Research Progress and Prospects on the Anti-liver Fibrosis, Blood Circulation-promoting and Stasis-resolving Effects of Curcuma kwangsiensis Based on W-P Bodies
Weiqian GUO, Mingzhe LU, Yue PENG, Jiang LIN, Qianyu LIU, Miao YANG
AbstractLiver fibrosis is a necessary stage in the progression of chronic liver disease to cirrhosis. So far, no satisfactory drugs have been found to intervene in liver fibrosis. Liver microcirculation disorders are one of the important pathogenesis of chronic liver disease, and hepatic sinusoidal endothelial cells (HSECs) are the main cells that constitute the liver microcirculation barrier. In clinical practice, W-P bodies have been detected in HSECs of most patients with liver fibrosis. W-P bodies serve as a site for the synthesis and storage of vW factors, ET-1 and other cytokines that promote liver fibrosis. They can disrupt the structure and function of HSECs, cause liver microcirculation disorders, and exacerbate the progression of liver fibrosis. Previous studies have found that the Guangxi specialty ethnic medicine, C. kwangsiensis S.G.Lee et C.F. Liang, has definite effects in promoting blood circulation, resolving blood stasis, and resisting liver fibrosis. Based on this, a further research idea has been derived, stating that the blood circulation-promoting, blood stasis-resolving, and anti-liver fibrosis effects of C. kwangsiensis are produced by affecting the formation of W-P bodies, the synthesis and storage of contents in W-P bodies, and intervening in their exocytosis capacity.
Key wordsCurcuma kwangsiensis; Anti-liver fibrosis; Promoting blood circulation and resolving blood stasis; Hepatic sinusoidal endothelial cells; W-P body
DOI:10.19759/j.cnki.2164-4993.2023.04.014
Liver fibrosis refers to the occurrence of steatosis, inflammation and necrosis of liver cells after being affected by various physical and chemical factors. It is a chronic liver disease occurs in the original necrotic area where excessive proliferation and abnormal deposition of extracellular matrix components coexist, after irregular regeneration of liver cells. There are many causes of liver fibrosis, such as chronic hepatitis B, chronic hepatitis C, fatty hepatitis (including alcoholic or non-alcoholic), autoimmune liver disease, schistosomiasis liver disease, drug-induced liver disease, and other chronic liver damage factors, which can all cause this disease[1]. Hepatic fibrosis is a typical pathological feature that occurs in the development of chronic liver diseases, as well as a necessary pathological process for various chronic liver diseases to develop into cirrhosis or even liver cancer[2]. One third of patients with liver fibrosis can develop into cirrhosis, leading to liver cancer. In China, 1/30 of the population is patients with chronic liver disease. Without appropriate and effective treatment, 1/50 of these patients will develop cirrhosis every year. After the occurrence of liver cirrhosis, the probability of cancer transformation reaches half within ten years[3]. Therefore, we should attach great importance to the high incidence rate and high mortality of the disease in China. Numerous liver disease researchers have pointed out that the early and middle stages of liver fibrosis are actually reversible pathological phenomena. Professor Hans Popper, the chief scholar of contemporary liver disease research, believes that methods that can prevent or delay liver fibrosis will be able to treat most liver diseases. Others believe that[4], liver fibrosis is easier to be reversed than pulmonary fibrosis, cardiac fibrosis and scleroderma. If hepatitis B and hepatitis C are effectively treated, it can effectively prevent the development of liver fibrosis, which effectively proves the reversibility of liver fibrosis. In summary, it can be seen that finding effective means to effectively block the progression of liver fibrosis in the early and middle stages has positive clinical significance for controlling and improving the development of liver fibrosis patients condition and disease prognosis.
