Delivery room resuscitation intensity and associated neonatal outcomes of 24+0–31+6 weeks’ preterm infants in China:a retrospective cross-sectional study
Si-Lu Wang·Chun Chen·Xin-Yue Gu·Zhao-Qing Yin·Le Su·Si-Yuan Jiang·Yun Cao·Li-Zhong Du·Jian-Hua Sun·Jiang-Qin Liu ·Chuan-Zhong Yang on behalf of Chinese Neonatal Network Investigators
Abstract Background The aim of this study was to review current delivery room (DR) resuscitation intensity in Chinese tertiary neonatal intensive care units and to investigate the association between DR resuscitation intensity and short-term outcomes in preterm infants born at 24+0–31+6 weeks’ gestation age (GA).Methods This was a retrospective cross-sectional study.The source population was infants born at 24+0–31+6 weeks’ GA who were enrolled in the Chinese Neonatal Network 2019 cohort.Eligible infants were categorized into five groups: (1)regular care; (2) oxygen supplementation and/or continuous positive airway pressure (O 2/ CPAP); (3) mask ventilation; (4)endotracheal intubation; and (5) cardiopulmonary resuscitation (CPR).The association between DR resuscitation and shortterm outcomes was evaluated by inverse propensity score-weighted logistic regression.Results Of 7939 infants included in this cohort, 2419 (30.5%) received regular care, 1994 (25.1%) received O 2/ CPAP, 1436(18.1%) received mask ventilation, 1769 (22.3%) received endotracheal intubation, and 321 (4.0%) received CPR in the DR.Advanced maternal age and maternal hypertension correlated with a higher need for resuscitation, and antenatal steroid use tended to be associated with a lower need for resuscitation (P < 0.001).Severe brain impairment increased signif ciantly with increasing amounts of resuscitation in DR after adjusting for perinatal factors.Resuscitation strategies vary widely between centers, with over 50% of preterm infants in eight centers requiring higher intensity resuscitation.Conclusions Increased intensity of DR interventions was associated with increased mortality and morbidities in very preterm infants in China.There is wide variation in resuscitative approaches across delivery centers, and ongoing quality improvement to standardize resuscitation practices is needed.
Keywords Cardiopulmonary resuscitation·Delivery room·Endotracheal intubation·Neonatal resuscitation·Preterm
Introduction
The transition of the fetus from an intrauterine to extrauterine environment is accomplished through multiple physiological changes that occur before and at birth, and most newborns can successfully complete this transition without medical intervention.However, up to 10% of newborns will need some degree of resuscitation after birth, and approximately 5% of term infants receive positive-pressure ventilation (PPV) to make a successful transition, 2% are intubated, 0.1% receive cardiac compressions, and 0.05% receive compressions with epinephrine [1, 2].Preterm infants generally need more resuscitation interventions at birth due to their anatomical and physiological characteristics, especially 6%–7% of preterm infants < 32 weeks’ gestational age (GA) [3].High resuscitation intensity increases the risk of short- or long-term adverse outcomes, which is influenced by initial resuscitation in the frist few minutes in the delivery room (DR) [1].
The Neonatal Resuscitation Program guidelines published by the American Academy of Pediatrics recommend a standardized set of resuscitation practices in DR, including initial steps, PPV, endotracheal intubation, cardiopulmonary resuscitation (CPR), and medications [4].Most infants are stabilized with non-invasive respiratory support after birth,but about 40% of preterm infants still require higher-level resuscitation methods, such as endotracheal intubation for invasive respiratory support [5, 6].
In China, a study demonstrated a significant correlation between different treatment practices and tertiary hospitals in each study.The number of preterm infants is increasing in different provinces, and treatment practices are improving[7].This means that there is variation in Chinese hospitals and a lack of adherence to standardized neonatal resuscitation guidelines based on the China neonatal resuscitation guideline [8].However, there is still a gap in treatment practices compared to developed countries.
As the Chinese Neonatal Network (CHNN) is a large standardized collaborative network of 70 tertiary Chinese neonatal intensive care units (NICUs), this research aimed to describe the variations in the intensity of resuscitation in DR for preterm infants with a GA of 24+0–31+6in China.The research also aimed to investigate the correlation between different highest levels of intensity and short-term outcomes of very preterm infants in DR.
