Verification of the Tokyo guidelines for acute cholangitis secondary to benign and malignant biliary obstruction: experience from a Chinese tertiary hospital
Beijing, China
Verification of the Tokyo guidelines for acute cholangitis secondary to benign and malignant biliary obstruction: experience from a Chinese tertiary hospital
Gang Sun, Lu Han, Yun-Sheng Yang, En-Qiang Linghu, Wen Li, Feng-Chun Cai, Jin-Yan Kong, Xiang-Dong Wang, Jiang-Yun Meng, Hong Du, Hong-Bin Wang, Qi-Yang Huang, Quratulain Hyder and Xiu-Li Zhang
Beijing, China
BACKGROUND:The lack of widely-accepted guidelines for acute cholangitis largely lags behind the progress in medical and surgical technology and science for the management of acute cholangitis. This study aimed to verify the Tokyo guidelines for the management of acute cholangitis and cholecystitis of 2007 edition (TG07) in patients with obstructive cholangitis due to benign and malignant diseases.
METHODS:The patients were retrieved from our existing ERCP database. Final diagnosis of acute cholangitis was made by detecting purulent bile during biliary drainage. We examined and compared the guidelines concerning benign and malignant obstruction.
RESULTS:In 120 patients in our study, 82 and 38 had benign and malignant biliary obstruction, respectively. Guidelines based diagnosis was made in 68 (82.9%), 36 (94.7%), and 104 (86.7%) patients with benign, malignant, and overall biliary obstruction, respectively, which were significantly higher than 44 (53.7%), 17 (44.7%), and 61 (50.8%) diagnosed by Charcot's triad (P<0.001). Treatment consistent with the guidelines was offered to 58 (70.7%) patients with benign obstruction and15 (39.5%) patients with malignant obstruction (P=0.001). No significant association was observed between clinical compliance, guidelines-based severity grades and clinical outcomes. In the multivariate model, intrahepatic obstruction (OR=11.2, 95% CI: 1.55-226.9) and hypoalbuminemia (≤25.0 g/L; OR=17.3, 95% CI: 3.5-313.6) were independent risk factors for a 30-day mortality.
CONCLUSIONS:The TG07 are more reliable than Charcot's triad for the diagnosis of acute cholangitis albeit with limited prognostic values. Intrahepatic obstruction and hypoalbuminemia are new predictors of poor prognosis and need further assessment.
(Hepatobiliary Pancreat Dis Int 2013;12:400-407)
acute cholangitis;the Tokyo guidelines; endoscopic biliary drainage; diagnosis
Introduction
Acute cholangitis (AC) is a bacterial infection of the biliary tract. The spectrum of its severity ranges from mild to life-threatening with mortality rates between 8% and 10%.[1,2]Choledocholithiasis has been the leading cause of AC.[3,4]However, underlying malignancies of the bile duct, the pancreas and liver are seen with increasing frequency in the past two decades.[5-7]
Although right upper quadrant abdominal pain, fever and jaundice (i.e. Charcot's triad, 1877[8]) with or without mental confusion and hypotension (i.e. Reynolds' pentad, 1959[9]) are still used as the clinicalparameters to diagnose AC, the full complement of the signs and symptoms remains elusive in planning further management.[10]Several scoring systems have been devised for the diagnosis and severity grading of AC,[11-13]but the standard guidelines for clinical practice virtually do not exist, lagging behind the progress in medical and surgical technology.[14]
The Tokyo guidelines for the management of acute cholangitis and cholecystitis, formulated in 2007 (TG07) for the diagnosis, severity assessment, and treatment of AC,[15]aimed to be accommodated in clinical practice based on worldwide expert consensus. However, minimal recognition of the TG07 has been achieved outside Japan.[16-20]Several retrospective studies[16,17,20]have validated its diagnostic value in comparison with Charcot's triad albeit with little agreement on the criteria for severity assessment and treatment strategy. For example, the TG07 require 24-hour observation of patients to differentiate between mild and moderate AC. This is practically inapplicable if an urgent intervention is performed aiming to prevent progression of sepsis.[20]There are no potential benefits on applying the TG07 in the treatment of AC. Moreover, the application of the guidelines has been mostly examined in AC patients due to choledocholithiasis with minimal reference to malignant etiology, thereby reinforcing the need for a continuous update.[18,21]The present study includes patients with benign as well as malignant biliary obstruction to verify the TG07 with the intent to provide evidences for further optimization.
Methods
This study was approved by the institutional review board of the Chinese PLA General Hospital. Clinical information between January 2000 and December 2009 was collected from our prospectively established endoscopic retrograde cholangiopancreatography (ERCP) database. The inclusion criterion was identification of purulent bile during endoscopic biliary drainage. The patients <18 years of age and those with prior biliary drainage after onset were excluded from the study. For patients with multiple hospitalizations during the study period, only the initial episode was reviewed.
