The effect of intelligent management interventions in intensive care units to reduce false alarms: An integrative review
Bingyu Li ,Liqing Yue ,* ,Huiyu Nie ,Ziwei Co ,Xioy Chi ,Bin Peng ,Tinge Zhng ,Weihong Hung
aTeaching and Research Section of Clinical Nursing,Xiangya Hospital of Central South University,Changsha,Hunan,China
b Xiangya School of Nursing,Central South University,Changsha,Hunan,China
c“Mobile Health” Ministry of Education -China Mobile Joint Laboratory,Xiangya Hospital of Central South University,Changsha,Hunan,China
Keywords:
ABSTRACT Objective:In intensive care units (ICU),frequent false alarms from medical equipment can cause alarm fatigue among nurses,which might lead to delayed or missed responses and increased risk of adverse patient events.This review was conducted to evaluate the effectiveness of intelligent management interventions to reduce false alarms in ICU.Method: Following the framework of Whitmore and Knafl,the reviewers systematically searched six databases: PubMed,EMBASE,CINAHL,OVID,Cochrane Library,and Scopus,and studies included intelligent management of clinical alarms published in the English or Chinese language from the inception of each database to December 2022 were retrieved.The researchers used the PICOS framework to formulate the search strategy,developed keywords,screened literature,and assessed the studies’quality using the Joanna Briggs Institute-Meta-Analysis of Statistics,Assessment,and Review Instrument (JBI-MAStARI).The review was preregistered on PROSPERO (CRD42023411552).Results:Seven studies met the inclusion criteria.The results showed that different interventions for intelligent management of alarms were beneficial in reducing the number of false alarms,the duration of alarms,the response time to important alarms for nurses,and the alarm fatigue levels among nurses.Positive results were found in practice after the application of the novel alarm management approaches.Conclusion:Intelligent management intervention may be an effective way to reduce false alarms.The application of systems or tools for the intelligent management of clinical alarms is urgent in hospitals.To ensure more effective patient monitoring and less distress for nurses,more alarm management approaches combined with artificial intelligence will be needed in the future to enable accurate identification of critical alarms,ensure nurses are responding accurately to alarms,and make a real difference to alarm-ridden healthcare environments.
What is known?
· Alarm fatigue is a common phenomenon in hospitals,which causes nurses to feel nervous or stressed and distrustful of the alarm system,thus delaying a response,ignoring,muting,or turning off alarms.
· Due to the high frequency and consequences of alarm-related adverse events,alarm management has been highly concerned and widely investigated.
What is new?
· Intelligent management interventions can reduce the total number and duration of alarms and false alarms in an alarmridden environment,minimize response time to important alarms for nurses,and reduce alarm fatigue among nurses.
· The intelligent interventions are effective in reducing alarms,but the magnitude of the effect is uncertain.Accuracy of alarm signals also remains to be confirmed.
· More studies are needed to apply artificial intelligence combined with alarm management to the clinical setting.
1.Introduction
A clinical alarm is a notification from a medical device used to diagnose,treat,or monitor a patient [1].It is an audible or visual signal to alert healthcare professionals that patients’ physiological parameters are outside of the set limits or that a device dysfunction exists.According to studies,there were an average of 43 alarms per hour in the Intensive Care Unit (ICU),52.8% of which were multiparameter monitor alarms,42.5% of the alarms were unanswered,and only about 6.4% of the alarms were related to clinical physiological changes in the patients [2].The generation of alarms is related to changes in patients’ conditions,as well as to the sensitivity of the monitoring and treatment equipment.The occurrence of a plethora of alarms often lies in the inability of healthcare professionals to set the correct range of alarm thresholds according to the individual patients,and insufficiently regular maintenance of the instruments leading to intermittent failures such as sensors or cables [3,4].As a result,multiparameter monitors can generate a large number of clinical alarms,but most are technically false or clinically irrelevant alarms,and very few of them reflect changes in the patient’s condition that require nurses’ management or intervention.The high frequency of alarms can easily lead to alarm fatigue among healthcare professionals.In addition,these alarms may endanger patients’ lives if they are not handled promptly.Therefore,hospital administrators and health professionals need to prioritize the 6.4%of clinical alarms related to clinical physiological changes in patients.
Alarm fatigue is a common phenomenon in hospitals,where frequent clinical alarms and a high percentage of false alarms cause nurses to feel overloaded or less sensitive to alarms,nervous and stressed,and distrustful of the alarm system,thus delaying a response,ignoring,muting or turning off alarms [4,5].The Joint Commission on Accreditation of Healthcare Organizations(JCAHO)reported 98 alarm-related adverse events from 2009 to 2012,including 80 cases of deaths,13 cases of permanent loss of function,and 5 cases of patients with prolonged hospital stays [6].Safety risks will occur when nurses manage alarms poorly,reducing or delaying the observation and management of patients’ conditions,and it causes nurses to miss important alarms,delaying the treatment of patients and threatening their lives [7].
