Hepatic venous pressure gradient: Inaccurately estimates portal venous pressure gradient in alcoholic cirrhosis and portal hypertension
Dan Zhang,Tao Wang,Zhen-Dong Yue,Lei Wang,Zhen-Hua Fan,Yi-Fan Wu,Fu-Quan Liu
Abstract BACKGROUND Portal hypertension (PHT) in patients with alcoholic cirrhosis causes a range of clinical symptoms,including gastroesophageal varices and ascites.The hepatic venous pressure gradient (HVPG),which is easier to measure,has replaced the portal venous pressure gradient (PPG) as the gold standard for diagnosing PHT in clinical practice.Therefore,attention should be paid to the correlation between HVPG and PPG.AIM To explore the correlation between HVPG and PPG in patients with alcoholic cirrhosis and PHT.METHODS Between January 2017 and June 2020,134 patients with alcoholic cirrhosis and PHT who met the inclusion criteria underwent various pressure measurements during transjugular intrahepatic portosystemic shunt procedures.Correlations were assessed using Pearson’s correlation coefficient to estimate the correlation coefficient (r) and determination coefficient (R2).Bland-Altman plots were constructed to further analyze the agreement between the measurements.Disagreements were analyzed using paired t tests,and P values < 0.05 were considered statistically significant.RESULTS In this study,the correlation coefficient (r) and determination coefficient (R2)between HVPG and PPG were 0.201 and 0.040,respectively (P=0.020).In the 108 patients with no collateral branch,the average wedged hepatic venous pressure was lower than the average portal venous pressure (30.65 ±8.17 vs. 33.25 ± 6.60 mmHg,P=0.002).Hepatic collaterals were identified in 26 cases with balloon occlusion hepatic venography (19.4%),while the average PPG was significantly higher than the average HVPG (25.94 ± 7.42 mmHg vs 9.86 ± 7.44 mmHg;P < 0.001).The differences between HVPG and PPG < 5 mmHg in the collateral vs no collateral branch groups were three cases (11.54%) and 44 cases (40.74%),respectively.CONCLUSION In most patients,HVPG cannot accurately represent PPG.The formation of hepatic collaterals is a vital reason for the strong underestimation of HVPG.
Key Words: Portal hypertension;Portal venous pressure gradient;Hepatic venous pressure gradient;Alcoholic cirrhosis;Hepatic collateral
INTRODUCTION
Alcoholic cirrhosis is a vital factor in portal hypertension (PHT),with an increased prevalence in recent years[1].The blood alcohol concentration in those with extended periods of heavy drinking tends to exceed the recommended consumption limits by far.With intrahepatic vasoconstriction,the blood flow is decreased,and hemodynamic disorder occurs,which can trigger hepatic microvascular disturbances and hypoxemia[2].Hepatocellular necrosis can occur,leading to fibrosis.This gradual development causes the segmentation and destruction of the normal structure of the hepatic lobules,with the occurrence of pseudolobules and nodular regeneration of hepatocytes,development of alcoholic cirrhosis[3],and progression to PHT.The initial stage has no characteristic symptoms,while a series of clinical patterns may occur during decompensation in patients with alcoholic cirrhosis,including gastroesophageal varices,gastrointestinal bleeding,and ascites[4,5].These symptoms are directly related to an increased portal venous pressure (PVP),which contributes to the accurate diagnosis and prognosis of patients with PHT[6].The PVP gradient (PPG) is the gold standard for the diagnosis of PHT.PPG is calculated by subtracting the inferior vena cava (IVC) pressure (IVCP) from PVP.The portal vein is located in the abdominal cavity,and PVP measurements requires strong technical skills.PVP is measured by direct cannulation of the portal vein,which is more invasive and carries a higher risk than the wedged hepatic venous pressure (WHVP).Therefore,PVP cannot be applied in a broad range of clinical settings.Currently,WHVP is used to represent PVP.The hepatic venous pressure gradient (HVPG) is calculated by subtracting the free hepatic venous pressure (FHVP) from WHVP.Because the technique for measuring hepatic vein pressure is simple,HVPG has been the gold standard in PHT diagnosis,as it indirectly reflects PPG[7].
Few studies have deeply explored the relationship between HVPG and PPG in patients with alcoholic cirrhosis and PHT.Therefore,whether HVPG can represent PPG remains controversial.
The present study aimed to examine the correlation between HVPG and PPG in patients with alcoholic cirrhosis and complications of PHT as well as determine whether HVPG can represent PPG.
MATERIALS AND METHODS
Patients’ basic information
We performed a retrospective study of patients with alcoholic cirrhosis and PHT complications who underwent transjugular intrahepatic portosystemic shunt (TIPS) placement and were admitted to our hospital between June 2017 and June 2020.Approval for the study was obtained from the ethics committee of our institution,and all patients provided informed consent to undergo TIPS creation and pressure measurements.The following inclusion criteria were applied: (1)Indication for TIPS;(2) age of 18-75 years;(3) elective TIPS surgery;and (4) normal hepatic veins and IVC.The following exclusion criteria were applied: (1) Portal vein tumor thrombus;(2) arteriovenous fistula;(3) portal vein thrombosis affecting blood flow (e.g.,generally occurring over one-third of the main portal vein);(4) administration of drugs affecting PVP within 1 wk;and (5) intraoperative factors affecting the accuracy of manometry,such as gallbladder cardiac reflex and incomplete balloon closure.
