Evidence relating cigarette, cigar and pipe smoking to lung cancer and chronic obstructive pulmonary disease: Meta-analysis of recent data from three regions
Peter Nicholas Lee, Katharine J Coombs,Jan S Hamling
Abstract
Key Words: Cigarettes; Cigars; Pipes; Lung cancer; Meta-analysis; Review
INTRODUCTION
It is well-known[1,2] that smoking cigarettes markedly increases the risk of various diseases, particularly lung cancer, chronic obstructive pulmonary disease, ischaemic heart disease and acute myocardial infarction, and stroke.However, the increase in risk associated with smoking of cigars and pipes, and with the use of other nicotine-containing products is less well characterized.As part of a project comparing relative risks (RRs) of these diseases for currentvsnever use of various products, we have previously published in this journal a review with meta-analysis of the epidemiological evidence relating to the use of snus (Swedish snuff) and of smokeless tobacco[3].Here we present a systematic review with meta-analysis of the evidence relating both lung cancer and chronic obstructive pulmonary disease (COPD) to current smoking of cigarettes, cigars and pipes based on publications in 2010 to 2020,and a planned further publication will review recent evidence relating current smoking of the same three products to ischaemic heart disease, acute myocardial infarction and stroke.More recently introduced products, such as electronic cigarettes and heat-not-burn products, are not considered in our project at this time, as large long-term epidemiological studies relating their use to the main smokingrelated diseases have not so far been conducted.It should be noted that our objective is only to conduct meta-analyses relating to current use of the products considered, and to investigate how the resultant RR estimates vary by other factors, such as sex and region.We do not consider how RRs vary by amount smoked, duration of smoking, or time quit.
The work described in this publication represents a partial update of two earlier meta-analyses we were involved in.One related lung cancer risk to smoking of cigarettes, cigars and pipes, based on publications in the 1900s[4], reporting overall random-effects RR estimates of 8.43 (95%CI 7.63-9.31) for cigarettes, 4.67 (CI 3.49-6.25) for cigars and 5.20 (CI 3.50-7.73) for pipes.The other related COPD risk to cigarette smoking only based on publications up to 2006[5], giving an RR estimate of 3.51 (CI 3.08-3.99).We compare the RR estimates we derive from the more recent publications with these earlier results,and with the findings of various other meta-analyses published in 2000 to 2020[6-18].
MATERIALS AND METHODS
Study inclusion and exclusion criteria
Attention was restricted to publications in English in the years 2010 to 2020 which provided RR estimates for lung cancer or COPD comparing current and never smokers of cigarettes, of cigars, or of pipes.These had to be based on epidemiological cohort or nested case-control studies or randomized controlled trials which were conducted in North America, Europe or Japan, and which involved at least 100 cases of the disease of interest.The studies were excluded if they were restricted to specific types of lung cancer or COPD, or to patients with specific medical conditions, or if the results were superseded by corresponding later results from the same study.
Literature searches
Initially, at stage 0, literature searches were conducted on MEDLINE using simple text searches for publications in 2010 to 2020.For lung cancer the search, carried out on November 7, 2021, used the terms “smoking” and “lung cancer”.For COPD the search, carried out on 9th November 2021, linked“smoking” to the term “COPD” or the following terms associated with it – “Pulmonary Disease,Chronic Obstructive”, “Lung Disease, Obstructive”, “Bronchitis” and “Emphysema”.
Then, at stage 1, titles and abstracts were screened to select publications that appeared to describe studies satisfying the inclusion criteria, and both meta-analyses and reviews that may cite other relevant publications.The initial screening was usually carried out by Katharine J Coombs (KJC), with acceptances checked by Peter N Lee (PNL), though in some cases PNL did the initial screening and KJC checked.Disagreements were resolvedviadiscussion.
Then, at stage 2, the full texts of the selected publications (and of relevant Supplementary material and other publications linked to them in the MEDLINE search) were obtained, and examined by PNL,who classified the publication as being an acceptance (i.e.it appeared to include relevant data), a reject(giving reason), a relevant review or a relevant meta-analysis.The rejections were then checked by KJC,with any disagreements resolved.
At stage 3, additional accepted publications not detected by the MEDLINE searches were sought by examination of reference lists of the accepted papers and of the relevant reviews and meta-analyses and,when obtained, dealt with as in stage 2.
Finally, at stage 4, copies of all the accepted publications (not the meta-analyses) were organized, first by country, and then by study within country, with studies conducted in multiple countries considered as a separate group.The aim was to eliminate from consideration those publications giving results for a study that were superseded by a later publication, and those publications which, on more detailed examination, did not fully satisfy the inclusion criteria.
Data entry
Data were entered into a study database and into an associated RR database.The study-specific information recorded was: Study name; country; region (North America, Europe, Japan or multiple);study design (cohort, nested case-control, or randomized controlled), study population (international,national, regional or specific,e.g.workers in a particular industry); study size (number of cases of the disease); year of start; length of follow-up; sexes considered (males only, females only, or both); and age range considered.
The information recorded relating to each RR was: The RR itself and its 95% confidence interval (CI),the RR and CI being estimated from the data provided if necessary; the study to which it related; an identifier for the paper providing the estimate; the year of publication of the paper; for COPD only the definition of COPD used; the product considered (cigarettes, cigars or pipe); whether the RR related to exclusive use of the product; the sex to which it related (males, females or combined - combined RRs only being entered if sex-specific RRs were not available); the age range considered; the years of followup considered; the endpoint (from death certification only, or involving in-life diagnosis); whether a latency rule was applied (i.e.whether cases identified in the first few years of follow-up were ignored),and the number of adjustment factors applied to the risk estimate.
Meta-analyses
Meta-analyses could not be conducted relating risk of COPD to current cigar or current pipe smoking as the available data originated from a single study.
Otherwise, individual study RR estimates were combined using fixed- and random-effects metaanalyses[19], with the significance of between-study heterogeneity also estimated.
For current cigar and for current pipe smoking and the risk of lung cancer, where the extent of available data was rather limited, meta-analyses were based on the most adjusted RR estimate per study, with heterogeneity studied by sex and by region.
For current cigarette smoking, where data were much more extensive, more detailed meta-analyses were conducted, as described below.
Initially, meta-analyses were conducted based on either two RR estimates from each study, if separate RRs were available for each sex, or on a single estimate if the study reported only combined sex results or results for only one sex.Where there was a choice of RRs available for a study, those selected were based on a sequence of preferences applied in turn.
For lung cancer the sequence was as follows: (1) Exclusive rather than non-exclusive cigarette smoking; (2) a latency rule had been applied rather than not; (3) the longest follow-up period available;4) adjustment for the most possible confounders; (5) lung cancer identified by diagnosis rather than death; and (6) separate sex RRs selected rather than the combined sex RR.For COPD the sequence only involved preferences 1, 2 and 6 in turn, due to the more limited data.
For lung cancer the RRs were estimated overall, with heterogeneity studied by the following factors:Sex; region; study population; year of start; study size; exclusive use; latency rule used; study type;lowest age considered; years of follow-up; endpoint; and number of adjustment factors.Grouped levels of the variables were used as appropriate.For COPD, the same factors were studied, except that study type was omitted (all the COPD studies proving to be cohort studies), and that heterogeneity was also studied by definition of COPD (excluding bronchiectasis, including bronchiectasis, or other).
