Current Mycoplasma pneumoniae epidemic among children in Shanghai: unusual pneumonia caused by usual pathogen
Xiao-Bo Zhang·Wen He·Yong-Hao Gui·Quan Lu·Yong Yin·Jian-Hua Zhang·Xiao-Yan Dong·Ying-Wen Wang·Ying-Zi Ye·Hong Xu·Jia-Yu Wang·Bing Shen·Dan-Ping Gu·Li-Bo Wang·Yi Wang
Mycoplasma pneumoniae(M.pneumoniae), primarily transmitted through respiratory droplets when infected individuals cough or sneeze, is a common cause of communityacquired pneumonia, especially among school-age children and adolescents.The infection occurs endemically with an epidemic peak every few years.The worldwide incidence confirmed by direct test methods was reported to be 8.61%between 2017 and 2020 across all age groups [1].During the coronavirus disease 2019 (COVID-19) pandemic, from 2020 to 2021, the incidence decreased to 1.69% due to nonpharmaceutical interventions (NPIs) [1].Until 2022, despite the relaxation or discontinuation of NPIs, reductions in incidence continued to be seen in 20 countries across Europe,Asia, the Americas, and Oceania [2].In China, there was initially a consistent trend in the number of patients withMycoplasma pneumoniaepneumonia (MPP) both before and after the pandemic [3–6].After that, an unusually different pattern was observed starting in 2021.Typically,M.pneumoniaeinfection presents with symptoms of fever and cough, often accompanied by sore throat, coryza, and occasionally, headache [7].From April 2020 to early December 2022, has been among the strictest, longest approaches to tackling the pandemic anywhere in the world.Such a longterm NPI has caused a potential for more severe respiratory pathogens epidemics due to a so-called immunity debt.With the lifting of NPI policy, China has experienced peaks in influenza viruses, respiratory syncytial virus (RSV), andM.pneumoniaeover the past year.Notably,M.pneumoniaehas undergone a prolonged non-seasonal epidemic, gaining prevalence from April and reaching its peak from October to November.The vast majority of the children, especially infants and preschool children, who have not been exposed to these respiratory pathogens, become a susceptible population that is so large that a sizable unseasonal outbreak occurs when a previously usual respiratory pathogen begins circulating.Therefore, the recently reported spike in respiratory illnesses, especially pneumonia in children is mostly caused byM.pneumoniaeinfection.Additionally, macrolide-resistantM.pneumoniaeinfection also complicates the clinical treatment of this MPP epidemic [8–10].
Shanghai serves as a vital medical hub for the Yangtze River Delta.Here, we provide an overview of pediatric MPP admissions in 36 municipal hospitals in Shanghai and focus on sharing the data from the Children’s Hospital of Fudan University, the Children’s National Medical Center, where a surveillance mechanism was established to monitor MPP transmission in children for the benefit of treating MMP pediatric patients.
Trends of Mycoplasma pneumoniae infection in children admitted to Shanghai municipal hospitals
Data from the Shanghai Hospital Medical Quality Assessment and Improvement Platform, authorized by Shanghai Hospital Development Center, illustrated the trend ofM.pneumoniaeinfection in the last 5 years (Fig.1) as well as the prevalence of respiratory pathogens between January 2023 and November 2023 (Fig.2).In 2019, there were 7859 hospitalized patients with MMP in 36 municipal hospitals, with 1114 patients of severe MPP (SMPP).Amid the COVID-19 pandemic, the absolute number of MPP and SMPP patients sharply declined due to the strict intervention measures implemented.Since 2023, there has been a notable increase, surpassing the previous trend.Moreover,the overall proportion of SMPP is increasing, and there is a trend toward shifting the focus away from children’s specialized hospitals to general hospitals.