A total of 134 patients with alcoholic cirrhosis and PHT complications undergoing TIPS were included in this study.Various venous pressures were measured during the TIPS procedure,and HVPG and PPG were calculated.Patient characteristics are summarized in Table 1.Patients were aged from 18-75 years old (average,55.02 ± 10.65 years) and included 119 men (88.8%) and 15 women (11.2%).Of the 134 patients,77 cases were complicated by gastrointestinal bleeding (57.5%),46 had refractory ascites (34.3%),6 had gastrointestinal bleeding associated with refractory ascites(4.5%),and 5 had other conditions (e.g.,shunt restenosis and abdominal pain).According to the Child-Pugh classification,52 (38.8%) patients had class A,68 (50.8%) had class B,and 14 (10.4%) had class C liver disease.Fifteen patients with alcoholic cirrhosis and PHT also had hepatocellular carcinoma.
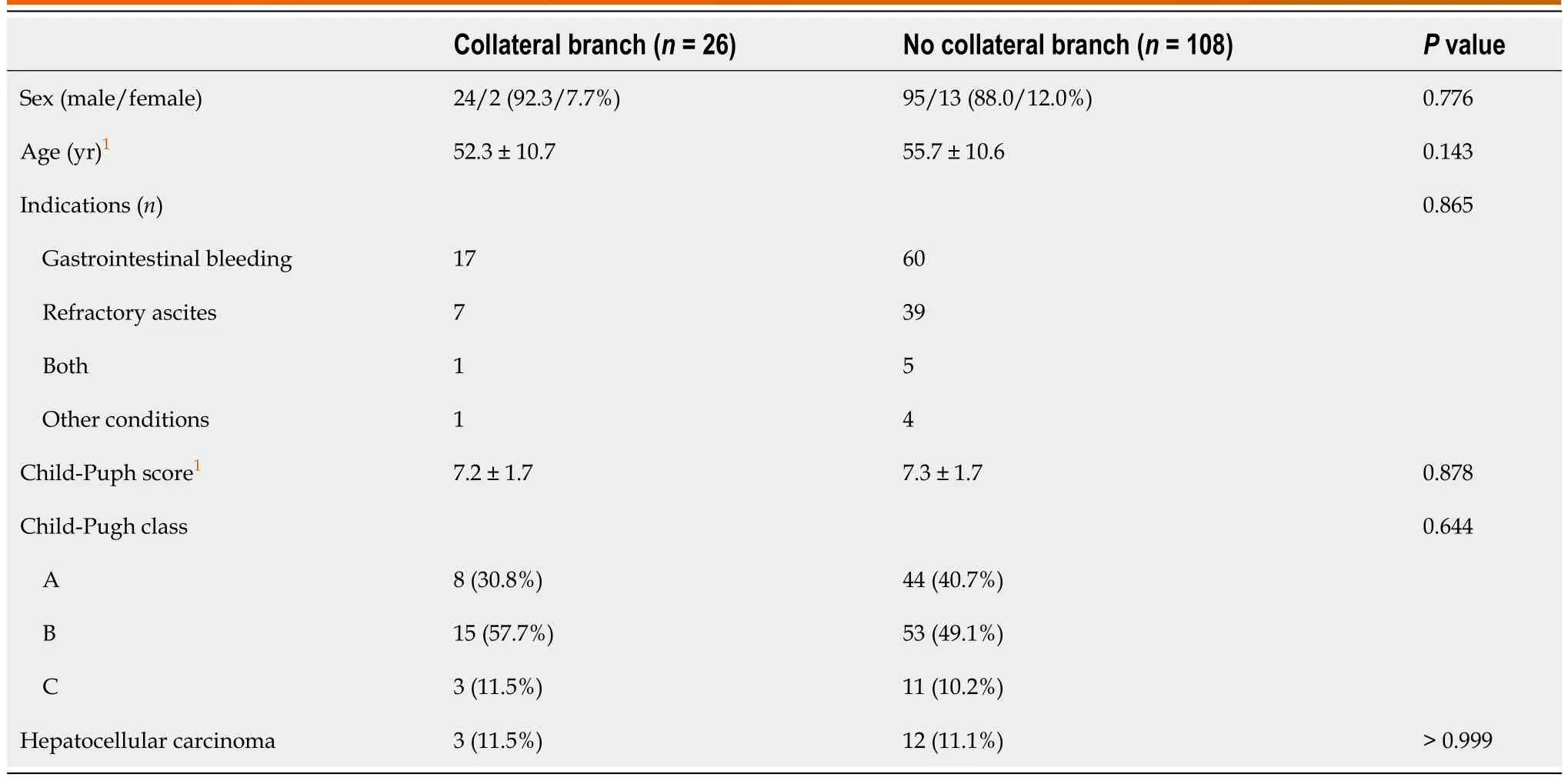
Table 1 Baseline characteristics of study patients
Pressure measurement method
Preoperatively,all patients underwent various examinations,including a complete blood count,biochemical tests;quantitation of liver function;analysis of the indocyanine green retention rate at 15 min,blood ammonia level,blood type,coagulation status,and tumor markers;electrocardiogram;portal vein ultrasound;and enhanced abdominal CT and/or magnetic resonance examination.The coagulation status,platelet count,and bilirubin,albumin,and hemoglobin levels were adjusted to adapt to interventional surgery.The effects and risks of the surgery were explained to the patients and their families,and informed consent was obtained.The ethics committee of the hospital approved the protocol[2018(01)],and all patients provided written informed consent to participate in the study.
