Prognostic value of N-terminal pro B-type natriuretic peptide and troponin I in children with dengue shock syndrome
Truyen Phuoc Le ,Phung Nguyen The Nguyen
1University of Medicine and Pharmacy at Ho Chi Minh city,Ho Chi Minh City,Vietnam
2Children's Hospital 1,Ho Chi Minh City,Vietnam
ABSTRACT Objective: To investigate the contribution of N-terminal pro B-type natriuretic peptide (NT-pro BNP) and troponin I to mortality in children with dengue shock syndrome.Methods: A longitudinal study was conducted on children with dengue shock syndrome in a hospital in southern Vietnam.Detailed clinical histories,physical examinations,and laboratory parameters,including NT-pro BNP and troponin I,were recorded.A comparison between survival and non-survival was carried out to identify factors influencing mortality.Results: A total of 107 patients with a median age of 9 years were included in the study.Among them,63.6% (68/107) presented with compensated shock,36.4% (39/107) had hypotensive shock,23.4%(25/107) required mechanical ventilation,and 12.1% (13/107) died.The NT-pro BNP levels were 3.9 pmol/L (IQR: 1.9,10.3) and 15.2 pmol/L (5.8,46.3),while the median high sensitivity troponin I levels were 20 pg/L (6,95) and 62 pg/L (12,325) at the first and second measurements,respectively.The mortality group exhibited higher rates of hypotensive shock,prolonged shock,lactate levels,liver damage,NT-pro BNP,and troponin I levels.Hypotensive shock(OR 12.96,95% CI 2.70-62.30,P=0.004),prolonged shock (OR 39.40,95% CI 6.68-232.70,P<0.001),AST > 1 000 IU/L (OR 9.50,95% CI 2.63-34.34,P=0.041),and NT-pro BNP > 7 pmol/L (OR 44.40,95% CI 5.44-362.20,P=0.001) were identified as predictive factors for mortality in dengue shock syndrome.Conclusions: The NT-pro BNP level could serve as a potential biomarker for predicting mortality in children with dengue shock syndrome.
KEYWORDS: Dengue shock syndrome;Cardiac enzyme;NT-pro BNP;Troponin I
1.Introduction
Dengue is a significant global tropical disease,primarily prevalent in the Asia-Pacific region.It imposes a substantial burden on healthcare systems,households,and economies[1,2].Annually,over 50 million cases are reported in dengue-endemic areas,with Vietnam experiencing a fivefold increase in 2022 compared to 2021[3].Dengue manifests in various clinical forms,from mild to severe,highlighting the critical need for early detection,particularly in resource-limited settings.Current methods,including the World Health Organization (WHO)'s warning signs,lack sensitivity in the early stages.There is an urgent demand for a reliable biomarker to improve the early management of severe dengue cases.In recent years,there has been increased recognition of myocarditis as a potentially life-threatening complication of dengue infection.Researchers and healthcare professionals are increasingly investigating the link between dengue and myocarditis,with an estimated prevalence of around 12%,particularly higher among children,despite varying diagnostic criteria in studies.Additionally,myocarditis in dengue patients was linked to an increased risk of severity (relative risk of 2.44) and mortality (relative risk of 19.41)when compared to dengue patients who did not exhibit signs of myocarditis[4].Troponin I is a specific cardiac troponin released from damaged cardiomyocytes.Therefore,troponin I is a suitable marker for detecting myocarditis or cardiac injury[5,6].
In the treatment of dengue shock syndrome,intravenous fluid resuscitation is crucial[2].However,sometimes it is difficult to distinguish between pulmonary edema,acute respiratory distress syndrome,acute heart failure,or fluid overload in a patient with respiratory distress.N-terminal pro B-type natriuretic peptide(NT-pro BNP) is an ideal biomarker for acute heart failure,as it is released in response to myocardial stretch when there is fluid overload in the circulation[7,8].
Until now,there have been some studies on NT-pro BNP and troponin I in dengue patients,but almost no studies have specifically focused on NT-pro BNP and troponin I in dengue shock syndrome.The objective of this study was to assess NT-pro BNP and troponin I levels in children with dengue shock syndrome to evaluate their importance in classifying patients with dengue shock.Additionally,the study aimed to explore the potential of NT-pro BNP and troponin I as dependable biomarkers for early-phase prediction of mortality in dengue shock syndrome.