For lung cancer it became clear that RRs were much lower in Japan than in North America or Europe,so these analyses were also repeated excluding RRs from Japan.
While these meta-analyses and heterogeneity investigations were based on variation in RRs between studies, some additional investigations were conducted on within-study variation in RRs, based on data from the same publication.For sex, these meta-analyses were based on the ratio of the RR for males to that for females, while for level of adjustment, results were compared based on the ratio of the RR adjusted for multiple potential confounding variables to the RR adjusted for no variables.Where multiple pairs of results were available within a publication, the pair selected was chosen based on the preferences described above.For within-study variation of other characteristics, where there was far less data available, the results were simply summarized in the text.
RESULTS
Literature searches
Flowcharts of the searches are shown in Figure 1 for lung cancer and in Figure 2 for COPD.Starting with over 10000 papers identified in the initial MEDLINE searches for each disease, 53 study reports were identified for lung cancer and 19 for COPD, which provided results for, respectively, 44 and 18 studies.
For lung cancer there were in total 152 RRs available for analysis, 138 for cigarette smoking, six for cigar smoking and eight for pipe smoking, single studies sometimes providing multiple estimates,e.g.for separate sexes, for several levels of adjustment for covariates, or for several products.For COPD there were 58 RRs available for analysis, 52 for cigarette smoking, three for cigar smoking and three for pipe smoking.Table 1 (lung cancer) and Table 2 (COPD) gives some details of the studies considered.Eleven of these studies provided data for both diseases.
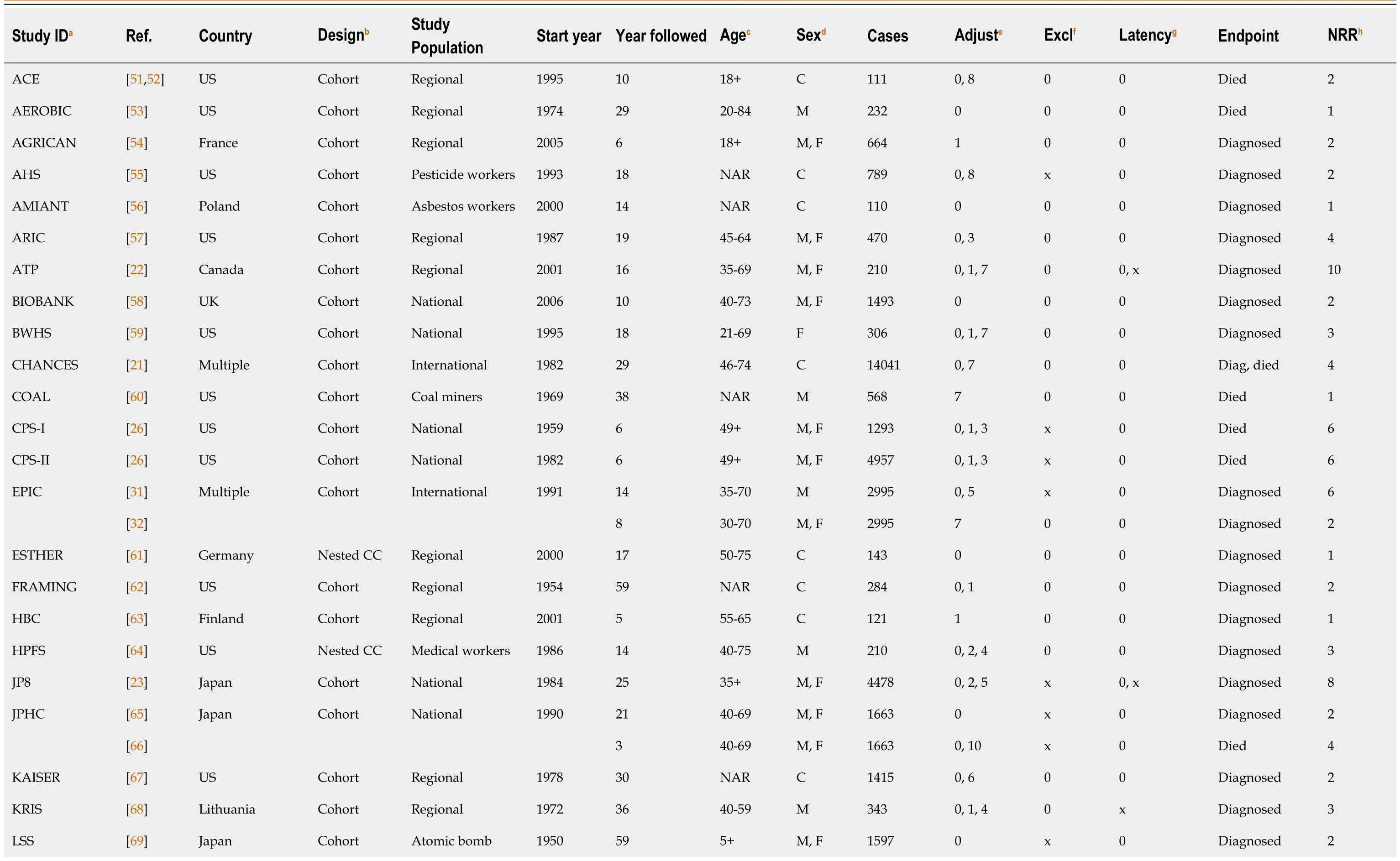
Table 1 Details of the 44 studies of lung cancer

survivors MWOMEN [24]UK Cohort National 1996 15 50-69 F 6331 0, 10 x 0, x Died 3 NHANES [70]US Cohort National 1988 18 40+C 269 0 0 0 Died 1 NHIS [71]US Cohort National 1987 28 18-84 C 7420 0, 11 0 0 Died 2[72]9 25-79 M, F 7420 0, 4 0 x Died 4 NHS [73]US Cohort Medical workers 1980 24 34-59 F 1729 1, 13 0 0 Died 2[74]24 38-63 F 1729 0 0 0 Diagnosed 1 NIHAARP [75]US Cohort Regional 1995 11 50-71 M, F 17846 0, 5 x x Diagnosed 4[76]16 50-71 C 17846 0 0 0 Diagnosed 1 NLCS [29]Netherlands Nested CC National 1986 17 55-69 C 3355 0 0 0 Diagnosed 3[30]20 55-69 M, F 3355 0 0 0 Diagnosed 2 NLMS [28]US Cohort National 1985 26 35-80 C 3890 0, 1, 5 x 0 Died 8 NLST [77]US Cohort Construction workers 1998 18 NAR M 352 0, 2 0 0 Died 2 NONMET [78]US Nested CC Non-metal miners 1947 50 NAR M 198 0, 7 0 0 Died 2 NOWAC [79]Norway Cohort National 1991 24 31-70 F 1507 0, 1, 3 0 0 Diagnosed 3 PLCO [80]US Cohort Regional 1993 15 55-74 C 1040 0 0 0 Died 1[81]15 55-74 F 1040 6 0 0 Died 1 QRESEAR [82]UK Cohort National 1998 15 25-84 M, F 32187 0, 6 0 0 Diagnosed 4 SCCS [83]US Nested CC Regional 2002 14 40-79 M, F 1334 0 0 0 Diagnosed 2[84]7 40-79 C 1334 10 0 0 Diagnosed 1 SHEETME [85]Multiple Cohort Sheet metal workers 1986 24 NAR M 808 0 0 0 Died 1 THIN [86]UK Cohort National 2000 12 30-99 C 1015 0 0 0 Diagnosed 1 THREEC [20]Norway Cohort Regional 1974 33 20-49 M 858 0, 10 0, x 0 Died 6[87]35 35-49 M, F 858 0 0 x Died 2 USA5[26]US Cohort National 1986 24 45+M, F 11420 0, 1, 3 0 0 Died 6 VETERAN [88]US Cohort Regional 1987 28 21-89 M 105 0 0 0 Diagnosed 1 VITAL [89]US Cohort Regional 2000 7 50-76 C 797 0 0 0 Diagnosed 1

aStudy IDs are ACE: The Adverse Childhood Experiences Study; AEROBIC: Aerobics Center Longitudinal Study; AGRICAN: Agriculture and Cancer Study; AHS: Agricultural Health Study; AMIANT: Amiantus; ARIC: Atherosclerosis Risk in Communities study; ATP: Alberta’s Tomorrow Project; BIOBANK: The UK Biobank Study, BWHS: The Black Women's Health Study; CHANCES: Consortium on Health and Ageing: Network of Cohorts in Europe and the United States; COAL: Underground coal miners from 31 US mines; CPS-I: Cancer Prevention Study 1; CPS-II: Cancer Prevention Study 2; EPIC: European Prospective Investigation into Cancer and Nutrition; ESTHER: Epidemiologische Studie zu Chancen der Verhütung, Früherkennung und optimierten Therapie chronischer Erkrankungen