Due to the high frequency and consequences of alarm-related adverse events,JCAHO ranked alarm management as the first patient safety goal for hospitals from 2014 to 2016 [8,9],and it also mentioned that hospitals should focus on managing the clinical alarm systems that have the most direct relationship to patient safety in 2023 National Patient Safety Goals [10].Alarm management is a series of interventions for medical devices and their alarms to reduce the total number of alarms or improve the positive predictive value of alarms and/or prevent false negatives [11].For alarm management,the American Association of Critical-Care Nurses (AACN) published an evidence-based practice on recommended nursing practices,which includes providing proper skin preparation for electrocardiogram (ECG) electrodes (Evidence B),providing initial and ongoing training on alarm equipment (Evidence E),and creating interprofessional teams to address alarm issues(Evidence E)and so on [12].Alarm management has been a matter of great concern and widely investigated [13].
Several clinical investigations and trials have identified solutions to the alarm problem.Fujita et al.adopted evidence-based transformation strategies to reduce alarms by changing default settings,alarm setting education,and accountability [14].A trial showed that alarm management in the ICU was very complicated.Changing the default alarm settings and standardizing the use of training monitors were not sufficient to improve the security of alarm systems [15].Studies reported that significant reduction in the number of clinical alarms and a significant improvement in nurses’ alarm fatigue with different alarm management strategies [16-19].However,excessive amounts of clinical alarms may be the result of multiple factors.Alarm management solely through evidence-based interventions or training healthcare professionals to change their perceptions does not adequately address the high number of false alarms,alarm fatigue among healthcare professionals,and the low positive predictive value of alarm systems [20].The risks resulting from alarms generated by various devices that are not handled promptly would be mitigated if some technical measures can be adopted,such as intelligent devices to reduce the number of false alarms,identify critical alarms,and notify healthcare professionals to respond in a timely manner.
In the information-based medical environment,medical devices’software and hardware technologies are constantly evolving,and the accumulated alarm data in ICUs is increasing.This situation has laid the foundation for optimizing alarm management using Internet technology.To further enhance alarm management,the 2015 Physionet Challenge proposed that the use of expert-defined rule-based logic to analyze patient physiological signals through Internet of Things(IoT)technology could effectively reduce the rate of false alarms for cardiac arrhythmias [21].A large number of studies have emerged that use approaches with artificial intelligence to solve alarm problems,such as the use of information systems to integrate different types of alarms to reduce the number of false alarms,the use of wearable smartwatches to receive alarms timely so that they can be dealt promptly,and the use of information in different colors in displays to remind nurses to response.New options for alarm management may improve patient safety [22].Healthcare professionals believe that the use of artificial intelligence in ICUs will help identify complications early and decrease the risk of death [23].
Interventions for intelligent alarm management based on Internet technology have begun to be explored,but there are no guidelines or consensus to demonstrate that any type of intelligent management intervention will consistently improve the problem of nurses receiving large numbers of alarms.Therefore,this review aims to evaluate the effect of intelligent management interventions in ICUs to reduce clinical alarms,including the reduction of excessive,false,and non-actionable alarms.
2.Methods
2.1.Protocol and registration
Because of the uncertainty of the effects of individual studies,aggregating the results of many different individual studies,and synthesizing and evaluating them can have effects that exceed the power that individual studies possess [24].Various types of studydesigns were includ ed in the integrative review, including quantitative studies and mixed studies. This paper presented an integrative review to examine the effectiveness of intelligent management of alarms in ICUs based on the framework of Whitmore and Knafl [25]. Following the methodology of Whittemore and Knafl, the manuscript proceeded in five consecutive steps: (a)problem identification, (b) systematic literature search, (c) data evaluation,(d) data analysis,and (e) presentation of findings.
The review protocol was prospectively registered in the International Prospective Register of Systematic Reviews (PROSPERO):CRD42023411552.The review was reported according to the PRISMA checklist [26].
2.2.Problem identification
The review was guided by two research questions.(a) What intelligent management interventions have been applied in existing studies to reduce false alarms in ICUs? (b) how effective were these interventions in reducing false alarms?
