Gastric inflammatory myofibroblastic tumor,a rare mesenchymal neoplasm: A case report
Manuel Fernandez Rodriguez,Pedro Joaquin Artuñedo Pe,Alejandro Callejas Diaz,Gala Silvestre Egea,Cristián Grillo ,Eva Iglesias Garcia,Jose Luis Lucena de La Poza
Abstract BACKGROUND The inflammatory myofibroblastic tumor (IMT) is a rare mesenquimal tumor of doubtful biological behaviour.It’s characterised for affecting mainly children and young adults,although it can appear at any age,being the lungs the primary affected organ (in children it represents 20% of all primary pulmonary tumors).CASE SUMMARY We present the case of a 45 year old woman,with a computed tomography (CT)finding of injury on the anterior surface of the fundus/gastric body and a solid perigastric injury of 12 mm in the ecoendoscopy.The case is presented in the tumor committee deciding to perform a laparoscopic wedge resection.The histological diagnosis was a IMT.The diagnosis is based on imaging tests like the abdominal CT,abdominal ecography and the ecoendoscopy but to confirm the diagnosis a pathological study is necessary.CONCLUSION Due to the unpredictable nature of this tumor,surgical resection is the best therapeutic option.
Key Words: Inflammatory myofibroblastic tumor;Gastric;Wedge resection;ALKmutation;Case report
INTRODUCTION
The inflammatory myofibroblastic tumor (IMT) is a rare mesenquimal tumor of doubtful biological behaviour[1].Previously known as inflammatory pseudotumor,plasmatic cell granulome,inflammatory miofibroblastoma and inflammatory miofibrohistiocityc proliferation,it’s characterised for affecting mainly children and young adults,although it can appear at any age,being the lungs the primary affected organ (in children it represents 20% of all primary pulmonary tumors)[2].
CASE PRESENTATION
Chief complaints
We present the case of a 45 year old woman who requested a follow-up in our center for a second opinión after discovery of injuries that could relate to a peritoneal carcinomatosis in other center.
History of present illness
She was examined in another center given her clinic of difuse abdominal pain of long evolution without association with any other clinical manifestation,identifying in a computed tomography (CT) a “nodular isodense image,at omental level,adyacent to the anterior right abdominal wall,without discarding infiltration of the anterior right abdominal rectum.Increase in density and trabeculation of the mesenteric fat and inespecific micronodular images,findings which could relate to a peritoneal carcinomatosis”.
Personal and family history
She has a history of venous insuficiency and cronic gastritis,cesarean and adenoidectomy.She denied family history of malignant tumours.
Physical examination
On physical examination,the vital signs were as follows: Body temperature,36.8°C;blood pressure,121/70 mmHg;heart rate,89 beats per min;respiratory rate: 17 breaths per min.Furthermore,the patient did not have abdominal pain,but minimal ascitites in flanks was found.
Laboratory examinations
Levels of serum tumour markers were normal [carcinoembryonic antigen < 0.5 ng/mL (0.0-3.0),carbohydrate antigen(CA) 125 14.0 U/mL (0.0-35.0),CA 19-9 5.0 U/mL (0.0-40.0),CA 15-3 14.9 U/mL (0.0-28.0)].No abnormality was found in routine blood analyses.
Imaging examinations
A gastroscopy is requested evidencing a gastric submucous injury of 1 cm in lesser curvature and a biopsy is performed.The anatomopatological diagnosis was superficial cronic gastritis not observing an intestinal metaplasia.
Subsequently,a positron emission tomography CT is performed with the following results: “Decrease in the size of the nodular image in greater omentum,with a mild affinity for FDG.Improvement of the ascitis and the trabeculation of the omental and mesenteric fat.Hepatic injury without metabolic translation”.
Further diagnostic work-up
A core needle biopsy is performed of the omental injury observing fibrous tissue with no tumoral infiltration and tumor markers are requested,which come out negative.