in der älteren Bevölkerung; FRAMING: Framingham Heart Study; HBC: Helsinki Birth Cohorts; HPFS: Health Professionals Follow-up Study; JP8: Pooled analysis of eight prospective studies in Japan; JPHC: Japan Public Health Center-based Prospective Study; KAISER: Kaiser Permanente Medical Care Program Study; KRIS: Kaunas–Rotterdam Intervention Study; LSS: Life Span Study; MWOMEN: Million Women Study; NHANES: National Health and Nutrition Examination Survey; NHIS: National Health Interview Survey; NHS: Nurses' Health Study; NIHAARP: National Institutes of Health-American Association of Retired Persons Diet and Health Study; NLCS: Netherlands Cohort Study on Diet and Cancer; NLMS: National Longitudinal Mortality Study; NLST: National Lung Screening Trial; NONMET: Nonmetal Mining; NOWAC: Norwegian Women and Cancer study; PLCO: Prostate, Lung, Colorectal, and Ovarian Cancer study; QRESEAR: QResearch database; SCCS: Southern Community Cohort Study; SHEETME: Sheet Metal Workers; THIN: The Health Improvement Network; THREEC: Three counties in Norway; USA5: Pooled analysis of five US cohort studies, VETERAN: Veterans Exercise Testing Study; VITAL: Vitamins and Lifestyle; VLAGT:Vlagtwedde-Vlaardingen Study; WHI: Women’s Health Initiative Observational Study; US: United States; UK: United Kingdom.bNested CC: Nested case-control.cNAR: No age restriction.dC: Results only for sexes combined.eNumber of adjustment factors for which RR available (0 = unadjusted, 1 = age adjusted, N > 1 = adjusted for N factors).fx: Results available for exclusive use.gx: Results available with deaths excluded in the early period of follow-up.hNumber of RRs available.
Cigarette smoking results
The full details of the results summarized below are given in Supplementary material 1 for lung cancer and Supplementary material 2 for COPD.Below, the results are summarized firstly for lung cancer (see also Table 3) and then for COPD (see also Table 4).
Lung cancer
Data available for cigarette smoking: Each of the 44 studies provided data for current cigarette smoking, with data coming from two publications for nine of these studies.Of the 44 studies, 26 were from North America [24 United States (US), one Canada, and one from both the US and Canada], 14 were from Europe [four United Kingdom (UK), two Netherlands, two Norway, and one each from Finland, France, Germany, Lithuania, Poland, and from multiple countries], three were from Japan, and one from multiple countries in North America and Europe.Thirty-nine were cohort studies, and five were nested case-control studies.Eight studies were of workers in specific industries and one was of atomic bomb survivors, the rest considering regional, national or international populations.As shown in Table 1, the studies varied in regard to various factors, including the start year, the length of follow-up,the ages and sexes considered, the number of lung cancer cases studied, and the extent of adjustment for potential confounding factors.
Meta-analyses for cigarette smoking: In total, data were entered on 138 RRs, with up to 10 per study.The initial meta-analyses for cigarette smoking involved 62 of the RRs, selected based on the preferences described in the methods section.As shown in Table 3 and Figure 3, the overall random-effects RRestimate was 12.14 (CI 10.30-14.30) based on RR estimates that were highly significantly (P< 0.001)heterogeneous.
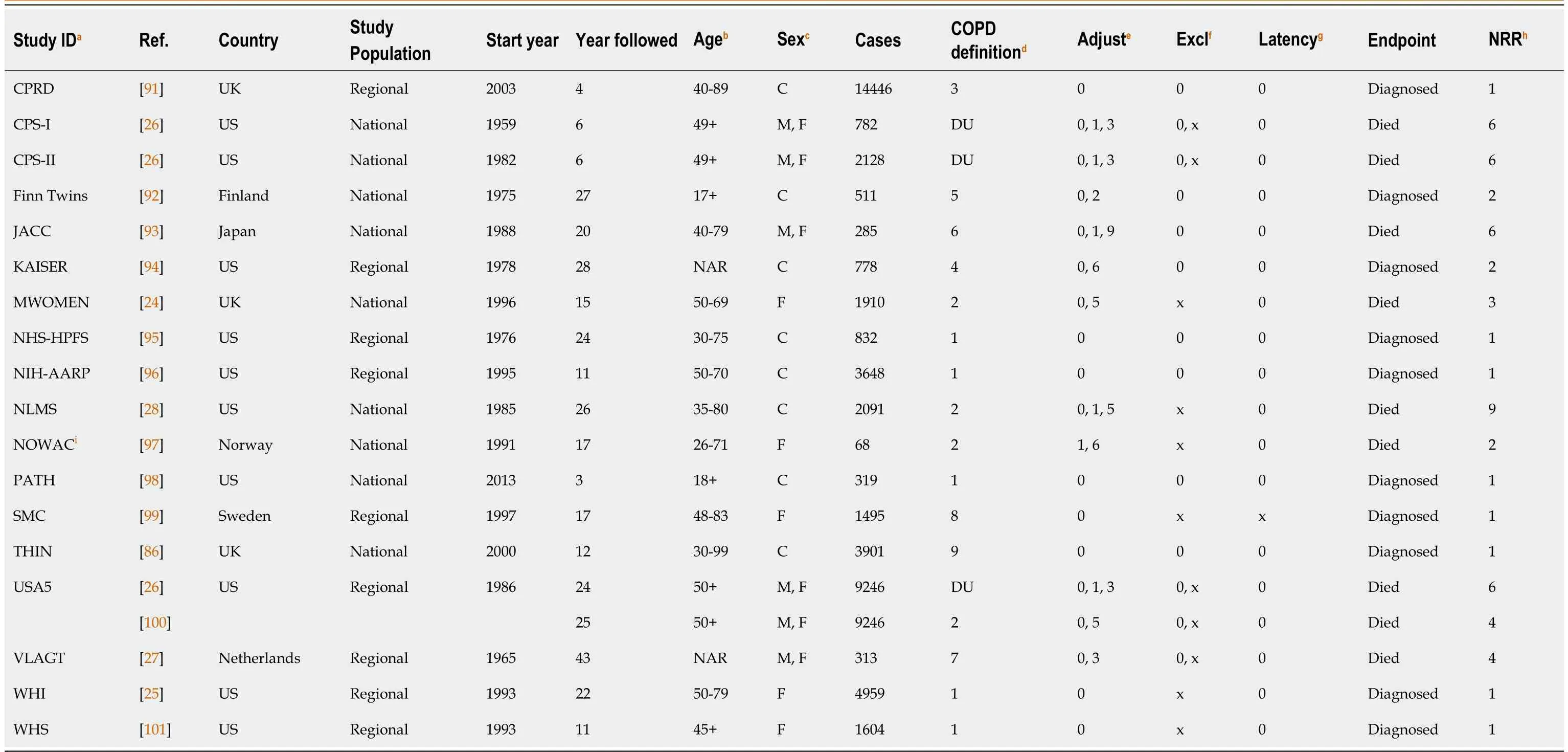
Table 2 Details of the 18 studies of chronic obstructive pulmonary disease
Table 3 also gives RRs by level of 12 different characteristics of the study or of the RR, with the most striking evidence of variation being for region, where the estimate for Japan (3.61, CI 2.87-4.55) was much lower than those for North America (15.15, CI 12.77-17.96), Europe (12.30, CI 9.77-15.49) or the single study conducted in North America and Europe (13.10, CI 9.91-17.32).This is also shown in Figure 3 (North America, Europe, Japan).There was also much weaker evidence that RRs were higher in studies starting more recently and in those with shorter follow-up periods, where the cigarette smokers may also have smoked cigars and/or pipes, where the endpoint was lung cancer death rather than diagnosis, and where more adjustment factors were taken account of.