2.3.Literature search
We conducted a comprehensive and systematic search of six electronic databases,including PubMed,EMBASE,CINAHL,OVID,Cochrane Library,and Scopus.The comprehensive search strategies for electronic databases were used to retrieve articles for intelligent management of alarms.Published articles from the inception of each database to December 2022 were searched to obtain comprehensive evidence.The researchers identified the initial keywords,analyzed the text words contained in the headings,determined the keywords based on the Medical Subject Headings (MeSH)in conjunction with the synonyms of the terms used in the retrieval database,and evaluated the applicability of the draft English keywords created by an expert in alarm management and an expert in artificial intelligence based on the PICOS framework.P (Population):nurses,nursing students,health professionals,health personnel;I (Intervention): intelligent alarm management,smart alarm management;C (Comparator): routine alarm management,intelligent alarm management measures not used;O (Outcomes):the primary outcomes: reduction in the number of false alarms;and the secondary outcomes:the reduction in alarm fatigue among nurses,the reduction in the duration of alarms and time to respond important alarms;S (Study design): randomized controlled trials,non-randomized controlled trials,quasi-experimental studies,before and after studies,prospective and retrospective cohort studies,case-control studies (more details in Appendix A).
Afterward,the keywords for which the experts’agreement had been obtained were used to search the databases.By using keywords and index terms,a systematic search was taken using the Boolean operators “OR” and “AND ”.The search terms included(Nurs*OR Nurse OR Nursing OR Nurses OR healthcare professional OR health personnel) AND (management OR smart management OR intelligent management OR quality improvement)AND(clinical alarms OR physiological alarms OR monitor alarms OR patient monitoring alarms OR false alarms OR nuisance alarms) OR alarm fatigue.The reference lists of included articles were also searched to identify any further studies.
Studies that met the following inclusion criteria were included:(a) articles in English or Chinese,(b) any form of intervention for intelligent alarm management that can reduce the number of false alarms,nonactionable alarms,and nuisance alarms,(c) studies conducted with patients (adults,children,neonatal) or simulated patients,(d)studies in ICUs or simulated ICUs,and(e)alarms were generated by multiparameter monitors,physiological monitors.
The exclusion criteria were as follows: (a) unpublished papers,editorials,opinions,or discussions,(b)non-original data,(c)studies focused on models or algorithms developed in the laboratory that have not been applied in the hospital or a simulated hospital environment,(d)studies focusing on detection of alarms generated by a single alarm,and (e) the outcomes of studies focus on improvement of the true positive rate,true negative rate,false positive rate,false negative rate.
2.4.Data evaluation
All retrieved studies were imported into EndNote v.20 software to exclude duplicates [27].Two reviewers (BL and BP) independently screened the titles and abstracts of the studies to evaluate their eligibility.If there was a difference of opinion between the two reviewers,a discussion was made with the third reviewer(TZ).Finally,all the studies identified were screened and evaluated.
The Joanna Briggs Institute-Meta-Analysis of Statistics,Assessment,and Review Instrument (JBI-MAStARI) was used to evaluate the quality of the articles intended to be included in the review by three independent reviewers(BL,BP and TZ)[28].The studies were evaluated as follows: randomized controlled studies (1.c),quasiexperimental studies (2.c),and pretest-posttest studies (2.d).The tools used were as follows: the checklist for randomized controlled trial of the Joanna Briggs Institute Assessment and Review Instrument has 13 items,including internal truthfulness,truthfulness of statistical findings,and further subcategorization of the items into selection and allocation,intervention/exposure management,outcome measures,and participant loss to visit.The checklist for the quasi-randomized controlled trial of the Joanna Briggs Institute Assessment and Review Instrument has 9 items that evaluate the overall quality of class experimental studies in terms of causality of study variables,baseline,control,measurement of outcome indicators,and analysis of data.Researchers made “yes,” “no,” “unclear,” and “not applicable” judgments for each of the evaluation items.Three reviewers checked whether the evaluated studies were consistent with the statements in the checklist.One point would be awarded for a“yes”answer to the items,and no points for the rest of the cases.The results of the quality evaluation of the included studies are shown in Appendix B.
2.5.Data abstraction and synthesis
Two reviewers (BL and BP) examined and analyzed independently the included studies.Detailed characteristics of the studies identified were presented in a table with the following data categories: first author,year of publication,country,type of study,method,setting,and main findings of the study.This table was used to compare and synthesize the results of these studies,including similarities and differences across studies.
3.Results
3.1.Search outcome
The initial search of the six databases yielded a total of 2,325 publications.After removing duplicates,the abstracts of the 1,735 obtained documents were reviewed.Two reviewers removed studies that were inconsistent with the theme of the research and independently reviewed the titles and abstracts of citations according to inclusion and exclusion criteria.In addition,two studies were found in the literature references.After reviewers read the full text of 347 papers,a total of 7 articles were finally included in the integrative review(Fig.1).
