Facilitators and barriers to the implementation of dietary nutrition interventions for community-dwelling older adults with physical frailty and sarcopenia: A qualitative meta-synthesis
Lijun Chn ,Hunhun Hung ,Siqi Jing ,Hiyn Yo ,Li Xu ,Qi Hung ,Mingzho Xio ,Qinghu Zho ,*
a Department of Nursing,The First Affi liated Hospital of Chongqing Medical University,Chongqing,China
b Library,The First Affiliated Hospital of Chongqing Medical University,Chongqing,China
c Health Management Center,The First Affiliated Hospital of Chongqing Medical University,Chongqing,China
d School of Public Health and Management,Chongqing Medical University,Chongqing,China
e Department of Urology,The First Affiliated Hospital of Chongqing Medical University,Chongqing,China
Keywords:
ABSTRACT Objectives: With the acceleration of an aging society,the prevalence of age-related chronic diseases such as physical frailty and sarcopenia is gradually increasing with numerous adverse effects.Dietary nutrition is an important modifiable risk factor for the management of physical frailty and sarcopenia,but there are many complex influences on its implementation in community settings.This study aimed to summarize the facilitators and barriers to the implementation of dietary nutrition interventions for community-dwelling older adults with physical frailty and sarcopenia,and to provide a reference for the formulation of relevant health management programs.Methods:Searches were conducted in databases including PubMed,Web of Science,Medline (Ovid),Embase (Ovid),and Cochrane Library from inception to January 2023.Searches were completed for a combination of MeSH terms and free terms.The Critical Appraisal Skills Program(CASP)instrument was used to appraise quality.Coding and analysis of the extracted information were performed using the socio-ecological modeling framework.The study protocol for this review was registered on the PROSPERO (CRD42022381339).Results:A total of 10 studies were included.Of these,four were nutrition-only focused interventions,and six were dietary nutrition and exercise interventions.The facilitators and barriers were summarized based on the socio-ecological model that emerged at three levels: individual trait level,external environment level,and intervention-related level,containing ten subthemes.Conclusion:Individual internal motivation and external support should be integrated with the implementation of diet-and nutrition-related interventions in community-living aged people with physical frailty and sarcopenia.Develop “tailored” interventions for participants and maximize available human and physical resources.
What is known?
· Physical frailty and sarcopenia are age-related chronic diseases that are becoming increasingly common in an aging society.
· Dietary nutrition is a modifiable risk factor that plays a crucial role in managing physical frailty and sarcopenia.
· Implementing dietary nutrition interventions for older adults with physical frailty and sarcopenia could be challenging due to various complex influences in community settings.
What is new?
· Dietary nutritional interventions that meet individual preferences and preexisting lifestyles in community settings are of great importance.
· Interventions that utilize individual motivation combined with external support are beneficial in addressing individual and organizational barriers to implementing dietary nutrition interventions.
· Utilizing a theoretical framework to summarize facilitators and barriers to interventions is beneficial for informing the theoretical framework of future interventions.
1.Introduction
Physical frailty is a subset of frailty that is characterized by unintentional weight loss,self-reported exhaustion,weakness (low grip strength),slow walking speed,and low physical activity [1].Sarcopenia is an age-related loss of muscle mass with a decrease in muscle strength and/or somatic function;it became an officially coded category of the International Classification of Diseases-10th revision (ICD-10) in 2016 [2,3].Studies have found that physical frailty and sarcopenia share common pathophysiological mechanisms and exhibit significant clinical overlap [4,5].Recently,a progressive increase in the prevalence of physical frailty and sarcopenia has been reported as the global population ages [6],affecting functional and health outcomes [5] and leading to an increased risk of adverse health outcomes such as falls,disability,or all-cause mortality [7-11].However,the insidious clinical symptoms of physical frailty and sarcopenia,coupled with the lack of awareness among doctors,nurses,and patients [12],make the prevention and treatment of physical frailty and sarcopenia difficult and require urgent attention.
Currently,there is no pharmacologic treatment for physical frailty and sarcopenia[13].Dietary nutrition has gained increasing attention from clinical and research scholars as a modifiable risk factor and an implementable interventional measure.Studies have demonstrated the positive effects of certain dietary patterns and nutrients on promoting improved skeletal muscle health and physical function [14,15].A large amount of high-quality evidence [15-17] has also confirmed the role of dietary nutrition interventions for physical frailty and sarcopenia.In addition,the International Clinical Practice Guidelines for Sarcopenia (ICFSR)Guidelines [18] and consensus from the Asian Working Group for Sarcopenia (AWGS) [19] specifically recommend dietary nutrition interventions for the prevention and treatment of physical frailty and sarcopenia in primary care settings.Despite the strong evidence that nutrition can prevent and treat physical frailty and sarcopenia,it has proven unsatisfactory in community settings.