The method for measuring the hepatic pressure has been described previously[8].Briefly,after routine disinfection and towel placement,the right internal jugular vein was punctured under local anesthesia and intubation was performed.The Rösch-Uchida Transjugular Liver Access Set (RUPS-100,specialized for TIPS;Cook Medical,United States) was placed in the right atrium and IVC,and the pressure was measured.A Fogarty balloon catheter (Edwards Lifesciences,United States) was inserted through the 10-French outer sheath.Under the guidance of the guidewire,the catheter was passed through the superior vena cava,right atrium,and IVC and was then advanced into the hepatic vein.The balloon-tipped catheter was placed 3-5 cm peripheral to the junction of the hepatic vein and the IVC.WHVP and FHVP measurements were obtained before and after occlusion of the hepatic vein using a balloon inflated with 5 mL of contrast medium.All measurements were performed three times.Pressure values were recorded when they were stable,and the mean WHVP and FHVP values were taken;HVPG was subsequently calculated.After measurements,the balloon was blocked to obtain occluded hepatic venography (15 mL of contrast agent,5 mL/s,pressure 200-300 psi),and WHVP and FHVP were remeasured.After observing the balloon catheter occlusion after balloon expansion,the balloon catheter position was adjusted for retesting and angiography once occlusion occurred.The hepatic parenchyma and portal vein were punctured through the IVC or hepatic vein.After a successful puncture,a pigtail catheter was inserted into the splenic or superior mesenteric vein for venography.Before shunting,the pressure of the main trunk of the portal vein was measured three times for an average value,and PPG was calculated.Subsequently,the liver tissue from the preshunt channel was obtained,and the shunt channel was established.The pressure of the main trunk of the portal vein was remeasured three times for an average value,and PPG was calculated.An indwelling catheter was placed in the portal vein for at least 24 h postoperatively,and PVP was measured three times daily.IVCP and right atrial pressure measurements were repeated three times during extubation to obtain average values.
Statistical methods
Statistical analyses were performed using SPSS (version 25.0;IBM SPSS Statistics,NC,United States) and GraphPad Prism 8 (GraphPad,Inc.,La Jolla,CA,United States).The results are expressed as mean ± SD.Correlations were assessed using Pearson’s correlation coefficient to estimate the correlation coefficient (r) and the determination coefficient (R2).Bland-Altman plots were constructed to further analyze the agreement between measurements.Differences between PPG and HVPG,WHVP and PVP,and FHVP and IVCP were analyzed using paired t-test.Statistical significance was set atPvalues < 0.05.
RESULTS
Among the 134 patients with alcoholic cirrhosis with PHT complications,intraoperative venograms showed portal vein collateral formation in 26 (19.40%) patients and no portal vein collateralization in 108 (80.60%) patients (Figure 1).As shown in Figure 2,WHVP and HVPG were significantly lower than PVP and HVPG,respectively.The average FHVP was higher than the average IVCP.

Figure 1 Hepatic venography during transjugular intrahepatic portosystemic shunt. A: Hepatic vein collateral branches (orange arrow) as shown on venography imagery;B: Venography image demonstrating the absence of hepatic vein collateral branch.
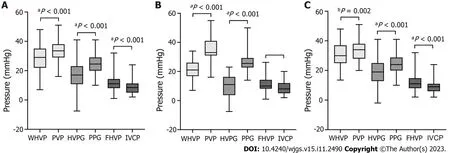
Figure 2 Box plots of pressure differences during transjugular intrahepatic portosystemic shunt. A: All patients (n=134);B: With hepatic vein collateral branches (n=26);C: With no hepatic vein collateral branch (n=108).P values were calculated by the paired t-test.WHVP: Wedged hepatic venous pressure;PVP: Portal venous pressure;HVPG: Hepatic venous pressure gradient;PPG: Portal venous pressure gradient;FHVP: Free hepatic venous pressure;IVCP: Inferior vena cava pressure.
In the 134 patients with alcoholic cirrhosis with PHT complications,the average WHVP was lower than the average PVP (28.70 ± 8.78 mmHgvs33.58 ± 6.91 mmHg;P< 0.001) (Table 2).The r and R2values between WHVP and PVP were 0.270 and 0.073,respectively (P=0.002),and the average difference between them was -4.82 ± 9.60 mmHg [95% limits of agreement (LoA) -23.64 to 13.99] (Table 3 and Figure 3).The average HVPG was lower than the average PPG (16.96 ± 9.41 mmHgvs24.73 ± 6.92 mmHg;P< 0.001) (Table 2).The r and R2values between the HVPG and PPG were 0.201 and 0.040,respectively (P=0.020),and the average difference between them was -7.77 ± 10.50 mmHg (95% LoA -28.35 to 12.80)(Table 3 and Figure 3).