2.Subjects and methods
2.1.Study design
A longitudinal study was conducted in the Emergency Department and Intensive Care Unit at Children’s Hospital 1 at Ho Chi Minh city,Vietnam for 2 years from January 2021 to December 2022.
2.2.Ethics statement and informed consent
The study was approved by the Ethics Committee of University of Medicine and Pharmacy at Ho Chi Minh city with protocol ID 2130-DHYD and was registered in ClinicalTrials.gov with ID NCT04837430.Patient recruitment was carried out with prior authorization from the Ethics Committee of Children's Hospital 1,identified by ID CS/N1/21/04.Informed consent,which included a thorough explanation,was obtained from all patients and their parents.The details of the reports were kept completely confidential.
2.3.Participants characteristics
This prospective study included all children aged from 1 month to 16 years old who were diagnosed with dengue shock syndrome and admitted to the Emergency Department of Children's Hospital 1.Dengue-positive cases were confirmed through clinical examination and the presence of either a positive NS1 antigen (Humasis Co.,Ltd.,South Korea) or positive dengue IgM antibodies (NovaLisa™,Novatec German).
All patients enrolled in the study underwent a comprehensive clinical history assessment and full physical examination.Monitoring of patients occurred every 6 hours while they were in the Emergency Department (ED) and Intensive Care Unit (ICU) to observe hemodynamic changes and clinical signs.Prolonged shock was defined as shock that continues to occur in the ICU or persists for 6 hours after admission to the ED.Laboratory investigations included arterial blood gas,lactate,and serum albumin,which were performed every 6 hours.Additionally,complete blood counts(CBC),prothrombin time with international normalized ratio (PT with INR),activated partial thromboplastin time (aPTT),fibrinogen,and liver function tests,including serum alanine transaminase (ALT)and serum aspartate transaminase (AST),were conducted daily or as needed based on clinical requirements.Renal function tests,encompassing blood urea and serum creatinine,were also performed daily or as clinically indicated.All these tests were done at the Biochemistry Department at Children's Hospital 1.
NT-pro BNP and high sensitivity troponin I (troponin Ihs)measurements were taken at 6-hour and 18-hour for each subject.Approximately 2.5 mL of blood was collected in serum separator tubes (SST).After centrifugation,the serum specimens were stored at temperatures between -18 ℃ and -25 ℃.The measurements of NT-pro BNP and troponin Ihs were conducted using the ARCHITECT system 2R10 by Abbott.NT-pro BNP and troponin Ihs tests were performed at the Biochemistry Department at Cho Ray hospital.An NT-pro BNP level exceeding 7 pmol/L was considered abnormal,while a troponin Ihs level surpassing 100 pg/L was also defined as abnormal.
2.4.Statistical analysis
Data analysis was performed using IBM SPSS Statistics software version 26.0 for Mac (SPSS Inc.,Chicago,IL,USA).Categorical variables were presented as frequencies and percentages.Continuous variables with non-normal distributions were expressed as median(interquartile range,IQR),while continuously normally distributed variables were expressed as mean ± standard deviation.For comparisons,the frequencies of categorical variables were analyzed using Pearson χ2or Fisher's exact test when appropriate.The means of two continuous,normally distributed variables were compared using independent samples Student's t-test,while the Mann-Whitney U test was employed to compare means of two groups of variables that were not normally distributed.A value of P<0.05 was considered significant.
3.Results
3.1.Patient demographic and baseline characteristics
A total of 107 patients were enrolled in this study.The median age was 9.0 years (IQR: 6.4,11.7),with the majority of patients being older than 5 years old (79.0%).Among the 107 patients,65 (60.7%)were males,and 42 (39.3%) were females.The median duration of illness at the time of admission was 5 days (IQR: 4,5),with the majority of cases occurring on the 4th and 5th days (79.0%).The most common chief complaint was lethargy,presented in 51 patients(47.7%).The second most common symptom was abdominal pain in 20 patients (18.7%),followed by persistent vomiting in 17 patients(15.9%),fever in 12 patients (11.2%),cold extremities in 4 patients(3.7%),seizures in 2 patients (1.9%),and diarrhea in 1 patient(0.9%).Overall,68 patients (63.6%) presented with compensated shock,while 39 patients (36.4%) had hypotensive shock.Regarding nutritional status,6.5% of patients were undernourished (7 patients),24.3% were of normal weight (26 patients),11.2% were overweight(12 patients),and 57.9% were obese (62 patients).