The control CT evidences “resolution of previous peritoneal affectation with persistence and stability of a left subdiafragmatic nodulary injury on the anterior surface of the fundus/gastric body” (Figure 1).A gastric Ecoendoscopy is requested identifying a solid perigastric injury of 12 mm with indeterminate endosonographic appearance.A biopsy is performed on 3 occasions,without obtaining a representative sample.
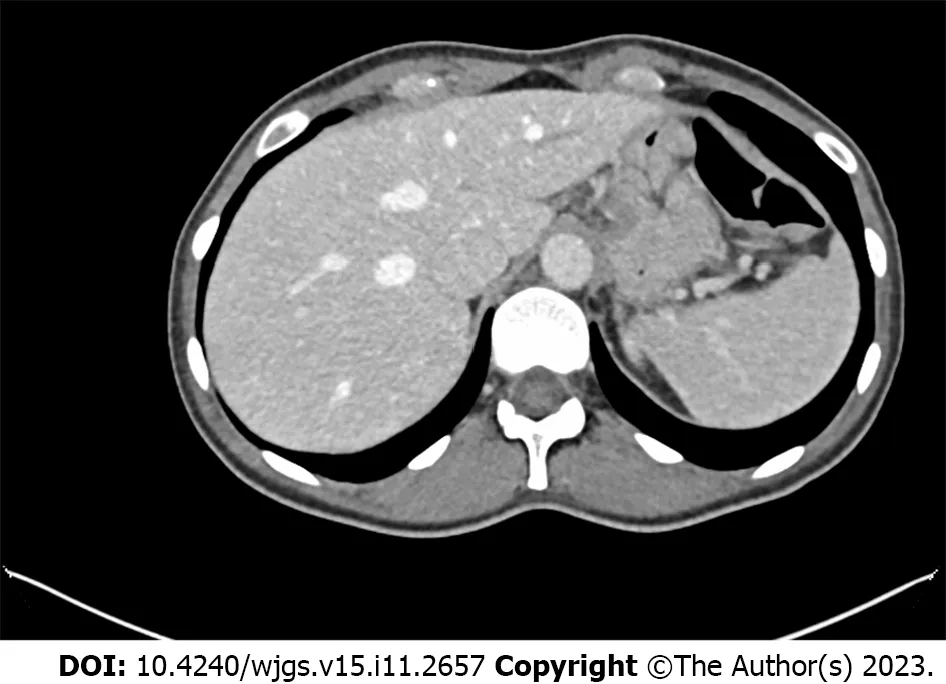
Figure 1 Nodulary injury on the anterior surface of the fundus/gastric body.
MULTIDISCIPLINARY EXPERT CONSULTATION
The case is presented in the tumor committee deciding to perform an exploratory laparoscopy.
FINAL DIAGNOSIS
The pathology study reported a “mesenquimal injury of 1.3 cm growing in the muscular layer of the gastric wall,which is in contact with the resection margin.It’s sparsely celular,mainly constituted by fibrous tissue predominantly colagenised,with presence of spindle-shaped cells without significant atypia.Presence of psammomatous calcifications is also observed.The inmunophenotype of the tumor is: CK AE1-AE3+,Actina 1A4+muy focal,ALK1-,Actina HHF35-,desmina-,caldesmon-,calponina-,CD34-,CKIT-,S100-” (Figure 2).Being the final diagnosis a IMT.