3.2.Description of included studies
The included studies were from the United States of America(USA)(n=6)and the Netherlands(n=1).Studies methodologies:randomized controlled trial (n=1),uncontrolled before and after design(n=5),observation,and Quasi-experimental study(n=1).All of the interventions were performed in the hospital or hospital simulation:neonatal intensive care unit(NICU)(n=1),ICU(n=1),surgical progressive care unit (n=1),acute care cardiology unit(ACCU) (n=1),cardiovascular surgical intensive unit (CSICU)(n=1),and acute care hospital unit simulation(n=2).The majority of interventions in studies included changes in alarm notification,updated alarm technology,measures related to reducing the number of clinical alarms,response time for nurses to respond to important alarms,and nurses’ alarm fatigue.A summary of these studies is provided in Table 1.
3.3.Details of interventions
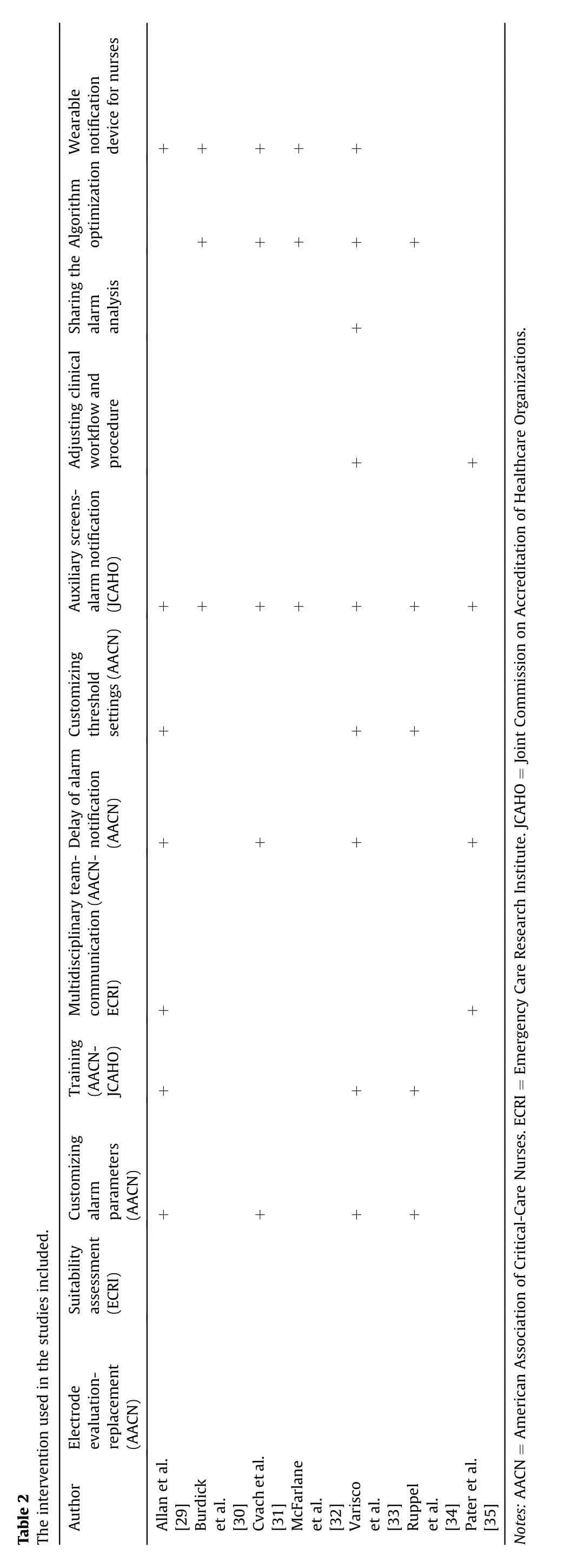
The seven studies included in this review show that alarm technologies have been updated and upgraded in recent years.Alarms from monitors need to be sent through a centralized monitor to an emergency server,then from the emergency server to a centralized server,and then from the centralized server to the handheld device.After the algorithm upgrade,alarms from the monitor only need to go through one server to process the alarm,and the handheld device can display the alarm message and is also allowed to display the waveform of the signal.After a second system upgrade,the alarm signal can be accessed in real-time on the handheld device [29-35].Not only that,the intelligent means of alarm management have also transitioned from pagers to customized software for smartphones and smartwatches developed by different research teams [29,30,35].In addition,the upgraded alarm system can send alarms to different people and different devices at different times.A red alarm is forwarded to a nurse’s handheld device,and if that nurse does not respond within 45 s,the alarm is forwarded to a pre-identified fellow nurse[33].In another study,alarm signals for cardiac monitoring were sent to a separately confirmed pager,while voice communications and all other clinical communication alarms (e.g.,nurse call alerts: toilet assist,ventilator alert,code blue) were sent to the nurse’s Wi-Fi phone [29].
