Retinal thickness and fundus blood flow density changes in chest pain subjects with dyslipidemia
Jin Wang, Yu-Cen Wang, Pei Zhang,3, Xin Wang, Rong-Rong Zong, Jing Jiang, Yu Zhang,Yi-Wen Qian, Qing-Jian Li, Zhi-Liang Wang
1Department of Cardiology, Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 200010,China
2Department of Ophthalmology, Huashan Hospital, Fudan University, Shanghai 200040, China
3Department of Ophthalmology, Shanghai Gonghui Hospital,Shanghai 200040, China
4Fujian Provincial Key Laboratory of Ophthalmology and Visual Science; Fujian Engineering and Research Center of Eye Regenerative Medicine; Eye Institute of Xiamen University; Xiamen University School of Medicine, Xiamen 361005, Fujian Province, China
Abstract
● KEYWORDS: blood flow density; retinal thickness;optical coherence tomography angiography; dyslipidemia;serum lipid
INTRODUCTION
Dyslipidemia is defined as a functional disease resulting in increased or decreased levels of lipoproteins which included total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), and high-density lipoprotein cholesterol (HDL-C)[1].In the past 30y, the prevalence of dyslipidemia has increased significantly,especially in China.By 2016, the overall prevalence of dyslipidemia in Chinese adults is as high as 40.4%[2].Current studies have confirmed that being overweight or obese was a major risk factor for all forms of dyslipidemia.Blood lipid levels are known to vary depending on race, sex, age, smoking,dietary habit[3].In addition, chronic non-communicable diseases such as hypertension and hyperglycemia can also elevate the risk of dyslipidemia[4].The increased atherosclerotic cardiovascular disease risk is the most commonly associated clinical consequence of dyslipidemia[5-6].Chest pain is often the herald of cardiovascular disease as a common presenting symptom.For patients with chest pain, clinical assessment should be performed to confirm or exclude the diagnosis of cardiovascular disease.Globally in 2019, 3.78 million of 8.54 million (44.3%) deaths from ischemic heart disease were attributable to high LDL-C levels, and 0.61 million of 2.73 million (22.4%) deaths from ischemic stroke were attributable to high LDL-C levels[7].Additionally, there are other clinical consequences including hypertriglyceridemiaassociated pancreatitis, hepatosteatosis, and fat-soluble vitamin deficiencies[8].Moreover, dyslipidemia also acts on microcirculation, which can have a detrimental effect on the eyes.Αccording to existing studies, dyslipidemia is identified as an independent risk for retinal diseases.Dyslipidemia states potentiated the deleterious effects of diabetes on retinal neurons, and high LDL-C is a significant risk factor for diabetic macular edema and retinal hard exudates[9-10].Elevated levels of HDL-C are associated with an increased risk for advanced age-related macular degeneration in European and Asian populations[11].
The retinal vasculatures are responsible for nourishing the inner retinal layers, while the choriocapillaris provides nutrients and oxygen to the retinal pigment epithelium (RPE)and outer retinal layers[12].The neural tissue of the retina has the highest oxygen consumption per volume in the entire body and the choroid has a correspondingly high rate of blood flow[13].This makes the retina and choroid particularly susceptible to systemic diseases, such as coronary artery disease (CAD), hypertension, diabetes, and progressive neurodegenerative disease like Alzheimer’s type dementia[14].Due to the special structure of the eyeballs, the circulatory system of the retina can be dynamically observed directly in the living body.As a recently developed non-invasive diagnostic imaging technology, optical coherence tomography angiography (OCTA) employs motion contrast extracted from high-speed images to produce depth-resolved, highresolution images of retinal and choroidal vasculature, and it is a highly sensitive tool with good repeatability[15], to evaluate and quantify vascular density or blood flow at different fundus anatomical layers without dye injection[16-17].OCTA of the retina and choroid can make rapid evaluation on various indicators which may be helpful in the diagnosis of systemic diseases.
To our knowledge, there have been rare studies in the field about the correlation between dyslipidemia and the fundus blood flow density or retinal thickness.Based on the abovementioned facts, the purpose of this study was to analyze changes in fundus blood flow density and retinal thickness between chest pain subjects with dyslipidemia and the controls.