Patient management
The initial diagnosis in the majority of our hospitalized patients was made on Charcot's triad. Upon admission, the patients were fasted and hematologic and radiologic evaluations were carried out for evidence of biliary obstruction and acute infection. Their vital signs and urinary output were monitored 6 hourly. Blood counts, blood cultures, hepatic and renal function tests, along with urinary biochemistry including glucose and amylase levels were estimated on admission and regularly thereafter. Abdominal ultrasonography was routinely performed within 12 hours, while plain or enhanced computed tomography (CT) and magnetic resonance cholangiopancreatography (MRCP) were chosen appropriately according to the clinical necessity and the patient's tolerance. Intravenous fluid with broad-spectrum antibiotics was given immediately and a central venous line was established in case of hypotension or in shock.
In our institution, emergent endoscopic drainage within 24 hours of admission is recommended to any AC patients once the causes and site of obstruction are identified, regardless of etiology and severity of diseases. A waiting period of 24 to 48 hours is permitted for pretreatment assessment in complicated cases and an immediate endoscopic drainage will be performed in those who present signs of worsening illness. Therapeutic ERCP was performed under conscious sedation with propofol. Commonly, procedures were done in a prompt fashion to avoid unanticipated worsening of sepsis due to prolonged manipulation. In our institution, the high risk patients, as defined by advanced age ≥75 years, hypotension with a systolic blood pressure of <90 mmHg, peritonism, altered sensorium, and associated renal failure are deemed to urgent biliary decompression either by stents placement or by nasobiliary drainage. The definitive management would be undertaken until cholangitis subsided. The selection of drainage modality is merely based on the site of obstruction and sufficiency of cholangiography. For definite extrahepatic obstruction, a 10-Fr plastic straight flap stent is preferred, while a short-term use of 7-Fr nasobiliary catheter will be considered in complicated cases either with intrahepatic obstruction or inadequate cholangiography due to hemodynamically unstable status. Multiple ERCP sessions were also needed for those who had residual bile duct stones and undrained segments. Intensive postoperative observation was continued for ERCP-related complications. ERCP was deemed successful if it resulted in complete and effective relief of biliary obstruction, regardless of the final clinical outcomes. Ultrasound-guided percutaneous transhepatic biliary drainage or surgery was used as the alternate modalities if ERCP was non-rewarding. Hospital stay was defined as the time period from admission of a patient to his/her exit from the hospital. Given the different etiologies in our patient cohort, death of the patient within 30 days of admission was regarded as the clinical endpoint.
Re-validation of the TG07
The data on demography, presenting features, diagnostic evaluation of patients, and clinical outcomes were retrieved and summarized to compare between AC patients due to benign and malignant biliary obstruction. The TG07 for AC were re-examined in depth with a special reference to:
1) The diagnostic yield of the TG07 in comparison with Charcot's triad. Table 1 shows the TG07 for AC,[15]including three components (A, B, and C) and seven subcategorized items; by which a definite diagnosis is made either by Charcot's triad or by addition of positive findings in both laboratory (component B) and imaging (component C) data in suspected patients.
2) Clinical compliance with the TG07. In terms of severity assessment of AC, there are three severity grades with respective treatment as follows: grade I (i.e. favorable response to antibiotics; elective biliary drainage); grade II (i.e. failure of conservative treatment; biliary drainage within 24 hours); grade III (i.e. progression to organ dysfunction; biliary drainage within 12 hours).[15]In the present study, patients were classified into consistent and inconsistent groups based on whether complied with the timing of biliary drainage recommended by the TG07.
3) The impact of severity grades and clinical compliance on the clinical outcomes.
4) The identification of potential risk factors predicting the mortality.
Statistical analysis
The Chi-square test and Student'sttest/Wilcoxon's rank-sum test were applied to determine the categorical data and continuous variables, respectively. JMP package 9.0 (SAS Institute Inc., Cary, NC, USA) was used for all statistical analyses. The risk factors were analyzed by univariate and multivariate (stepwise) logistic regression tests. APvalue of <0.05 was considered statistically significant.
Results
Of the 120 AC patients, 83 (69.2%) were male (age 66.0 ± 15.1 years). The patients were divided into two groups on the basis of etiology of AC: 82 (68.3%) in the benign group and 38 (31.7%) in the malignant group. In terms of the characteristics such as age, gender, comorbidity and changes in vital signs, no significant difference was observed in both groups (Table 2). Typical Charcot's triad and Reynolds' pentad occurred in 61 (50.8%) and 12 (10.0%) of our patients, respectively, with a similar incidence between the two groups (P=0.36). The patients with acute biliary pancreatitis were observedonly in the benign group (P<0.05). The total white blood cell count, polymorphonuclear neutrophil count and C-reactive protein (CRP) level were identical in both groups (P>0.05). The platelet count was higher in the malignant group. The levels of total bilirubin, direct bilirubin and alkaline phosphatase (ALP) were also significantly higher in the malignant group than in the benign group (P<0.05). However, alanine aminotransferase (ALT) was lower in the malignant group than in the benign group (94.6±21.6 vs 164.6± 15.0 U/L,P=0.01).