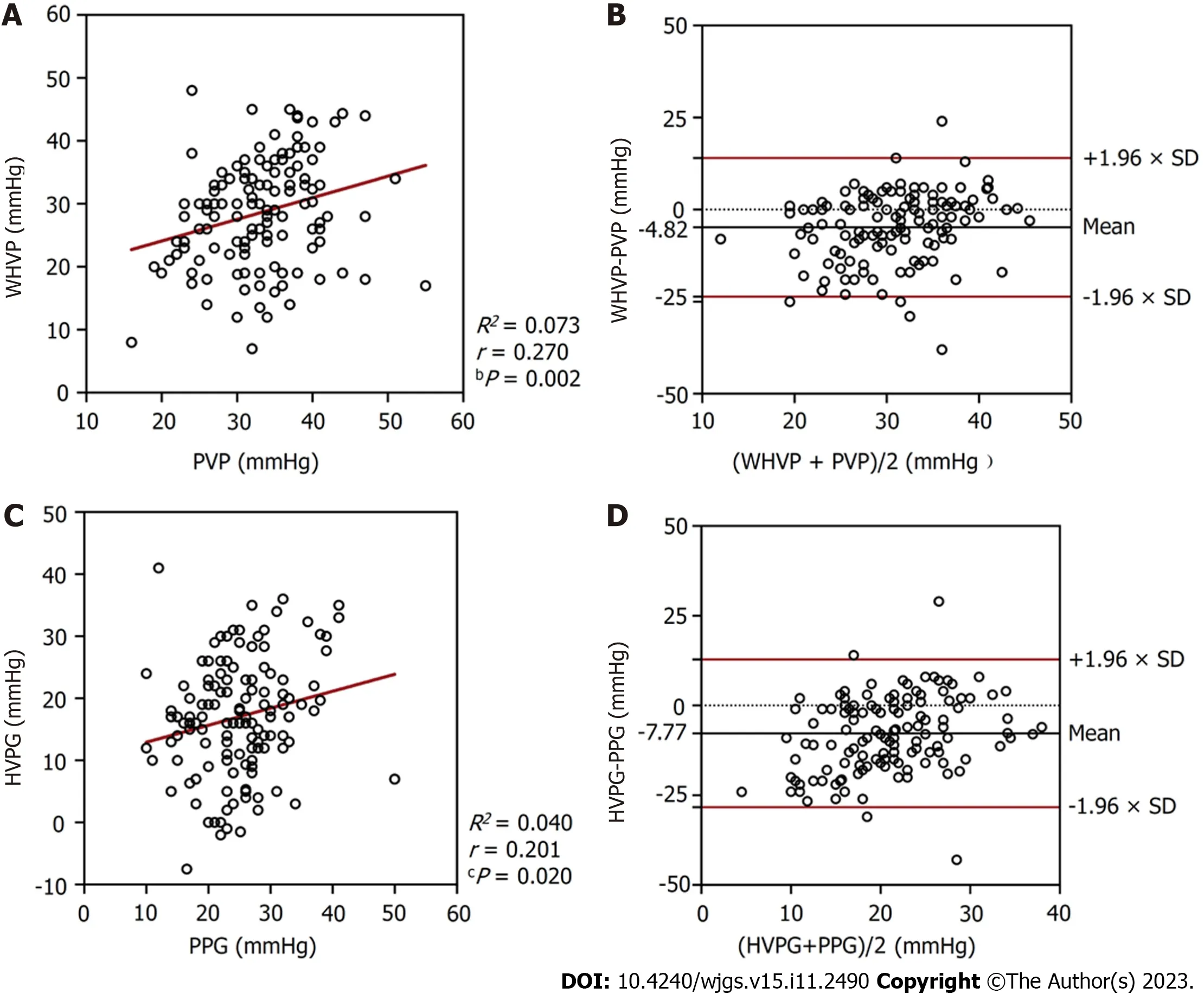
Figure 3 Relationships between the pressures measured in all patients (n=134). A: A scatterplot of wedged hepatic venous pressure (WHVP)against portal venous pressure (PVP);B: A Bland-Altman plot to assess agreement between WHVP and PVP;C: A scatterplot of hepatic venous pressure gradient(HVPG) against portal venous pressure gradient (PPG);D: A Bland-Altman plot to assess agreement between HVPG and PPG.WHVP: Wedged hepatic venous pressure;PVP: Portal venous pressure;HVPG: Hepatic venous pressure gradient;PPG: Portal venous pressure gradient.
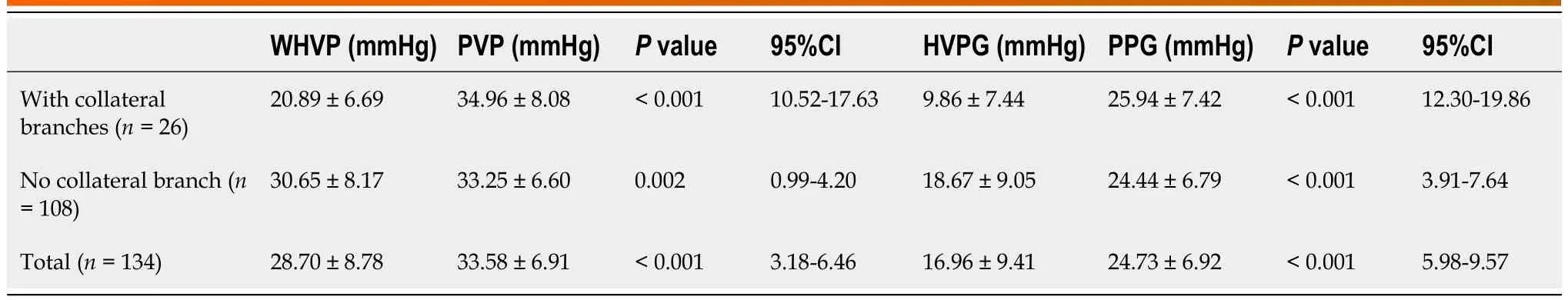
Table 2 Differences between wedged hepatic venous pressure and portal venous pressure and between hepatic venous pressure gradient and portal venous pressure gradient in patients with and without collateral branches
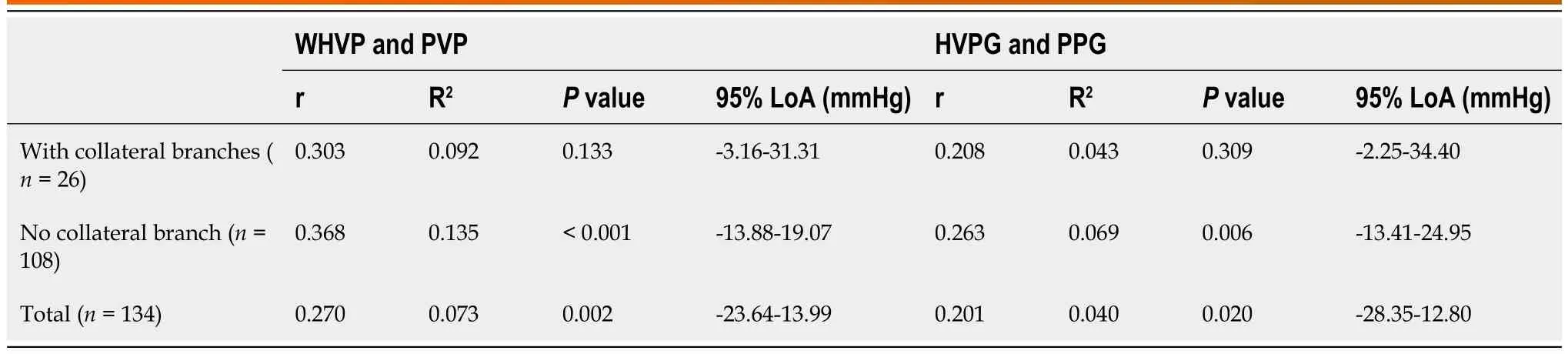
Table 3 Relationships between wedged hepatic venous pressure and portal venous pressure and between hepatic venous pressure gradient and portal venous pressure gradient in patients with and without collateral branches