Liver Microcirculation, Hepatic Sinusoidal Endothelial Cells and the Occurrence and Development of Liver Fibrosis
The liver, as the most important metabolic organ in the human body, constantly undergoes active blood circulation and material exchange. The disturbance of microcirculation in the liver is an important factor in the progression of chronic liver disease. Improving the microcirculation of the liver[5] has a very positive effect on the recovery of liver function, and can effectively intervene in the development of liver fibrosis and the formation of liver cirrhosis lesions. The key exchange channel of liver microcirculation is called the hepatic sinusoid, which is one of the most permeable substance exchange structures in the human body. In the structure of the hepatic sinusoid, the content of endothelial cells in the hepatic sinusoid exceeds two-thirds. Therefore, the hepatic sinusoidal endothelial cells (HSECs) are the most important cells for maintaining normal microcirculation of the liver and ensuring material permeability and exchange between blood and liver cells[6]. Normal HSECs are different from general vascular endothelial cells. Their biggest structural feature is that they are densely packed with fenestrae in sieve-shaped arrangement, and there is no basement membrane barrier outside the cell wall, so substances can freely pass through the fenestra structure on HSECs, quickly and freely exchanging between blood and liver cells. The number and size of fenestrae of HSECs and the presence or absence of extracellular basement membrane structure jointly regulate the microcirculation of the liver and directly determine whether the material exchange between hepatocytes and blood is smooth. When liver fibrosis occurs[7], extracellular matrix deposits around the hepatic sinusoid structure, and continuous basement membrane blocking material exchange appears between HSECs and hepatocytes, accompanied by reduction or disappearance of window holes and activation of hepatic stellate cells. The above three lesions are collectively called hepatic sinusoid capillarization. When liver fibrosis occurs[7], extracellular matrix deposits around the hepatic sinusoid structure, and continuous basement membrane blocking material exchange appears between HSECs and hepatocytes, accompanied by reduction or disappearance of fenestrae and activation of hepatic stellate cells. The above three lesions are collectively called sinusoid capillarization. Sinusoid capillarization is a characteristic lesion that occurs during the process of liver fibrosis and cirrhosis, which can significantly affect liver microcirculation function and cause portal hypertension difficult to treat clinically. After the formation of basement membrane, it can also bind and store a large number of cytokines that promote the development of liver fibrosis. These cytokines can regulate the proliferation and activation of hepatic stellate cells, thereby significantly accelerating the progression of liver fibrosis. There are research results indicating that[9], the occurrence of "sinusoid capillarization" lesions always occurs earlier than liver fibrosis, and can significantly accelerate the development of liver fibrosis lesions. The damage of HSECs has become a necessary and critical condition for the activation of hepatic stellate cells. After removing the causes of hepatic sinusoid capillarization lesions, fibrotic lesions can also undergo significant reversal[10-11]. We thus inferred that structural or functional changes in HSECs can significantly affect the microcirculation of the liver, thereby affecting the occurrence and development of liver fibrosis diseases. Therefore, in the theory of traditional Chinese medicine, the therapy of promoting blood circulation and resolving blood stasis, which can significantly improve the microcirculation of the liver, has become a potential target for research on the prevention and treatment of liver fibrosis diseases by combining traditional Chinese and Western medicine, and a new hotspot in research on the prevention and treatment of chronic liver disease.
W-P Bodies in HSECs and the Occurrence and Development of Liver Fibrosis
In the middle of the 20th century, scholars found a short rod-shaped large organelle in the cytoplasm of the endothelial cells of the pulmonary artery in rats, which originated from the Golgi apparatus and is called W-P body. W-P bodies serves as a special secretory organelle in endothelial cells. They contain von Wiliebrand factor, P-selectin, ET-1, histamine, nitric oxide synthase and other cytokines related to the coagulation process and the development of inflammation[12]. These cytokines use the W-P bodies as storage sites and release bases. After being released into the cytoplasm, they rapidly activate coagulation factors, accelerate platelet adhesion, and contract endothelial cell fenestrae, thereby deteriorating organ microcirculation[13]. W-P bodies are not present in normal sinusoidal endothelial cells, but can be found in large quantities in the cytoplasm of sinusoidal endothelial cells in many patients with chronic liver diseases. Studies have shown that these HSECs with W-P bodies had obvious structural changes, such as reduced number of fenestrae, significantly reduced diameter of fenestrae, and even a continuous flaky basement membrane formed outside the cells[14]. These HSECs with W-P bodies have undergone a transformation into general vascular endothelial cells, and their structure has also begun to transform into continuous capillaries. W-P bodies interfere with the coagulation process of the hepatic sinusoid, contract the hepatic sinusoid fenestrae, and disrupt liver microcirculation. And they are closely related to the formation and development of liver fibrosis.