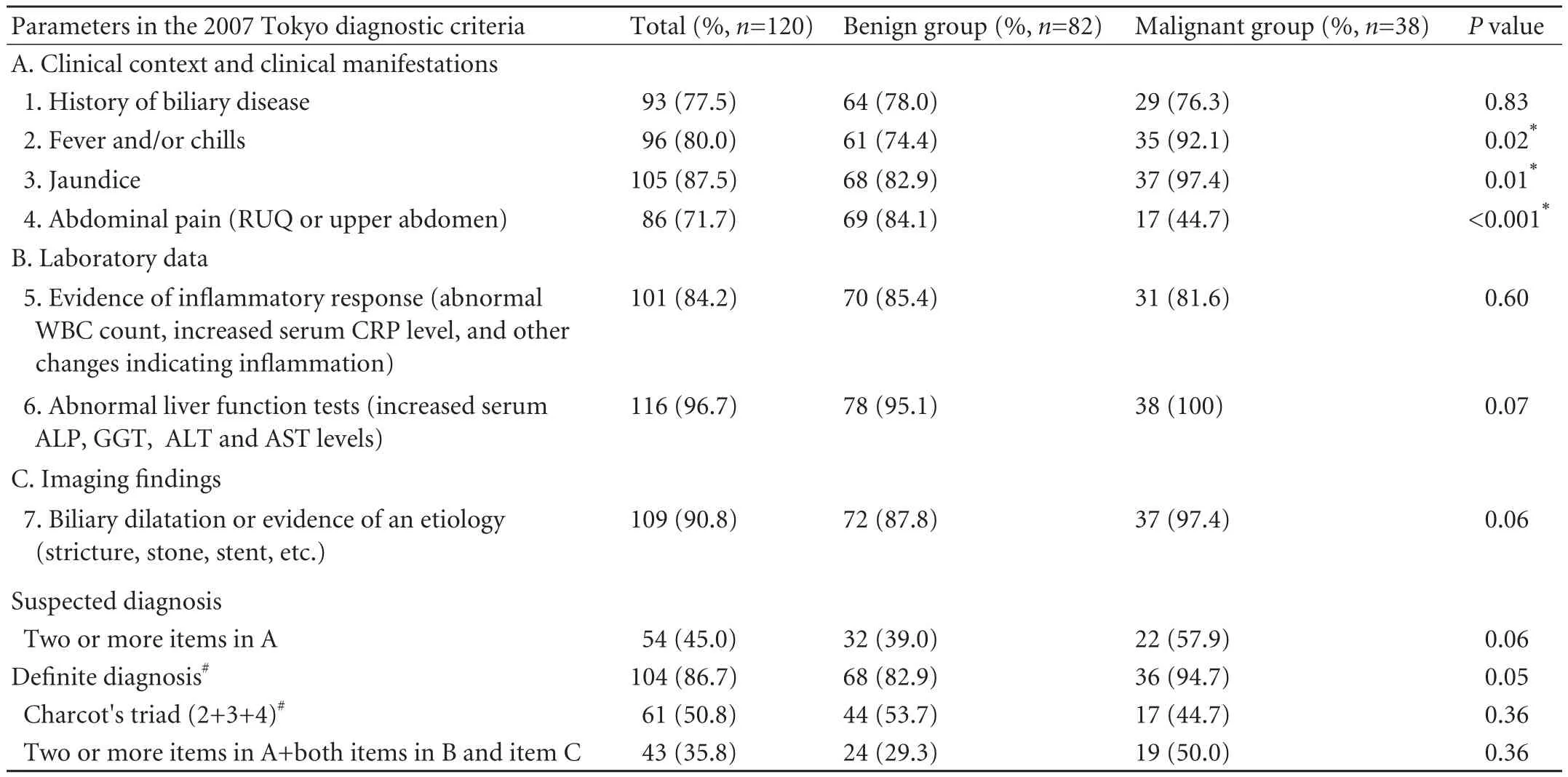
Table 1.Performance of the diagnostic criteria of the TG07 in benign and malignant biliary obstruction

Table 2.Baseline characteristics of patients with acute cholangitis

Table 3.Etiology and site of biliary obstruction
Malignant AC resulted from cholangiocarcinoma, periampullary carcinoma, pancreatic cancer, and metastatic liver disease in 22 (57.9%), 5 (13.2%), 8 (21.1%), and 3 (7.9%) patients, respectively (Table 3). Bile duct stones accounted for 90.2% (74/82) of the patients with benign AC. Intrahepatic biliary obstruction was caused more frequently by malignancies (55.3%, 21/38) than by benign conditions (13.4%, 11/82) (P<0.001).
Endoscopic biliary drainage as the first line treatment was successful in 105 (87.5%) of the patients with no serious procedure-related complications such as perforation and severe pancreatitis. However, mild to moderate post-ERCP complications were recorded in 12 (10.0%) patients: acute pancreatitis in 8 (6.7%), and bleeding from sphincterotomy in 4 (3.3%). No significant difference in the complication rate was observed between the two groups (P=0.89). Alternative modalities were successful in 10 (8.3%) patients: percutaneous transhepatic biliary drainage in 2 (1.7%), and surgical drainage in 8 (6.7%). Six (5.0%) of our patients died early of refractory biliary infection (5, 4.2%) and cerebral hemorrhage (1, 0.8%), including the malignant group 5 (13.2%) and the benign group 1 (1.2%) (P=0.007).
