Prognostic and diagnostic scoring models in acute alcohol-associated hepatitis: A review comparing the performance of different scoring systems
Jad Mitri, Mohammad Almeqdadi, Raffi Karagozian
Abstract
Key Words: Alcohol-associated hepatitis; Prognostic scores; Mortality; Maddrey discriminant function; Model for end stage liver disease; Acute kidney injury
INTRODUCTION
Alcohol consumption could result in numerous liver diseases, the most severe one being alcohol-associated hepatitis (AAH).AAH, otherwise known as alcoholic hepatitis, is clinically characterized by rapidly progressing jaundice, malaise, tender hepatomegaly, and discreet systemic inflammatory response syndrome (SIRS) features[1].While the burden of this disease is well known, little improvement in survival has been noted over the years[2].Therefore, research and development for AAH are desperately needed to improve patients’ outcomes and reduce its morbidity and mortality.In fact, since the coronavirus disease 2019 pandemic, the incidence of AAH has increased by over 50%, with a subsequent increase in referrals to liver transplant centers for patients with AAH[3,4].Additionally, liver transplant waiting list additions increased by 105.6% and liver transplant recipients increased by 411.8% in patients with AAH[5].The mortality of AAH may be as high as 30% at 28 d and surpass 50% at 1 year[1].Several prognostic scores have been created and studied throughout the years in an attempt to predict the mortality of AAH.For instance, the Maddrey discriminant function (MDF), conceived in 1978, has been the first[6] and the most discussed score for the assessment of disease severity and guidance of treatment initiation.However, emerging data has supported other prognostic scores such as the model for end stage liver disease (MELD) score.Among others scores, the dynamic Lille score is renowned for its ability to assess the response of AAH to therapy as the disease progresses.There is no consensus regarding the superiority of one score compared to the other.This review aims to discuss the most recent evidence regarding the clinical relevance and performance of the available AAH prognostic scores.
DIAGNOSIS AND SEVERITY OF ALCOHOL-ASSOCIATED HEPATITIS: CLINICAL, BIOLOGICAL AND HISTOLOGICAL FEATURES
AAH is a potentially fatal complication of chronic alcohol abuse that commonly occurs after a sudden increase in alcohol consumption.Although AAH may present abruptly, it most often progresses insidiously over days or weeks with patients complaining of fatigue and malaise followed by anorexia, nausea and vomiting before developing ascites or jaundice[7].While the latter are the most important symptoms for diagnosis in clinical practice settings, other signs and symptoms may be seen including tender hepatomegaly, low-grade fever, and abdominal pain[8].The diagnosis is mainly clinical, however abdominal imaging should also be performed to rule out obstructive biliary disease.Additional workup should rule out acute viral hepatitis, severe autoimmune liver disease and Wilson disease[9,10].The gold-standard diagnostic test remains liver biopsy.The decision of performing biopsy should be guided by the pre-test probability of AAH and should consider the risk of complications such as bleeding.As per the AAH consortia in 2016 outlining the consensus criteria for the diagnosis of AAH[9], the clinical diagnosis of AAH is based on the presence of typical clinical features as well as laboratory tests that help rule out other causes of liver injury and guide treatment decisions.The most important clinical feature is the onset of jaundice within 8 wk of heavy alcohol consumption overlying a daily consumption that is superior to 40 g/d in women and 60 g/d in men for at least 6 mo.Serum bilirubin level is typically above 3 mg/dL.Other important features include elevated transaminases (aspartate aminotransferase AST > 50, AST to alanine aminotransferase ratio ALT ratio > 1.5) that do not surpass 400 IU/L[9].