Compared with hospitalized patients or residents in long-term care institutions,community-dwelling older adults have poorer access to specialized dietary and professional guidance [20].Moreover,these individuals also report lower adherence to prescriptions[21].Since most interventions in specialized institutions are implemented in highly controlled environments,it is not possible to conclude the effectiveness of their implementation in real life [22].Consequently,there is a need to translate these efficacious clinical interventions to real-life health care and community settings and investigate their effectiveness in practice.
Interventions that use theory as a guiding framework are more effective in improving the diet of older adults [23].A recent systematic review found that interventions informed by theory were more successful in improving diet than those that did not utilize theory [24].The Social Ecological Model (SEM) is derived from Bronfenbrenner’s Ecosystem Theory,which seeks to explore the complex issues affecting individual behavior [25].According to SEM,behavior is influenced by individual (e.g.,knowledge,attitudes,self-efficacy),social (e.g.,social norms,family,peers),and environmental factors (e.g.,family environment,community,public policy) [26].It has become a useful tool for exploring factors associated with dietary or exercise adherence in different populations [27,28].
Qualitative studies are evaluated by guidelines in the physical frailty and sarcopenia field[29],which can be used to reveal issues of the adherence to and acceptability of interventions,including the importance of the social environment.To address the existing challenges in dietary and nutritional interventions for seniors with physical frailty and sarcopenia,we collated existing research to understand the facilitators and barriers to implementing interventions from different perspectives using SEM as a framework and to inform effective interventions.Similarly,understanding patients’ perceptions of dietary nutrition interventions to prevent and treat physical frailty and sarcopenia will help to develop and implement patient-centered interventions or management strategies.
2.Methods
The protocol of this systematic evaluation has been published in the PROSPERO database (ID: CRD42022381339).This review was reported according to the Enhancing Transparency of Reporting the Synthesis of Qualitative Research(ENTREQ) framework[30].
2.1.Study selection and selection criteria
Combined with keyword and subject terminology (MeSH)terms,a systematic search was performed in PubMed,Web of Science,Medline (Ovid),Embase(Ovid),and the Cochrane Library.Drawing on the search methodology of similar-urpose studies[31],studies were retrieved from database creation to the end of January 2023,and references relevant to this study were also searched and screened.The detailed search strategy can be found in Appendix A.The search strategy was developed in consultation with librarians (HY).The inclusion criteria used the following the PICo framework: (a) Population: older adults (≥60 years) with physical frailty or sarcopenia(prefrailty or sarcopenia possible);(b)Interest: the intervention is dietary nutrition alone or in combination with others (exercise),and facilitators and barriers of the intervention were discussed;(c) Context: community or homebased.The study type was not limited to qualitative study;studies involving qualitative data collection were included.Studies were excluded if they were reviews,research protocols,commentaries,editorials,or conference abstracts.The study was also excluded if the participants were not involved or could not be identified with sarcopenia or physical frailty.
2.2.Literature screening and data extraction
Duplicates were removed from the retrieved literature using the literature management software Endnote before two researchers(LC and SJ)independently read the title and abstract sections of the literature and excluded ineligible papers based on the inclusion and exclusion criteria.The two researchers screened articles that ultimately met the criteria through the reading of the full text of the paper.Any disagreements that arose during the screening process were resolved through discussion and consensus with a third researcher (HH).Articles that did not meet the screening criteria were excluded,and each researcher was asked to report the reasons for exclusion.
2.3.Quality assessment
We assessed the quality of the qualitative studies included in this review using the Critical Appraisal Skills Program (CASP)qualitative research assessment criteria[32].The tool consists of 10 questions,each of which is scored 1 point for a “yes” answer and 0 points for a“no”or“can’t tell”answer,with a maximum score of 10 points.Studies evaluated based on CASP with a score of <7 indicate low methodological quality and will not be included.Our study was committed to maximizing the understanding of potential influences;thus,low-quality studies were not excluded.This analysis method has been used by other scholars [33].
2.4.Data analysis
Following Malterud’s “process of selecting and collecting relevant information from the included studies”[34].Two researchers created coding forms using inductive coding.First,information was extracted from the included studies,and information with the same connotation was grouped under a subtheme generalized from the extracted information.Second,each subtheme was categorized into three aspects of the socio-ecological model [35].
2.5.Rigor and credibility
Prior to the commencement of the study,the research plan was developed and registered in PROSPERO after discussion among the research team to ensure the rigor of the study.The search strategy was developed under the guidance of the librarian (HY).Two researchers(LC and SJ)performed literature screening independently based on the inclusion and exclusion criteria and reported the reasons for exclusion.The two researchers (LC and LX) conducted the literature quality assessment at the same time.When the results were inconsistent,a decision was made in consultation with a third researcher (HH).Two researchers (LC and LX) performed the data analysis simultaneously.In the case of disagreement,a decision was made by the research team after discussion to ensure the rigor and reliability of the study.
3.Results
3.1.Characteristics of the included research
A total of 2,025 records were retrieved from five databases,and 27 were retrieved from citations in the relevant review literature.After the abstract and full-text screening,472 duplicates were removed,and 1,468 records were excluded.A total of 10 papers were ultimately included (Fig.1).

Fig.1. PRISMA flow diagram of the literature screening and selection.