In the 26 patients with collateral branches,the average WHVP was lower than the average PVP (20.89 ± 6.69 mmHgvs34.96 ± 8.08 mmHg;P< 0.001) (Table 2).The r and R2values between WHVP and PVP were 0.303 and 0.092,respectively (P=0.133),and the average difference between them was 14.07 ± 8.79 mmHg (95% LoA -3.16 to 31.31) (Table 3 and Figure 4).The average HVPG was lower than the average PPG (9.86 ± 7.44 mmHgvs25.94 ± 7.42 mmHg;P< 0.001)(Table 2).The r and R2values between the HVPG and PPG were 0.208 and 0.043,respectively (P=0.309),and the average difference between them was 16.08 ± 9.35 mmHg (95% LoA -2.25 to 34.40) (Table 3 and Figure 4).
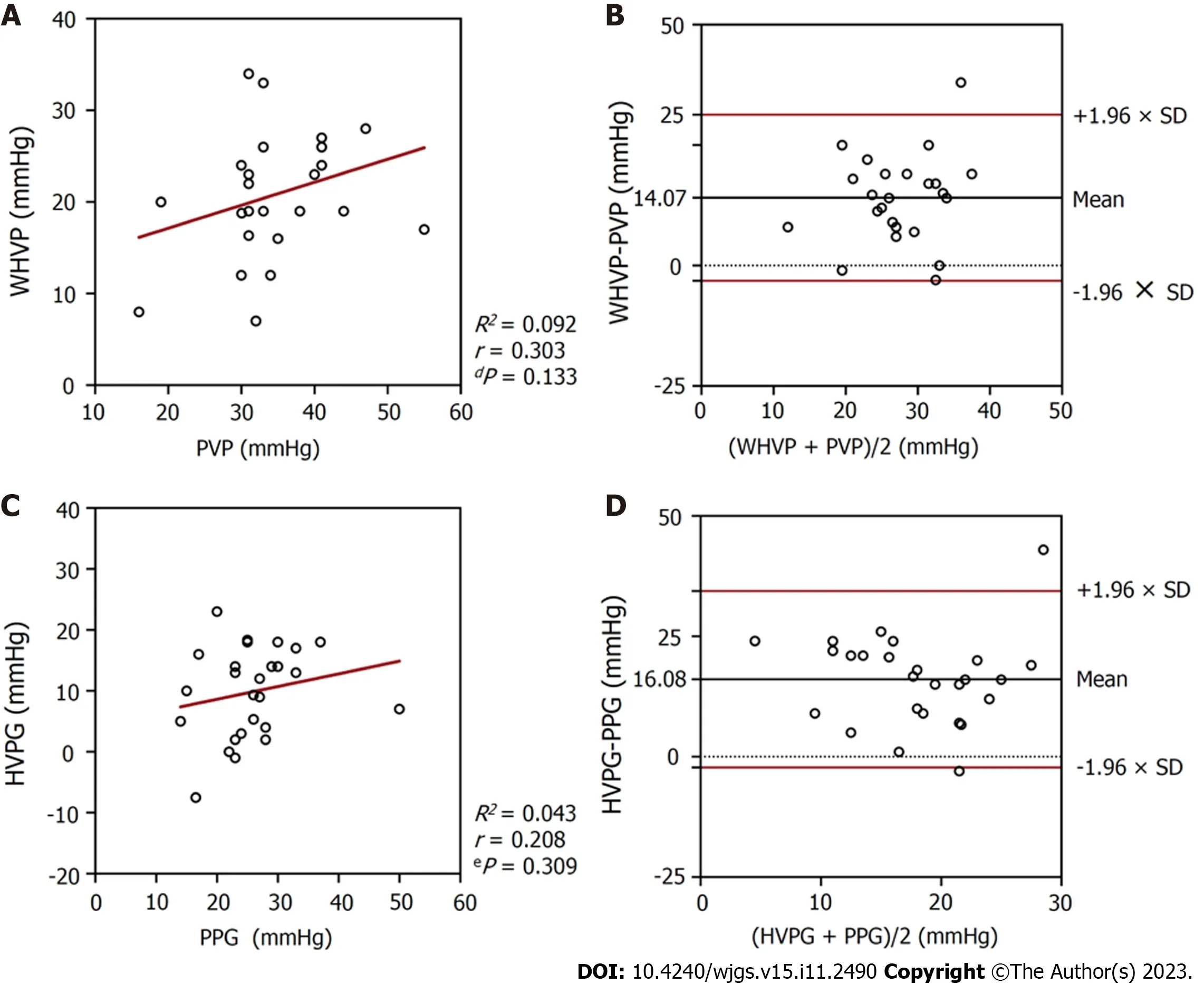
Figure 4 Relationships between the pressures measured in patients with hepatic vein collateral branches (n=26). A: A scatterplot of wedged hepatic venous pressure (WHVP) against portal venous pressure (PVP);B: A Bland-Altman plot to assess agreement between WHVP and PVP;C: A scatterplot of hepatic venous pressure gradient (HVPG) against portal venous pressure gradient (PPG);D: A Bland-Altman plot to assess agreement between HVPG and PPG.WHVP: Wedged hepatic venous pressure;PVP: Portal venous pressure;HVPG: Hepatic venous pressure gradient;PPG: Portal venous pressure gradient.