The diagnosis of definite, probable, or possible AAH depends on the presence of those typical clinical features as well as laboratory tests that help rule out other causes of liver injury and guide treatment decisions (Table 1)[9,11].While histological confirmation remains the gold standard, this approach not always necessary when other clinical and laboratory features are clearly suggestive of AAH.Liver biopsy may also help guide treatment decisions in some cases, for example, when there is uncertainty about the severity of liver injury or if drug-induced liver injury is suspected[10].Histological features of AAH include microvesicular steatosis, periportal Mallory-Denk bodies, and neutrophilic infiltration in the portal areas.Altamiranoet al[12] proposed an AAH histologic scoring system that included degree of fibrosis, neutrophil infiltration, type of bilirubinostasis, and presence mega-mitochondria.The authors were able to demonstrate that this scoring system was correlated with severity of liver dysfunction as well as mortality.However, this scoring system has not yet been validated in large cohorts and thus not yet routinely used clinically.
While histologic scoring systems may help to assess the severity of AAH, practically, clinical features remain the most important practical determinant of prognosis[8].Patients with more severe disease are more likely to require hospitalization and have a higher mortality rate.Multiple clinical scoring systems that assess the severity of liver disease of any cause exist, including MELD, Child-Turcotte-Pugh and Chronic Liver Failure Consortium-C (CLIF-C) ACLF (acute-onchronic liver failure) scores[13].Some scores were particularly aimed at predicting outcomes in AAH and are widely used including MDF and Age Bilirubin international normalized ratio (INR) Creatinine model (ABIC).Scoring criteria, clinical application and interpretation of relevant AAH prognostic scores are detailed in Table 2.While all these scoring systems have some value, they are far from perfect and need to be interpreted with caution.Head-to-head comparisons of these scores are lacking and it is unclear which, if any, is superior.
Patients with severe AAH have increased short-term mortality rates, causes include portal hypertension complications, multiorgan failure (liver, kidney) and infections[14].Assessment of the severity of AAH remains a complex task that requires careful clinical evaluation as well as consideration of multiple laboratory and imaging tests.The relevance of clinical prognostic scores to AAH pathophysiology is explained and illustrated in Figure 1.
PROGNOSTIC SCORING SYSTEMS
Maddrey discriminant function
MDF was the first prognostic score found for AAH.It was found through the discriminant analysis of biologic parameters associated with mortality in AAH.This was how, in an early clinical trial, Maddreyet al[6] found an independent association with death from AAH between the increase in prothrombin time (PT) and total bilirubin levels at the start of their study.
Discriminant Function = 4.6 × (Pt’s PT-control PT) + TBili.
Data on MDF sets the cutoff for severe AAH at 32, where patients with a score lower than 32 have a proven survival rate of 90% at 30 d without steroid therapy, which defines AAH as mild to moderate when MDF < 32.On the other hand, patients with MDF 32 or higher showed mortality exceeding 20%-30% at 30 d (severe AAH = MDF ≥ 32), and can be used as a threshold for initiation steroid therapy if no contraindications exist[15].
MDF was largely used in randomized controlled trials evaluating benefit of steroid therapy in AAH, which reported heterogenous results.In a meta-analysis of 418 patients with AAH, decreased 1-mo mortality after corticosteroid therapyvsplacebo was proven only in severe AAH (defined as MDF > 32) or in patients with hepatic encephalopathy (relative risk reduction of 36%)[16].
In a post-hoc multivariate analysis of the STOPAH trial (a large study that studied the effect of prednisolonevspentoxifylline on 28-d mortality), treatment with prednisolone displayed significantly improved survival at 28 d, which was limited to short term mortality when MDF > 32.No significant difference in mortality at 90 d or 1 year was found.Of note, the original STOPAH trial did not show any benefit with prednisolonevsplacebo on 28-d mortality[17].Because the trial was stopped prematurely (difficult to follow patients out long-term), 33 individuals were not included in 90 d or 1 year follow up and another 159 could not be followed for a full year.Even though the investigators met their goal enrollment of 1026 patients, the lower mortality than expected and use of MDF without liver biopsy probably led to many misclassifications.Furthermore, no taper was used in prednisolone treatment which may have caused harm to patients when they stopped taking the medication.