Methods
The Chinese Neonatal Network and participating hospitals
The CHNN is a national network of Chinese tertiary NICUs with the primary goal of conducting high-quality collaborative research dedicated to the improvement of neonatal-perinatal health in China [9].Hospitals enrolled in CHNN are required to be tertiary referral hospitals with large neonatal services and have expertise in caring for high-risk neonates.CHNN has established and maintained a standardized clinical database of preterm infants < 32 weeks’ gestation or < 1500 g with participating NICUs throughout China.This clinical database has been monitoring outcomes and care practices since January 1, 2019.A total of 57 hospitals in 25 provinces across the country collected data using the CHNN database in 2019.These 57 hospitals included four national children’s medical centers, four regional children’s medical centers,and 30 provincial perinatal or children’s medical centers.The other 19 hospitals comprised major referral centers in large cities across China.Forty-three hospitals were perinatal centers with birthing facilities, and 14 hospitals were free-standing children’s hospitals that only admitted outborn infants.All hospitals had the ability to provide care for infants < 32 weeks’ gestation.
Study population
The study population included infants delivered between January 1, 2019 and December 31, 2019 at 24+0_31+6weeks’GA who were admitted to CHNN hospitals and were retrospectively reviewed.Infants admitted within 3 days of age were included in this study.Stillbirth, DR deaths, and transfers to non-participating hospitals within 24 hours after birth were not included in this analysis.Readmissions and transfers between participating hospitals were tracked as data from the same infants.Infants were followed until NICU discharge or transfer or death.Infants with major congenital anomalies, unknown resuscitation details, palliative care, or no active resuscitation due to life-limiting diagnoses were excluded.Data collection at each site was approved by either the institution’s research ethics board or quality improvement and data management committee.
Data collection
Trained data abstractors were responsible for data acquisition in each hospital.Data were directly entered into a customized database with built-in error checking and a standard manual of operations and definitions.Data were electronically transmitted to the CHNN coordinating center in Children’s Hospital of Fudan University with patient identity kept conf diential.Site investigators were responsible for data quality control at each site.
DR resuscitation was defined as receipt of any assistance after birth besides regular care––this includes providing warmth, drying and/or plastic wrap, and stimulation of the infant [4].Infants were divided into five categories according to the highest intensity of resuscitation they received, in order from “lowest intensity” to “highest intensity”: (1) regular care including warmth, dry or plastic bag wrapping and suction when necessary; (2) oxygen supplementation and/or continuous positive airway pressure (O2/ CPAP); (3) PPV via mask ventilation; (4) PPV via endotracheal intubation(ETT-PPV); and (5) CPR with or without medical therapy.
Definitions
Intraventricular hemorrhage (IVH) was defined as ≥ grade 3 according to Papile’s criteria [10].Cystic periventricular leukomalacia (cPVL) was defined as the presence of periventricular cysts on cranial ultrasound or magnetic resonance imaging.Severe brain injury was defined as IVH (grade ≥ 3) and cPVL.Early-onset sepsis was defined as sepsis occurring within 72 hours after birth.Late-onset sepsis was defined as sepsis occurring after 72 hours of age [11].Respiratory distress syndrome (RDS) was diagnosed in preterm infants with the onset of respiratory distress shortly after birth and a compatible chest radiograph appearance [12].GA was determined using the hierarchy of the best obstetric estimate based on prenatal first trimester dating ultrasound, menstrual history, obstetric examination, or all three.If the obstetric estimate was not available or was different from the postnatal estimate of gestation by more than two weeks, the GA was estimated using the Ballard score [13].Small for gestational age(SGA) was defined as birth weight < 10th percentile for the GA according to the Chinese neonatal birth weight values [14 ].Prenatal care was defined as ≥ 1 pregnancyrelated hospital visit during pregnancy.
Statistical analysis
Maternal and infant characteristics, as well as neonatal outcomes of infants, were compared using ANOVA or the Kruskal–Wallis test as appropriate for continuous variables and the Chi-square test for categorical variables.The trends of demographic characteristics and outcomes across resuscitation intensity levels were tested by the Cochrane–Armitage trend test for binary variables or the Jonckheere–Terpstra trend test for continuous variables.Univariate and inverse propensity score-weighted logistic regression models were generated to indicate the significance of neonatal outcomes and NICU resource use associated with the five intensity levels of DR resuscitation.Covariates for propensity score calculation are either tested significantly different across resuscitation intensity groups or investigator selected due to their clinical knowledge, including GA, SGA, inborn/outborn status, maternal age, maternal hypertension, premature rupture of membranes (PROM) > 24 hours, and antenatal steroids (ANS).A two-sided significance level of 0.05 was used without adjustment for multiple comparisons.All analyses were performed using SAS 9.4 software.
Results
Study population
A total of 8297 infants across forty-three centers were enrolled in the CHNN database during 2019 (Fig.1).Sixty-three infants with major congenital anomalies, 277 with unknown resuscitation intensity, and 18 with palliative care or no resuscitation were excluded from this analysis.
