramesh BM, Washington R, et al. Prevalence of HIV and sexually transmitted infections among clients of female sex workers in Karnataka, India: a cross-sectional study.BMC Public Health2011;11(Suppl 6): S4.
[15] Ross MW, Nyoni J, Ahaneku HO, Mbwambo J, McClelland RS, McCurdy SA. High HIV seroprevalence, rectal STIs and risky sexual behaviour in men who have sex with men in Dar es Salaam and Tanga, Tanzania.BMJ Open2014;4(8): e006175.
[16] Schmidt AJ, Marcus U. Self-reported history of sexually transmissible infections (STIs) and STI-related utilization of the German health care system by men who have sex with men: data from a large convenience sample.BMC Infect Dis2011;11: 132.
[17] Tsai HC, Sy CL, Lee SS, Wann SR, Chen YS. Optimal treatment for asymptomatic neurosyphilis. Int J STD AIDS2012;23(10): 756-757.
10.12980/APJTB.4.201414B413
*Corresponding author: Dr. Sadia Khan, MD, Clinical Assistant Professor, Department of Microbiology, Amrita Institute of Medical Sciences, Ponekara, Kochii-682041, Kerala, India.
Tel: +91484-2801234 (Extn: 8119)
Fax: +91484-2802020
E-mail: drsadiakhan83@gmail.com
STD
VDRL
Methods:A total of 14 639 samples received from various patient groups including antenatal cases, patients attending sexually transmitted disease (STD) clinic, blood donors and HIV positive patients were screened.
Results:Among the 14 639 samples collected, 103 were positive by VDRL test. Of these 89 cases were confirmed by quantitative VDRL test andTreponema pallidumhemagglutination assay. The cumulative seroprevalence over two years was found to be 0.61% in this study. The syphilis seroprevalence reduced from 0.88% in 2006 to 0.40% in 2008. Among the various sub-populations studied, patients attending the sexually transmitted infection clinic showed a seroprevalence of 2.62%. The seroprevalence decreased significantly from 4.00% in 2006 to 1.39% in 2008.
Conclusions:Our study showed a statistically significant declining rate of syphilis in STD clinics as well as the overall seroprevalence. These findings could be interpreted as indicators of improved programmes for prevention and management of STDs.
 Asian Pacific Journal of Tropical Biomedicine2014年12期
Asian Pacific Journal of Tropical Biomedicine2014年12期
- Asian Pacific Journal of Tropical Biomedicine的其它文章
- Changing trends of cardiovascular risk factors among Indians: a review of emerging risks
- An unusual cause of optic neuritis: rickettsiosis disease
- Histopathological and molecular study of Neospora caninum infection in bovine aborted fetuses
- Genetic polymorphisms of GSTM1, GSTP1 and GSTT1 genes and lung cancer susceptibility in the Bangladeshi population
- Expression of p-PPARγ in the aging thoracic aorta of spontaneously hypertensive rat and inhibitory effect of rosiglitazone
- In vitro germination and propagation of a threatened medicinal orchid, Cymbidium aloifolium (L.) Sw. through artificial seed