In the 108 patients with no collateral branches,the average WHVP was lower than the average PVP (30.65 ± 8.17 mmHgvs33.25 ± 6.60 mmHg;P=0.002) (Table 2).The r and R2values between WHVP and PVP were 0.368 and 0.135,respectively (P< 0.001),and the average difference between them was 2.60 ± 8.41 mmHg (95% LoA -13.88 to 19.07)(Table 3 and Figure 5).The average HVPG was lower than the average PPG (18.67 ± 9.05 mmHgvs24.44 ± 6.79 mmHg;P< 0.001) (Table 2).The r and R2values between the HVPG and PPG were 0.263 and 0.069,respectively (P=0.006),and the average difference between them was 5.77 ± 9.79 mmHg (95% LoA -13.41 to 24.95 mmHg (mean) (Table 3 and Figure 5).
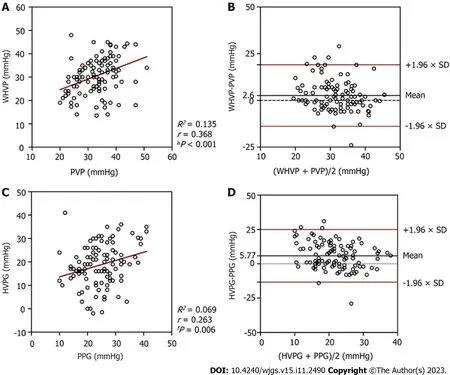
Figure 5 Relationships between the pressures measured in patients with no hepatic vein collateral branch (n=108). A: A scatterplot of wedged hepatic venous pressure (WHVP) against portal venous pressure (PVP);B: A Bland-Altman plot to assess agreement between WHVP and PVP;C: A scatterplot of hepatic venous pressure gradient (HVPG) against portal venous pressure gradient (PPG);D: A Bland-Altman plot to assess agreement between HVPG and PPG.WHVP: Wedged hepatic venous pressure;PVP: Portal venous pressure;HVPG: Hepatic venous pressure gradient;PPG: Portal venous pressure gradient.
As shown in Figure 6,3 (11.54%) patients in the collateral branches group and 59 (54.63%) patients in the no collateral branches groups had differences between WHVP and PVP of less than 5 mmHg.In addition,3 (11.54%) patients in the collateral branches group and 44 (40.74%) patients in the no collateral branches groups had differences between HVPG and PPG of less than 5 mmHg.