SUBJECTS AND METHODS
Ethical ApprovalIn accordance with Helsinki Declaration principles, this cross-sectional observational research was performed at Huashan Hospital affiliated with Fudan University between September 2021 and January 2022.It has been approved by the Institutional Review Board of Huashan Hospital (No.KY2016-274).Written informed consent was obtained from all subjects after a detailed explanation of the study.
Study PopulationBasic information was collected including gender, age, and clinical characteristics from outpatients with chest pain as the main symptom.All participants accepted a comprehensive ophthalmologic examination and a laboratory examination.Only the left eye of the participant was included for analysis.
Inclusion CriteriaThe inclusion criteria included: 1)presenting to the clinic for the first time with the symptom of chest pain; 2) ability to move autonomously and cooperate with long-time OCTA exam; 3) best-corrected visual acuity>20/50 Snellen; 4) spherical equivalent refraction between-4.00 and +4.00 D; 5) axial length <26 mm; 6) without severe cataract that affect OCTΑ image quality; 7) without a history of retinal pathology, such as epiretinal membrane, diabetic retinopathy, or retinoschisis; 8) no history of lipid-lowering medication use, to avoid the influence of drugs.
Blood Lipids TestingBlood samples were collected from the antecubital vein during 7 to 8a.m.after 12h of fasting.Serum TG, TC, HDL-C, and LDL-C were determined as the main indicators of clinical blood lipids.Dyslipidemia usually refers to increases in TC, TG, or both levels in serum, which is generally called hyperlipidemia.In fact, dyslipidemia also extensively refers to various blood lipid abnormalities,including HDL-C hypolipidemia.In this study, we defined the dyslipidemia group as TC≥6.2 mmol/L, LDL-C≥4.1 mmol/L,HDL-C<1.0 mmol/L, or TG≥2.3 mmol/L, based on the Chinese guidelines for the management of dyslipidemia in adults[18].A control group of age- and sex-matched participants without dyslipidemia was included in the study.
Optical Coherence Tomography AngiographyOCTA images were obtained using the OCT-HS100 (Canon, Tokyo,Japan).All of the images were captured individually by the same examiner in the same position.The OCT angiogram area selected for this study was a 6 mm×6 mm scan [232 A-scan(H) ×232 B-scan] for examination of the macular area and the optic nerve area.Signal strength was portrayed on a scale of 1 to 10 and images with a signal strength <5 were excluded from the study.The measurement area of the scan was divided into five subfields composed of a 1 mm center and four quadrant sectors (superior, inferior, nasal, and temporal) for analysis.These zones were partitioned automatically by the Canon OCT-HS100 Software (Version 4.5.1), then artificially adjusted according to the actual situation of the picture by the same examiner.And for vessel density, the images were automatically segments into four layers: superficial capillary plexus, deep capillary plexus, choriocapillaris, and radial peripapillary capillaries (RPC) layer, then fitted the designated margins and measured the vessel density.All the images have been processed after AI denoising by the built-in software.
Statistical AnalysisStatistics were calculated using SPSS software (IBM SPSS, Version 26, IBM Corporation, IL, USA).Categorical data were presented by frequencies (percentages)and continuous data by mean±standard deviation (SD).Chisquare tests were used for comparisons of categorical data between the two groups.The paired Student’st-test was used for continuous data.P<0.05 was considered as statistically significant.
RESULTS
A total of 87 eligible participants with dyslipidemia and 87 age- and gender-matched controls without dyslipidemia were recruited in this study.The demographic and clinical information of the two groups was listed in Table 1.No significant difference was observed in the distribution of smoking, drinking, hypertension, or diabetes mellitus between the dyslipidemia group and the control group.For the blood lipids indicators, TG and HDL-C showed significant differences between the two groups.While differences of TC and LDL-C had no statistical significance.
The retinal thickness of the dyslipidemia subjects in all regions was thinner than that of the controls.But only the differences of the inferior and temporal regions were statistically significant, both inner and outer layers (Table 2).
In terms of blood flow density in macula, there was a decreasing trend of all regions (both retinal and choroidal layer) in the dyslipidemia group compared with the control group.While no statistical difference was shown except the inferior and temporal regions in superficial and deep layers,central and nasal regions in superficial layer, and temporal region in choroidal layer (Table 3).