Overall,interviewees in the included papers were older adults(n=113) and healthcare providers (n=157).The healthcare providers included community healthcare workers,nutritionists,general practitioners,physiotherapists,nurses,and members of multidisciplinary teams.They are collectively referred to as health care personnel (HCPs).The countries included in the studies were all economically developed countries,of which seven were in Europe and only one in North America,one in Asia and one in Oceania.In addition,seven qualitative studies and three mixed studies were included in the qualitative part of the research.Concerning the methodology,five studies used semi-structured interviews,two used focus group interviews only,two combined semi-structured and focus group interviews,and one used an open-ended questionnaire to collect information.Four of the included studies were nutrition care-based interventions,and the interventions in six studies included mixed dietary nutrition and exercise guidance.The detailed characteristics of all included studies [36-45] are shown in Table 1.
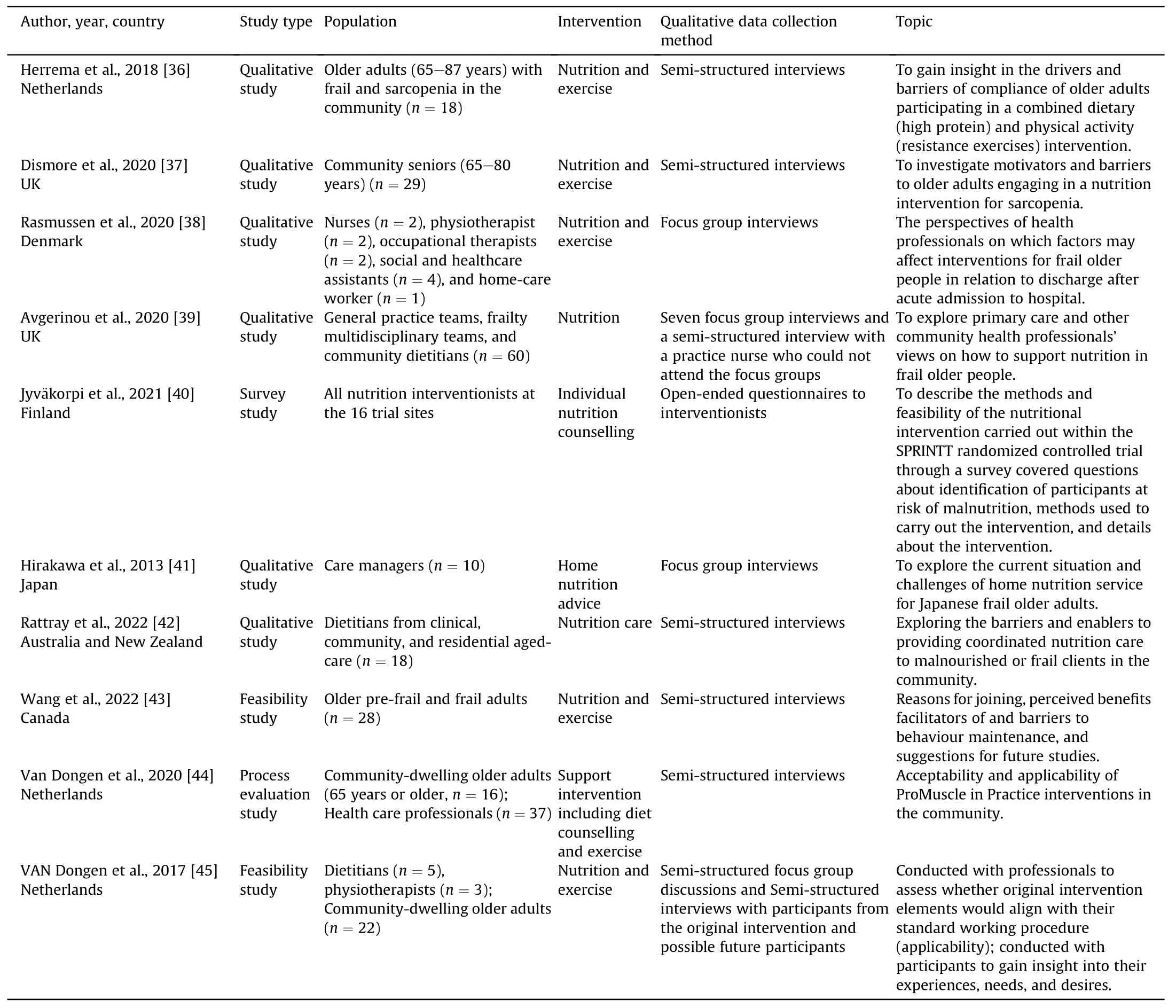
Table 1 The characteristics of the included studies.
According to the quality evaluation tool,the total score of the included qualitative studies was between 8 and 10 points,indicating high quality.Four studies did not answer question 6,and two studies were not clear about the ethic consideration (question 7).The assessment result is detailed in Appendix B.