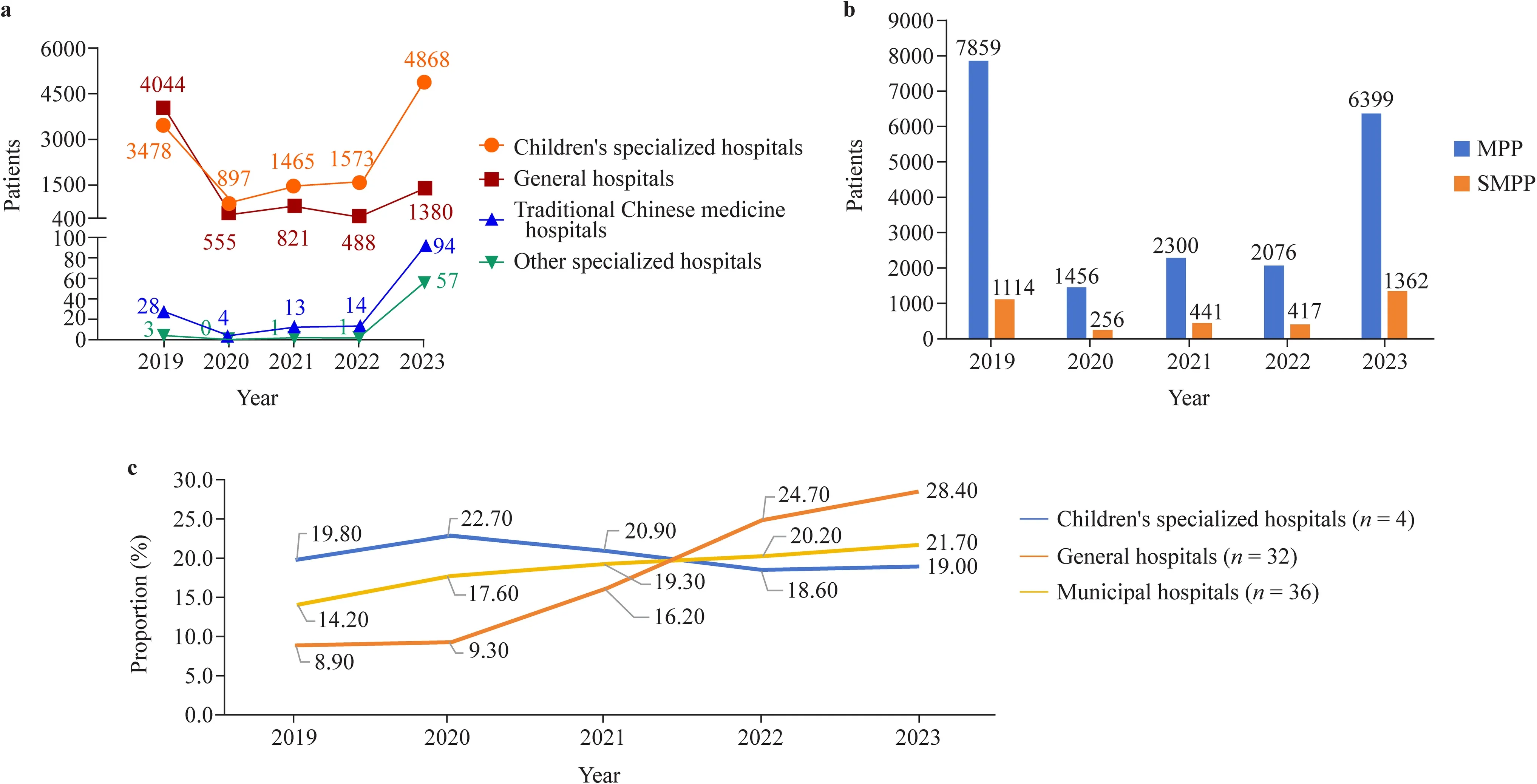
Fig.1 Typical trend of Mycoplasma pneumoniae infection in the last five years.a Hospitalized MPP visits in different types of municipal hospitals; b hospitalized MPP visits categorized by disease severity; c proportion of SMPP visits, illustrating the time trends of pediatric MPP patients from 2019 to 2023.All the data were collected from 36 municipal hospitals in Shanghai.The data for the years 2019–2022 represent the entire year, while the data for 2023 are available for the period from January to September.MPP Mycoplasma pneumoniae pneumonia, SMPP severe Mycoplasma pneumoniae pneumonia
Clinical profiles of Mycoplasma pneumoniae infection
In response to the epidemic and based on the previous experience [11], a dedicated ward in Children’s Hospital of Fudan University was opened for the implementation of standardized diagnosis and treatment protocols.Patients were diagnosed with MPP if they met all the following criteria [12,13]: (1) had evidence of acute respiratory tract infections,accompanied by chest radiography-proven pneumonia [13];(2) a fourfold or greater increase in MP antibody titers of paired sera, or > 1:160 titer of single serum MP antibody, or MP-DNA(+) or MP-RNA(+) [14].The diagnosis of SMPP is made in MPP patients with either of the following criteria:(1) high fever (> 39 °C) for more than 5 days or fever for more than 7 days without a declining trend in peak temperature; (2) hypoxemia (maintained an SaO2< 92% on room air); (3) increasing respiratory and pulse rates with clinical evidence of respiratory distress and exhaustion with or without a raised PaCO2; (4) signs of intrapulmonary infection, such as moderate to large pleural effusion, large area of pulmonary consolidation, plastic bronchitis, pulmonary embolism, necrotizing pneumonia, and acute asthma exacerbations; and (5) signs of extrapulmonary complications,such as meningoencephalitis, ascending (i.e., Guillain-Barré) paralysis, myopericarditis, erythema multiforme,autoimmune hemolytic anemia, hemophagocytic syndrome,or disseminated intravascular coagulation.From August 1,2023, to September 30, 2023, 494 patients with MPP were admitted to the newly opened ward.We analyzed the data of these admitted patients.