Similarly, there was also a decreasing trend in blood flow density of optic nerve head (ONH) in the dyslipidemia group.The differences were statistically significant shown in superficial and deep layers, except the central and nasal regions in deep layer.For choroidal blood flow density, the differences of only the central and temporal regions were statistically significant.When comparing the blood flow density in RPC between the dyslipidemia group and the control group, all five regions showed a significant reduction (Table 4).
DISCUSSION
Dyslipidemia is an important component of the metabolic syndrome, and an identified factor of premature vessel atherosclerosis.While the consequences of dyslipidemia are multiorgan damage including liver, pancreas, skin, and sometimes ocular changes.This study was designed to investigate changes in the retina and choroid between subjects with and without dyslipidemia.According to our results, there was a decrease in retinal thickness and blood flow density,especially in the inferior and temporal regions when comparing the dyslipidemia group with the control group, which indicatedabnormal serum lipid levels have a negative effort on the retinal.
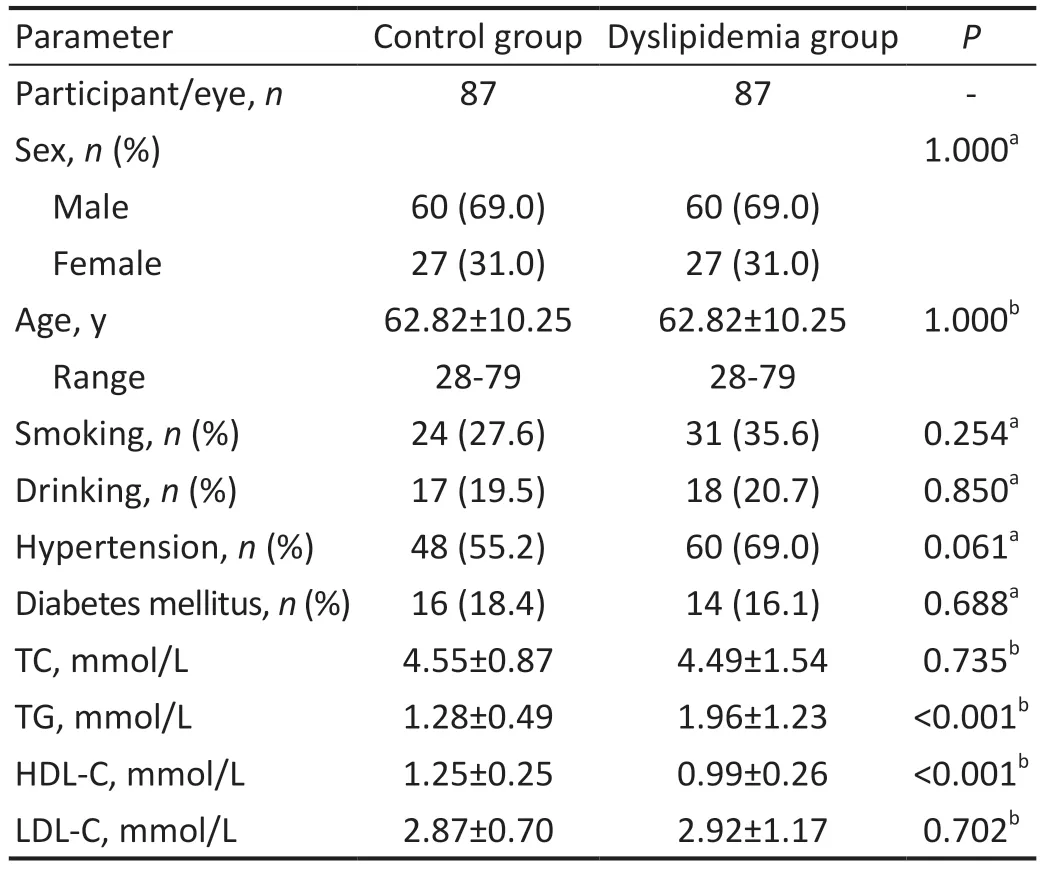
Table 1 Demographic and clinical characteristics
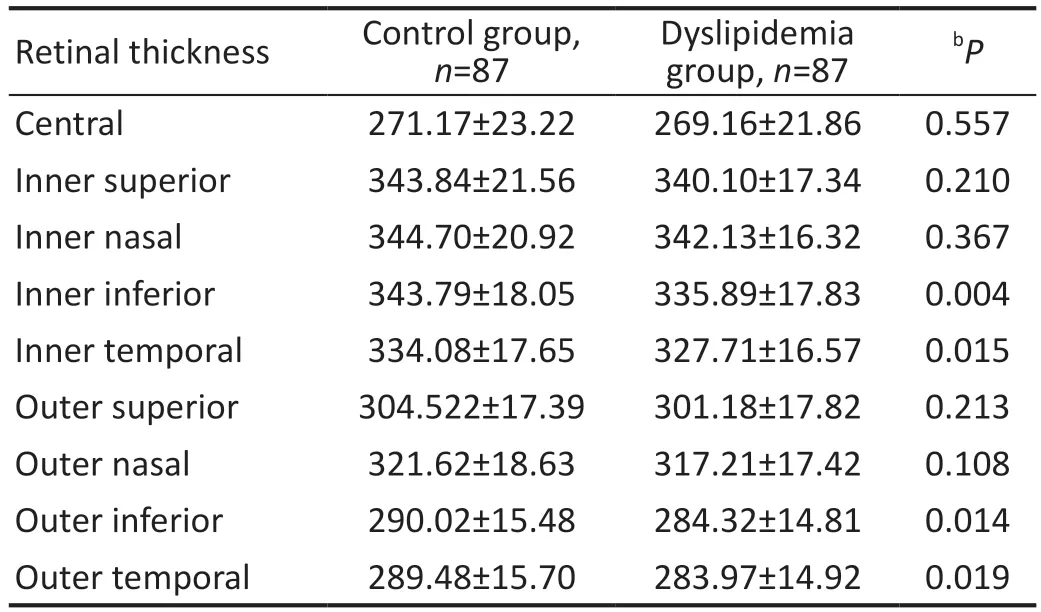