3.2.Facilitating factors and barriers analysis based on the socialecological model
The literature yielded a total of ten subthemes,which we generalized to form three broad themes that fit the individual trait,external environment,and intervention-related dimensions of the social-ecological model,as detailed in Table 2.
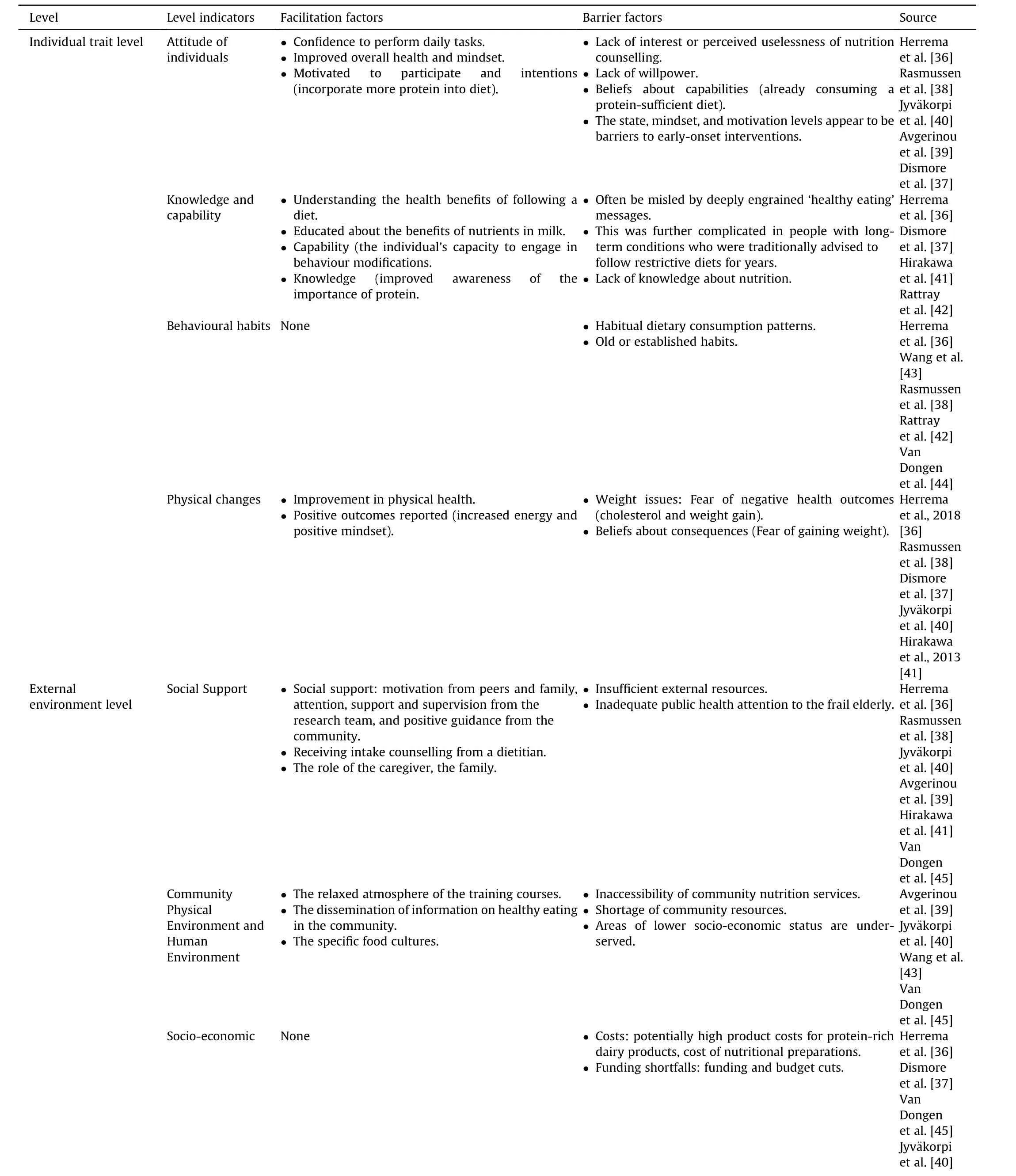
Table 2 Facilitators and barriers based on social-ecological model to the implementation of dietary nutrition interventions for community-dwelling older adults with physical frailty and sarcopenia.
Facilitating factors and barriers emerged at all three levels (see Table 3).Four themes emerged at the individual trait level (i.e.,attitude of individuals,knowledge and capability,behavioural habits,and physical changes),three themes emerged at the external environment level (i.e.,social support,community physical environment and human environment,and socioeconomic),and three themes emerged at the intervention-related level (i.e.,intervention protocols,implementers of interventions,and products for dietary advice or intervention).