The contents of W-P bodies can be classified as follows: ① von Wiliebrand factor: It is a unique cytokine of endothelial cells, and W-P bodies themselves are composed of von Wiliebrand factor and its pre-rupture sequence. Immunohistochemical detection of the expression level of von Wiliebrand factor is considered a classic indicator for identifying W-P bodies[15]. This factor, as a constituent structure of coagulation factor VIII, can significantly promote blood coagulation. As a connector, it connects the specific receptors on the platelet membrane to the tissue beneath the vascular endothelium, causing platelets to adhere to the site of vascular injury. The von Wiliebrand factor can also connect and stabilize coagulation factor VIII in the circulating blood. When the von Wiliebrand factor is secreted by W-P bodies into the cytoplasm of HSECs and arranged and expressed along the hepatic sinusoid structure[16], it can cause the blood flow in the hepatic sinusoid to be in a prethrombotic state, which is prone to the formation of microthrombosis, which exacerbates liver microcirculation disorders. ② P-selectin: It is synthesized by mitochondria and stored in the resting HSECs, and distributed close to the inner membrane of W-P bodies. If P-selectin appears in the cytoplasm of HSECs, it is an early marker of cell activation and plays an important role in the early inflammatory response. When HSECs become active or is stimulated by thrombin[17], P-selectin will be secreted from the inner side of the membrane of W-P bodies and released into the cytoplasm, and quickly migrate to the surface of HSEC cells. As a transmembrane glycoprotein, it mediates the rolling of neutrophils and slows down their flow rate, and adheres to and attaches to the surface of HSEC cells, causing microcirculation disorder. In chronic liver inflammation, P-selectin can be taken into W-P bodies for many times, repeatedly secreted and released, and participate in and intensify the inflammatory process throughout. ③ Endothelin-1: ET-1 in the liver is mainly stored in W-P bodies, and it is known to be the strongest biological peptide for vasoconstriction, and the only substance that shrinks capillaries below 50 nm. It can significantly shrink the portal vein and hepatic sinusoid, make the fenestrae of HSECs disappear, and cause liver microcirculation disorder. This event has a very important relationship with the formation of portal hypertension[18], resulting in decreased liver blood flow and turbid and swollen hepatocytes, and promoting the occurrence and development of liver diseases. When liver injury occurs, HSECs produce a large amount of ET-1 and store it in W-P bodies. Yang et al.[19] pointed out that the large storage and secretion of ET-1 is precisely due to the dysfunction and damage of HSECs. The results showed that in animal models of liver injury, the content of the premessenger RNA of ET-1 derived from HSECs multiplied; it was found that ET-1 derived from HSECs could effectively activate hepatic stellate cells and cause strong contraction of hepatic stellate cells; and the result of such behavior was to surround and compress the hepatic sinusoid structure, further reducing the diameter of the hepatic sinusoid and exacerbating the obstruction of liver microcirculation[20]. ④ Histamine: W-P bodies are an important storage place of histamine in the liver. When the liver is repeatedly stimulated by injury, histamine is released into HSECs, which can promote CD8+T cells to secrete lymphocyte chemokines. When P-selectin has caused the rolling adhesion of white blood cells in the blood, histamine can further increase the flow of rolling white blood cells, increase the permeability of blood vessels, enhance the adhesion of white blood cells induced by lymphocyte chemokines, and participate in aggravating the disorder of liver microcirculation. ⑤ Nitric oxide synthase: This enzyme can catalyze the guanidine removal of L-arginine, producing nitric oxide localized within W-P bodies. The main types of nitric oxide synthase in the liver are endothelial nitric oxide synthase (eNOS) and inducible nitric oxide synthase (iNOS), with significant differences in their physiological functions. Under normal circumstances, the liver only expresses endothelial nitric oxide synthase, while the amount of inducible nitric oxide synthase is very low[21]. Endothelial nitric oxide synthase produces a basic level of nitric oxide, which plays a protective role in the liver, can resist stimulating factors that damage the liver, regulate liver perfusion, and prevent platelet adhesion and the formation of microthrombosis. Inducible nitric oxide synthase is not expressed in the liver under physiological conditions. However, after the HSECs are repeatedly stimulated by lipopolysaccharide and cytokines, inducible nitric oxide synthase can appear, and can continuously produce a large amount of nitric oxide, resulting in pathophysiological effects that damage the liver, including interference with the biotransformation of the liver, reduction of the metabolic rate of hepatocytes, and induction of apoptosis of hepatocytes and DNA damage.