Based on the diagnostic criteria contained in TG07 for AC (Table 1), the definite diagnosis of AC was achieved in 68 (82.9%), 36 (94.7%), and 104 (86.7%) benign, malignant, and overall patients, respectively, which were significantly higher than 44 (53.7%),17 (44.7%), and 61(50.8%), diagnosed by Charcot's triad (P<0.001 for each pair comparison). Although the diagnostic rate for malignant patients was higher than that for benign patients numerically, the difference did not reach a statistical significance (P=0.05). Sixteen (13.3%) patients were misinterpreted by the TG07: 14 (11.7%) in the benign group and 2 (1.7%) in the malignant group (P=0.05). In the benign patients, 3 patients only met 1 item in component A; none of the remaining 11 patients with suspected diagnosis could satisfy both component B and C necessary to establish a definite diagnosis. Two malignant patients were suspected but were precluded for a definite diagnosis due to the absence of evidence of inflammatory response (item 5) in component B.
The numerical distribution of severity grades in our patients revealed: grade I 27 patients (22.5%), grade II 68 (56.7%), and grade III 25 (20.8%). There were totally 73 (60.8%) consistent patients, in which the benign patients (58/82, 70.7%) were treated more frequently in accordance with the Tokyo guidelines than the malignant patients (15/38; 39.5%) (P<0.001). Such a difference was predominately seen in grade I and II patients, but with an inverse trend (Fig.). No significant difference in the clinical outcome was observed among patients of different severity grades (P>0.05; Table 4) and between consistent and inconsistent categories (P>0.05; Table 5).