Demographic characteristics
Of the 494 admissions, 252 (51%) were males, and 124(25.1%) were classified as having SMPP.The median age was 6 years (interquartile range: 4–9), ranging from 12 months to 13 years.A total of 295 (59.7%) patients were observed in children aged 5 and above, with 78 (26.4%)of these children having SMPP.Among 199 MPP patients under 5 years, 46 (23.1%) patients had SMPP.Eighty-seven(43.7%) MPP patients were under 3 years old, with 19(19.5%) of them having SMPP.This revealed thatM.pneumoniaeinfection is still reported as somewhat uncommon in children under 5 years of age, as was shown in an earlier study [15], but a growing trend of incidence in younger children under 5 years of age can be observed, as in recent reports before the COVID-19 pandemic [16].
Symptoms and signs
A total of 489 (99%) patients presented fever.Among them,372 (76.1%) experienced high fever (≥ 39 °C), while 105(21.5%) had extremely high fever (≥ 40 °C).The average duration of fever across all grades was 9.21 ± 6.93 days.Based on pulmonary auscultation, wet rales were detected in 254 (51.4%) patients, whereas dry rales were present in 39 (7.9%).Wheezing was observed in 43 (8.7%) patients,and in 11 (2.2%), shortness of breath was reported.Among seven (1.4%) patients with dyspnea, five presented "three depression signs” (supraclavicular fossa, suprasternal fossa,intercostal space).
Among the MPP patients, 367 (99.2%) had a high fever(≥ 39 °C), and 73 (19.7%) experienced an extremely high fever (≥ 40 °C).The average duration of fever in this group was 8.92 ± 6.97 days.A total of 171 (46.2%) patients had wet rales, whereas 27 (7.3%) patients had dry rales.Twenty-nine(7.8%) patients reported wheezing.Of the SMPP patients,122 (98.4%) had a high fever (≥ 39 °C), with 46 (37.1%)experiencing an extremely high fever (≥ 40 °C).The average duration was 10.15 ± 7.98 days.Wet rales were found in 83 (66.9%) patients, while 12 (9.7%) patients exhibited dry rales.Fourteen (11.3%) patients had wheezing.
Laboratory characteristics
All patients underwent the following laboratory tests during their hospital stay: complete blood counts, C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, etiological indicators, and specific immunological indicators.Pulmonary injuries associated with refractory MPP or SMPP occur owing to excessive host immune responses rather than direct microbial damage.LDH is generally considered to be a reliable biomarker of refractory MPP [9], and D-dimer and CRP are statistically significant biomarkers to predict refractory MPP in Chinese pediatric patients [17].MPP patients with higher levels of D-dimer had more severe clinical manifestations [18], and they were more likely to develop refractory MPP [19].According to the data collected in our hospital, SMPP patients tended to have higher CRP levels than non-SMPP patients (10.76 vs.7.77;P< 0.05), while the levels of Ferr and interferon-γ showed no significant difference between the two groups.Out of 264 (49.8%)patients with abnormal LDH levels, 80 (64.5%) had SMPP,and 166 (44.9%) had non-SMPP.The average LDH value for patients with SMPP was 434 ± 245 U/L.while the average LDH value for non-SMPP patients was 373 ± 74.0 U/L.Furthermore, 136 (27.5%) patients exhibited elevated levels of D-dimer, with 55 (44.4%) having SMPP and 81 (21.9%)having non-SMPP.The average D-dimer value for SMPP patients was 1.55 ± 1.60 mg/L, whereas the average D-dimer value for non-SMPP patients was 0.913 ± 0.424 mg/L.