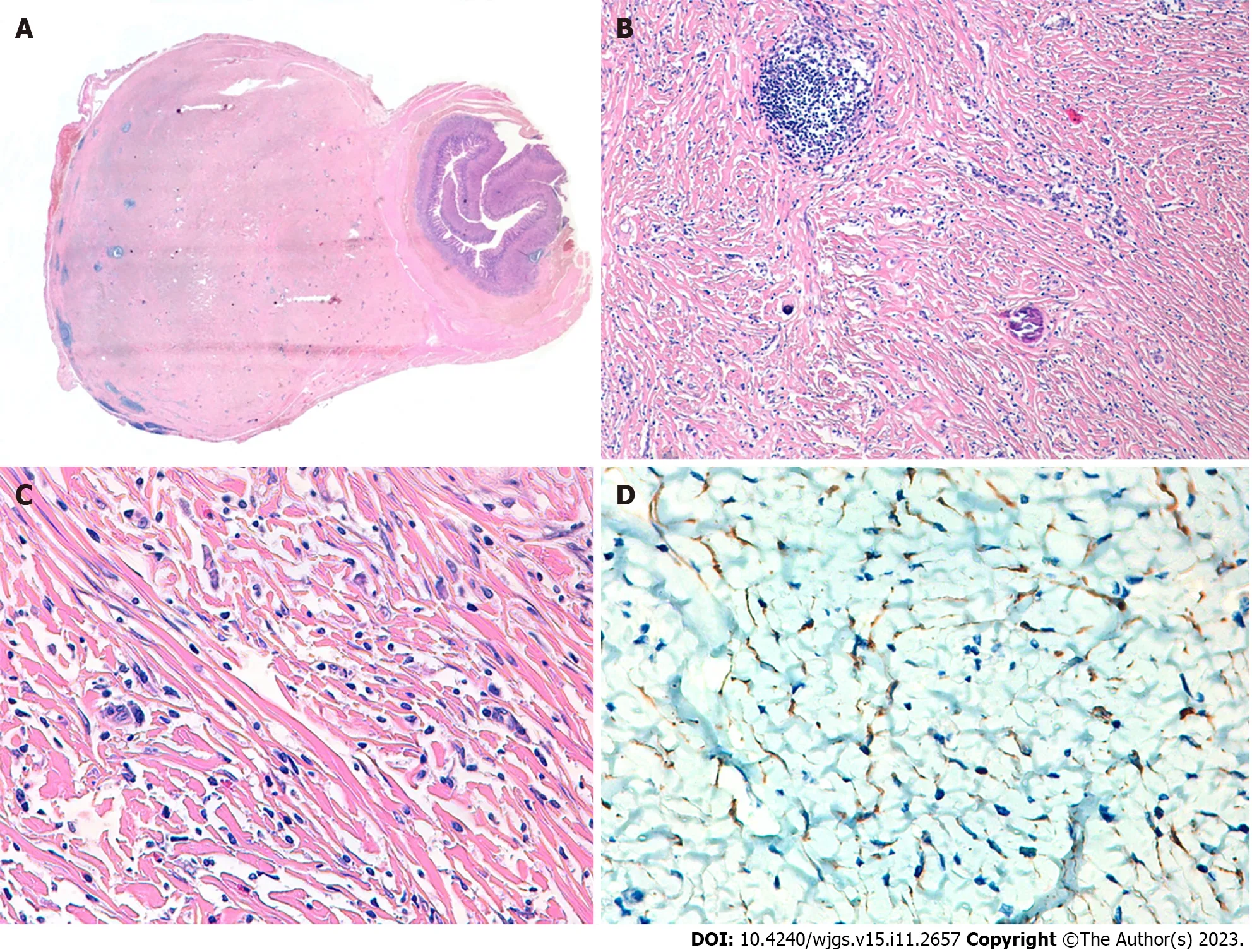
Figure 2 Histopathological analysis and immunohistochemical examination of the resected specimen. A: Panoramic image of the lesion;B:Mesenquimal injury and psamomatous calcifications;C: Mesenquimal lesion with infiltrate of eosinophils,plasma cells and masts cells;D: Positive expression of Cytokeratins AE1-AE3.
TREATMENT
We perform an exploratory laparoscopy.During the intervention,an injury of aproximately 2 cm is identified on the anterior gastric face,and a wedge resection of the injury is performed.The patient evolves favourably and is discharged to the second postoperative day.