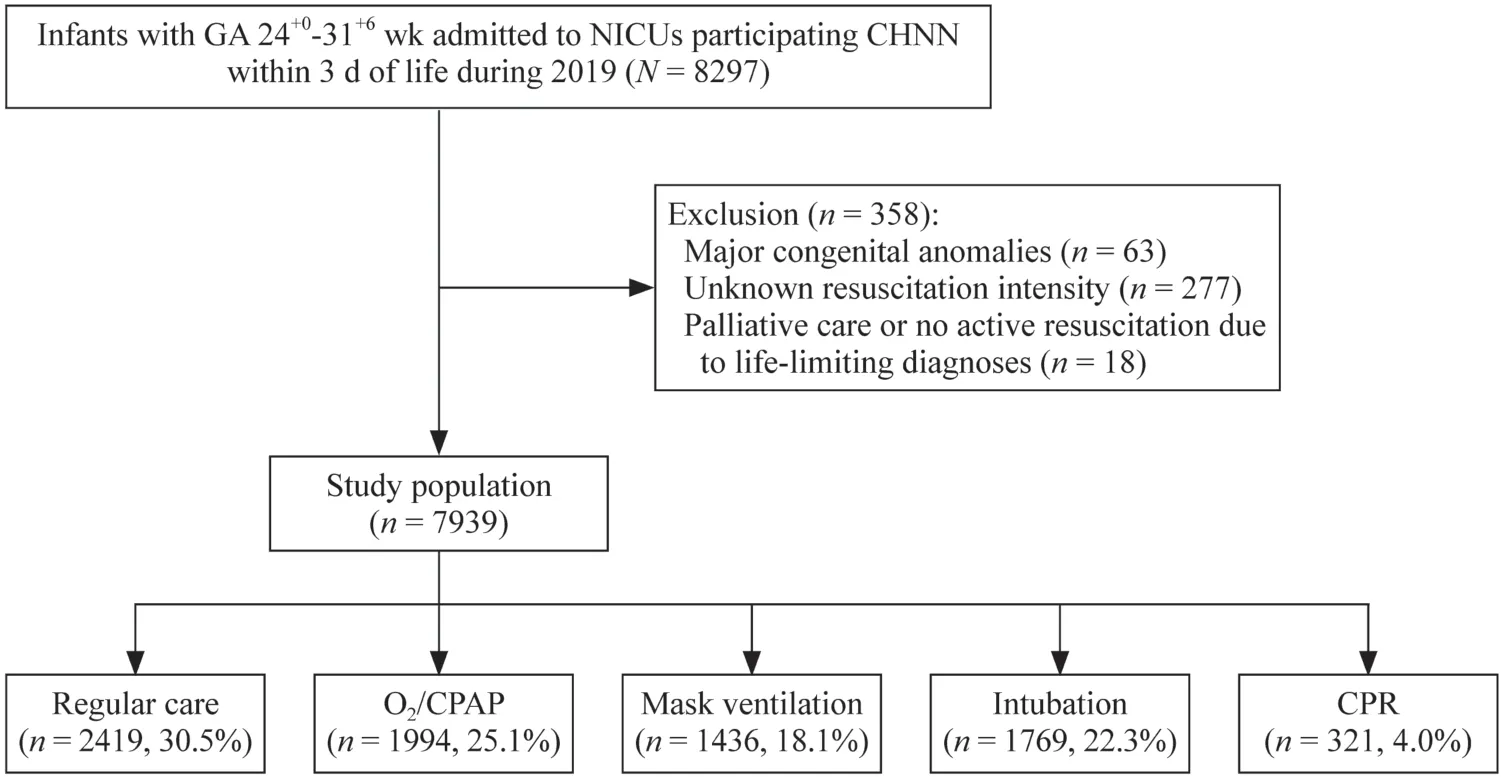
Fig.1 Flow chart for the study population.GA gestation age, NICUs neonatal intensive care units, CHNN Chinese Neonatal Network,CPAP continuous positive airway pressure, CPR cardiopulmonary resuscitation
General population and variation across gestational age
Of 7939 infants included in this cohort, 2419 (30.5%)received regular care without additional resuscitation;1994 (25.1%) received O2/ CPAP; 1436 (18.1%) received non-invasive mask ventilation; 1769 (22.3%) received ETT; and 321 (4.0%) were given CPR.The proportion of the different resuscitation intensities received at each GA is shown in Fig.2.More than half of preterm infants at 24–25 weeks’ GA received endotracheal intubation in the DR, and with the increase in GA, the proportion of endotracheal intubation received gradually declined.Less than 25% of babies born after 29 weeks’ GA received ETT-PPV.In general, the older the GA, the fewer preterm infants receive endotracheal intubation or CPR.