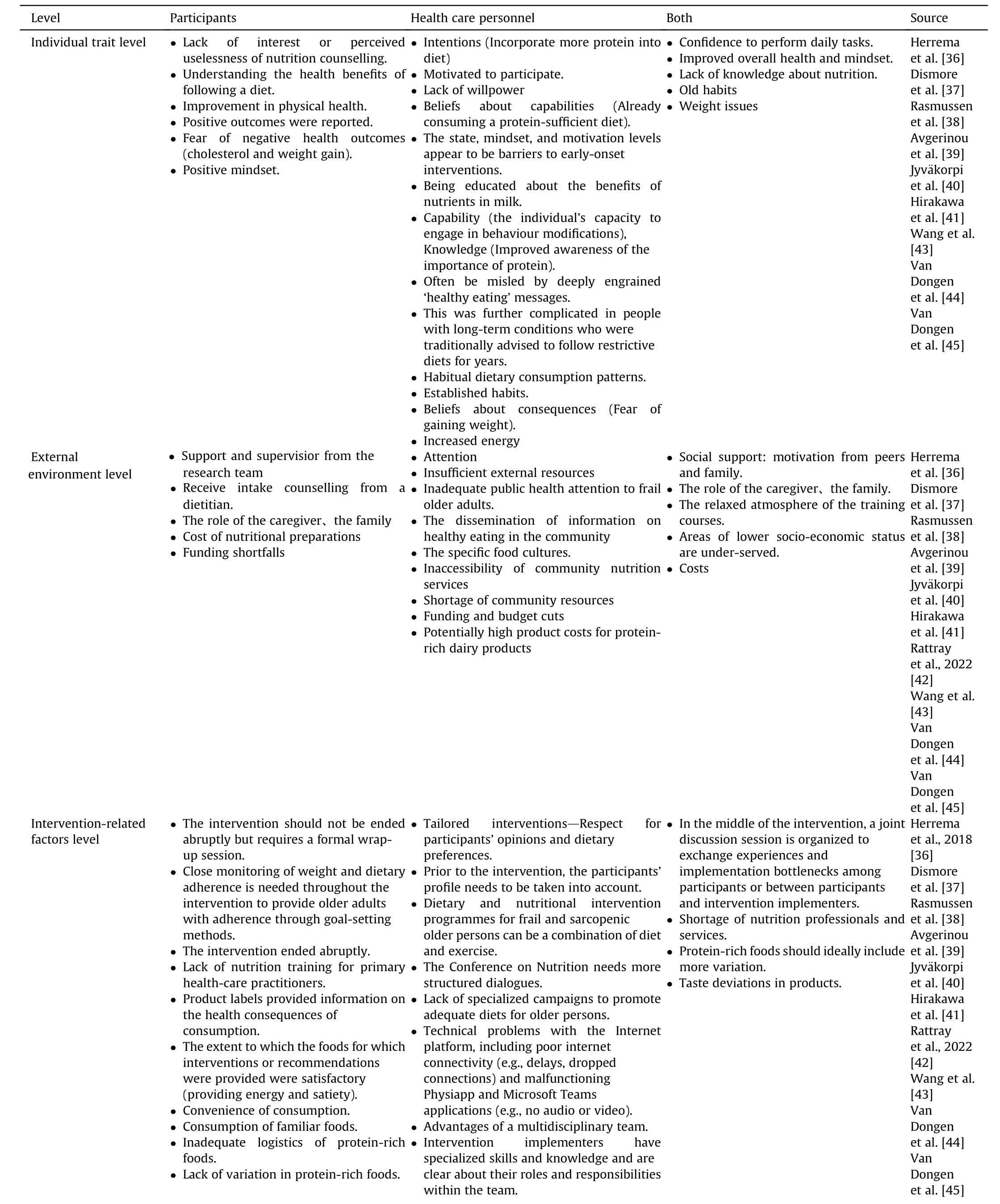
Table 3 Patients’ and professionals’ perceptions of implementing dietary nutrition interventions related to social-ecological models.
3.2.1.Individual trait level
3.2.1.1.Attitude of individuals.Attitude is defined as an individual’s positive or negative response to a behavior,which influences an individual’s behavioral intentions and,thus,behaviors [46].Many older adults expressed confidence in adhering to the recommended foods and perceived both physical and psychological benefits in participating as well [36,37,43].
“I started to feel fitter,realized I was fitter … more strength and stamina.” (Senior)
“Already consuming a protein-sufficient diet…” (Senior)
The state,mindset and motivational level appear to be barriers to the early implementation of nutritional interventions [38].The state of mind of frail older adults directly prevents them from eating more nutritious foods or even directly expresses a lack of interest or confidence [38,44].
“… they don’t have knowledge about what is good for them.And what you have to think about and what strengthens their muscles and bones.” (HCP)
3.2.1.2.Knowledge and capability.Some older adults are aware of the health benefits of following dietary recommendations,are educated about the benefits of nutrients in milk,and can engage in behavior change [36,37,45].
“A lot to talk about(milk)encouraged me to buy more and I’m no longer drinking semi-skimmed.” (Senior)
However,it is sometimes difficult for older people to make behavioral changes when they are misled by deeply engrained “healthy eating” messages or lack knowledge about disease or nutrition [39].