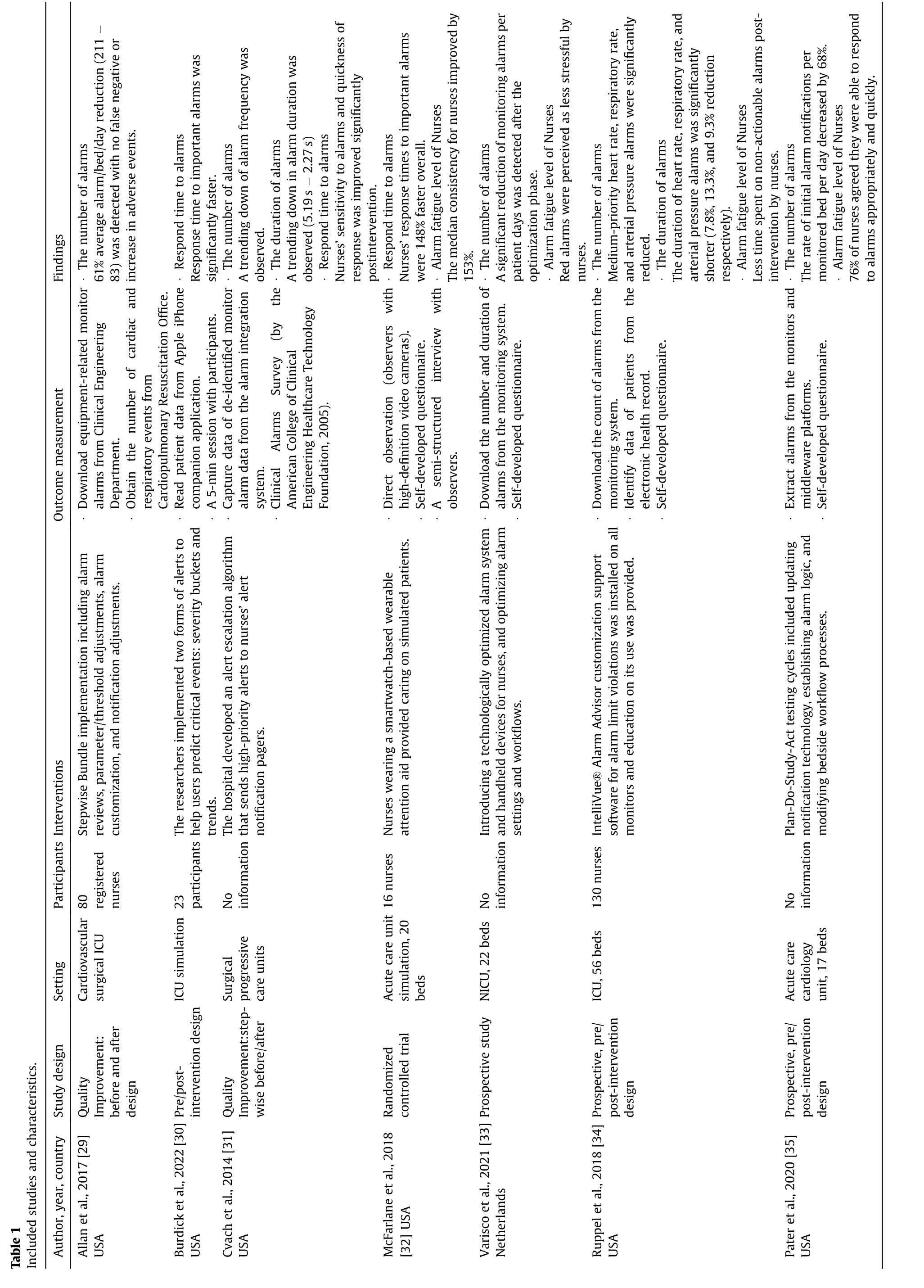
Three studies provided self-designed applications or software [30,34,35],all of which used sensory features to varying degrees.Visual notifications appeared on monitors installed with customized software [34] when repeated alarms from nurses for the same infraction were triggered and muted for a specified period.Audible notifications and touch notifications are sent to specific nurses when the smartphone sends different alerts with different seconds of delay [35].Simultaneous visual,tactile,and auditory alerts can be used in a multisensory application to provide tri-modal alarms among patients.