OUTCOME AND FOLLOW-UP
At 1 mo postoperatively,the patient was still alive.Given these findings,the case is presented again to the multidisciplinar committee,which decides to carry out an annual Ecoendoscopy and toracic CT to examine the pulmonar nodule.
DISCUSSION
The IMT is rare tumor,predominantly located in the lungs but can also be found in the retroperitoneum,mesentery,head,neck and stomach.The latter case,presented by our patient,is extremely rare,with very few described in literature(Table 1).
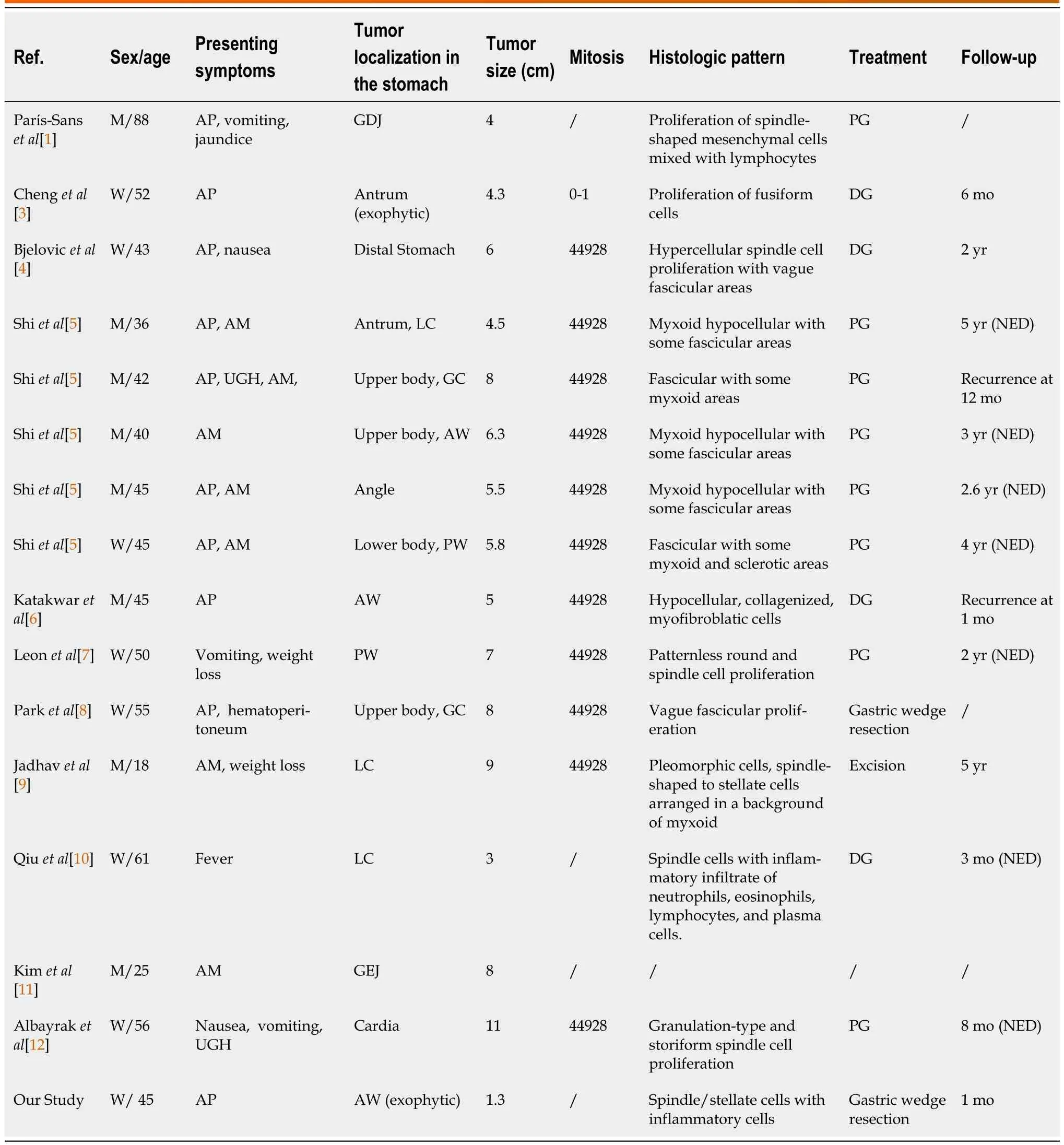
Table 1 Clinicopathological characteristics of inflammatory myofibroblastic tumors in adults,described in the literature
It is characterized by local recurrence but rarely incurs in distant metastasis[3].Risk factors for the development of IMT have not been established,but cases have been described which suggest association with Virus Epstein bar,genetic alterations like the reorganisation of the anaplastic lymphoma kinase (ALK) gene in the 2p23 cromosome or alterations of the inmune system[3,4].They are usually asymptomatic or present inespecific symptoms like abdominal pain,toracicpain,and up to 30% develop a constitutional syndrome[1,2].