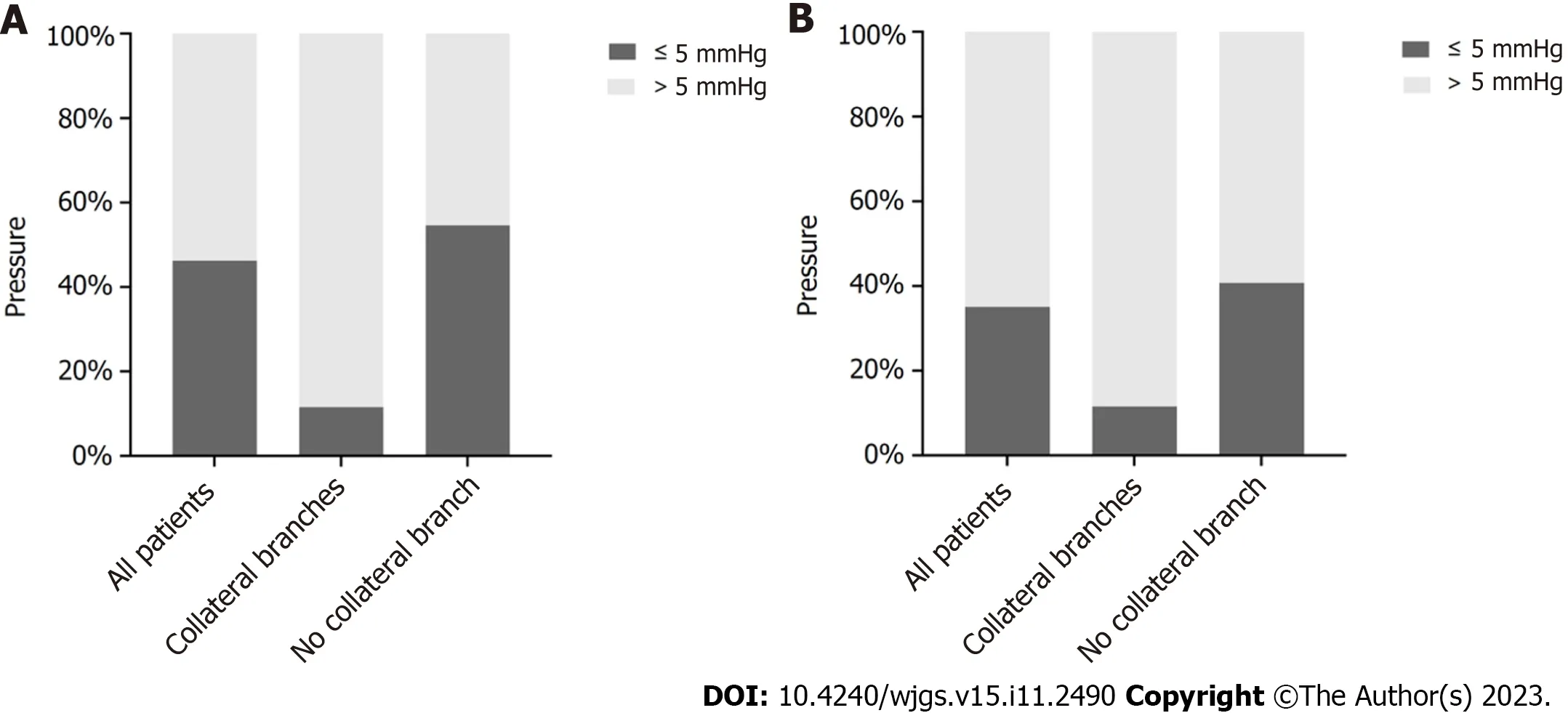
Figure 6 Difference between the pressures measured in patients with alcoholic cirrhosis and portal hypertension. A: The difference between wedged hepatic venous pressure and portal venous pressure.B: The difference between hepatic venous pressure gradient and portal venous pressure gradient.
DISCUSSION
Alcoholic cirrhosis associated with PHT is a common liver disease.Based on the pathological changes in the liver,significant changes in liver hemodynamics occur,and vascular resistance is increased,causing gradually elevated PVP.Clinically,the symptoms gradually become more conspicuous and their severity is directly associated with the degree of PVP[9].In clinical practice,the degree of PHT in patients with liver cirrhosis is mainly evaluated based on clinical symptoms,signs,imaging examinations,and gastroscopy;however,these evaluation methods typically have a low sensitivity.Accurate assessments require direct PVP measurements[10].Comparing the risks and benefits of the assessment,the technique is too complicated,and the trauma is too severe.In recent years,many researchers have measured the hepatic vein pressure instead of directly measuring PVP as the gold standard to reflect PVP in clinical applications[11,12].Research on noninvasive portal vein manometry also considers the hepatic vein pressure as a standard.There are two principal ways to measure the hepatic vein pressure: Intubating the hepatic vein through the jugular or femoral vein to measure WHVP or FHVP,respectively.HVPG is calculated by subtracting FHVP from WHVP.WHVP can be measured using two methods: Measuring the pressure after the balloon blocks the hepatic vein or obtaining the pressure by inserting an end-hole catheter into the end of the branch of the hepatic vein.The former method is more accurate and is commonly used[13].In normal liver hemodynamics,PVP is equal to or greater than the hepatic sinus pressure,WHVP is equal to the hepatic sinus pressure,and FHVP is 0.5-1.0 mmHg higher than IVCP[7].Therefore,HVPG indirectly represents PPG and the portal vein perfusion pressure[8,14].It is more meaningful to use PPG than PVP to predict the risk of various PHT complications[8,15].Significant pathological changes occur in the hepatic tissuestructure of patients with alcoholic cirrhosis and PHT,resulting in significant changes in liver hemodynamics.Regarding whether WHVP is representative of PVP,some scholars believe that WHVP and PVP are correlated in patients with alcoholic cirrhosis[16,17].However,this remains controversial,as the number of cases is limited.Difference in WHVP and PVP have been reported in patients with cirrhosis with the same etiology but different pathology types.In macronodular cirrhosis,WHVP and PVP are poorly correlated[18],possibly due to the existence of normal tissues between macronodules[16].Few studies have reported whether HVPG can accurately reflect PPG.The results of this study showed that the correlation between WHVP and PVP is very poor,and the correlation between HVPG and PPG also poor.In 47 patients,PPG exceeded HVPG by less than 5 mmHg,accounting for 35.1% of patients.Therefore,most HVPG measurements cannot accurately represent PPG,partly because of the vascularization of the collateral branches of the hepatic vein.In our study,26 patients (19.4%) had collateral branches of the hepatic vein,and WHVP and HVPG were both grossly underestimated.These results are consistent with those of other studies.Patients without collateral branches of the hepatic vein accounted for a large proportion (80.6%).The average WHVP was lower than the average PVP,and the average HVPG was significantly lower than the average PPG.For a small number of patients,the WHVP was greater than the PVP,and the HVPG was greater than the PPG.However,the underlying mechanism remains unclear.Reportedly,patients with a WHVP higher than the PVP are likely to have adverse hepatic blood flow,opening of the paraumbilical vein,anastomoses between the portal vein and IVC,and a gastrorenal shunt[16,19].These scenarios were not present in the vast majority of patients in this study.