Five studies provided interventions for more than two months [29,31,33-35],while two of the remaining tested in simulated settings for less than one day [30,32].Two studies provided only interventions for the intelligent management of clinical alarms [27,29],and five studies also provided other measures such as changing processes,changing default thresholds,staff education,delaying the time for alarms [29,31,33,34] (Table 2).Only one study followed up on the intervention and sustained it for eight months [29].
3.4.Effects of intervention
3.4.1.Reduction of the number of false alarms
Five studies examined the number of clinical alarms after the intervention,and all five studies reported a significant reduction in clinical alarms [29,31,33-35].Allen et al.reported a reduction in the average number of alarms per monitored bed from 211 to 83 per unit,a 61% reduction in the number of alarms after project implementation was completed [29].Pater et al.implemented interventions such as delaying high and low oxygen saturation (SpO2) alarms,modifying registered nurse (RN) escalation algorithms,and introducing new alarm systems,resulting in an average reduction of initial alarm notifications to 22.4 per monitoring bed per day.This meant a total decrease of 68%within the expected intervention period [35].
The types and priorities of alarm reduction were not consistent when using different alarm intelligent management interventions.Two of the studies considered the number of different types of alarms [33,34].The number of SpO2alarms was also significantly reduced by optimizing the workflow and handling architecture of alarms[33].In Rupple’s analysis of weighted alarm data by alarm types using alarm advisor to process alarms,a significant reduction was found for respiratory,heart rate,and arterial pressure alarms,while there was no change in SpO2alarms [34].Two studies considered the prioritization of alarms [33,34].Alarms in the NICU were classified into three different levels of priority,which include red (critical),yellow (alerting),and blue (technical) alarms [33].Implementation of the new alarm management system resulted in a significant reduction in the number of all red monitoring alarms (SpO2≤80% alarms),at the expense of an increase in 80% <SpO2≤88% alarms (yellow alarms) [33].The implementation of the Alarm Advisor software resulted in a significant reduction in the average number of all medium-priority alarms (yellow,warning) compared to the preimplementation period [34].
3.4.2.Reduction of the duration of alarms
Three studies reported the duration of alarms in the process of intelligent management of alarms[31,33,34].Cvach et al.reported a more significant decrease in the slope of average daily alarm duration in units where the nurse manager responsible for responding to all alarms was equipped with a pager than in units where the nurse manager responsible for responding to all alarms was equipped with a pager[31].Varisco et al.analyzed the duration of different types of alarms and found that the duration of red and yellow monitoring alarms and alarms associated with SpO2decreased during each nurse’s use of the handheld device to receive alarms,but the duration of bradycardia and heart rate alarms remained similar.Also,the duration of parallel alarms was lower during this phase in all cases [33].Duration of heart rate,respiratory rate,and arterial blood pressure alarms were significantly reduced,but the duration of SpO2alarms was not,after using the custom software Alarm Advisor.The total duration of all mediumand high-priority alarms did not decrease either [34].
3.4.3.Reduction in nurses’ response time to important alarms
Two studies examined the time for nurses to respond to alarms after the intervention[30,32].The time nurses responded to alarms was improved (relatively shorter response times) when using the Human Alerting and Interruption Logistics -Clinical Alarm Triage (HAIL-CAT) wear-able compared to the control condition.Wearing an attention-aid device,nurses could use the device to categorize alarms and respond quickly to patients when critical situations occur[32].Response time for solo alarms was slower than primary co-alarms and faster than secondary co-alarms [30].
3.4.4.Alarm fatigue level of nurses
All seven included studies used questionnaires or semistructured interviews to investigate nurses’ perceptions of clinical alarms [29-35].
Four of the seven studies reported on the level of alarm fatigue of nurses.The use of customized software improved perceptions of alarm loads interfering with workflow (from 66.7% to 45.5%) [34],and the use of pagers resulted in nurses’ increased sensitivity to alarms [31].Before updating their devices and workflow,92% of ACCU nurses surveyed strongly agreed or agreed that “nuisance alerts are frequent,” compared to 44% thereafter [35].Wearing a smartwatch reduces the workload of checking each alarm signal perception,allowing nurses to focus on the patient for a shorter period.These results are several parts of alarm fatigue [36].The new alarm notification system reduced nurses’mental and physical fatigue.In other words,nurses’ levels of alarm fatigue decreased (Table 3).

Table 3 Effects of intelligent management in included studies.
3.5.Accuracy of alarm signals
Three studies mentioned the accuracy of alarm signal recognition after the implementation of novel intelligent management schemes [29,30,35].The novel multisensory smartwatch application could improve the overall accuracy of alarm signal recognition significantly,but the improvement in the accuracy of individual alarms was not statistically significant[30].The recognition rate of critical alarms displayed in the surveillance corridor was 84%,but the recognition rate of code blue using Wi-Fi phones was only 68%,and even the most critical alarms could not be fully recognized[29].After Pater introduced the third-generation alarm system and the third-generation RN upgrade algorithm,it was found that the ratio of average initial alarm notification to total alarm notification decreased to 40%.However,this reduction is considered an appropriate benchmark for the new system [35].