At the time of admission,72.9% of patients had age-adjusted hypotension (n=78),54.2% of patients had tachycardia (n=58).Notably,64.4% (n=69) of the patients were in shock at the time of admission.Additionally,17.8% experienced a change in mental state(n=19).Concerning peripheral pulse volume,62.6% had weak or absent pulses (n=67).About 77.6% of patients had cool peripheries or cold extremities (n=83).In terms of respiratory rate,55.1% had tachypnea (n=59),although all patients had good oxygen saturation.
After 6 hours,25.2% of patients still had age-adjusted hypotension,and 21.5% of patients continued to have tachycardia.Furthermore,15.9% experienced a change in mental state (n=17),4.7% had weak or absent peripheral pulses (n=5),and 12.1% still had cool peripheries or cold extremities (n=13).Shock was observed in 7.5%(n=8) of the patients after 6 hours post-admission (prolong shock).Regarding respiratory rate,66.4% had tachypnea (n=71),but all patients maintained good oxygen saturation,with a mean SpO2of 99% (IQR: 98%,100%).Regarding laboratory parameters,the median lactate level was 3.31(2.07,5.33) mmol/L,with 39.3% (n=42) of patients having lactate levels exceeding 4 mmol/L.Hepatic involvement was reflected in AST levels,which had a median of 313 (131,1 053) IU/L,and ALT levels,with a median of 149 (53,384) IU/L.Notably,25.3% (n=27)of patients had AST levels exceeding 1 000 IU/L,while 11.2%(n=12) had ALT levels surpassing 1 000 IU/L.The median albumin level was 2.38 g/L (1.71,3.05),and 36.4% (n=39) of patients had albumin levels below 2 g/L.The median CRP level was 4.0 (2.3,8.5)mg/L.In arterial blood gas analysis,the median pH was 7.47 (7.42,7.50) with 9.3% (n=10) of patients exhibited a pH lower than 7.3,and the median base excess was -5.5 (-10.0,12.5).Over half of the patients (53.3%,n=57) had BE levels below -5.Furthermore,the INR was 1.39 (1.12,1.80) with 36.4% (n=39) over 1.50.Meanwhile,hematocrit was 0.48 (0.41,0.53),with 30.8% (n=33) having hematocrit higher than 50%,and platelets were 23 (16,38) K/mcL,with 89.7% (n=96) having platelets lower than 50 K/mcL.
Regarding treatment,total fluid resuscitation was 193 (165,253)mL/kg in 36.5 (32.0,45.0) hours.The velocity of intravenous fluid resuscitation at 6-hour and 12-hour intervals was 5.00 (4.17,6.25)mL/kg/h and 4.00 (3.00,5.09) mL/kg/h,respectively.The rate of inotropes/vasopressor usage was 25.2%,and the rate of mechanical ventilation was 23.4% (Table 1).

Table 1.Baseline characteristics of the study patients.
3.2.NT-pro BNP and troponin Ihs levels
The median NT-pro BNP level was 3.9 pmol/L (1.9,10.3) at the initial measurement and 15.2 pmol/L (5.8,46.3) at the subsequent measurement.Meanwhile,the median troponin Ihs level was 20 pg/ L (6,95) at the initial measurement and 62 pg/L (12,325) at the subsequent measurement (Table 1).29.9% (n=32) and 72.0% (n=77)of the subjects had abnormal NT-pro BNP levels during the initial and subsequent measurements,respectively.Additionally,22.4%(n=24) and 42.1% (n=45) of the subjects had abnormal troponin Ihs levels during the initial and subsequent measurements,respectively.
3.3.Predictors of mortality of dengue
The overall mortality rate in our study was 12.1% (13/107),with 7 males and 6 females.All of these patients were in the ventilated group,and they received intravenous fluid resuscitation of 504 mL/ kg (IQR: 368,674) over 50 hours (IQR: 45,69),with a velocity of intravenous fluid resuscitation at 9 mL/kg per hour.Additionally,all of these patients received vasopressor and inotropic therapies,including adrenaline in 11 cases,noradrenaline in 10 cases,dobutamine in 9 cases,and dopamine in 8 cases.
As discribed in Table 2,when we compared the mortality group to the survival group,the rates of hypotensive shock,prolonged shock,lactate level,AST level,NT-pro BNP,and the amount of intravenous fluid resuscitation were higher in the mortality group.The patients in the non-survival group tend to experience shock in the early days of illness,typically on day 4 or day 3.As a result,the duration of plasma leakage is longer for this group.In contrast,the survival group tends to develop shock later in the course of the disease (P<0.05).While the percentage of shock at admission did not differ between the two groups (P=0.813),the percentages of both hypotensive shock and prolonged shock were higher in the non-survival group (P<0.001).Most patients in the survival group presented with compensated shock at admission.