Table 2 Retinal thickness mean±SD, µm
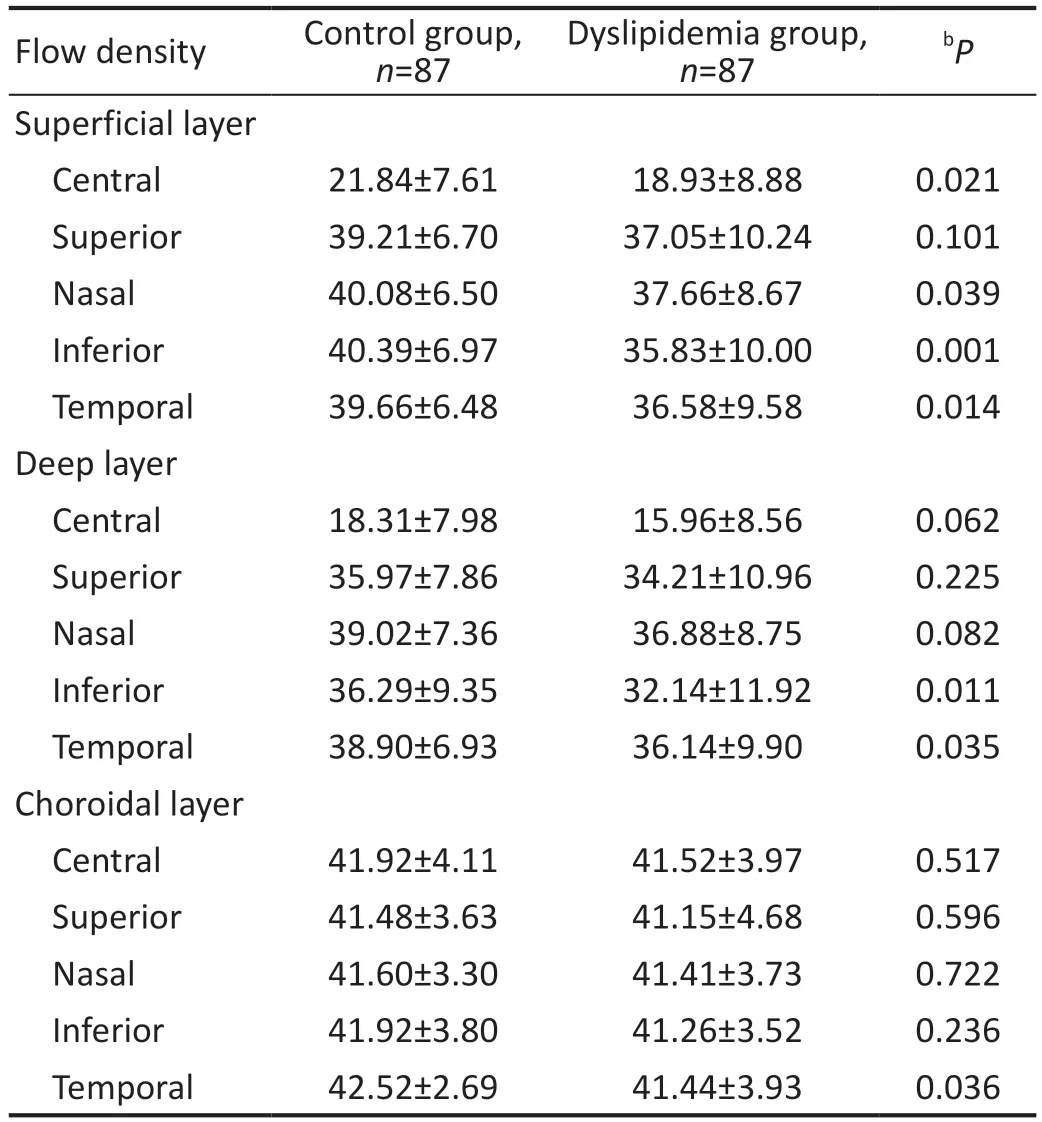
Table 3 Blood flow density in macula mean±SD, %
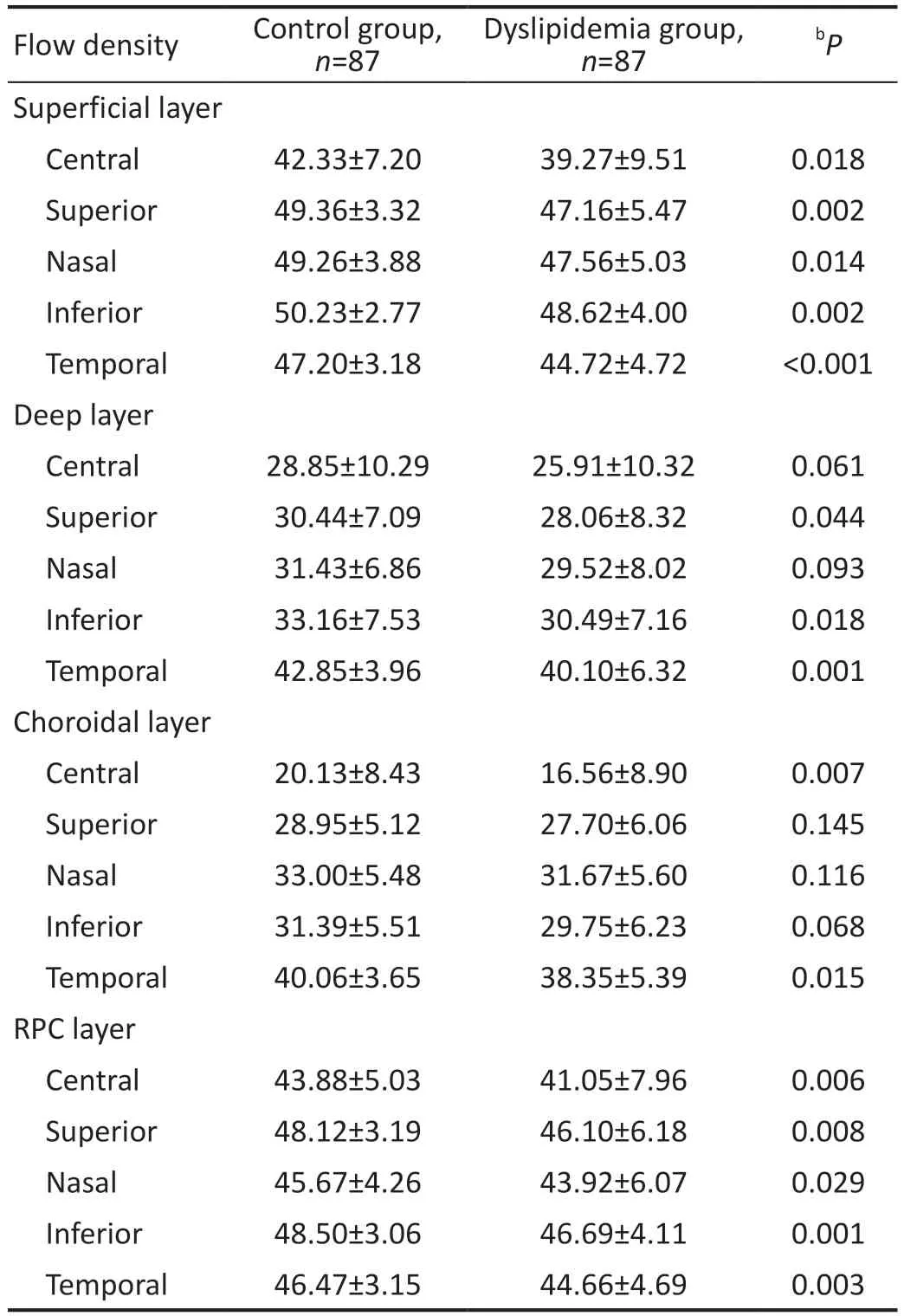
Table 4 Blood flow density in optic nerve head mean±SD, %
Lipid metabolism disorders affect retinal function to some extent.Montgomeryet al[19]measured visual and retinal function in a chemically induced dyslipidemia mouse model.They noticed the decline of the retina by flash electroretinography (fERG), but did not observe a significant difference in visual function.Zhanget al[20]measured the potential changes of the retina by fERG and found that all fERG amplitude parameters were significantly lower in the dyslipidemia group compared with the control group, which indicated that the rod and cone systems were impaired in patients with dyslipidemia.Lipemia retinalis is a rare condition caused by primary or secondary hyperlipidemia, and the clinical characteristics include the milky discoloration of the retinal vessels and salmon-colored fundus[21].A few cases showed visual deficits, and the vision and retinal changes would recover after lipid-lowering therapy[22].