One study found other effects when the number of alarms changed [29].The cardiac arrests or acute respiratory compromise events showed a decreasing trend when the number of alarms decreased [29].In addition,this study reported on the premise of implementing interventions without affecting patient safety,making patient monitoring outcomes at least as safe as traditional vital signs monitoring [29].
4.Discussion
This integrative review explored the effectiveness of novel approaches to intelligent management on the reduction of false alarms and the safety of the application in hospital and simulated hospital settings.A comprehensive Internet-based approach is a promising way to address the problem of alarms in critical care medicine [37].However,the number of studies on the application of novel forms of alarm management combined with the Internet was limited.
The results of the study evaluated the total number of clinical alarms,duration of alarms,nurse response time to importantalarms,alarm fatigue level of nurses,and accuracy of the alarm signal,focusing on alarms algorithm escalation systems,alarms management servers,alarms secondary notification devices,and multimodal alarms notification application [29-35].Based on the analysis of the studies included in this review,most of the systems for intelligent alarm management had positive impacts when applied,and these impacts included reductions in the total number of alarms,duration of alarms,and nurses’response time to alarms,and improvement of alarm fatigue among nurses.Moreover,the accuracy of alarm signal recognition was also improved in a few studies.Even one study that consistently tested alarms eight months after program completion still found a consistent decrease in the total number of clinical alarms [29].It is reasonable to assume that intelligent approaches with the latest technologies are crucial for alarm management.Healthcare professionals have also expressed that support systems based on artificial intelligence are useful,and they require intelligent devices to detect patients remotely and optimize alarm management [38].
The interventions included in the literature were not only for the intelligent management of alarms but also included training,threshold changes,multidisciplinary collaboration,alarm delay settings,etc.This is because we did not find studies with interventions that only did intelligent alarm management,we chose studies that included intelligent alarm management in their interventions.We were unable to ascertain the magnitude of the impact of measures for intelligent alarm management on the reduction in the number of alarms.The most effective interventions for safely reducing unnecessary alarms were also unclear [13].Combining tools or systems for the intelligent management of alarms with evidence-based interventions has been effective in improving nurses’ alarm management behaviors.However,not all studies directly measured changes in the number of alarms,and the types of alarms that decreased in number were inconsistent.The results of only two studies considered changes in the number of alarms at different priority levels [33,34],but the effects were different,with a reduction in the number of high-priority alarms [33]and a reduction in the number of medium-priority alarms[34].The impact of intelligent alarm interventions on false alarms remains uncertain,but we still believe that an intelligent management approach in conjunction with the Internet is essential.Future studies should be considered directly measuring changes in the number of false alarms after intervention as this may help to better understand the effects of the interventions.
More efforts should be made to utilize the visual and tactile characteristics of alarm messages to create more clinically effective alarm management devices.The use of multimodal alarm systems to notify nurses can also be effective in reducing nurse response time and reducing the cerebral workload[30].The auditory nature of the alarm is still utilized in most current studies to notify nurses.While signal monitoring algorithms continue to improve,different tones help nurses recognize the severity of a patient’s changing condition [39].Moffatt-Bruce has noted that efforts to improve auditory alarm recognition in hospital settings are severely limited by the inability to modify the alarm signal characteristics of medical devices[23].As a result,we still have a lot of work to do to ensure better patient monitoring and reduce the distress that alarms cause to nurses.
Due to the ever-changing nature of patients’ vital signs,the prerequisite for the application of new systems or equipment should be to ensure the accuracy of the system in identifying emergencies.Among the included studies,we found several promising approaches,including upgrading the alarm algorithms,sending alarms to a handheld device with a specific time delay,and so on.Professionals involved in the development of medical devices should also conduct further clinical testing to confirm that these novel alarm management devices or systems using advanced technology are not missing real alarms and that the accuracy of alarm notifications and recognition rates need to be monitored by a professional or organization.The availability of technology usability-referring to the efficient,effective,and safe use of technology should be emphasized[40,41].Healthcare professionals need to be constantly aware of changes in the patients’ condition in any situation,rather than relying exclusively on the alarm system,although advanced alarm technology may have a recognition accuracy of 100% in future research.Hospital training programs should also reinforce information related to emerging technologies at every step of education to adapt to the global needs of ICU branches and existing market requirements [20].