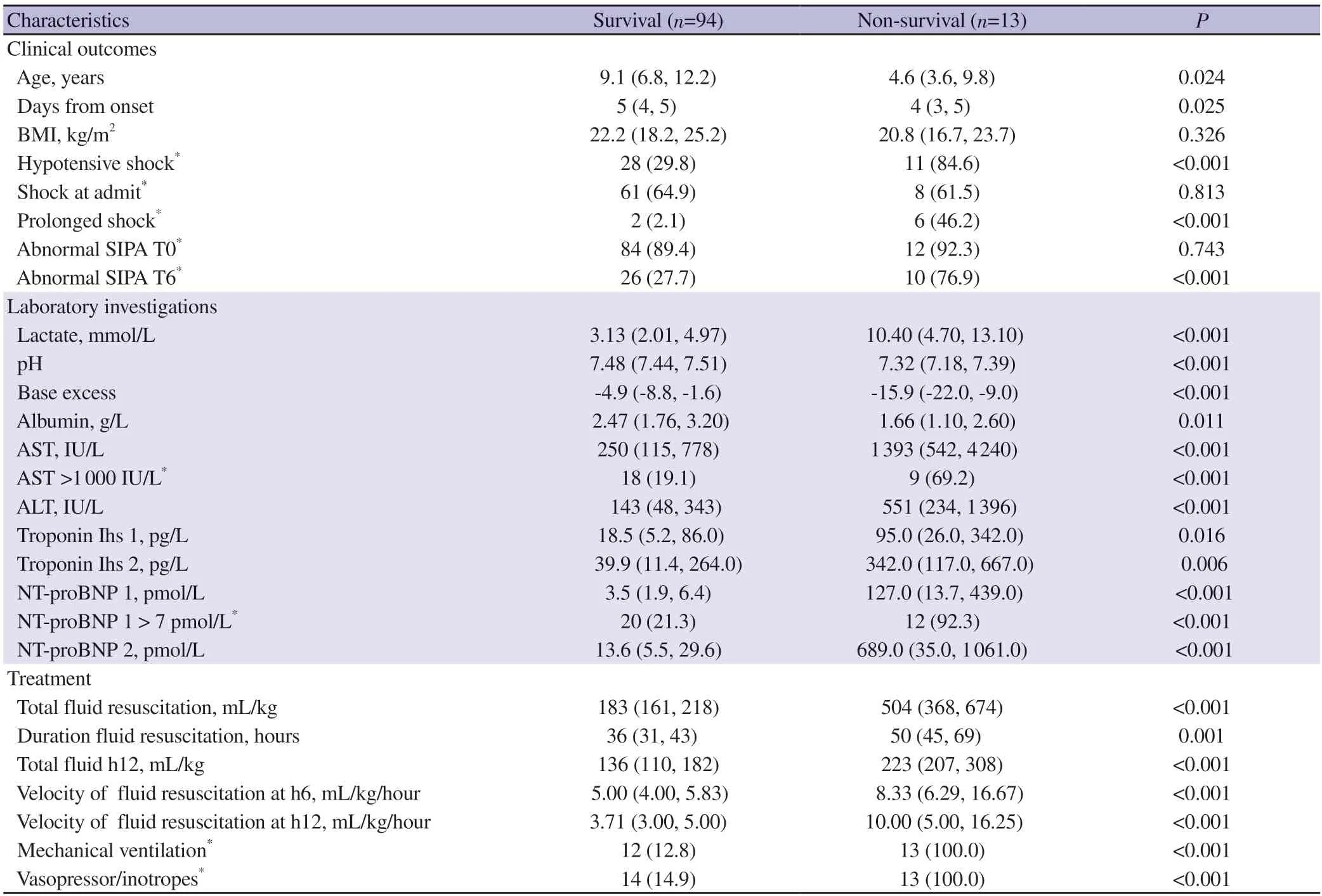
Table 2.Comparison between survival and non-survival groups.