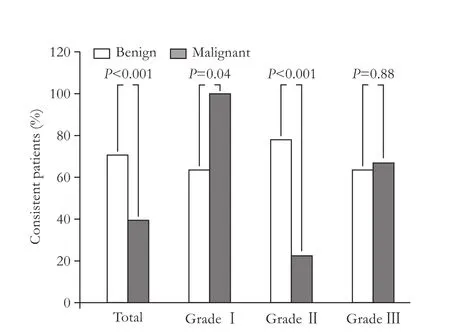
Fig.Clinical compliance with the TG07 for the treatment of acute cholangitis. Benign patients were more likely to comply with the TG07 than malignant patients, with an inverse trend in grade I and II classification.
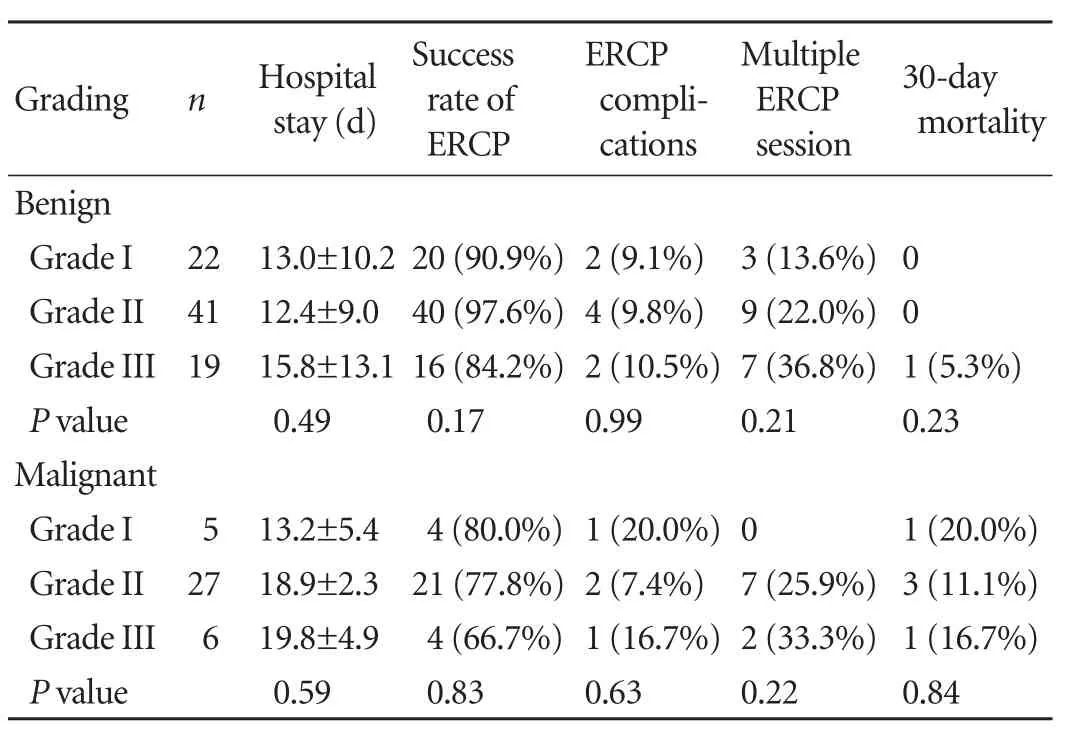
Table 4.Impact of the severity assessment criteria of the TG07 on the clinical outcomes
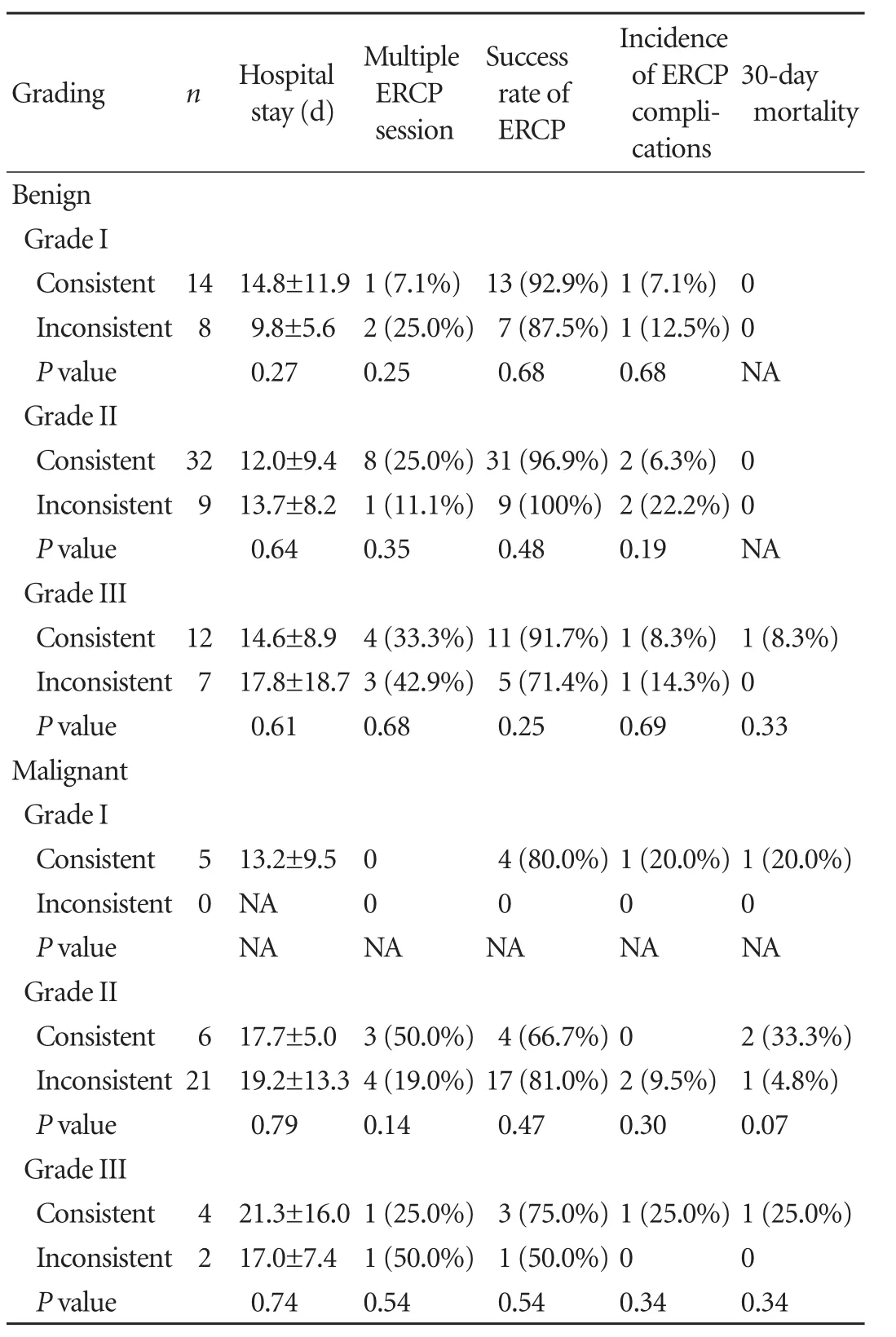
Table 5.Impact of clinical compliance with the TG07 on the clinical outcomes
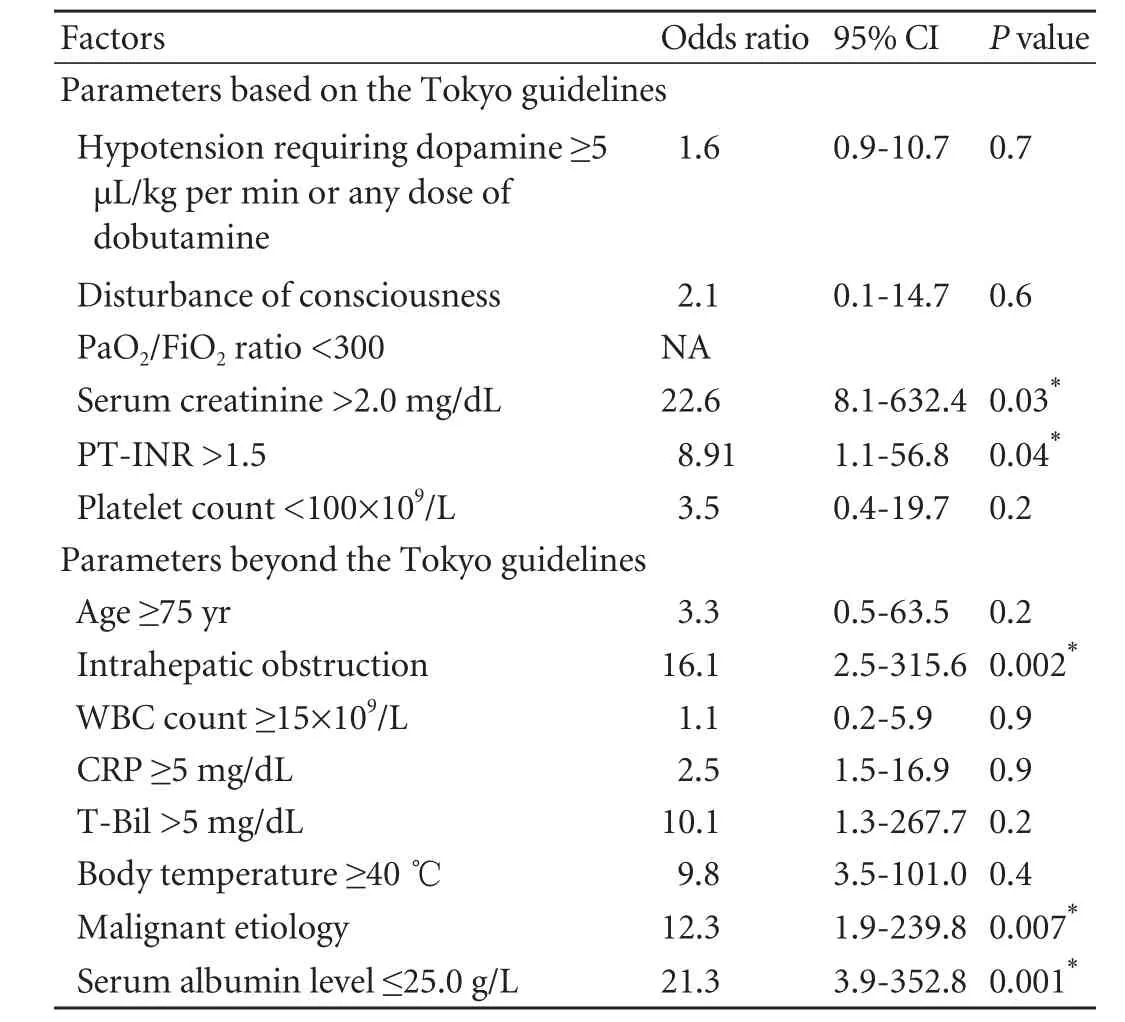
Table 6.Univariate analysis of risk factors predicting a 30-day mortality
A total of 14 prognostic variables for a 30-day mortality were analyzed: 6 variables for organ dysfunction in severity grade III;[15]8 variables predicting mortality or urgent biliary drainage in previously published studies.[5,18,22,23]Univariate analysis revealed that serum creatinine >2.0 mg/dL, PT-INR>1.5, intrahepatic biliary obstruction, malignant etiology and serum albumin level≤25.0 g/L were significantly associated with a 30-day mortality (Table 6). In a multivariate regression model, intrahepatic biliary obstruction (OR=11.2, 95% CI: 1.55-226.9;P=0.007) and serum albumin level ≤25.0 g/L (OR=17.3, 95% CI: 3.5-313.6;P<0.001) were independent risk factors for a 30-day mortality in the present series.
Discussion
The present study tries to reinforce the concept that the diagnosis of AC due to benign or malignant biliary obstruction can be achieved more accurately by application of the TG07 as compared with Charcot's triad. However, irrespective of the underlying etiology, the TG07 severity grading appears to have no significant impact on the clinical outcome in AC. We have also observed that intrahepatic biliary obstruction and hypoalbuminemia (≤25.0 g/L) are independent risk factors for AC related mortality.
The diagnostic value of the TG07 has been previously demonstrated in studies from Japan with sensitivity rates between 63.9%-94% in comparison with <40% by Charcot's triad.[16,18,20]Our results are in conformity with these reports. Of note, approximately 95% of our patients in the malignant group were positive for the TG07 diagnostic criteria. This observation apparently has important implications such as early diagnosis and timely treatment of these high risk patients. The current guidelines are superior to the conventional guidelines primarily based on clinical symptoms due to incorporation of Charcot's triad as one of the diagnostic criteria for AC, and patients without full complement of Charcot's triad can still be identified if the abnormalities are demonstrated in both laboratory data and image findings. However, some confounding factors may affect the diagnostic potential of these guidelines in AC. For examples, decompensate liver cirrhosis and hypersplenism are responsible for normal peripheral blood counts in AC in these cases. Urgent ultrasonography for detection biliary obstruction is somewhat experience-dependent and can be falsely negative in some other subjects. Therefore, an early identification of these confounding factors may facilitate modification of the current diagnostic criteria. Redefining leukocytosis in subjects with hypersplenism/ hematopoietic abnormality and the use of enhanced CT or MRCP in suspected cases with negative sonography may improve the reliability of the TG07.