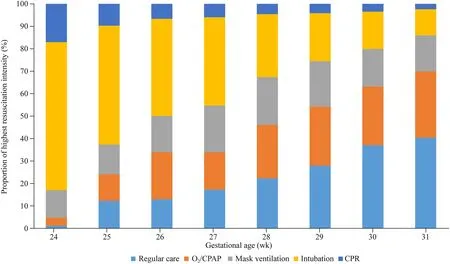
Fig.2 Variation in delivery room resuscitation intensity in China by gestational age of very preterm infants.The X-axis represents gestational age, and the Y-axis represents the proportion of each intensity of resuscitation.Different colors represent different resuscitation intensities.CPAP continuous positive airway pressure, CPR cardiopulmonary resuscitation
Variation across site
The differences in the intensity of resuscitation between the different centers are shown in Fig.3.Resuscitation strategies appear to vary widely among centers, with over 50% of preterm infants in eight (19%) centers requiring the highest intensity resuscitation (endotracheal intubation and CPR).There is also one center with more than 70% of preterm deliveries requiring mask ventilation.The resuscitation intensity in the remaining centers was mostly mild stimulation (CPAP and PPV via mask ventilation).

Fig.3 Variation in delivery room resuscitation intensity among very preterm infants between 24 +0 and 31 +6 weeks’ gestation in CHNN, emphasizing “inborn” infants.The X-axis represents the hospitals participating in this study, and the Y-axis represents the proportion of each intensity of resuscitation.Different colors represent different resuscitation intensities.They were ranked from high to low from left to right according to endotracheal intubation and CPR.CHNN Chinese Neonatal Network, CPAP continuous positive airway pressure, CPR cardiopulmonary resuscitation
Baseline characteristics