The secretion behavior of W-P bodies releasing their stored cytokines into the cytoplasm of hepatic HSECs is of great significance for the microcirculation of the liver. It will significantly affect multiple pathological and physiological processes such as blood coagulation, thrombosis, and inflammation development in the body. The specific secretion process is described as follows[22]: under the stimulation of adrenaline and Ca2+, W-P bodies move towards the cell membrane of HSECs, forming vesicles, which release the contents towards the cytoplasm of the membrane through exocytosis. Some studies have pointed out that[23], cAMP-mediated exocytosis of W-P bodies caused by the increase of adrenaline is the most important physiological regulation mode to increase the level of von Wiliebrand factor and P-selectin in the cytoplasm of HSECs. After downregulating the gene expression of cell adhesion molecule Zyxin in vascular endothelial cells, it can significantly inhibit the secretion of vW factor caused by cAMP agonists, while mice undergone Zyxin gene knockout can exhibit phenotypes such as prolonged bleeding time and slower thrombosis formation. It can be observed from live cell imaging systems that Zyxin protein can induce the remodeling of microfilament molecules around submembrane vesicles of endothelial cells, forming a circular "scaffold" structure that precisely regulates the secretion behavior of vesicles in time and space, which plays an indispensable role in vascular repair, blood coagulation, and thrombosis processes[24]. Further research has shown that Myosin IIa is the strongest binding protein of Zyxin molecules, and downregulating the expression of Myosin IIa gene can significantly inhibit the secretion of vW factor caused by cAMP agonists. However, mice undergone endothelial Myosin IIa gene knockout can exhibit phenotypes such as prolonged bleeding time and slower thrombosis formation. And a rheostat-like regulatory mechanism was discovered for W-P body secretion: Myosin IIa and Zyxin protein undergo skeletal binding, and then can jointly regulate the relationship between submembrane microfilament molecules and vesicles, leading to exocytosis. The above research not only discovered a new structural molecule, Zyxin, that directly regulates endothelial cell secretion, but also the binding protein, Myosin IIa, which is essential when Zyxin plays its role. Based on the above research results, the interaction between microfilament molecular network and vesicle was observed for the first time in living cells, and a new skeleton model for regulating vesicle secretion was proposed. This research result provides new ideas and models for studying the driving force mechanism of stimulating vesicle secretion. It further provides new directions and targets for clinical treatment of thrombotic diseases and microcirculatory disorders.
Agricultural Biotechnology2023Blood Stasis Syndrome in Traditional Chinese Medicine and Liver Fibrosis in Western Medicine
Traditional Chinese medicine theory describes liver fibrosis as: “Liver fibrosis has symptoms such as blood stasis or accumulation, and belongs to the category of hypochondriac pain, jaundice, accumulation, and abdominal mass”. Blood stasis becomes a pathological product that is easily formed during the course of chronic liver disease, as the liver stores blood and controls conveyance and dispersion, that is, the liver entity belongs to yin, but its function belongs to yang. After formation, it becomes the cause of liver fibrosis, further exacerbating it. Research on the integration of traditional Chinese and Western medicine has pointed out that the essence of blood stasis is the proliferation and degeneration of fibrous connective tissue, as well as microcirculation disorders. Many traditional Chinese medicine scholars believe that the treatment of this disease should start with resolving blood stasis, and the first step is to dispel potential blood stasis. It is believed that the treatment of liver fibrosis disease should be mainly based on promoting blood circulation and resolving blood stasis throughout the entire process. Traditional Chinese medicine theory believes that blood stasis is an important factor in the occurrence and development of liver fibrosis, and meanwhile, blood stasis is often accompanied by symptoms such as stagnation of liver qi, damp heat, phlegm, and deficiency of qi and blood[27]. In the clinical treatment of traditional Chinese medicine, the famous formula of promoting blood circulation and resolving stasis, "Xuefu Zhuyu Decoction", has been used on many patients with liver fibrosis, achieving precise therapeutic effects. It also confirms the close relationship between blood stasis in traditional Chinese medicine and liver fibrosis in Western medicine from the perspective of therapeutic effect. Traditional Chinese medicine believes that qi stagnation and qi deficiency hinder the normal movement of qi and the distribution and operation