“This was further complicated in people with long-term conditions who were traditionally advised to follow restrictive diets for years.”(HCP)
“Preparing three meals a day is tiresome for many older people.”(HCP)
3.2.1.3.Behavioural habits.Eating habits tend to deteriorate with age,with older people prefer habitual dietary consumption patterns that are difficult to change [36,39-41,43].
“For their new food intake routine,they had to make substantial changes compared to their existing habitually consumed breakfast and lunch products,making it harder to comply.” (HCP)
“Older people develop a preference for unhealthy food due to a change in their sense of taste.” (HCP)
3.2.1.4.Physical changes.Positive signs of physical change provided an impetus for older adults to continue to participate in the intervention [36,43].As the intervention progressed,older adults perceived improvements in overall health -increased energy and positive mindset [37].At the same time,weight concerns were identified as a common barrier factor[43-45].
“Fear of negative health outcomes(cholesterol and weight gain)…”(Senior)
3.2.2.External environmental level
3.2.2.1.Social support.Adequate support includes support from“intervention implementers”,“family and friends”,“community health care workers” or “like-minded peers” [36,43-45].Support consisted of “information,tools,physical and psychological attention”etc.[36,43-45].Conversely,“lack of support from all sources”[44]often prevented older adults from continuing to adhere to the programs developed.Another contradictory theme was mentioned:“Cooking together as a family”could be supportive and appetizing for family members but did not meet the specific food or nutritional needs of each individual [38].
3.2.2.2.Community physical environment and human environment.The physical and human environment of the community can potentially influence the implementation of interventions.Community dissemination of disease-specific information on healthy eating through various channels or the creation of a relaxed atmosphere during the training sessions of the intervention is conducive to participants’ adherence to healthy eating [44].Of course,some places have their own specific dietary cultures,and it may be somewhat difficult to ask them to implement new dietary patterns [38].In addition,some communities have limited resources and poor access to services,and it may be difficult for them to follow a particular dietary recommendation [40,42].
“There’s a lack of community dietetic services available to us …”(Senior)
3.2.2.3.Socioeconomic.The issue of cost is critical for both the research team and the participants.The potentially high productcost of protein-rich dairy or meat products is often a key reason why participants struggle to stay on track[36,39,40,42,44].Funding and budget cuts or even funding shortfalls during the course of an intervention can be very detrimental to the continuation of the intervention [37].
3.2.3.Intervention-related level
3.2.3.1.Intervention protocols.The implementation of dietary and nutritional interventions for aged people with community physical frailty and sarcopenia requires a more individualized intervention protocol,which has to be adapted to the target group and to the working procedures of the HCP [37,44].
“Different settings -different nutritional approaches.” (HCP)
Before the intervention,the participants’ profile needs to be taken into account,especially dietary preferences and a comprehensive description of the benefits of consuming a diet with sufficient protein [36,43,45].In the middle of the intervention,a joint discussion session is organized to exchange experiences and implementation bottlenecks(e.g.,in the case of some participants,logistical problems in distributing protein-rich foods) among participants or between participants and intervention implementers [44].The intervention should not be ended abruptly but requires a formal wrap-up session [43].
“Participants felt that the intervention ended quite abruptly and voiced concerns over the lack of guidance on how to progress exercises safely on their own.” (HCP)
Close monitoring of weight and dietary adherence is needed throughout the intervention to provide older adults with adherence through goal-setting methods[40,41].Dietary and nutritional intervention protocols for older persons with physical frailty and sarcopenia can be a combination of diet and exercise,but specialized exercises to promote adequate eating in older persons arelacking [43,44].In addition,in the case of online interventions,technological issues should be considered in advance [44].
3.2.3.2.Implementers of intervention.Multidisciplinary teamwork facilitates the integration of the strengths of the resources of each discipline [36,39,44,45].Intervention implementers need to have specialized skills and knowledge and be clear about their roles and responsibilities within the multidisciplinary team.
“Dietitians have the required competencies,including interpersonal skills and knowledge….”(HCP)
“HCP’s prior training courses and clear manuals and registration forms contain sufficient information…” (HCP)
Sometimes there are also issues of shortage of nutrition professionals and services resulting in a high workload for intervention implementers or community dietitians who do not form close working relationships or are not aware of other HCPs,which may affect the orderly progress of the overall intervention [39,42].In other cases,there is a lack of nutrition training for primary care practitioners to the extent that they are unable to meet the information needs of the intervention population [38].
“….I don’t think we’ve ever formally had any nutrition training.”(HCP)
3.2.3.3.Products for dietary advice or intervention.It was easier for the participants to consume attractive foods and stick to them [36,44].For example,there are product labels for food packages that provide information on the health consequences of consumption.
“Well,this yogurt drink has a label that states that it should be good for your muscles.Therefore,it catches my attention…”(Senior)
Dietitian-recommended foods that provide energy and satiety,match individual tastes,are versatile,and are easy to consume can be more beneficial to participants.Comprehensive nutrition education brochures and videos are also necessary [39,43-45].
“You know,some of the materials,as I say,you know,without sounding too full of myself,I think I’m fairly knowledgeable about nutrition already.”(Senior)
Conversely,providing interventions with products that are poorly flavored,have little variety,do not take into account the energy content of the product,and have insufficient food logistics can weaken participant adherence [38,40].