AlthoughM.pneumoniaeculture is the gold standard for diagnosis, due to the special culture conditions and slow growth, it is not implemented forM.pneumoniaedetection.The greatest number of positive tests was obtained with direct test methods followed by a combination of PCR and serology or serology alone (only immunoglobulin M was considered if all isotypes were reported).Moreover, compared with non-SMPP patients, SMPP patients had a higher number of MP-DNA copies.
Complications and concomitant infections
Of 124 (25.1%) patients experiencing intrapulmonary complications, pleural effusion (n= 123, 24.9%) was most common, followed by acute asthma exacerbations (n= 12, 2.4%),plastic bronchitis (n= 5, 1.0%), and necrotizing pneumonia(n= 5, 1.0%).Furthermore, we identified five patients of secondary pulmonary embolism, a less common occurrence in infection-acquired thrombophilic states [20, 21].This highlights the need for increased awareness in patients where chest pain persists despite therapy, especially in the absence of tachypnea and hypoxemia.Extrapulmonary complications were also noted, with secondary liver dysfunction being the most prevalent (n= 26, 5.3%).Complications affecting the nervous system, circulatory system, and blood system were each less than 1%.Additionally, 240 patients exhibited T-cell immune dysfunction, and among them, 68 (54.8%)had SMPP.
Real-time-polymerase chain reaction was conducted on nasal swabs to detect the presence of respiratory pathogens, including adenovirus (ADV), rhinoviruses (RV),human bocavirus (HBoV), parainfluenza virus (HPIV),RSV, metapneumovirus (HMPV) and influenza A and B viruses.Influenza A virus and ADV were more commonly to be detected withM.pneumoniae[22].Strong and highly statistically significant antagonistic interspecies interactions were detected betweenM.pneumoniaeand influenza virus infections [23].Of our 499 MPP patients, seven (1.4%) were found to have concurrent bacterial infections, among whichStreptococcus pneumoniaecoinfection (n= 5, 1.0%) was the most prevalent, followed byStaphylococcus aureus(n= 2,0.4%) andPseudomonas aeruginosa(n= 2, 0.4%).Moreover, 13 patients were infected with influenza A, 40 with ADV, 28 with HBoV, 70 with RV, 30 with HPIV, 25 with HMPV, 13 with H3N2, and 29 with RSV.SMPP patients were more likely to be coinfected with RV than non-SMPP patients, but the coinfection situation with other viruses was not different between the groups.
Treatment of Mycoplasma pneumoniae pneumonia
According to the guidelines, the priority treatment forM.pneumoniaeinfection is macrolide antibiotics, which can also be prescribed for patients with clinical findings.Nevertheless, due to the absence of a cell wall, a characteristic that setsMycoplasmaapart from other pathogenic bacteria, the use of appropriate antibiotics may not always lead to the resolution of symptoms, and the widespread use of macrolides have also caused treatment resistance [9, 24].Therefore, macrolide-resistantM.pneumoniaehas become increasingly prevalent.From 2016 to 2019, the reported resistance rate was approximately 80%–90% in Asian countries, including China, Japan, and South Korea [25–27].In some cases, patients may experience persistent fever and clinical deterioration, which can even progress to severe disease [28, 29].As a result, quinolones and tetracyclines, in addition to other regimens such as corticosteroids and immunoglobulin, can be considered alternative treatment options for macrolide-resistantM.pneumoniae.Our hospital commenced testing for resistance genes A2063G and A2064G in MPP patients concerning the use of macrolide antibiotics in June 2023.A total of 434 MMP patients underwent these tests, yielding a resistance gene positivity rate of 80%.Among the 124 SMPP patients, 97 (88.2%) tested positive,a significantly higher rate compared to non-SMPP patients.Out of the 494 MPP patients, 155 (31.3%) patients received specific quinolones or tetracyclines, with 71 (57.2%) of them being SMPP patients.