When these analyses were restricted to studies in North America and Europe (see detailed results in Supplementary material 1), there was no evidence (P≥ 0.1) of variation by sex, region or any of the other factors considered in Table 3 except two.One was whether a latency rule was applied, with a significantly (P< 0.01) higher RR (19.52, CI 16.27-23.42) for studies excluding cases occurring shortly after baseline than the RR (13.29, CI 11.42-15.46) for studies considering all cases occurring after baseline.The other was study design, with a significantly (P< 0.05) higher RR (14.58, CI 12.71-16.74)based on cohort studies than the RR (10.41, CI 8.04-13.48) based on nested case-control studies.
Within-study comparisons for cigarette smoking: There were 18 otherwise comparable pairs of male and female RRs from the same study (see Supplementary material 1).The male RR exceeded the female RR in 13 pairs, and the random-effects estimate of the male/female ratio was significant (ratio 1.52, CI 1.20-1.92).
There were 36 pairs of unadjusted RR estimates and estimates adjusted for 2 or more covariates.Adjustment increased the RR in 24 of these pairs, and decreased the RR in 12.However, this difference was not significant (P> 0.1) and in most cases the effect of adjustment was quite small, with adjustment increasing the RR by a factor > 1.25 in six cases, and decreasing it by the same factor in six cases.
Within the studies considered, current cigarette smoking RRs also varied by four other characteristics:exclusive cigarette smoking; latency; years of follow-up; and endpoint.However, the data available were extremely limited, and some of the variation (and all of it for years of follow-up) related to different publications within the same study, where other characteristics varied as well.When attention was limited to results from the same publication within a study, there was no significant evidence of variation in risk for any of the other three characteristics.Thus, study THREEC[20] reported RRs that were virtually identical for exclusive cigarette smoking (32.58) and non-exclusive cigarette smoking(32.83), while study CHANCES[21] provided RRs for the endpoints died (13.10) and diagnosed (11.50)which clearly did not differ significantly.More data were available for latency, with five pairs of results,one for each sex from ATP[22] and from JP8[23], and one for females from Million Women Study(MWOMEN)[24].However (see the estimates in Supplementary material 1) the estimates taking and not taking latency into account were very similar.
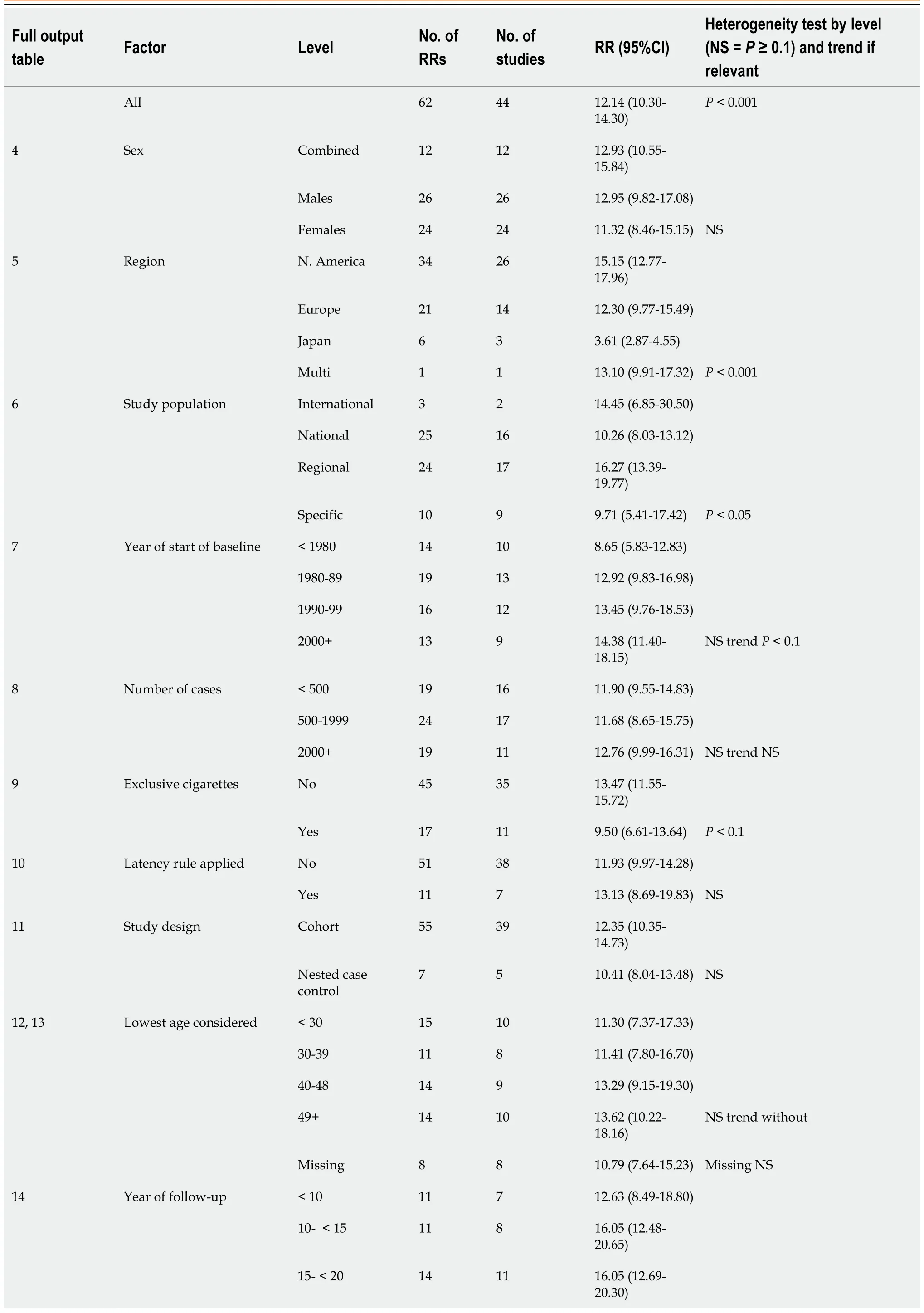
Table 3 Lung cancer and current vs never cigarette smoking – results from random effects meta-analyses
20- < 30 15 11 9.08 (6.26-13.15)30+11 8 9.57 (6.01-15.26)P < 0.05 trend P < 0.1 15 Endpoint Died 23 17 14.85 (11.99-18.38)Diagnosed 39 27 10.82 (8.61-13.60)P < 0.05 16 None 20 15 9.65 (7.13-13.05)Number of adjustment factors Age only 4 3 11.80 (5.24-26.56)More 38 28 13.68 (11.46-16.34)NS trend P < 0.1 RR: Relative risk; NS: Not significant.