Maternal and neonatal characteristics are shown in Table 1.Lower birth weight and GA, lack of ANS, prolonged rupture of membranes, advanced maternal age, and inborn birth were associated with a higher intensity of resuscitation(P< 0.001).Maternal hypertension was significantly associated with a lower intensity of resuscitation.The lower the birth weight and GA, the greater the need for endotracheal intubation; preterm infants who require CPR have the lowest ANS use rate.As the incidence of PROM increases, the need for higher intensity resuscitation in the DR is lessened.
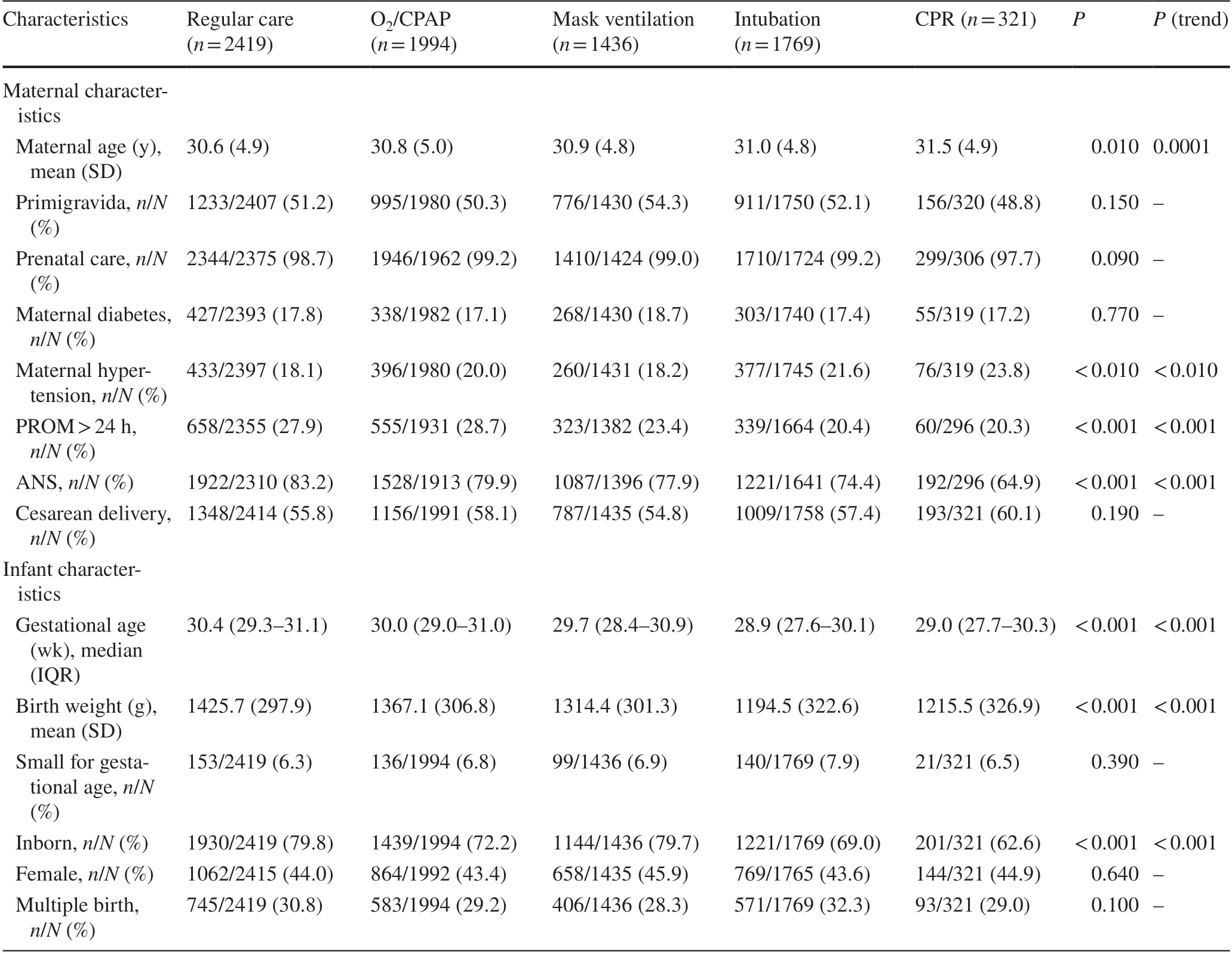
Table 1 Maternal and infant characteristics across resuscitation intensity group among very preterm infants between 24+0 and 31+6 weeks’ gestation in CHNN
Observed incidence of outcomes across groups
Short-term outcomes among preterm infants with different levels of resuscitation are shown in Table 2.The incidence of overall death, early death (≤ 7 days old), severe brain impairment, IVH (grade ≥ 3), pneumothorax, and hypothermia on admission all increase significantly with the increase in theintensity of resuscitation.There was a trend of other adverse short-term outcomes increasing with higher levels of resuscitation, including sepsis, cPVL, and RDS.Because of the missing data because the infants died before the first ultrasound scan, the denominator of IVH ≥ grade 3 was lower than that of RDS or death.
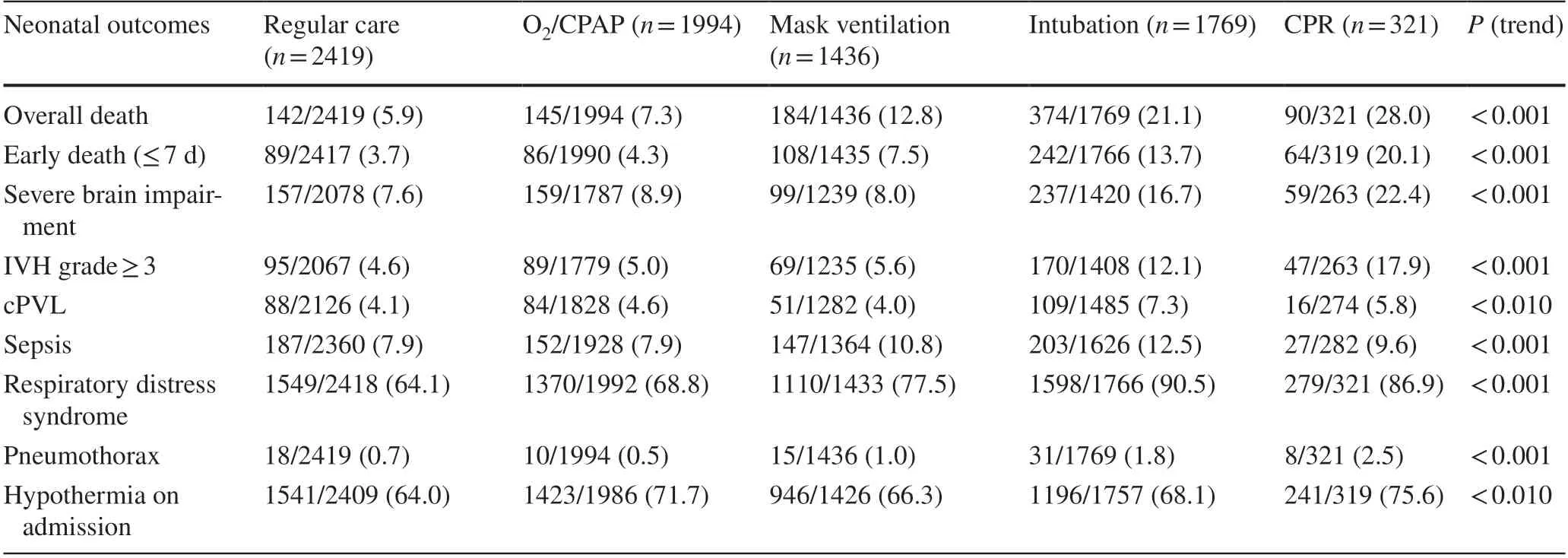
Table 2 Observed rates of neonatal outcomes of very preterm infants between 24+0 and 31+6 weeks’ gestation in CHNN across res uscitation intensity group
The odds ratios between resuscitation intensity and incidence of outcomes
