Radiofrequency Ablation of Hepatic Paragonimiasis:a Case Report
Wei-gang Cao and Bao-an Qiu*
Department of Hepatobiliary Surgery,PLA Navy General Hospital,Beijing 100048,China
HEPATIC paragonimiasis is a rare disease with non-specific manifestation,which is often misdiagnosed in clinical practice.Long-time drug therapy treating this disease would be accompanied by the possible development of side effects.Given the fact that this disease has seldom been reported in the literature,we provide in this article a detailed report of one case with hepatic paragonimiases treated by radiofrequency ablation,which brought favorable outcome,aiming to shed some light on the understanding of this rare condition.
CASE DESCRIPTION
General information and examination
A 56-year-old male patient was diagnosed as having hepatic neoplasm one month earlier without any symptoms such as fever,chills,nausea,vomiting,abdominal pain,or jaundice.He was admitted to PLA Navy General Hospital on July 4,2011.Upon admission,no history of hepatitis virus infection,exposure to contaminated water,or living experience in the epidemic area could be offered.Physical examination revealed no remarkable signs.Laboratory tests showed that tumor markers were negative,and the results of blood,urine,and stool tests all turned out normal.
Ultrasonography showed a 3.8 cm×2 cm low-echo zone in Segment 4b of the liver with no significant blood supply on Doppler scan (Fig.1a).Computed tomography(CT) scan showed that the mass was low in density,about 2 cm in diameter,and slightly enhanced on the edge in the arterial phase in enhanced CT.No enhancement in the venous phase was observed,nor was it noted in the delay phase (Fig.1b).No abnormality was detected in lung field on CT scan.
Pathological studies
Liver biopsy was performed,the result of which showed liver tissue necrosis surrounded by fibrous tissue,eosinophil and neutrophil infiltration,and epithelial cell response (Fig.2a).Charcot-Leyden crystals,degeneration and calcification of the egg-like structure were seen in the necrotic liver tissue (Fig.2b),which were in accordance with the pathological changes of hepatic paragonimiases.Hepatic tumors could be excluded based on the pathological results.
Therapeutic procedures
Given the diagnosis of hepatic paragonimiasis,treatment with radiofrequency ablation was decided upon for the patient.When he was lying in supine position,a 150-T30 radiofrequency (RF) needle (Olympus-Celon AG Medical Instruments Company,Hamburg,Germany) was punctured into the mass lesion under ultrasound guidance with local anesthesia.Under intravenous anesthesia,the RF needle was successfully positioned to the foci for radiofrequency ablation.Energy of 25 J was applied,which could destroy a lesion of 5 cm in diameter.The ablation area was approximately 4.0 cm× 2.6 cm,covering all the paragonimiasis foci (Fig.3).The condition of the patient remained stable during ablation.No immediate complication occurred after the procedure.The patient was discharged from the hospital 5 days later.During the follow-up period of 5 months,the lesion was found subsided gradually,with no clear recurrence on liver CT scan.
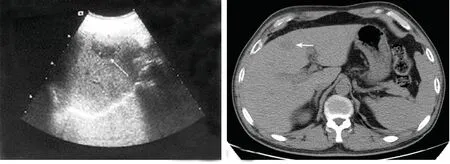
Figure 1.Imaging findings of a 56-year-old male patient with hepatic paragonimiasis.
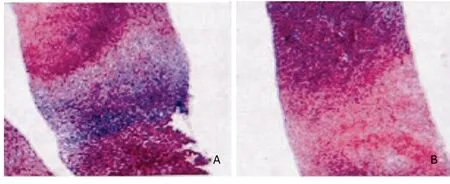
Figure 2.Pathological findings of the patient before treatment.HE ×400
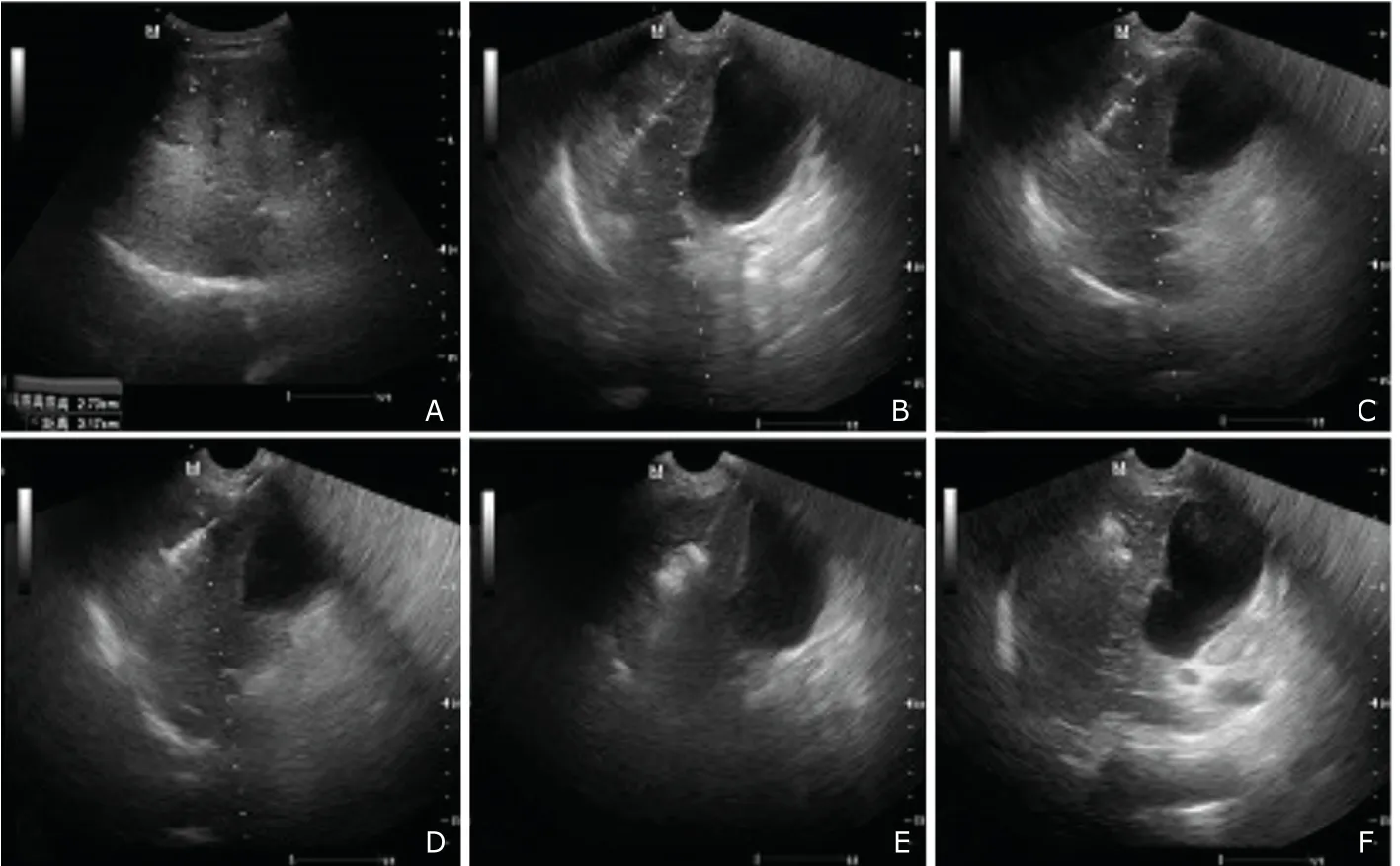
Figure 3.Ultrasonographic images during the procedure of radiofrequency ablation.