Statins are commonly used in lipid-lowering therapy.Statin has been proven to slow down or may even partially reverse atherosclerosis.Moreover, they can also improve peripheral endothelial function and decrease carotid intima-media thickness[23].A connection between statin administration and the improvement of capillary rarefaction and microcirculation has been found in a previous study[24], and Istvánet al[25]found a beneficial effect of statin use on retinal blood flow.Liet al[26]found a significant effect of rosuvastatin on retinal microvasculature, including artery-vein ratio increase, venular constriction, and arteriolar dilation for patients with a low-tomoderate risk of CAD after 6-12mo of rosuvastatin treatment.Obesity is known to be associated with microvascular dysfunction that culminates in reduced vasodilator reactivity to flow[27].Laiginhaset al[28]reported a retinal thickening after bariatric surgery, which indicated that the thickening of the retina might represent an increased and improved perfusion of the retina triggered by bariatric surgery.
An animal experiment showed that the dyslipidemia mice induced by a high-fat diet andApoegene deletion had thinner retinal thickness than the wild-type mice[29].They found the changes only in the peripheral retina, and ascribed it to the rich blood supply, good nutrients, and lack of aggregation of inflammatory cytokines in the central area.In our study, we found thinner retina of the inferior and temporal regions in subjects with dyslipidemia, while in more clinical studies there seemed no statistically significant relationship between blood lipid levels and macular thickness[30-31].
In general, changes of the state of systemic blood vessels also affect the ocular blood flow.Then few studies have focused solely on lipid levels and retinal blood flow density yet.The pathophysiologic model for the role of lipids in retinopathy is commonly assumed to reflect the pathophysiology of atherosclerosis[32].Xiaoet al[33]have observed an association between elevated serum lipids and narrower arterioles,independent of body mass index (BMI) and blood pressure.Narrowing of retinal arterioles might represent the constriction of systemic arterial vessels, which could cause an increase in peripheral vascular resistance, and eventually lead to several systemic conditions.Similarly, dyslipidemia also plays a synergistic role in diabetic retinopathy.Davoudiet al[34]found that the presence of macular hyperreflective foci, which is the sign of intraretinal hard exudates, in patients with type 2 diabetes is associated with higher TC and LDL-C, and they also pointed out that the outer plexiform layer was most commonly involved.In our study, we found a decrease of blood flow density in subjects with dyslipidemia.