Figure 1 Literature searches, lung cancer.

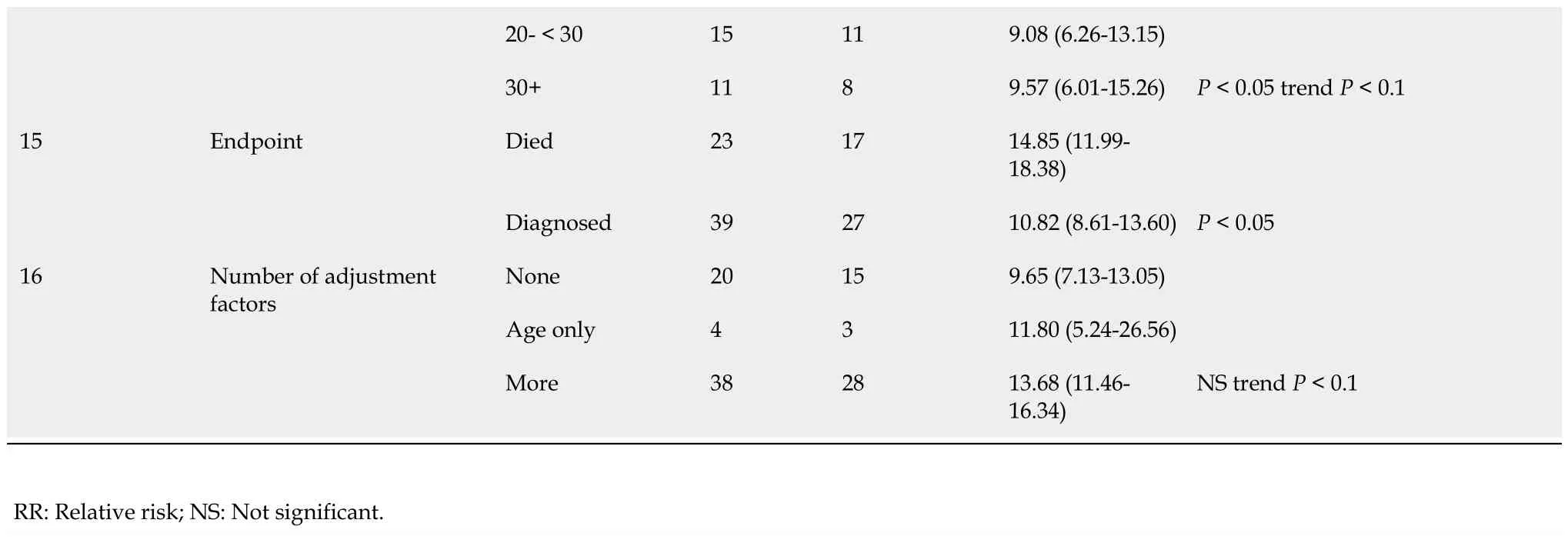
Table 4 Chronic obstructive pulmonary disease and current vs never cigarette smoking – results from random effects meta-analyses

Figure 2 Literature searches, chronic obstructive pulmonary disease.COPD: Chronic obstructive pulmonary disease.
COPD
Data available for cigarette smoking:Each of the 18 studies provided data for current cigarette smoking, with data coming from two publications for one of these studies.Of the 18 studies, 10 were from the US, seven from Europe (three UK, and one each from Finland, Netherlands, Norway, and Sweden), and one from Japan.All 18 studies were of cohort design.Nine studies were of national populations and nine of regional populations, with none of workers in specific industries.
As shown in Table 2, the studies varied in regard to several factors, including the start year, the length of follow-up, the ages and sexes considered, the number of COPD cases studied, the definition of COPD used, and the extent of adjustment for potential confounding factors.
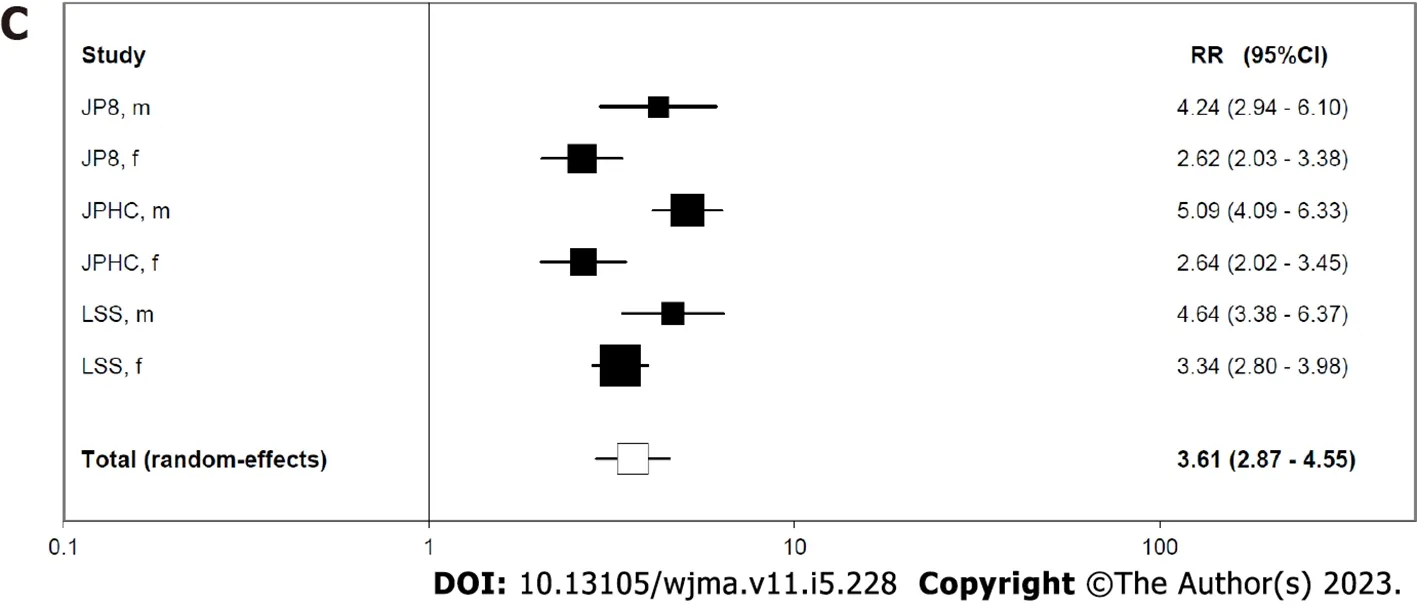
Meta-analyses for cigarette smoking:Data were entered on a total of 52 RRs, with up to 10 per study.The initial meta-analyses involved 23 of the RRs, selected based on the preferences described in the methods section.As shown in Table 4 and Figure 4, the overall random-effects RR estimate was 9.19 (CI 6.97-12.13) based on RR estimates that were highly significantly (P< 0.001) heterogeneous, the RRs varying from 3.21 (CI 2.96-3.47) in WHI[25] to 36.70 (CI 30.20-44.70) in MWOMEN[24].