“… energy content of products should be taken into account in advice.”(HCP)
3.3.Implications for the intervention
Facilitators and barriers to the implementation of dietary nutrition interventions for community-dwelling older adults with physical frailty and sarcopenia emerged at all three levels.The findings shed light on the potential ways of designing effective interventions and managing physical frailty and sarcopenia in community healthcare settings for older adults (Fig.2).

Fig.2.Facilitators and barriers to the implementation of dietary nutrition interventions for community-dwelling older adults and implications for interventions.
4.Discussion
Physical frailty and sarcopenia are prevalent conditions among older adults that can significantly impact their quality of life and independence.Dietary interventions have been shown to be effective in managing and preventing these conditions,but the implementation of such interventions can be challenging.Understanding the facilitators and barriers to implementation can help healthcare professionals develop effective strategies to promote the uptake of dietary interventions and improve the health outcomes of older adults with physical frailty and sarcopenia.We found that facilitators and barriers emerged at all three levels(individual trait,external environmental,and intervention-related level),which may provide implications for the future intervention design or management of older adults with physical frailty and sarcopenia in community health care settings.
At the individual trait level,we found that facilitators and barriers to dietary or nutrition interventions revolved around psychological factors,knowledge and capability,behavioral habits and physical changes.This corroborates the knowledge,attitude and practices (KAP) model,in which the knowledge base and attitude facilitation have an impact on individual practices[47].This is also supported by previous findings [48,49],which showed that psychological state is an effective mediator of behavioral change in lifestyle interventions.The relationship between food and health is widely recognized,but there is a knowledge-behavior gap regarding healthy eating among older adults and a lack of awareness of the dietary risks associated with chronic diseases [50,51].This requires primary healthcare providers are called upon to play a health-education role through multimedia public-health campaigns as a means of raising awareness,providing information and changing attitudes towards healthy eating among older persons.Moreover,our findings highlight the importance of physical changes in dietary interventions.Positive physical and psychological changes can increase an individual’s confidence in their abilities [52],known as self-efficacy,which can then influence their behaviors.However,physical changes may not always go as planned.The main objective of dietary nutrition interventions is to improve physical functioning in older adults with physical frailty and sarcopenia,but weight problems may become a new issue deferred from the intervention.For this reason,goal-oriented measures can be instituted in interventions to assist participants in setting measurable goals for physical improvement and guiding them to engage in exercise that is coordinated with their diets and nutrients to help allay concerns about weight change.
Consistent with previous research [53,54],most interviews discussed the importance of community support.Community support encompasses different levels of family,community,and government with manifest and potential support.We found that partners and health care professionals play an important role in providing social support by providing thorough supervision [37,44,52],timely feedback and emotional support,which is conducive to helping older adults improve self-efficacy and adhere to beneficial dietary recommendations[38,43,55].The high cost of healthy foods or nutritional preparations is a common barrier to adherence to recommended diets among older adults,and this cost can easily undermine persistence to recommended diets due to the absence of continued support after the intervention [56].Interestingly,a paradoxical situation has also been identified,with studies mentioning that “cooking together as a family” may increase appetite [40],but it may also be easy to neglect recommended dietary advice.Some researchers have found that people may ignore their usual norms of eating behavior in social situations such as workplaces,holidays,or parties [57,58].However,older adults usually make simpler food choices when eating alone [59],which is more detrimental to older people with physical frailty and sarcopenia.Some studies have noted that eating in public settings,such as the community,is beneficial for improving older adults’dietary choices and nutritional status as well as promoting muscular health [60,61].This practice has been recommended by AWGS expert consensus [19].Based on this,we suggest families should be mobilized,meanwhile establishing public cafeterias in the community to address the above issues,encouraging the functional embedding of nonprofit organizations to provide meal choices tailored to the needs of different chronic illnesses,and creating a good social support environment for healthy eating among community-based older adults with physical frailty and sarcopenia.
Unlike conventional socio-ecological models,which concentrate on broader factors such as the policy level,our study focuses more on the modifiable aspects of the intervention itself.Targeting the more controllable parts of an intervention can help interventionists make more actionable decisions to improve participant compliance [62].Similar to other studies [63,64],we found that tailored interventions,expert guidance from healthcare professionals and diverse health education resources are all important dietary nutrition interventions for older people in the community [63].Combining dietary nutrition interventions with exercise appears to increase the effectiveness and adherence of nutritional interventions for older people with physical frailty and sarcopenia.Studies have shown that dietary protein intake after resistance exercise increases postexercise muscle protein synthesis rates and inhibits muscle protein catabolism[65-67],which is important for promoting muscle health in older adults.Interestingly,previous studies have considered the facilitating role of specialists (e.g.,dietitians or general practitioners)in guiding patients to healthy diets [36-40,42-45,55],but we found that some“specialists”could be a barrier to intervention implementation for not being able to give adequate and effective guidance promptly if they lacked sufficient competence,played weak roles or the intervention stopped abruptly.This is particularly pronounced in primary care settings where healthcare resources are relatively scarce [38,39,68],which puts higher demands on the adequacy,professionalism and timeliness of interventionists.Furthermore,we found that the level of intervention is important.Compared to exercise interventions,dietary and nutritional interventions may take longer to show results [69],which requires more time and effort and consumes more resources for service providers,while time-saving interventions have yet to be developed and applied.Some studies have demonstrated the effectiveness of information technology [70,71],which is not limited by time and space as well as providing a wealth of specialized resources and,more importantly,can be used by subjects after the intervention period has ended to avoid participant discomfort and disruption of the effects of a suddenly discontinued.Therefore,we suggest that a scientific intervention program is the foundation,and in the future,information technology can be used to compensate for these shortcomings,build a bridge of communication and interaction between professionals and older adults,and utilize the information platform to provide diversified healthy dietary resources to construct an intervention with long-term benefit s.