Regarding laboratory findings,the non-survival group showed more severe indicators of shock,with higher lactate levels (10.40 mmol/ L vs.3.13 mmol/L),lower pH values (7.32 vs.7.48),and reduced base excess levels (-15.9 vs.-4.9) compared to the survival group.Furthermore,the non-survival group displayed more pronouncedliver damage,indicated by elevated AST and ALT levels,along with increased plasma leakage characterized by lower serum albumin levels.Simultaneously,NT-pro BNP and troponin I were higher in the non-survival group compared to the survival group (Table 2).
Regarding treatment,the non-survival group received a greater overall volume of fluid for resuscitation and had a longer duration of fluid resuscitation compared to the survival group.Intubation and ventilation were necessary for 100% of the non-survival group,while only 12.8% of the survival group required this intervention,typically initiated around 18 hours after admission to the Emergency Department.As a result,we conducted an analysis using the amount of fluid administered before this time as a predictive factor for intubation.Our findings indicated that the total fluid volume administered within the initial 12 hours and the rate of fluid administration at 6 and 12 hours were higher in the nonsurvival group.Essentially,an inability to reduce the rate of fluid resuscitation at 6 and 12 hours suggested that these patients might require intubation and ventilation.
In the end,as discribed in Table 3,regression analysis was conducted to identify the factors influencing mortality in dengue shock syndrome.Initially,all variables underwent univariate regression analysis,and only those variables that showed significance were subsequently subjected to multivariate analysis.At the time of the analysis,it was determined that hypotensive shock,prolonged shock,AST levels above 1 000 IU/L,and abnormal NT-pro BNP(exceeding 7 pmol/L) were predictive factors for mortality in dengue shock syndrome.
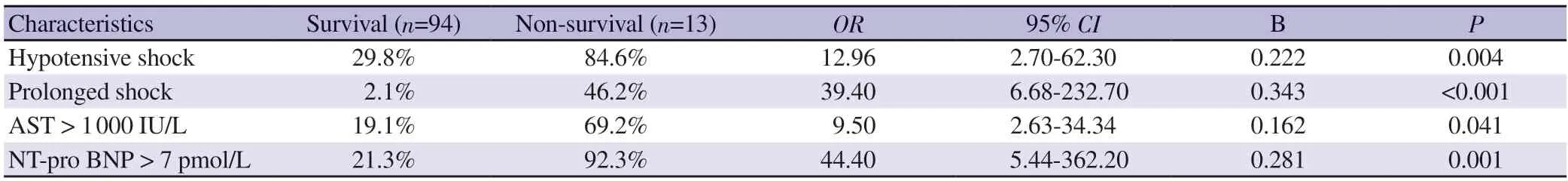
Table 3.Factors influencing mortality in dengue shock syndrome.
4.Discussion
This study was a longitudinal investigation conducted over a duration of two years,spanning from January 2021 to December 2022,and it encompassed a sample of 107 children diagnosed with dengue shock syndrome.The median age was 9 years,dominant in children older than 5 years and prominent in male.This result was familiar with Saiful Islam in Bangladesh,Nutnicha Preeprem in Thailand and Nguyen Phung in Vietnam[9-11].This distribution highlights that dengue shock syndrome can affect a broad age range in children,with the majority falling within this relatively older age group.Typically,children in this study presented with dengue shock syndrome on the fourth or fifth day of the disease.Chief complaints and symptoms shed light on the clinical presentation of these children.Lethargy was the most common chief complaint,reported in 47.7% of patients,followed by abdominal pain,which was the second most frequent symptom,occurring in 18.7% of cases.These signs and symptoms align with the warning signs outlined in the WHO classification for dengue management[2].The prevalence of nutritional status among the study participants is a notable observation.Among them,11.2% were overweight,and 57.9% were obese.These characteristics are known predisposing factors for severe dengue[12].
Our study was conducted in dengue shock patients,so the signs and symptoms of peripheral vascular collapse were evident.The median systolic blood pressure was notably low,with 72.9% of patients had hypotension.Tachycardia was prevalent in 54.2% of cases,indicating increased stress on the cardiovascular system.A significant proportion of patients exhibited altered mental states,weak or absent peripheral pulses,and cool extremities,all indicative of circulatory collapse.Neeraja and Menwal had the same findings when researching severe dengue patients[13,14].While 55.1% had tachypnea,their maintained good oxygen saturation suggests that respiratory function remained relatively unaffected.Interestingly,within 6 hours,systolic blood pressure showed a moderate improvement,even though 25.2% still below the normal range.The pulse rate decreased,but tachycardia persisted in 21.5% of cases.The presence of such severe shock signs highlights the need for rapid and aggressive intervention in dengue shock syndrome cases to improve patient outcomes.