Table 4 also gives RRs by level of 12 different characteristics of the study or of the RR.There was some evidence (0.05 Figure 3 Forest plot for lung cancer and current vs never cigarette smoking.A: North America; B: Europe; C: Japan. Figure 4 Forest plot for chronic obstructive pulmonary disease and current vs never cigarette smoking. Within-study comparisons for cigarette smoking:There were five otherwise comparable pairs of male and female RRs from the same study (see Supplementary material 2).The male RR was the higher in three pairs, and the female RR was the higher in two, and the random-effects estimate of the male/female ratio was not significant (ratio 1.08, CI 0.88-1.34). There were 15 pairs of unadjusted RR estimates and estimates adjusted for two or more covariates.Adjustment increased the RR in 13 of these, and decreased it in two (P< 0.01), emphasising the conclusion from the previous section.The increase was greater by a factor of 1.5 in 5 of the 14 increases,with a decrease by a similar factor in one case, the adjusted/unadjusted factor varying from 0.65 to 3.17. Except for in four studies (CPS-I[26], CPS-II[26], USA5[26], VLAGT[27]), where the female RR was taken to be for exclusive cigarette smoking but the male RR was not, the only other characteristic varying within study was latency.Here MWOMEN[24] gave similar adjusted RRs of 35.30 (CI 29.20-42.50) based on analyses involving the whole follow-up, and 36.70 (CI 30.20-44.70) based on analyses excluding occurrences in the first few years of follow-up. Lung cancer:The full output for cigar smoking is given in Supplementary material 3.The data are very limited, coming from one study in the US (NLMS[28]), one in the Netherlands (NLCS[29,30]) and one of multiple studies in Europe (EPIC[31,32]), with the RR estimate from NLCS based on far more lung cancer cases in current cigar smokers (520) than seen in NLMS (11) or EPIC (3).Only an unadjusted RR estimate was available from NLCS, while the other studies provided RRs by level of adjustment.All the RR estimates are in the range 2.68 to 4.71, with the combined random-effects estimate, based on the most adjusted data, being 2.73 (CI 2.36-3.15), with no evidence of heterogeneity (P> 0.1). The full output for pipe smoking is given in Supplementary material 4.Again, the data are very limited, coming from the same three studies as for cigar smoking (NLMS, NLCS and EPIC), plus one in Norway (THREEC[20]).The most precise RR estimate comes from NLCS.As for cigars, RR estimates by level of adjustment were available from each study except for NLCS.Based on the most adjusted data the overall random-effect RR estimate was 4.93 (CI 1.97-12.32), the wide confidence interval reflecting the highly significant heterogeneity (P< 0.001), with individual study most-adjusted RRs being over 10 for two studies (EPIC 13.30, THREEC 10.32) and under 3 for the other two (NLMS 1.51, NLCS 2.80). COPD:The data for pipe and cigar smoking, shown in Supplementary material 5, are very limited,coming from only one study, which was conducted in the US (NLMS[28]).This reported combined sex RRs for exclusive cigar smokingvsnever smoking of 2.21 (CI 0.89-5.47) adjusted for age only, and of 2.44(CI 0.98-6.05) after additional adjustment for sex, race/ethnicity, education and survey year.The corresponding estimates for exclusive pipe smoking were, respectively, 1.04 (CI 0.27-4.10) and 1.12 (CI 0.29-4.40). There were eleven studies, seven in the US and four in Europe, which provided comparable results for both lung cancer and COPD.For seven of the studies (CPS-II, Kaiser, NIH-AARP, NLMS, THIN,VLAGT and WHI) the RRs were higher for lung cancer than for COPD, while for two (MWOMEN and NOWAC) the RRs were lower.For USA5 the RRs were very similar in both sexes, being slightly higher for lung cancer for females and slightly higher for COPD for males.For CPS-I the RRs were clearly higher for lung cancer in males and slightly higher for COPD in females.(See Supplementary material 1 and 2 for the RRs).These within-study comparisons are consistent with the higher overall RR estimates for lung cancer than for COPD. Comparison with earlier reviews – cigarettes:Our conclusion that current cigarette smokers have a substantially increased risk of lung cancer is consistent with that of major bodies (e.g.[1,2]).Our overall random-effects RR estimate of 12.14 (CI 10.30-14.30) for currentvsnever cigarette smoking is not dissimilar from an estimate of 10.92 (CI 8.28-14.40) from a meta-analysis based on 34 cohort studies published in 2013[13] (though based on currentvsnon rather than currentvsnever cigarette smoking),and somewhat higher than estimates of 7.33 (CI 4.90-10.96) for males and 6.99 (CI 5.09-9.59) for females based on 99 cohort studies published by 2016[16] and of 8.43 (CI 7.63-9.31) based on our earlier metaanalysis, of studies published in the 20thcentury[4]. We also found much higher RR estimates for North America (15.15) and Europe (12.30) than for Japan(3.61).Strong evidence of regional variation in risk is also evident based on publications in the 20thcentury[4], where RRs for currentvsnever smoking of any product were 11.68 (CI 10.61-12.85) for North America, 7.53 (CI 5.40-10.50) for the UK, 8.68 (CI 7.14-10.54) for Scandinavia, 8.65 (CI 5.98-12.51) for other regions of Europe, 2.94 (CI 2.23-3.88) for China, 3.55 (CI 3.05-4.14) for Japan and 2.90 (CI 2.04-4.13)for other regions of Asia.Similar, relatively low, RRs have been reported based on meta-analyses conducted in Japan[6,15] or in the whole of Asia[7,17], while relatively high RRs for Europe and the US have been reported in recent meta-analyses or large studies[10,13,33,34].There is considerable heterogeneity between the estimates from different studies, with, for example, 11 of the 34 selected RR estimates for North America exceeding 20, and 7 less than 10.However, the fact that the highest of our six individual RR estimates for Japan was 5.09 emphasises the regional difference, with a very recent large study in China[35] having also reported similarly relatively low RRs for smoking. Our analyses show a somewhat higher RR in males than females, with the within-study comparison estimating the ratio as 1.52 (CI 1.20-1.92).A similar difference was also seen in our earlier meta-analyses[4] where the RRs were 9.16 (CI 8.00-10.49) for males and 6.76 (CI 5.65-8.08) for females.Other recent reviews or analyses of large studies have all also reported a higher RR in males, though with one exception, where the RRs from a pooled analysis of case-control studies were 23.6 (CI 20.4-27.2) for males and 7.8 (CI 6.8-9.0) for females[10], the RRs for the others[6,7,15,16] were at most 60% higher in males. Of the other factors studied in our latest analyses (see Table 2) some were not considered earlier.Of those that were, neither set of analyses showed any clear variation by study size, by study type, by whether the exposed group smoked exclusively cigarettes or not, or by the extent of adjustment for potential confounding factors.There was a tendency for RRs to be greater for studies starting later, more clearly seen in the earlier analyses, a difference which may partially explain why the RRs tend to be somewhat higher for the later than for the earlier analyses. Comparison with earlier reviews – cigars and pipes:Our combined RR of 2.73 (CI 2.36-3.15) for cigar smoking was based on estimates from