The TG07 define the severity of AC on the basis of clinical response to antibiotics within 24 hours and the onset of organ dysfunction.[15]However, controversies exist over these consensus-based criteria. The differentiation between mild and moderate AC may be difficult while conducting biliary drainage within 24 hours.[20]The physicians remain cautious about the 24-hour time period for observation lest the delay in endoscopic intervention results in progression of sepsis.[20,21]Moreover, no predictive and prognostic values of the TG07 severity criteria were observed in our study, which might partially reflect the insufficiency of the TG07 in evaluation of the actual status of AC. On the other hand, the widespread use of early biliary drainage in our patients presumably played an important protective role, attenuating the prognostic values of the TG07. Nevertheless, two independent risk factors for 30-day mortality were identified, i.e. intrahepatic obstruction and hypoalbuminemia (≤25.0 g/L). Similar observations were also reported by other researchers. Using the TG07, Tsuyuguchi et al[19]have revealed significant association of hypoalbuminemia (≤25.0 g/L) with refractoriness of AC. Nishino et al[21]have identified four independent predictors of urgent ERCP in univariate analysis and by addition of organ dysfunction index, they have also devised a severity scoring system for AC, yielding a sensitivity of 87.5% and a specificity of 95.8%, respectively in predicting theneed for urgent ERCP. These controversies of the TG07 have obliged the scientists to revise and optimize the TG07. In the new revised guidelines 2013 (TG13), the item about clinical response to conservative treatment in the first 24-hour has been omitted and new clinical and laboratory parameters are added.[18]The revised version seems more practical although there is an obvious need to validate the efficacy and reliability of the added features.
In the TG07, timing of the biliary drainage is determined by severity grades of AC, i.e. with more severe illness, an earlier drainage is recommended and vice versa. Tsuyuguchi et al[19]investigated this strategy with the conclusion that the overall AC-related mortality was 4.2%: being 20%, 2.3% and 0% in severe, moderate and mild AC, respectively. However, the clinical outcome remains unclear with this strategy because no control group was used in this report. This limitation had actually obliged us to place our patients in consistent and inconsistent subgroups. The protocol at our facility is to perform early biliary drainage irrespective of the etiology and severity grade of AC. This strategy is supported by the present study with adherence to the TG07 showing no impacts on clinical outcome of our cohort. A low 30-day mortality of 5% and a morbidity of 10% at 10-year time span further augment our therapeutic approach, which is apparently inconsistent with the Tokyo guidelines. Further investigations with better study design especially randomized controlled trials are required to address this issue.
With regard to certain limitations, there is selection bias due to retrospective nature of the present study, which was carried out exclusively on hospitalized cases in a single center. Moreover, AC might be diagnosed when (i) presence of purulent bile, (ii) symptoms relief by biliary decompression; or (iii) remission achieved by antibiotics alone as defined by Kiriyama et al.[18]Our inclusion criteria of considering only the patients with purulent bile on ERCP might have been inadvertently missed some atypical cases and may lead to a higher sensitivity and a lower specificity. The inclusion of outpatients and control group, and recruitment of AC patients using new standards would have further strengthened our observations through a broader evaluation.
In summary, this is the first study to verify the application of the TG07 for diagnosis and treatment of AC in Chinese patients. We, therefore, support and recommend the TG07 based on their feasibility and reliability in comparison with Charcot's triad in the diagnosis of AC. However, the TG07 are insufficient and less practical in predicting grade of severity and clinical outcome in these patients. The latest 2013 edition of the Tokyo guidelines for AC has been recently proposed with updated items in many aspects compared to the former edition, but limited data available at the present time. We are in the process of conducting new studies with better study design to validate its potential advantages.
Contributors:YYS proposed the study. SG, LEQ, LW, CFC, HQY and ZXL performed ERCP procedures. SG and HL collected, analyzed the data and wrote the first draft. SG and HL contributed equally to this study. HQ analyzed the data and revised the manuscript. All authors contributed to the design and interpretation of the study and to further drafts. YYS is the guarantor.
Funding:None.
Ethical approval:This study was approved by the institutional review board of the Chinese PLA General Hospital.
Competing interest:No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
1 Lai EC, Mok FP, Tan ES, Lo CM, Fan ST, You KT, et al. Endoscopic biliary drainage for severe acute cholangitis. N Engl J Med 1992;326:1582-1586.
2 Leung JW, Chung SC, Sung JJ, Banez VP, Li AK. Urgent endoscopic drainage for acute suppurative cholangitis. Lancet 1989;1:1307-1309.
3 Friedman GD. Natural history of asymptomatic and symptomatic gallstones. Am J Surg 1993;165:399-404.
4 Beger HG, Schwarz A. Review article: Spectrum of biliary infections in the West and in the East. HPB Surg 1995;8:215-222.
5 Gigot JF, Leese T, Dereme T, Coutinho J, Castaing D, Bismuth H. Acute cholangitis. Multivariate analysis of risk factors. Ann Surg 1989;209:435-438.
6 Kumar R, Sharma BC, Singh J, Sarin SK. Endoscopic biliary drainage for severe acute cholangitis in biliary obstruction as a result of malignant and benign diseases. J Gastroenterol Hepatol 2004;19:994-997.