In our study,39.3% had lactate levels higher than 4 mmol/L,and 53.3% had a base excess less than -5.Simultaneously,AST levels had a median of 313 (131,1 053) IU/L,with 25.3% of patients having AST levels exceeding 1 000 IU/L.Researchers such as Mansanguan and Miranda also found a higher rate of liver damage in dengue shock syndrome patients[15,16].The CRP level in our study was lower than that in Rao et al's study,possibly due to the higher proportion of liver damage observed in our study[17].Another explanation is that Rao et al.focused on adult patients with many chronic diseases,leading to a high baseline level of CRP,whereas our study specifically concentrated on children with a lower baseline CRP level.
The analysis of NT-pro BNP and troponin Ihs levels in children with dengue shock syndrome offers valuable insights into their prognostic significance.NT-pro BNP levels displayed a notable increase between the initial and subsequent measurements,indicating a progression in the severity of the disease.Similarly,troponin Ihs levels exhibited an increase,although not as pronounced.A considerable proportion of patients exhibited abnormal levels,particularly during the subsequent measurements,underscoring these biomarkers' role as indicators of cardiac involvement in dengue shock syndrome.Atmaja and Bhatt found troponin I,NT-pro BNP corresponds to an increase in the dengue severity level in patients with dengue shock syndrome[18,19].
Our study found that in children with dengue shock syndrome,early and prolonged shock experiences are associated with a higher risk of mortality.Laboratory findings revealed that non-survivors had more severe shock indicators and cardiac involvement.Additionally,these patients received more extensive fluid resuscitation and required mechanical ventilation.Regression analysis identified hypotensive shock,prolonged shock,elevated AST levels,and high NT-pro BNP as predictive factors for mortality.Early recognition of these factors can improve risk assessment and guide interventions to enhance patient outcomes.The patients in our study are more severe than those in Nguyen Phung’s study,with 77.6% of our patients having hepatic damage,which was defined when patients had AST or ALT levels > 120 UI/L,compared to 60% in Nguyen Phung’s study[20].
Regarding treatment,the non-survival group received greater volumes of fluid resuscitation over a longer duration.The need for intubation and mechanical ventilation was universal in the nonsurvival group,in contrast to the survival group,where only 12.8% of patients required this intervention,typically initiated around 18 hours after admission.Analysis using the amount of fluid administered within the initial 12 hours and the rates of fluid administration at 6 and 12 hours revealed significant differences between the two groups,underscoring the impact of fluid management on outcomes.
In the end,regression analysis highlighted specific factors predictive of mortality in dengue shock syndrome.These included hypotensive shock,prolonged shock,elevated AST levels above 1 000 IU/L,and abnormal NT-pro BNP levels exceeding 7 pmol/ L.Recognizing these factors can aid in early risk stratification and targeted interventions to improve patient outcomes.
Acknowledging the study's scope,a limitation is the modest tally of 25 cases requiring mechanical ventilation,suggesting the potential for deeper insights with a larger subset.Additionally,the assessment of NT-proBNP and troponin markers at only two intervals indicates a need for more frequent testing to enhance our understanding.
Conflict of interest statement
We declare no conflict of interests.
Funding
The authors received no extramural funding for the study.
Acknowledgments
We extend our gratitude to Dr.Nguyen Thi Mai Anh for participating as a content expert reviewer.We also acknowledge the cooperation and support of all healthcare workers at Children's Hospital 1 and Cho Ray Hospital for their dedicated efforts in the study.
Authors’contributions
All authors played significant roles in drafting,revising,and providing final approval for the article to be submitted.TPL contributed to the study's design,data acquisition,conducted data analysis,and interpreted the findings.NNTP contributed to the study's design and data interpretation.
 Asian Pacific Journal of Tropical Medicine2024年4期
Asian Pacific Journal of Tropical Medicine2024年4期
- Asian Pacific Journal of Tropical Medicine的其它文章
- Recent advances on vaccines against malaria: A review
- Role of doxycycline in the treatment of dengue infection: An open-label,randomized,controlled,pilot trial
- Expression and clinical significance of pattern recognition receptor-associated genes in hand,foot and mouth disease
- A rare complication of measles infection presented with subacute sclerosing panencephalitis: Report of two cases in India
- Using X Social Networks (formerly Twitter) and web news mining to predict the measles outbreak