only three studies.It is somewhat lower than the RR of 4.67 (CI 3.49-6.25) reported in our earlier review[4] based on 15 estimates, though there the individual study estimates showed marked heterogeneity (P< 0.001) with three RRs above 10 and four less than 4, the two having the greatest weight being the RRs of 3.30 (CI 2.68-4.06) and of 5.20 (CI 4.10-6.60) derived from the American Cancer Society CPS I and CPS II studies[36,37].It is also not dissimilar from estimates of 2.98 (CI 2.08-4.26) from a recent review of US studies[18], of 1.87 (CI 0.53-6.55) from a more recent US study[33,34] and of 2.73 (CI 2.06-3.60) from five US cohorts[14] based on evervsnever smoking. Our combined RR estimate of 4.93 (CI 1.97-12.32) for pipe smoking was based on estimates from only four studies which were markedly heterogeneous (P< 0.001).It is similar to that of 5.20 (CI 3.50-7.73)reported earlier[4] based on 12 estimates for current pipe only smoking.These 12 estimates also showed marked heterogeneity (P< 0.001), with three RRs above 10 and three less than 4, the two having the greatest weight being that of 5.85 (CI 4.52-7.58) derived from the West European case-control study[38]and of 2.14 (CI 1.46-3.13) from the US veterans study[39].These estimates are not dissimilar from the more recent estimates of 5.00 (CI 4.16-6.01) from the US CPS II study[40] or of 3.18 (CI 1.35-7.52) from an analysis of five US cohorts[14] based on evervsnever smoking. The available data were too limited to study sources of variation in the results for cigar and pipe smoking in the same way that we addressed them for cigarette smoking. Comparison of risks by tobacco product:Our results suggested that RRs for current cigar smoking and for current pipe smoking are substantially lower than for current cigarette smoking, though the individual study results for pipe smoking are rather heterogeneous.This conclusion is consistent with the results of our previous review[4].Although the risks we found for cigar and pipe smoking are lower than for cigarette smoking we agree with McCormacket al[31], 2010, who concluded that smoking of these products is “not a safe alternative to cigarette smoking” and suggested that “the lower cancer risk of pipe and cigar smokers as compared to cigarette smokers is explained by lesser degree inhalation and lower smoking intensity”.Christensenet al[28], 2018, considered that the lower risks for pipe and cigar smoking are probably because “cigar and pipe smokers use these products less frequently per day than cigarette users.” Exceptionally, based on a study in Norway, Tverdalet al[20], 2011 concluded that “pipe smoking is not safer than cigarette smoking” but the overall evidence reviewed seems inconsistent with this conclusion.It should be noted that all four of the RRs for pipe smoking given in Supplementary material 3 are lower than the corresponding estimates for cigarette smoking from the same study given in Supplementary material 1 (EPIC 13.30vs32.00, THREEC 10.32vs16.78, NLCS 2.80vs7.57, NLMS 1.51vs11.82), the results from THREEC being those reported by Tverdal and Bjartveit, 2011[20]. Comparison with earlier reviews – cigarettes:We found clear evidence that current cigarette smokers,compared to never smokers, have a substantially increased risk of COPD, with an overall RR estimate of 9.19 (CI 6.97-12.13).As for lung cancer, this conclusion of a strong relationship is consistent with that of major bodies (e.g.[1,2]).Some earlier reviews have given rather lower RR estimates; 4.01 (CI 3.18-5.05)based on cohort studies published by 2013[13] but for currentvsnon smoking, 3.57 (CI 2.72-4.70) based on studies in Japan published by 2016[15], 3.51 (CI 3.08-3.99) based on studies published by 2006[5] and 3.26 (2.67-3.98) based on studies published by 2014[12]. However, there was considerable heterogeneity between the estimates from the different studies,with the RR estimates varying from 3.21 to 36.70.We found no significant (P< 0.05) variation in RR by sex or by region, though the direction of effect – higher RRs in males and in North American and European studies – was the same as that seen more clearly in our earlier review based on 133 studies published up to 2006[5].Our analyses also found some marginally significant (0.05 Comparison with earlier reviews – pipes and cigars:We only found one study published in 2010-2020,the NLMS study in the US[28], which reported RRs for current cigar smoking and for current pipe smoking, predominantly occurring in males.The adjusted RRs from this study, 2.44 (CI 0.98-6.05) for current cigar smoking, and 1.12 (CI 0.29-4.40) for current pipe smoking, are imprecise, but seem not inconsistent with earlier published evidence. For current cigar smoking, a recent review of evidence from the US[18] reported a combined estimate of 1.44 (CI 1.16-1.77) based on four studies, while another review[11], which did not provide metaanalysis results, reported estimates for males from two older studies, 1.30 (CI 0.00-7.45) from the Swedish Census study[41] and 3.70 (CI 1.10-12.0) from the Copenhagen City study[42]. Current pipe smoking estimates from the US included that of 2.36 from the Dorn study[43] (where we derived an approximate CI of 1.12-4.96 from the data provided) and of 2.98 (CI 2.17-4.11) from the CPS II study[40], while estimates from the Swedish study[41] and Copenhagen City study[42] were,respectively, 3.60 (with a derived approximate CI of 2.51-5.14) and 2.40 (CI 0.60-9.60). Comparison of risks by tobacco product:While the estimates cited above do not allow reliable conclusions as to whether, in the US or Europe, the COPD RR differs between current cigar smokers and current pipe smokers, it is clear that the risks for both products are substantially less than those for current cigarette smokers, where the meta-analysis results shown in Table 4 are 8.91 (CI 5.73-13.84) for the US and 10.63 (CI 6.93-12.24) for Europe. In many ways, the results for the two diseases are quite similar.Thus, our meta-analysis RR estimates for cigarette smoking, 12.14 (CI 10.30-14.30) for lung cancer and 9.19 (CI 6.97-12.13) for COPD, both show a very strong relationship, and indeed every single RR estimate for both diseases shown in the forest plots (Figures 3 and 4) is statistically significantly increased.For both diseases, the meta-analysis estimate for cigarette smoking is also substantially greater than the corresponding estimates for cigar smoking, 2.73 (CI 2.36-3.15) for lung cancer and 2.44 (CI 0.98-6.05) for COPD, and for pipe smoking, 4.93(CI 1.97-12.32) for lung cancer and 1.12 (CI 0.29-4.40) for COPD, though based on much more limited data.For both diseases, the RR estimates for cigarette smoking are also greater based on studies in North America and Europe than on studies in Japan, most clearly evident for lung cancer.They are also quite similar for males and females, and there is no strong evidence of variation by the other factors studied. While the evidence that cigarette smoking increases the risk of lung cancer and of COPD is absolutely clear, the RR estimates for both diseases show substantial between-study heterogeneity.There are multiple reasons for this, many inter-related, and only some of which we have investigated.Thus,populations in different regions and studies may vary in age and race which may affect precisely what is smoked, the daily amount smoked and the duration of exposure.Males