The above evidence elicits the role of MDF in AAH severity assessment and treatment decisions since it was commonly applied in the concerned trials.However, it has some drawbacks which give grounds for studies on evaluating potential superiority of other scores.MDF is calculated using PT and bilirubin.Despite its wide use in mortality prediction, the MDF lacks some important components which would strongly predict prognosis, such as serum creatinine[18].Moreover, PT is dependent on the control subject measurement, which creates variability among laboratories.These drawbacks make it mandatory to review research on other scores that might display better performance in AAH mortality prediction than MDF.There have been increasing reports that the MELD can exhibit superiority in AAH mortality prediction compared to MDF[18,19].
MELD score
The MELD is based on INR, bilirubin and creatinine.The new MELD-Na score also encompasses sodium levels.It is a widely used tool in prognostic and severity assessment of AAH.MELD score demonstrates comparable performance to MDF in mortality prediction at 1 mo (Se = 86%, Sp = 86%)[20,21] and at 90 d (Se = 75%, Sp = 75%).For example, a MELD score above 20 predicts 20% mortality at 90 d[22].Concerning the initiation of corticosteroid therapy in patients with AAH, benefit was proven for patients with MELD > 20, with evidence being the strongest in the range 25 to 39[23].MELDscore is widely used in prioritizing transplant receipt in patients with cirrhosis, that includes patients with severe AAH who are considered to have acute-on-chronic liver failure.

Table 1 Alcohol-associated hepatitis diagnosis probability in clinically suspected Alcohol-associated hepatitis[11]

Table 2 Alcohol-associated hepatitis prognostic scores: Components, purpose, clinical application and interpretation
Limitations of MELD score are related to elevated creatinine levels accentuating predicted mortality even when liver function is recovering.Acute kidney injury (AKI) is only one potential complication of AAH, the others (such as portal hypertension, infections, multiorgan failure) are not accounted for in the MELD score.Also, creatinine levels have interpersonal variability with factors such as sex, nutrition, and age, which could also create heterogeneity in MELD score profiles among individuals with similar degrees of hepatic injury, which might not correlate adequately with mortality levels.Sodium levels are also prone to fluctuation related to diuretic/free water administration rather than liver disease.Moreover, it is documented that MELD score for the same individual could differ depending on laboratory measurement of its variables (INR+++ > creatinine > bilirubin)[24-27].
MELD vs MDF: Which score is superior?
Multiple studies have compared MELD and MDF scores in predicting outcomes in AAH.A recent multinational retrospective analysis by Morales-Arráezet al[18](n= 2581), proved MELD superiority to MDF with a significant difference in the area under the curve in predicting mortality at 1 mo and 3 mo.The studied population was diversified by recruiting patients throughout 85 tertiary centers in 11 different countries from 3 different continents.The diversity of the population in the study of Morales-Arráezet al[18] reinforces findings by a previous analysis of the STOPAH trial by Forrestet al[28] in terms of MELD score superiority to MDF in AAH mortality/severity prediction, a finding reflected by multiple other database analyses of more homogeneous populations around the world[29-31].More details on the advantages and disadvantages of both scores as well as differences in scoring criteria are listed in Table 3.To analyze the evidence mentioned above: Despite the disadvantages of including creatinine levels in the MELD score and the abundance of MDF use and validation in early AAH trials, accounting for AKI in AAH prognosis is a large advantage of the MELD score over MDF as it addresses an important determinant of AAH mortality.Furthermore, using INR minimizes laboratory-dependent differences in PT values which provides a notable advantage to using MELD over MDF.