After adjusting for GA, SGA, inborn/outborn status, maternal age, maternal hypertension, PROM > 24 hours, and ANS, multivariate regression analysis showed that the risk of early death and overall death gradually increased with the intensity of resuscitation.CPR greatly increased the risk of early death and overall death.Sepsis and cPVL were highly associated with endotracheal intubation; RDS was highly associated with endotracheal intubation and CPR;IVH (grade ≥ 3) and pneumothorax were related to CPR(Table 3).
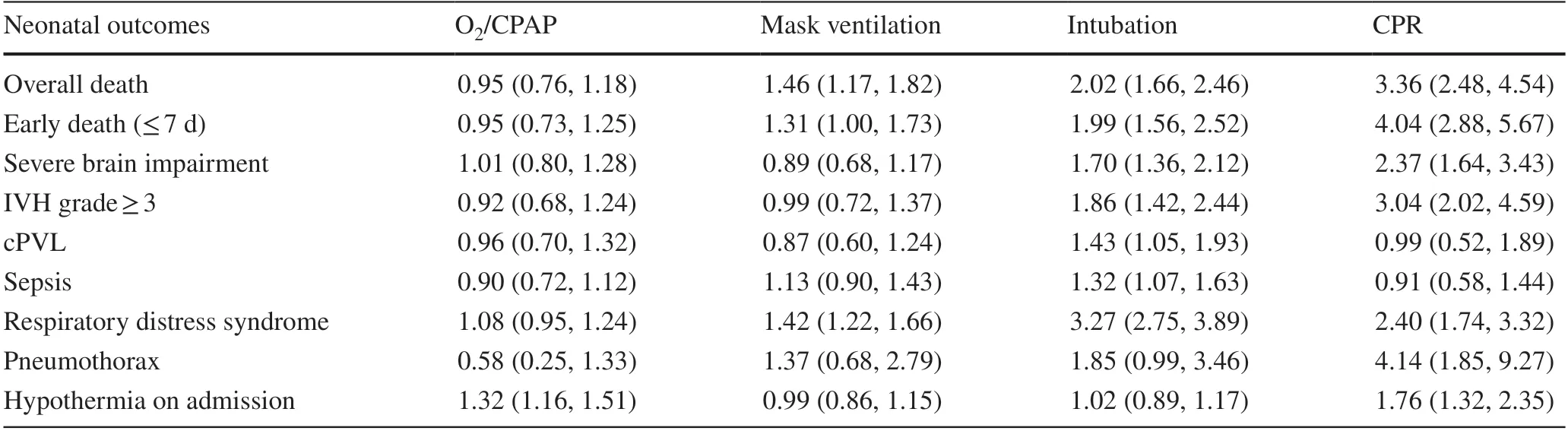
Table 3 Inverse propensity score-weighted adjusted ORa , b (95% CI) of neonatal outcomes across resuscitation intensity group among very preterm infants between 24+0 and 31+6 weeks’ gestation in CHNN
Intensive resuscitation and different gestational ages
Infants were divided into either no intensive resuscitation or intensive resuscitation groups depending on whether they received intubation or CPR (Supplementary Table 1).After adjusting for perinatal factors, including GA, SGA,inborn/outborn status, maternal age, maternal hypertension,PROM > 24 hours, and ANS, multivariate regression analysis showed that short-term outcomes, such as overall death[adjusted odds ratio (aOR) = 1.54, 95% confidence interval(CI) = 1.31–1.82], early death (≤ 7 days old) (aOR = 1.57,95% CI = 1.28–1.91), severe brain impairment (aOR = 1.83,95% CI = 1.48–2.26), IVH grade ≥ 3 (aOR = 1.99, 95% CI =1.55–2.55), cPVL (aOR = 1.53, 95% CI = 1.13–2.06), RDS(aOR = 2.62, 95% CI = 2.16–3.17), and pneumothorax (aOR 2.05, 95% CI = 1.15–3.65), were at increased risk of occurring after intensive resuscitation.