Mechanism behind the surge of respiratory infections in children: pandemic-related immunity gap or others?
We conclude that both the “see-sawing” features and“upsurging” patterns have been observed inM.pneumoniaeinfections, indicating that a notable increase in MPP cases among children may be imminent.Immunity debt take effects in the current unusualM.pneumoniaeinfection in children in China.“Immunity debt” is defined as a paucity of protective immunity raises concerns regarding susceptibility to infectious diseases [30].Previously, an immunity debt was observed during the 2009 H1N1 influenza pandemic on RSV seasonality.A delayed onset of the RSV epidemic occurred initially, followed by a subsequent surge in the following year [31].Similarly, children’s lack of exposure to various infectious pathogens during the COVID-19 pandemic lockdown has an impact on their developing immunity.It has been reported that innate immune cells, which are a critical part of the immune system activated to battle COVID-19,remain altered for at least a year after infection [32].This finding suggests that these cells may play a role in some of the lingering symptoms associated with long COVID-19,and other studies also revealed that T cells and inflammatory factors in the body remained at elevated levels [8, 33].The immunological mechanisms of SMPP and the activation of related cells following COVID-19 infection, along with elevated levels of inflammatory factors, are connected and warrant further investigation.This is not clear, and more studies are needed to confirm the connection.T-cell activation, cell-mediated inflammatory damage, and cytokinedriven proinflammatory environments in the respiratory tract are essential immunological mechanisms that induce SMPP[34].
In conclusion, since June 2023, Shanghai has experienced peak epidemiology inM.pneumoniaeinfection.Severe clinical manifestations were more frequently observed.The strains are mainly macrolide-resistantM.pneumoniae, which increases the difficulty of treatment.Delayed effective antimicrobial treatment is associated with prolonged and/or more severe disease.The appropriate prescription of antibiotics, as well as the rapid and accurate diagnosis of MPP, is helpful for patient treatment.Advocating disease awareness within the community and among healthcare professionals is beneficial.Establishing a standardized and practical monitoring system for respiratory pathogens, including influenza viruses, respiratory syncytial viruses,M.pneumoniae, and adenoviruses, is crucial.The system can offer timely and scientific evidence for developing a global strategy on infection prevention and control.Early case detection enables prompt treatment, ultimately reducing the severity and mortality rates.
AcknowledgementsWe would like to thank SNAS for their kind editing service with our manuscript.
Author contributionsZXB and HW contributed equally as co-first authors.ZXB contributed to methodology, funding acquisition, reviewing and editing.HW contributed to investigation, formal analysis, data curation, writing of the original draft.GYH contributed to methodology.LQ, YY, ZJH, DXY, and GDP contributed to data curation.WYW contributed to reviewing and editing.YYZ contributed to data curation.XH contributed to supervision.WJY contributed to formal analysis and data curation.SB contributed to data curation and investigation.WLB contributed to conceptualization, methodology and project administration.WY contributed to conceptualization, methodology and supervision.All authors approved the final version of the manuscript.
FundingThe study was funded by the Science and Technology Commission of Shanghai Municipality (No.21511104502), and Shanghai Hospital Development Center (No.SHDC22022221).
Data availabilityThe datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approvalNot needed.
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.The authors have no conflict of interest to declare.
 World Journal of Pediatrics2024年1期
World Journal of Pediatrics2024年1期
- World Journal of Pediatrics的其它文章
- Expert consensus on the diagnosis, treatment, and prevention of respiratory syncytial virus infections in children
- A comprehensive review of genetic causes of obesity
- Is tuberous sclerosis complex-associated autism a preventable and treatable disorder?
- Influence of preterm birth on the association between gestational diabetes mellitus and childhood developmental vulnerability: a causal mediation analysis
- Delivery room resuscitation intensity and associated neonatal outcomes of 24+0–31+6 weeks’ preterm infants in China:a retrospective cross-sectional study
- Neighborhood predictors of short sleep duration and bedtime irregularity among children in the United States: results from the 2019–2020 National Survey of Children’s Health