5.Limitations
There are several limitations to this review.First,only five search databases were included,which may have led to the omission of some studies.However,a manual screening and a wide range of search terms may have been beneficial in addressing this deficiency.In addition,the studies were not discussed disaggregated by gender,age,or cultural groups in their interpretation.Caution is needed when referring to the findings because the studies were mainly conducted in developed geographic areas,and socioeconomic differences may have a significant impact on the interpretation of the results.Finally,our stratification of the study results lacks nuance despite drawing on the social-ecological systems theory model.For example,similar and different components of participants’ impact within the intervention design existed for individual trait-level factors.In this paper,facilitators and barriers were treated as mutually exclusive at one level,although they may be intertwined,which may lead to an oversimplification of the findings.
6.Conclusions
We used SME to synthesize existing research on facilitators and barriers to community implementation of dietary and nutritional interventions from three perspectives: the individual,the intervention itself,and the social context.The study found that interventions that are “tailored” to the specific physiological conditions and needs of older adults with physical frailty and sarcopenia in community settings are more likely to be accepted and sustained.In addition,interventions that combine individual motivation and external support are useful in addressing the barriers that individuals and organizations face in implementing dietary nutrition interventions and are an approach to health management that has long-term benefits.In general,we pay close attention to the modifiable parts of the intervention and also try to overcome the external immutable aspects.Our study provides actionable recommendations for future preventive management of physical frailty and sarcopenia by community healthcare workers.As smart communities are built,intervention methods utilizing smart products and remoteness should be explored in the future.
Funding
This research was funded by Key R&D projects of Chongqing Municipal Bureau of Science and Technology (No.CSTC2021jscxgksb-N0021) and 2022 Postgraduate intelligent medicine Special research and development plan of Chongqing Medical University(No.YJSZHYX202206).
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
CRediT authorship contribution statement
Lijuan Chen:Conceptualization,Methodology,Validation,Formal analysis,Resources,Data curation,Writing -original draft,Writing -review &editing,Project administration.Huanhuan Huang:Conceptualization,Methodology,Validation,Formal analysis,Resources,Writing -review &editing,Supervision,Project administration.Siqi Jiang:Conceptualization,Methodology,Validation,Resources,Data curation,Writing -original draft.Haiyan Yao:Conceptualization,Methodology,Validation,Resources,Formal analysis,Data curation,Writing -review &editing,Supervision.Li Xu:Conceptualization,Methodology,Validation,Resources,Data curation,Writing -review&editing,Supervision.Qi Huang:Conceptualization,Methodology,Validation,Data curation,Writing -review &editing.Mingzhao Xiao:Conceptualization,Validation,Formal analysis,Resources,Writing -review &editing,Supervision.Qinghua Zhao:Conceptualization,Methodology,Validation,Formal analysis,Resources,Writing -review &editing,Supervision,Funding acquisition,Project administration.
Declaration of interest statement
The authors have no relevant financial information or potential conflicts to disclose.
Acknowledgments
The authors would like to sincerely thank all the participants who gave their time for this study.Many thanks to Xinyu Yu and Chunni Wang for drawing diagrams for this study.We would also like to express our gratitude to AJE Inc.for providing language touch-up services for this article,and the Chongqing Municipal Bureau of Science and Technology and Chongqing Medical University for providing financial support for this study.
Appendices.Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.12.007.
 International Journal of Nursing Sciences2024年1期
International Journal of Nursing Sciences2024年1期
- International Journal of Nursing Sciences的其它文章
- Nursing leadership: Key element of professional development☆
- Comparison of the performance of four screening tools for sarcopeni a in patients with chronic liver disease
- Associations among frailty status,hypertension,and fall risk in community-dwelling older adults
- The prevalence and factors associated with sarcopenia in Thai older adults: A systematic review and meta-analysis Phatcharaphon Whaikid,Noppawan Piaseu*
- Air quality self-management in asthmatic patients with COPD: An integrative review for developing nursing interventions to prevent exacerbations
- Measurement properties of assessment tools of Kinesophobia in patients with cardiovascular disease: A systematic review