The profiles of extremely preterm infants (24–27+6) and very preterm infants (28–31+6) are shown in Supplementary Tables 2 and 3.Comparing the effects of ventilation of very preterm infants and extremely preterm infants on the outcome shows that extremely preterm infants have a higher proportion of intensive resuscitation for different outcomes,such as overall death or early death and severe brain impairment (IVH grade ≥ 3, cPVL).
Discussion
Resuscitation status and variation in resuscitation intensity across the country
In this research, by understanding the variability of resuscitation across centers, a baseline was obtained to provide a basis for future quality improvement.We will adopt homogeneous management and training to narrow this difference.Our research reveals differences in the intensity of resuscitation of preterm infants at 24+0–31+6weeks of GA in China and provides useful data for resuscitation practices in the DR for extremely preterm infants and very preterm infants.A study by Bajaj et al.showed that 76% of 29+0–33+6weeks’preterm infants received a certain degree of resuscitation in the DR, 14.7% received endotracheal intubation, and 2.7%received CPR [4]; in a study in South Korea, nearly 93% of infants received supplemental oxygen at 29–32 weeks’GA, and 3% received CPR in the DR [15].Boyle et al.reported that 36.9% of infants delivered at 32–33 weeks’ GA received active resuscitation in the DR [16].A multicenter study in northern China showed that the proportion of preterm infants less than 28 weeks of GA and less than 1000 g of birth weight who received endotracheal intubation was 69.5%, and the proportion receiving chest compressions was 18.2% [7].A study on the morbidity and mortality of preterm infants < 32 weeks of GA in China showed that 26.7%received endotracheal intubation [9].In our study, 69.5% of preterm infants at 24+0–31+6weeks received resuscitation in the DR and 22.3% required ETT-PPV without CPR and an additional 4% required CPR, which is higher than studies from other countries and lower than other studies completed in China.However, studies from other countries tended to focus on very preterm infants (and did not include extremely preterm infants).Our research has confirmed the difference in the intensity of resuscitation received for extremely preterm infants and very preterm infants.
In our study, we described that the lower the GA, the higher the intensity of resuscitation needed.When GA was less than 26 weeks, more than 50% of preterm infants received a higher intensity of resuscitation, including endotracheal intubation and CPR.It has been shown in other studies that half of preterm infants at 24 weeks of GA may be able to maintain respiratory stability on DR-CPAP [17].In our study, the proportion stabilized on DR-CPAP was lower (25.1% vs.32.5%) [4].
Our study emphasizes the variation in the intensity of resuscitation of preterm infants “inborn” less than 32 weeks of GA; 26.3% of preterm infants received higher intensity resuscitation, such as endotracheal intubation.Our study includes data from 57 hospitals in 25 provinces across the country.A multicenter study in northern China (including tertiary and secondary hospitals in five provinces and regions) showed that the proportion of preterm infants less than 28 weeks of GA receiving high-intensity resuscitation,such as endotracheal intubation, was 68.4% [7 ].There are obvious differences in the intensity of resuscitation practices in different regions and different hospitals in China.This reminds us that we should carry out targeted training and quality improvement to improve the standardization of resuscitation practices for extremely premature infants and very preterm infants.
Higher intensity of resuscitation results in higher rates of mortality and morbidities
There is a correlation between the mortality of preterm infants and the intensity of resuscitation.The mortality rate of preterm infants in our study was 11.8%, which is lower than previously reported rates in China [18, 19] and similar to the report of Lee et al.in South Korea [20].It is still higher than the 7.4% reported by the Canadian Neonatal Network in 2018 [5].We found that higher mortality rates are associated with preterm infants who received CPR[21–23].As the intensity of resuscitation increases, the mortality rate increases.Our study shows that mortality after CPR is higher than that in the study by Bajaj et al.(28% vs.21%), and the risk of death after CPR is significantly higher than that of other resuscitative measures, especially in the first week of life.Low-intensity resuscitation had a significantly lower mortality rate (CPR 20.1% vs.O2/ CPAP 4.3%).Research by Arnon et al.showed that CPR is an important predictor of death or adverse outcomes [24].