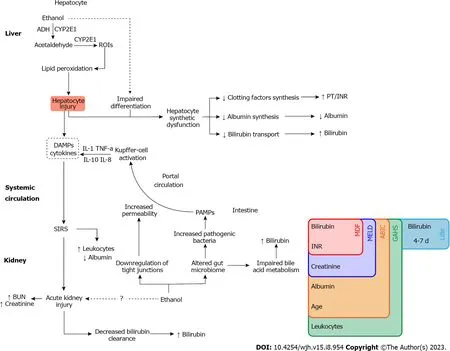
Figure 1 Pathophysiology of alcohol-associated hepatitis and correlation with prognostic scores.As hepatocytes metabolize ethanol, reactive oxygen species are generated and mediate hepatocyte injury through lipid peroxidation.Injured hepatocytes become unable to adequately perform their functions,this includes albumin and clotting factor synthesis as well as bilirubin transport.Damaged hepatocytes release inflammatory molecules such as danger-associated molecular patterns known as “DAMPs” which favor a systemic inflammatory response system (SIRS).With systemic inflammation, white blood cell count rises, and albumin concentration decreases.SIRS also precipitates acute kidney injury, resulting in a rise in serum creatinine and body urea nitrogen concentrations and causes decreased bilirubin clearance.Large amounts of ethanol alter the gut microbiome and increase intestinal permeability through the downregulation of tight junctions which impairs bile acid metabolism.Furthermore, there is favored growth of pathogenic bacteria that pathogen-associated molecular patterns (PAMPs).PAMPs reach the portal circulation through increased intestinal permeability and activate Kupffer cells in the liver.Which in turn amplifies systemic inflammation and the resulting consequences through cytokine secretion[8].PAMP: Pathogen-associated molecular patterns; SIRS: Systemic inflammatory response system; BUN: Blood urea nitrogen; MDF: Maddrey discriminant function; INR: International normalized ratio; MELD: Model for end-stage liver disease; GAHS: Glasgow alcoholic hepatitis score; PT: Prothrombin time.
A glimpse of other prognostic scores
Glasgow alcoholic hepatitis score: It is based on total bilirubin, age, blood urea nitrogen (BUN), PT and leukocyte count (white blood cell count; WBC).WBC and BUN are variables unique to GAH.GAH has demonstrated superior specificity and accuracy in predicting mortality in comparison to MDF or MELD, however GAH sensitivity to 1- and 3-mo mortality is inferior to MDF or MELD[32].While the concern for short-term mortality of AAH is substantial, a test with high sensitivity is preferred.GAH adds benefit in clinical decision making by complementing MDF: If MDF > 32, a GAHS 9 or greater is more accurate in predicting mortality, therefore in filtering steroid treatment indications.GAHS was only studied in a relatively homogenous population from one country, population, thus making it solely validated in the United Kingdom[33].
The ABIC model: Age, bilirubin, INR and serum creatinine level classifies patients into categories according to their survival risk.Risk groups are low, medium, and high, with respective survival rates of 100%-70%-25%.ABIC model ishelpful in prognosticating patients with AAH who were initiated on steroid treatment.However, ABIC model is not commonly used in assessing the indications for treatment initiation[34].