DISCUSSION
As a type of zoonotic parasitic disease,paragonimiasis is caused by paragonimus,which is widely distributed in Southeast Asian,African,and South American regions.The disease could be divided into intrapulmonary and extrapulmonary types,1the latter type including hepatic paragonimiasis.Hepatic paragonimiasis is caused by invasion of ectopic paragonimus.It can be divided into 3 types,one type involving only the liver,one type involving only the biliary system,and the other involving both the liver and the biliary system.2In the present case,only liver parenchyma was involved,and no biliary duct was found invaded by paragonimus.
The diagnosis of hepatic paragonimiasis is usually difficult due to the absence of specific symptoms and manifestations.Laboratory tests are no more reliable in providing diagnostic evidence.Pathological examination is the only useful and reliable means in the diagnosis of this disease.It demonstrates as pathological coagulation necrosis with the formation of small cysts or acupuncture points,a lot of Charcot-Leyden crystals,and massive eosinophil infiltration,which could help make a primary diagnosis of hepatic paragonimiasis.Doctors should consider the possibility of this disease when the patient with mass lesion in the liver has been in epidemic area and when malignancy could be excluded.
Although oral administration of deworming medicine such as praziquantel and sulfur double-dichlorophenol could be effective in some patients,especially in those with biliary duct involvement or mixed involvement,long-term oral medicine would be associated with a high possibility of side effects as dizziness,headaches,gastrointestinal reactions,rash,and even liver/kidney damages.Radiofrequency ablation under ultrasound guidance,which is usually used in tumor therapy,could destroy the parasite when the disease is localized.However,this application has not been reported before.The outcome of the present patient proved the efficacy of radiofrequency ablation in treating this disease.No significant side effect or complication appeared after the treatment,yet follow-up for a long period would be necessary to monitor any signs of residual paragonimus or recurrence.
As a simple,economical,and reproducible therapeutic procedure,radiofrequency ablation could be one of the means used in treating patients with local mass in the liver.Its application to hepatic paragonimiasis is also worth considering.Further observation of the method would be necessary in clinical practice to evaluate its therapeutic effects for hepatic paragonimiasis.
1.Carré JC.Houmdaophet S.[Paragonimiasis].Rev Pneumol Clin 1998;54:359-64.
2.Van Beers B,Pringot J,Geubel A,et al.Hepatobiliary fascioliasis:noninvasive imaging findings.Radiology 1990;174:809-10.
 Chinese Medical Sciences Journal2012年1期
Chinese Medical Sciences Journal2012年1期
- Chinese Medical Sciences Journal的其它文章
- Management of Pregnancy with Ankylosing Spondylitis
- Applicability of Community Periodontal Index Teeth and Random Half-mouth Examination to Gingival Bleeding Assessment in Untreated Adult Population in Beijing
- Personalized Management of Anastomotic Leak after Surgery for Esophageal Carcinoma
- Spectral Domain Optical Coherence Tomography of Vogt-Koyanagi-Harada Disease:Novel Findings and New Insights into the Pathogenesis
- Electrocorticography with Direct Cortical Stimulation for a Left Temporal Glioma with Intractable Epilepsy
- Primary Sjögren's Syndrome Accompanied by Intestinal Obstruction:a Case Report and Literature Review