The choroid is a vascular structure between the retina and the sclera.It supplies the RPE and outer retina.In view of the fact that the choroid has the highest blood flow of the body per unit of surface area, it may be easily affected by vascular risk factors like other organs[35-36].We observe a significant difference of the choroidal blood flow density in both macula and optic disk between the two groups.We speculated that this was also related to the anatomical features that the choroidal blood flow at the macular area could fluctuate according to changes in blood pressure[37].
The vascular supply of the ONH is complex.It has been reported that the superficial layers of the ONH are supplied by the central retinal artery while the deeper prelaminar regions by the posterior ciliary arteries which branch off the circle of Zinn-Haller[38].Glaucoma is a chronic optic neuropathy characterized by progressive loss of retinal ganglion cells[39].The damage to nerve cells is hypothetically localized in the ONH in glaucoma, and thus we can assume that the change of blood flow density in the optic disc reflects the degree of optic nerve injury.We observed a significant difference of the blood flow density in the superficial layer of ONH, which might suggest that the vessel density in there is more susceptible to abnormal lipid levels.
RPC comprises a unique vascular plexus of capillary bed within the retinal nerve fiber layer (RNFL) around ONH,that is predominantly found in the posterior pole of primates with a typical macula.It has been proved that during the course of glaucoma, the vessels in RPC layer are prone to be pathologically damaged[40-41].Previous studies have shown that the vascular density of RPC layer in glaucoma patients is significantly lower than that in the normal, and the reduction is significantly correlated with the thinning of RNFL thickness[42].And in our current study, the blood flow density in all five regions of RPC layer showed a statistically significant reduction between the dyslipidemia group and the control group.This may indicate that changes of RPC layer in the impaired blood flow state will be more sensitive.
Chest pain, caused by transient myocardial ischemia, is the most common manifestation of CAD.Chest pain has been found to have the greatest sensitivity for CAD in both the emergency department and outpatient settings[43-44].Even so, only about 10% of patients with chest pain are actually diagnosed[45-46].To avoid potentially life-threatening events, such as myocardial infarction, most patients are required to undergo further tests,including invasive coronary angiography.However, previous studies have shown that a large proportion of patients are found not to have coronary stenosis after coronary angiography[47],which increases costs and utilizes the time of both patients and medical personnel to some extent.We found decreased retinal thickness and blood flow density in patients with dyslipidemia in our study, suggesting that dyslipidemia is not only a risk factor for CAD in patients with chest pain, but also a possible risk factor for fundus oculi disease.Moreover, we speculate that these changes may be related to the degree of coronary artery stenosis.Therefore, OCTA, as a rapid non-invasive examination, is necessary for patients with chest pain who have not had coronary angiography.
This study had several limitations.First, the participants recruited were mostly the elderly with underlying diseases,which was difficult to match exactly.Second, since the research was a cross-sectional study, cause and effect relationship could not be established.We have demonstrated to some extent the quantifiable effect of dyslipidemia on the retina, which can be further validated in a large healthy population in the future.Third, coronary angiography had not been performed in these enrolled patients, and that will be further studied in our future projects.
Retinal and choroidal vessels are considered as a favorable surrogate for the systemic microvascular system due to the similarities between cerebral and myocardial microvasculature anatomically and physiologically.In this study based on patients with chest pain, there was a decrease in retinal thickness and fundus blood flow density in subjects with dyslipidemia.This may further validate the association between abnormal lipid metabolism and fundus microcirculation alterations.
ACKNOWLEDGEMENTS
Foundation:Supported by the Science and Technology Commission of Shanghai Municipality (No.20Y11910800).
Conflicts of Interest:Wang J,None;Wang YC,None;Zhang P,None;Wang X,None;Zong RR,None;Jiang J,None;Zhang Y,None;Qian YW,None;Li QJ,None;Wang ZL,None.
 International Journal of Ophthalmology2023年11期
International Journal of Ophthalmology2023年11期
- International Journal of Ophthalmology的其它文章
- Research progress on animal models of corneal epithelial-stromal injury
- Role of lymphotoxin alpha as a new molecular biomarker in revolutionizing tear diagnostic testing for dry eye disease
- Therapeutic potential of iron chelators in retinal vascular diseases
- Axial length and anterior chamber indices in elderly population: Tehran Geriatric Eye Study
- Development of a new 17-item Asthenopia Survey Questionnaire using Rasch analysis
- Analysis of independent risk factors for acute acquired comitant esotropia