The factors influencing the pressure measurements were strictly controlled before the operation.Patients who received preoperative health education and those who underwent elective surgery were selected,and patients were given adequate psychological preparation to allow for active compliance with the procedure.Suitable paracentesis was performed for patients with large ascites,and the use of drugs that affect the venous pressure,such as non-selective βreceptor blockers that influence PVP[12,20-22],or propofol deep sedation,which can affect PPG[19,23],were avoided.During the TIPS procedure and pressure measurement,clinicians should perform local anesthesia,measure the pressure after the patient is stable,repeat the measurement several times,and ensure that the catheter is at the same location for each measurement.Gallbladder-heart reflections and incomplete balloon occlusion shoud be considered during the procedure.If these conditions are not corrected,patients should be excluded.
Our study was limited by the fact that this was a retrospective study with a small sample size.Although all study patients had alcoholic cirrhosis patients,the degree of progression of cirrhosis and the pathological type varied,with some cases progressing to hepatocellular carcinoma,resulting in different hepatic structural and hemodynamic changes,the potential impact of which is unclear.Considering these preliminary findings,prospective studies are necessary to validate our findings.
CONCLUSION
In conclusion,the correlation is very poor between WHVP and PVP as well as that between HVPG and PPG in patients with alcoholic cirrhosis and complications of PHT.HVPG cannot accurately represent PPG in most patients,and the former is lower than the latter.The formation of hepatic collaterals is a vital reason for the strong underestimation of HVPG.Except for the influencing factors of hepatic collateral branches in a few patients,the correlation in most cases remained poor.The cause remains unknown,and further investigations are required in this area to elucidate these mechanisms.
ARTICLE HIGHLIGHTS
Research background
The hepatic venous pressure gradient (HVPG),rather than the portal venous pressure gradient (PPG),is regarded as the gold standard for diagnosing portal hypertension (PHT).
Research motivation
The relationship between HVPG and PPG is controversial and lacks substantial research to prove it.
Research objectives
This study aimed to classify the correlation between HVPG and PPG in patients with alcoholic cirrhosis and PHT.
Research methods
This retrospective analysis of various pressures during transjugular intrahepatic portosystemic shunt (TIPS) procedures explored the relationship between HVPG and PPG in patients with alcoholic cirrhosis and PHT.
Research results
The correlation coefficient (r) and determination coefficient (R2) between HVPG and PPG were 0.201 and 0.040,respectively (P=0.020).Hepatic collaterals were identified in 26 patients with balloon occlusion hepatic venography(19.4%),while the average PPG was significantly higher than the average HVPG (25.94 ± 7.42 mmHgvs9.86 ± 7.44 mmHg;P< 0.001).The collateral versus no collateral branches groups had 3 (11.54%) and 44 (40.74%) patients,respectively,with differences of < 5 mmHg between HVPG and PPG.
Research conclusions
HVPG cannot accurately represent PPG in most patients.The formation of hepatic collaterals is a vital reason for the strong underestimation of HVPG.
Research perspectives
Based on different pressures during TIPS procedures,the correlation and differences between HVPG and PPG of patients were explored.
FOOTNOTES
Author contributions:Liu FQ designed the research;Wang T,Yue ZD,Wang L,Fan ZH and Wu YF performed the research;Zhang D analyzed the data and wrote the paper;Liu FQ reviewed and revised the manuscript;All authors have read and approved the final manuscript.
Supported bythe Capital Health Research and Development of Special,No.2018-1-2081;National Natural Science Foundation of China,No.81871461.
Institutional review board statement:The study was reviewed and approved by the Beijing Shijitan Hospital,Capital Medical University Institutional Review Board [2018(01)].
Informed consent statement:All study participants or their legal guardian provided informed written consent about personal and medical data collection prior to study enrolment.
Conflict-of-interest statement:The authors declare that they have no conflict of interest.
Data sharing statement:Technical appendix,statistical code,and dataset available from the corresponding author at liufuquan@ccmu.edu.cn.Participants gave informed consent for data sharing.
Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license,which permits others to distribute,remix,adapt,build upon this work non-commercially,and license their derivative works on different terms,provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin:China
ORCID number:Dan Zhang 0000-0003-1478-0338;Tao Wang 0000-0002-2714-9804;Zhen-Dong Yue 0000-0001-5403-8336;Lei Wang 0000-0003-4080-1630;Zhen-Hua Fan 0000-0001-5417-1997;Yi-Fan Wu 0000-0003-2709-2729;Fu-Quan Liu 0000-0003-1972-7712.
S-Editor:Lin C
L-Editor:A
P-Editor:Zhang YL
 World Journal of Gastrointestinal Surgery2023年11期
World Journal of Gastrointestinal Surgery2023年11期
- World Journal of Gastrointestinal Surgery的其它文章
- Systematic sequential therapy for ex vivo liver resection and autotransplantation: A case report and review of literature
- Gastric inflammatory myofibroblastic tumor,a rare mesenchymal neoplasm: A case report
- Comprehensive treatment and a rare presentation of Cronkhite-Canada syndrome: Two case reports and review of literature
- Isolated traumatic gallbladder injury: A case report
- Metachronous primary esophageal squamous cell carcinoma and duodenal adenocarcinoma: A case report and review of literature
- Organ sparing to cure stage IV rectal cancer: A case report and review of literature