Some studies have shown that severe morbidity(IVH ≥ grade 3 or cPVL) was higher in the CPR group [3,4, 21, 24].Our study demonstrated that DR intubation and CPR were associated with a higher risk of severe IVH among very preterm infants between 24+0and 31+6weeks’ gestation.This finding is also consistent with the large cohort study by Handley et al.[23].In our univariate analysis, we found higher rates of cPVL and sepsis in the CPR group.However, this difference was not signif ciant after adjustment for confounders.This is probably because the neonates who died in the DR were not recorded in the database, causing a bias in the results.
In Table 2, the rates of hypothermia on admission were extremely high, but there was no significant difference.This means that insulation did not perform effectively during the resuscitation process, which we will enhance in future quality improvements.ANS can accelerate fetal lung development and reduce morbidity and mortality in preterm infants between 22 and 34 weeks of GA [17, 25], as well as reduce extensive resuscitation [26].In this research, the use of ANS was 83.2% in preterm infants without resuscitation compared with 64.9% who needed CPR, indicating that ANS reduced the intensity of resuscitation.Identification of high-risk pregnancies will help pediatricians prepare for resuscitation more fully.
Strengths and limitations
The first strength of this study was that we enrolled a very large population of very preterm infants between 24+0and 31+6weeks’ gestation in China.Second, the data collected were rigorously assessed in detail, especially DR resuscitation data.Third, we included all “inborn”infants from fifty-seven hospitals–forty-three hospitals participated in this study, which are widely distributed throughout China, giving a broad overview of resuscitative practices.
This study has some limitations.First, as a retrospective cross-sectional study, it is impossible to trace the specific indications for resuscitation, such as intubation and chest compressions in CPR.Second, this study is an observational study and may not show the impact of interventions on the long-term outcome of preterm infants.Third, because some cases with incomplete data were excluded and the neonates who died in the DR were not recorded in the database, there may be bias in the results.Finally, several differences in DR management of preterm babies in NICUs may affect the final results.
In conclusion, the intensity of resuscitation is associated with an increased risk of death or severe brain injury.The variation in resuscitative practices in different hospitals across China is evident, and to carry out quality improvement and achieve standardized resuscitation, we will use theoretical research, simulation training, and other techniques.
Supplementary InformationThe online version contains supplementary material available at https:// doi.o rg/ 10.1007/ s12519-0 23- 00738-2.
AcknowledgementsThe authors thank the data abstractors and all the staffat the coordinating center for providing organizational support(Lin Yuan, PhD; Tong-Ling Yang, RN; Hao Yuan, RN; Li Wang, RN;Yu-Lan Lu, PhD).
Author contributionsWSL and CC are co-first authors and contributed equally to this work.They contributed to investigation, data curation,and writing of the original draft.GXY contributed to methodology,data curation, formal analysis, and visualization.YZQ and SL contributed to investigation and resources.JSY contributed to methodology and investigation.CY, DLZ, and SJH contributed to supervision,resources, reviewing, and editing.LJQ and YCZ contributed to conceptualization, supervision, reviewing, and editing.The Chinese Neonatal Network contributed to data curation, supervision, and resources.All the authors approved the final version of the manuscript.
FundingNone.
Data availabilityData will be made available on reasonable request.
Declarations
Ethical approvalThis study was approved by the Ethics Committee of the Children’s Hospital of Fudan University (2018–296).Waivers of consent were granted at all sites.
Conflict of interestThe authors have no personal or financial conflicts of interest to disclose.Author Li-Zhong Du is a member of the Editorial Board forWorld Journal of Pediatrics.This paper was handled by the other Editor and has undergone rigorous peer review process.Author Li-Zhong Du was not involved in the journal's review of, or decisions related to, this manuscript.
Open AccessThis article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source,provide a link to the Creative Commons licence, and indicate if changes were made.The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material.If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http:// creat iveco mmons.org/ licens es/ by/4.0/.
 World Journal of Pediatrics2024年1期
World Journal of Pediatrics2024年1期
- World Journal of Pediatrics的其它文章
- Current Mycoplasma pneumoniae epidemic among children in Shanghai: unusual pneumonia caused by usual pathogen
- Expert consensus on the diagnosis, treatment, and prevention of respiratory syncytial virus infections in children
- A comprehensive review of genetic causes of obesity
- Is tuberous sclerosis complex-associated autism a preventable and treatable disorder?
- Influence of preterm birth on the association between gestational diabetes mellitus and childhood developmental vulnerability: a causal mediation analysis
- Neighborhood predictors of short sleep duration and bedtime irregularity among children in the United States: results from the 2019–2020 National Survey of Children’s Health