7 Thompson JE Jr, Tompkins RK, Longmire WP Jr. Factors in management of acute cholangitis. Ann Surg 1982;195:137-145.
8 Haubrich WS. Charcot of Charcot's triad. Gastroenterology 1998;115:541.
9 Reynolds BM, Dargan EL. Acute obstructive cholangitis; a distinct clinical syndrome. Ann Surg 1959;150:299-303.
10 Lee JG. Diagnosis and management of acute cholangitis. Nat Rev Gastroenterol Hepatol 2009;6:533-541.
11 Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, et al. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc 2005;62: 1-8.
对家长的干预包括:①肥胖相关知识讲座和健康教育手册发放;②运动干预:保证自身每日运动量不少于10 000步,同时监督儿童实现每日10 000步的目标;家长每周与儿童一起进行中等以上强度的运动一共不少于60 min。③合理安排与指导儿童膳食。
12 Zhang WZ, Chen YS, Wang JW, Chen XR. Early diagnosis and treatment of severe acute cholangitis. World J Gastroenterol 2002;8:150-152.
13 Williams EJ, Green J, Beckingham I, Parks R, Martin D, Lombard M, et al. Guidelines on the management of common bile duct stones (CBDS). Gut 2008;57:1004-1021.
14 Sekimoto M, Takada T, Kawarada Y, Nimura Y, Yoshida M, Mayumi T, et al. Need for criteria for the diagnosis and severity assessment of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg 2007;14:11-14.
15 Wada K, Takada T, Kawarada Y, Nimura Y, Miura F, Yoshida M, et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg 2007;14:52-58.
16 Yokoe M, Takada T, Mayumi T, Yoshida M, Hasegawa H, Norimizu S, et al. Accuracy of the Tokyo Guidelines for the diagnosis of acute cholangitis and cholecystitis taking into consideration the clinical practice pattern in Japan. J Hepatobiliary Pancreat Sci 2011;18:250-257.
17 Murata A, Matsuda S, Kuwabara K, Fujino Y, Kubo T, Fujimori K, et al. Evaluation of compliance with the Tokyo Guidelines for the management of acute cholangitis based on the Japanese administrative database associated with the Diagnosis Procedure Combination system. J Hepatobiliary Pancreat Sci 2011;18:53-59.
18 Kiriyama S, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Pitt HA, et al. New diagnostic criteria and severity assessment of acute cholangitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci 2012;19:548-556.
19 Tsuyuguchi T, Sugiyama H, Sakai Y, Nishikawa T, Yokosuka O, Mayumi T, et al. Prognostic factors of acute cholangitis in cases managed using the Tokyo Guidelines. J Hepatobiliary Pancreat Sci 2012;19:557-565.
20 Fujii Y, Ohuchida J, Chijiiwa K, Yano K, Imamura N, Nagano M, et al. Verification of Tokyo Guidelines for diagnosis and management of acute cholangitis. J Hepatobiliary Pancreat Sci 2012;19:487-491.
21 Nishino T, Onizawa S, Hamano M, Shirato I, Shirato M, Hamano T, et al. Proposed new simple scoring system to identify indications for urgent ERCP in acute cholangitis based on the Tokyo Guidelines. J Hepatobiliary Pancreat Sci 2012;19:698-706.
22 Hui CK, Lai KC, Yuen MF, Ng M, Lai CL, Lam SK. Acute cholangitis--predictive factors for emergency ERCP. Aliment Pharmacol Ther 2001;15:1633-1637.
23 Rosing DK, De Virgilio C, Nguyen AT, El Masry M, Kaji AH, Stabile BE. Cholangitis: analysis of admission prognostic indicators and outcomes. Am Surg 2007;73:949-954.
February 4, 2013
Accepted after revision June 10, 2013
Author Affiliations: Department of Gastroenterology and Hepatology (Sun G, Yang YS, Linghu EQ, Li W, Cai FC, Kong JY, Wang XD, Meng JY, Du H, Wang HB, Huang QY and Zhang XL), and Department of General Oncology (Han L), Chinese PLA General Hospital, Beijing 100853, China; Department of Gastroenterology, Pakistan Institute of Medical Sciences, G-8-3, Islamabad, Pakistan (Hyder Q)
Yun-Sheng Yang, MD, PhD, Department of Gastroenterology and Hepatology, Chinese PLA General Hospital, 28 Fuxing Road, Beijing 100853, China (Tel/Fax: 86-10-68212267; Email: sunny888@medmail.com.cn)
© 2013, Hepatobiliary Pancreat Dis Int. All rights reserved.
10.1016/S1499-3872(13)60062-4
 Hepatobiliary & Pancreatic Diseases International2013年4期
Hepatobiliary & Pancreatic Diseases International2013年4期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Effect of L-cysteine on remote organ injury in rats with severe acute pancreatitis induced by bile-pancreatic duct obstruction
- Impact of periampullary diverticula on the outcome and fluoroscopy time in endoscopic retrograde cholangiopancreatography
- The diagnostic value of high-frequency ultrasonography in biliary atresia
- Endobiliary radiofrequency ablation for malignant biliary obstruction
- Hepatic abscess associated with Salmonella serotype B in a chronic alcoholic patient
- Biliary-colonic fistula caused by cholecystectomy bile duct injury