In addition to these interventions,several studies have experimented with the intelligent management of alarms.Currently,the use of machine learning algorithms to build predictive models and evaluate the quality of the signal has entered the public view,mostly for heart rate or arrhythmia-related alarms at the laboratory level,and has not yet been applied in a hospital or simulated hospital setting.No studies have been found to construct alarm models by classifying alarms according to their clinical relevance and priority.Flohr suggested that staff in ICU need patient monitoring devices to be interoperable with other medical devices to optimize workflow and reduce redundant operations in the ICU [42].Therefore,more efforts are still needed to combine artificial intelligence and alarm management into clinical applications.Future work will need to facilitate newly developed technologies to address the alarm problem.
Summarizing the studies analyzed,we conclude that interventions for intelligent alarm management applied to clinical settings may have produced positive results.The results suggest that we remain uncertain about the effectiveness of interventions and tools targeting intelligently managed alarms in reducing the number and duration of alarms,shortening nurses’ response time to critical alarms,and improving patient safety.In the future,more researches are needed to integrate alarm management with the Internet to increase the positive predictive value of alarm systems,reduce the number of unnecessary alarms,and truly improve the alarm-ridden healthcare environment.
5.Limitations
We recognize the limitations of this review.Including only seven studies in this review resulted in a limited generalization of findings.Most of the included articles had relatively small sample sizes,limiting generalizability.This review had only focused on the application of novel alarm management systems and had not yet considered algorithms in the laboratory.Although alarm intelligent management measures were the focus of the study,alarm smart management measures were not the only interventions in the retrieved and included literature,making them even more limiting when analyzing the effects.Given the high degree of heterogeneity in methodology,we were unable to generate summary proportions of the observational studies or perform a meta-analysis of the intervention studies,and we presented descriptive summaries only.Finally,we need to conduct further studies on intelligent management of alarms and use effective measurement methods to assess their effectiveness.
6.Conclusion
New medical devices and digitalization have led to a growing workload of data analysis for healthcare professionals,making artificial intelligence-based systems an essential issue for the future.Therefore,the application of systems or tools for the intelligent management of clinical alarms is urgent in hospitals.This integrative review examined seven studies related to intelligent management interventions for clinical alarms in hospital and simulated hospital settings.The result showed that interventions and tools for the intelligent management of alarms were effective in reducing the number of false alarms,reducing the duration of alarms,reducing the time nurses have to respond to critical alarms,and reducing alarm fatigue levels among nurses.In future studies,more alarm management combined with the Internet is needed to enable accurate identification of critical alarms,ensure nurses respond quickly to alarms,and truly improve healthcare environments where alarms are rampant.
Funding
This work was supported by the General Program of National Natural Science Foundation of China (NSFC) [No.72174209].
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
CRediT authorship contribution statement
Bingyu Li:Conceptualization,Methodology,Validation,Formal analysis,Data curation,Writing-original draft,Writing-review&editing,Project administration.Liqing Yue:Conceptualization,Methodology,Validation,Formal analysis,Data curation,Writing -original draft,Writing -review &editing,Funding acquisition,Project administration.Huiyu Nie:Conceptualization,Methodology,Validation,Formal analysis,Resources,Data curation,Writingreview &editing,Supervision,Project administration.Ziwei Cao:Conceptualization,Methodology,Validation,Formal analysis,Resources,Writing -review &editing.Xiaoya Chai:Conceptualization,Methodology,Validation,Formal analysis,Writing-review&editing.Bin Peng:Conceptualization,Methodology,Validation,Formal analysis,Writing -review &editing.Tiange Zhang:Conceptualization,Methodology,Validation,Formal analysis,Writing -review &editing.Weihong Huang:Conceptualization,Methodology,Validation,Formal analysis,Funding acquisition,Writing -review &editing.
Declaration of competing interest
No conflict of interest has been declared by the authors.
Acknowledgments
Not applicable.
Appendices.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.12.008.
 International Journal of Nursing Sciences2024年1期
International Journal of Nursing Sciences2024年1期
- International Journal of Nursing Sciences的其它文章
- Nursing leadership: Key element of professional development☆
- Comparison of the performance of four screening tools for sarcopeni a in patients with chronic liver disease
- Associations among frailty status,hypertension,and fall risk in community-dwelling older adults
- Facilitators and barriers to the implementation of dietary nutrition interventions for community-dwelling older adults with physical frailty and sarcopenia: A qualitative meta-synthesis
- The prevalence and factors associated with sarcopenia in Thai older adults: A systematic review and meta-analysis Phatcharaphon Whaikid,Noppawan Piaseu*
- Air quality self-management in asthmatic patients with COPD: An integrative review for developing nursing interventions to prevent exacerbations