The diagnosis is based on imaging tests like the abdominal TC,abdominal ecography and the ecoendoscopy[5].
The differential diagnosis includes gastrointestinal stroma tumor,fibroid inflammatory polyp,single fibrous tumor or peripheral nerve tumors,amongst others[6].
Confirmation diagnosis is obtained with histological examination,which evidences proliferations of myofibroblasts,lymphoplasmacytic infiltrate,and a myxoid stroma[5].
Fifty-six percent of IMT present reorganisation of gene ALK.These patients present a higher risk of local recurrence but not distant metastasis (negative ALK),which suggests that reactivity to the ALK could be a protective factor[3].
CONCLUSION
Due to the unpredictable nature of this tumor,surgical resection is the best therapeutic option.Regarding gastric IMTs,depending on the tumor’s location,options go from a wedge resection to a partial gastrectomy[1-3].Patients which cannot undergo surgical interventions,can be treated with a combination of radiotherapy and chemotherapy.Patients with metastatic tumors or local advanced tumors resistent to conventional chemotherapy can be treated with Crizotinib if they present a mutation of ALK or Larotrectinib o Entrectinib,if they present mutations in the gene TRK[2].
The recurrence rate in the first year after surgery is of 15%-37%,therefore clinical and radiological follow-ups are indicated,without finding in the literature a defined periodicity for them[3,4].
FOOTNOTES
Author contributions:Fernandez Rodriguez M,Artuñedo Pe P and Lucena de La Poza JL contributed to manuscript writing and editing;Silvestre Egea G provided the images of the anatomopathological study;all authors have read and approved the final manuscript.
Informed consent statement:Informed written consent was obtained from the patient for publication of this report and any accompanying images.
Conflict-of-interest statement:The authors declare that they have no conflict of interest to disclose.
CARE Checklist (2016) statement:The authors have read the CARE Checklist (2016),and the manuscript was prepared and revised according to the CARE Checklist (2016).
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:Spain
ORCID number:Manuel Fernandez Rodriguez 0009-0007-9104-9000.
S-Editor:Lin C
L-Editor:A
P-Editor:Yu HG
 World Journal of Gastrointestinal Surgery2023年11期
World Journal of Gastrointestinal Surgery2023年11期
- World Journal of Gastrointestinal Surgery的其它文章
- Systematic sequential therapy for ex vivo liver resection and autotransplantation: A case report and review of literature
- Comprehensive treatment and a rare presentation of Cronkhite-Canada syndrome: Two case reports and review of literature
- Isolated traumatic gallbladder injury: A case report
- Metachronous primary esophageal squamous cell carcinoma and duodenal adenocarcinoma: A case report and review of literature
- Organ sparing to cure stage IV rectal cancer: A case report and review of literature
- Effect of perioperative branched chain amino acids supplementation in liver cancer patients undergoing surgical intervention: A systematic review