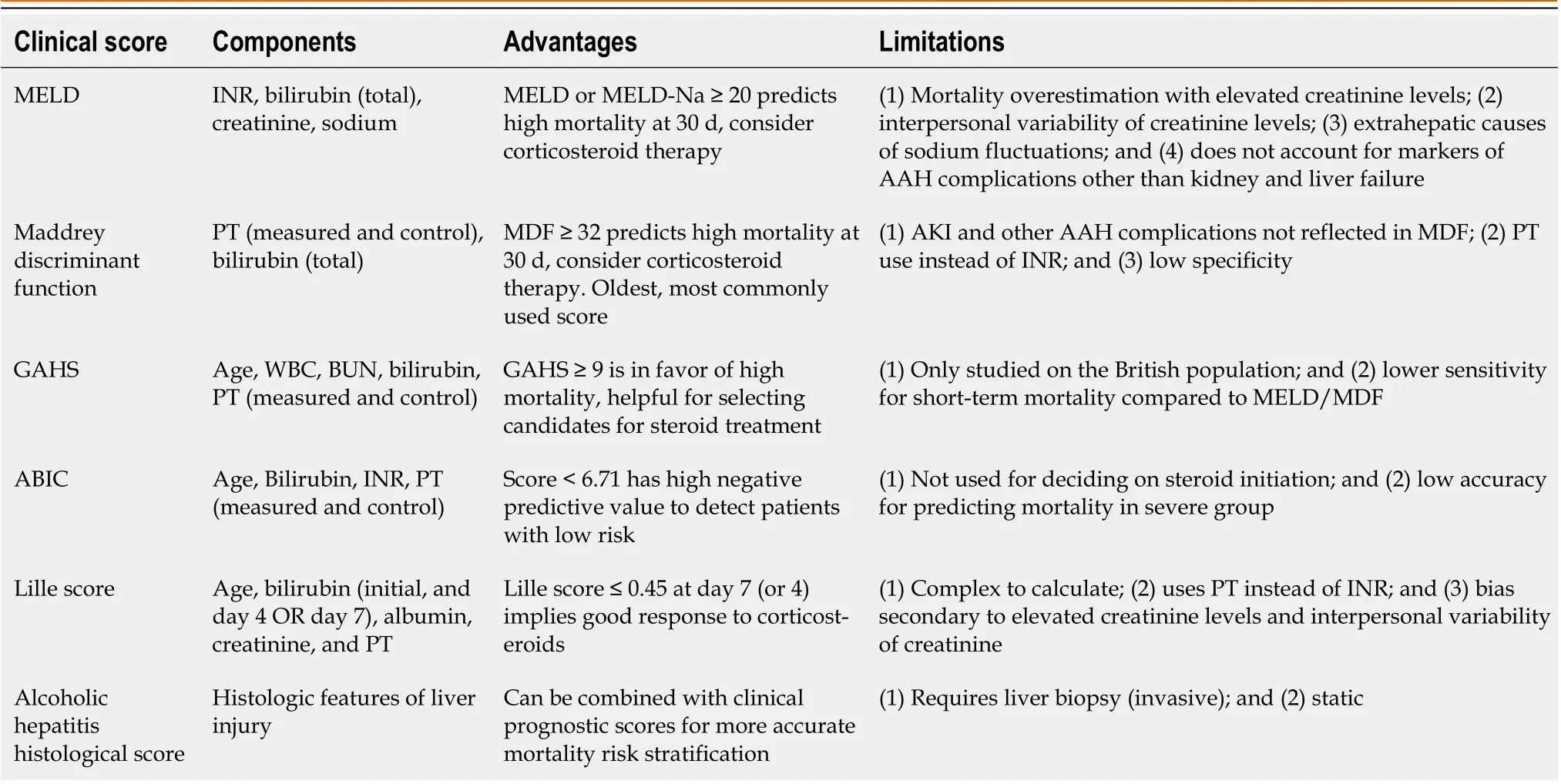
Table 3 Alcohol-associated hepatitis prognostic scores advantages and limitations
Static vs dynamic scores
As stativity brings bias into prognostic scoring for multiple reasons, some of which are mentioned above, dynamic scoring has been proposed and studied.Lille score adds dynamicity through the incorporation of bilirubin levels at 2 points in time: baseline levels and levels at day 7 of steroid therapy.Lille score is based on the concept that a decrease in bilirubin levels at the first week of treatment is a sign of good prognosis meaning that a score lower than 0.45 is suggestive of steroid treatment benefits outweighing the risks[35].On the other hand, a Lille score higher than 0.45 reflects a lack of response to steroids and therefore a low likelihood of benefiting from additional days of treatment[36].New studies are in favor of calculating Lille score at day 4 with comparable performance to day 7, this reduces the limitation of having to wait for 7 d[37].