and females may also vary by amount smoked.Study populations may also vary in the extent of exposure to other lung cancer and COPD risk factors, and the extent to which adjustment for this is made in the RR estimation.Variation between studies in the exact definition of the exposed and the unexposed groups is also an issue, only some studies considering exclusive exposure or restricting attention to smoking of some minimum lifetime number of cigarettes.Misclassification of smoking is also an issue, with some of those reporting never having smoked actually being current or former smokers, the studies considered generally not using nicotine biomarkers such as cotinine to check self-reports of smoking.Cohort studies also vary in the extent to which they monitor changes in an individual’s smoking over time, some studies only classifying subjects by baseline status, when current smokers may have subsequently quit or switched to other products, including e-cigarettes or heat-not-burn products, and some baseline never smokers may have later taken up smoking.Also, the precise definition of disease may vary between studies, as may changes over time in how lung cancer and COPD are treated, so affecting survival, possibly differently for current and never smokers.Some of these factors may also help to explain variations between our results and those reported in other studies or meta-analyses. While limited to studies in North America, Europe and Japan, our work gives good insight into the magnitude of the RR for currentvsnever use of cigarettes for both lung cancer and COPD, as was the main objective of our meta-analysis.Although heterogeneity of the RR estimates from the individual studies limits the precision of the overall estimates, we have attempted to investigate a range of individual factors that contribute to the heterogeneity.However, it would have been possible to carry out multivariate analyses investigating the extent to which RR estimates varied according to the list of factors studied.For cigar and for pipe smoking, our estimates for both diseases are also limited by the small number of studies that investigated these products.Some limitations are caused by the unfortunate lack of clear definition of the product used in some of the source publications, with the term“smoking” used variously for any tobacco product use, cigarette smoking or exclusive cigarette smoking.While we have attempted to determine the meaning as best we can, some errors may remain. Other limitations arose as the objectives of our study were less than those of our earlier meta-analyses of lung cancer studies published in the 20thcentury[4], or COPD studies published up to 2006[5].Thus,our investigations did not consider aspects of tobacco smoking, including amount smoked, duration of smoking, age of starting to smoke, the effect of quitting, and risks associated with the use of multiple products.Nor did it consider the role of e-cigarettes which were introduced towards the end of the follow-up period in some of the cohort studies.Nor did it consider results for individual histological types of lung cancer or subgroupings of COPD or for individual types of cigarettes, cigars and pipes.Nor did we attempt to quantify how misclassification of exposure, disease, or confounding variables might have biased the RR estimates. Results from 44 studies published in 2010-2020 confirm the strong association of current cigarette smoking with lung cancer risk, with RR estimates markedly higher for North American and European studies than for studies in Japan, and somewhat higher in males than in females, in cohort than in nested case-control studies, and in studies that excluded cases occurring shortly after baseline.Only limited evidence on lung cancer is available for cigar and pipe smoking, all from North America and Europe.While this indicates lower lung cancer risks than for cigarette smoking, the results for pipe smoking are rather heterogeneous. Results from 18 studies published over the same period also confirm a strong association of current cigarette smoking with COPD risk, though the RR estimates, which are somewhat lower than for lung cancer, do not vary significantly by region or sex.While the COPD RR estimates are markedly heterogeneous no study or RR characteristic was found that explains a major part of this variation.Only one study, in the US, provided evidence on COPD for current cigar and current pipe smoking, and while this suggested lower risks than for cigarette smoking, its results are uncertain. It is clear that smoking, particularly of cigarettes, markedly increases the risks of developing lung cancer and COPD.To most effectively reduce these risks, smokers should quit smoking[44,45], though alternative nicotine-containing products may substantially reduce these risks.This is clearest for Swedish snus[46-48] where considerable epidemiological evidence is available.However, it also may be true for much newer products, such as e-cigarettes and heated tobacco products which have toxicant levels that are lower by an average of > 90% compared with cigarette smoke[49].An earlier expert opinion[50] also considered that e-cigarettes cause about 5% of the harm of cigarettes, and less than the harm caused by cigar or pipe smoking. Consistent with evidence from earlier studies, risks for cigar and pipe smoking are much less than for cigarette smoking, both for lung cancer and COPD.Risk of lung cancer from cigarette smoking is much less in Japan than in the US or Europe. Smoking significantly increases the risks of developing lung cancer and COPD, with risks highest for cigarette smoking.To most effectively reduce these risks, smokers should quit, though evidence suggests that using alternative nicotine-containing products, such as snus, e-cigarettes and heated tobacco products should also substantially reduce these risks. We also thank Yvonne Cooper for typing the various drafts of the paper and obtaining the relevant references. Author contributions:Lee PN planned the study; Literature searches were carried out by Coombs KJ and by Lee PN;Statistical analyses were carried out by Hamling JS and checked by Lee PN; Lee PN drafted the text, which was checked by Coombs KJ and Hamling JS. Conflict-of-interest statement:The authors have carried out consultancy work for many tobacco organizations. PRISMA 2009 Checklist statement:The authors have read the PRISMA 2009 Checklist, and the manuscript was prepared and revised according to the PRISMA 2009 Checklist. Open-Access:This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BYNC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial.See: https://creativecommons.org/Licenses/by-nc/4.0/ Country/Territory of origin:United Kingdom ORCID number:Peter Nicholas Lee 0000-0002-8244-1904; Katharine J Coombs 0000-0003-0093-7162; Jan S Hamling 0000-0001-7788-4738. S-Editor:Liu JH L-Editor:Webster JR P-Editor:Liu JH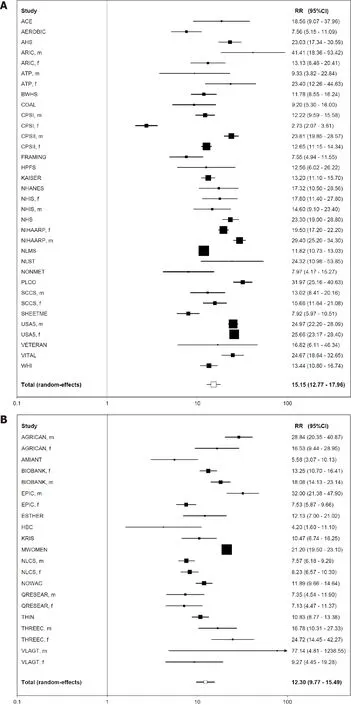

Cigar and pipe smoking results
Comparison within study of current cigarette smoking RRs for lung cancer and COPD
DISCUSSION
Lung cancer
COPD
Comparing risks by tobacco product - similarity of results for lung cancer and COPD
General considerations
Limitations of our work
CONCLUSION
ARTICLE HIGHLIGHTS


Research conclusions
Research perspectives
ACKNOWLEDGEMENTS
FOOTNOTES
 World Journal of Meta-Analysis2023年5期
World Journal of Meta-Analysis2023年5期