Despite recent studies favoring MELD over MDF, combining MELD score (static) with Lille score (dynamic) would be interesting to evaluate on large populations in future studies on this matter given fluctuating course of disease, need for treatment response assessment and superior performance of combinations compared to single scores.
One limitation of clinical prognostic scores is performance in the long term.Few studies evaluate long term performance.In one of the studies, mortality of AAH patients at 1 year was found to be significantly lower when MELD < 20, 10.4%vs31.4% MELD > 20 (P< 0.001)[38].In another retrospective study, patients with MDF < 32 had a 50% mortality at 5 years, but the study did not feature any comparison to patients with MDF > 32[39].In a comparison of the most commonly used scores in 44 patients with biopsy proven AAH: GAHS, MDF, MELD, and ABIC scores all performed poorly in survival prediction after the 6-mo mark[40].
Prognostication of AAH presenting as acute on chronic liver failure
Alcohol is an important trigger for decompensation of chronic liver disease, including ACLF.The AAH scores mentioned above fail to encompass multiple organ failure beyond acute kidney injury.ACLF prognostic scores are applied to patients with severe AAH complicated by organ failure as mortality rates are similar in ACLF whether infection or AAH are incriminated.Notable prognostic scores for ACLF are: CLIF-C (European) ACLF, Asian Pacific Association for the Study of the Liver acute-on-chronic liver failure Research Consortium (AARC), North American Consortium for the Study of End-Stage Liver Disease (NACSELD)[41].
Clinical score correlation with histologic severity
As previously discussed, clinical data is the cornerstone of AAH prognostication.Histologic severity has been studied, with AHHS (alcoholic hepatitis histological score) being proposed by Altamiranoet al[12] to predict 90-d mortality through the combination of histological parameters that were most strongly associated to death.Overall, no statistical difference was found among MELD, ABIC and AHHS in 90-d mortality prediction.However, there are cases with added benefit to combining clinical and histological scores.In patients with MELD < 21, 90-d survival was higher when AHHS was < 5 compared to 5 or higher (94%vs72%;P= 0.001).Similarly, patients with ABIC B (medium risk) and AHHS < 5 have shown a potentially lower risk of death at 90 d,vsa moderate risk of death at 90 d (95%vs70% survival,P= 0.003) for ABIC B patients with AHHS 5 or higher[12,42].
Role of artificial intelligence in AAH prognostication
As artificial intelligence (AI) has been more commonly incorporated in health care, there have been attempts of optimizing AAH prognostication through AI.Of note, a multicenter retrospective cohort by Kezeret al[43] validated a new 30-d mortality scoring system based on age, BUN, albumin, bilirubin and INR.The score was derived through AI: The Mortality Index for Alcohol-Associated Hepatitis.Performance showed comparable accuracy to clinical scores, however superiority was only demonstrated compared to MDF but not to MELD[43].
In a recent abstract by Dunnet al[44], a new AI-generated score was created with the aim of predicting 90-d survival in AAH and validated in a multicenter international retrospective cohort.The score incorporates age, INR, bilirubin, creatinine, albumin, blood urea nitrogen and neutrophil to lymphocyte ratio.The abstract reports statistical superiority to MDF, MELD, MELD-Na, MELD 3.0.ABIC, GAHS.Steroid use showed decreased mortality at 30 d in those with ALCHAIN score 0.30-0.70.
ROLE OF SCORING SYSTEMS IN PREDICTING KIDNEY INJURY
As previously discussed, AAH elevated short-term mortality correlates with numerous complications, developing AKI is one of them.AKI is an important prognostic determinant in AAH, which makes predicting AKI risk in a patient with AAH an important step in management.It has been demonstrated that patients with liver failure and/or fulfillment of the SIRS criteria in addition to the nephrotoxic effects of alcohol are linked to the occurrence of AKI[45-47].
In a multicentric prospective cohort conducted by Sujanet al[48], AAH with AKI were more likely to have hepatic encephalopathy, SIRS criteria upon admission, higher MELD, baseline bilirubin, creatinine and INR.In a second phase, the study developed a risk score for AKI.AUROC was 0.74 (95%CI: 0.69-0.80;P< 0.001).AKI risk score incorporates SIRS, hepatic encephalopathy presence and MELD score on admission.The score stratifies AKI risk to three categories: Low (< 3), moderate (3-4), and high (> 4).Patients with AKI risk score classified as high had significantly higher short-term mortality compared to those with moderate and low AKI risk scores (90-d survival respectively 47%vs68%vs88%,Pvalue < 0.001)[48].
PREDICTING ALCOHOL RECIDIVISM
Treating AAH includes minimizing the risk for recurrence.Alcohol recidivism prediction is routinely done when evaluating patients for liver transplant.In the United States, 6 mo of alcohol abstinence are usually required for liver transplant (LT) consideration in most centers.This period is useful in terms of observing patients with AAH for clinical improvement/adherence to the treatment plan (abstinence), and even possibly the dissipation of the need for LT.However, the pitfall of the 6-month abstinence condition involves depriving patients with overall poor prognosis and high mortality rates from receiving a curative intervention[49].
Parallel to AAH severity scoring tools, Sustained alcohol use post-liver transplantation score, Stanford Integrated Psychosocial Assessment for Transplantation, Alcohol Relapse Risk Assessment, and High-Risk Alcoholism Relapse are all scores developed to be used when considering patients with AAH for LT.So far, these scores have not formally been used alone for selecting LT candidates given the high stakes.More studies are required to optimize our understanding of their reliability[50].
CONCLUSION
The mortality of patients with severe AAH emphasizes the need for accurate prognostication when managing cases of AAH.Many clinical scores have been studied and used, the most common notable being MELD, MDF and Lille score.While MDF is the oldest and the most popularly used score (MDF > 32) to determine the indication for corticosteroid initiation in AAH, MELD score has been increasingly showing superiority in assessing AAH severity.Dynamic prognostication is superior to static.Therefore, initiating steroids for a MELD of 20 or above and continuing them for a day 7 Lille score < 0.45 (favorable response to steroids) is the logical approach towards managing severe AAH.However, more research on AAH is necessary to improve our understanding of the major driving factors that will lead the way to improving our prediction models.
FOOTNOTES
Author contributions: Mitri J and Almeqdadi M reviewed the literature, planned the outline, and created the tables and figure; Mitri J wrote the manuscript with contributions and supervision from Almeqdadi M and Karagozian R; Almeqdadi M and Karagozian R proofread the manuscript; Almeqdadi M designed figure 1; Mitri J, Almeqdadi M, and Karagozian R revised the manuscript and wrote the comments to reviewers.
Conflict-of-interest statement: The authors declare that there was no conflict of interest regarding the publication of this mini-review.
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers.It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial.See: https://creativecommons.org/Licenses/by-nc/4.0/
Country/Territory of origin: United States
ORCID number: Jad Mitri 0009-0005-7331-1592; Mohammad Almeqdadi 0000-0002-5503-2371; Raffi Karagozian 0000-0002-7690-0596.
S-Editor: Chen YL
L-Editor: A
P-Editor: Chen YL
 World Journal of Hepatology2023年8期
World Journal of Hepatology2023年8期
- World Journal of Hepatology的其它文章
- Emerging therapeutic options for non-alcoholic fatty liver disease: A systematic review
- Stages of care for patients with chronic hepatitis C at a hospital in southern Brazil
- Tenofovir alafenamide significantly increased serum lipid levels compared with entecavir therapy in chronic hepatitis B virus patients
- Liver transplant in primary sclerosing cholangitis: Current trends and future directions
- Impact renaming non-alcoholic fatty liver disease to metabolic associated fatty liver disease in prevalence, characteristics and risk factors