of blood, which is the physiological essence of the formation of blood stasis. qi stagnation and blood stasis, as well as Qi deficiency and blood stasis, are the main traditional Chinese medicine syndromes of liver fibrosis[29]. Research on the integration of traditional Chinese and Western medicine has pointed out that[30] the liver can exhibit signs of Chinese medicine blood stasis syndrome in the early stages of damage, and as liver fibrosis forms and worsens, the signs of blood stasis syndrome become more and more obvious. During liver fibrosis, changes in the secretion behavior of a series of vasoactive factors such as TGF-β1 and VEGF, changes in synthesis and secretion of extracellular matrix and changes in structural damage and functional disorder of HSECs, may occur. These lesions can jointly cause changes in liver morphology and hemodynamics; and the characteristics of these lesions are also consistent with the characteristics of Chinese medicine blood stasis syndrome. It can be concluded that blood stasis syndrome is one of the essence of most liver fibrosis diseases; and the traditional Chinese medicine method of promoting blood circulation and resolving stasis can effectively improve microcirculation disorders in the liver. According to the traditional Chinese medicine method for promoting blood circulation and resolving blood stasis, using Chinese herbs for promoting blood circulation and resolving blood stasis, can effectively open the bottleneck and dilemma in the treatment of liver fibrosis in Western medicine.
Establishing an Animal Model for the Study of Blood Stasis Syndrome―Liver Fibrosis Disease by Combining Traditional Chinese and Western Medicine
Under practical conditions, viral infection, alcohol damage, fat deposition, immune damage, various acute and chronic physical and chemical injuries, and traditional Chinese medicine etiology and pathogenesis damage, can all lead to fibrosis changes in the liver. The causes of liver fibrosis are numerous and complex, making it difficult to comprehensively and accurately replicate and imitate the complex fibrotic characteristics of human liver in the study of combining traditional Chinese and Western medicine to resist liver fibrosis, regardless of which single factor is used to model experimental animals, and of course, it is impossible to replicate the traditional Chinese medicine blood stasis syndrome with complicated conditions. Moreover, traditional single-factor modeling methods also have drawbacks such as long modeling cycles, high animal mortality rates, and unstable fibrotic lesions[31]. These technical deficiencies limit the applicability and research value of these liver fibrosis experimental animal models. The research on the pharmacology of traditional Chinese medicine for promoting blood circulation and resolving blood stasis and for resisting liver fibrosis mentioned above requires animal models that are rooted in the theory of blood stasis syndrome in traditional Chinese medicine, and prepared by combining with modern Western medicine theory and technology, using composite animal modeling techniques, based on multiple pathogenic factors. We have established an animal model of liver fibrosis of the blood stasis type induced by multiple factors, such as dimethylnitrosamine (DMN) plus injection of norepinephrine (NE) and bovine serum albumin (BSA), plus gavage with ethanol solution and high-fat and low-protein feeding[32]. This model has significant advantages in simulating the accuracy of human conditions and replicating Chinese medicine blood stasis syndrome similar to human liver fibrosis. At the end of modeling, the rats exhibited obvious Chinese medicine blood stasis symptoms such as blue and purple plaques on the tongue, varicose veins under the tongue, darkened eyeballs, bruises on the tail, weight loss, and easy shedding of hair, and pathological examination in Western medicine revealed fibrosis pathological changes such as proliferation of liver fibrous tissue, formation of pseudolobuli, and dilation and stasis of hepatic sinusoid. These research results indicated that the experimental animal model of liver fibrosis with blood stasis syndrome established by the combination of the above composite factors has been established; and the pathological examination results and Chinese medicine syndrome observation results of the experimental animal model were consistent with liver fibrosis lesions and Chinese medicine blood stasis syndrome. The successful establishment of this experimental animal model provides strong technical support for the research on the prevention and treatment methods of blood stasis type liver fibrosis combining traditional Chinese medicine with Western medicine and the treatment of chronic liver disease with traditional Chinese medicine for promoting blood circulation and resolving blood stasis.
Research Progress on the Anti-liver Fibrosis and Blood Stasis Syndrome Treatment Effects of Curcuma kwangsiensis
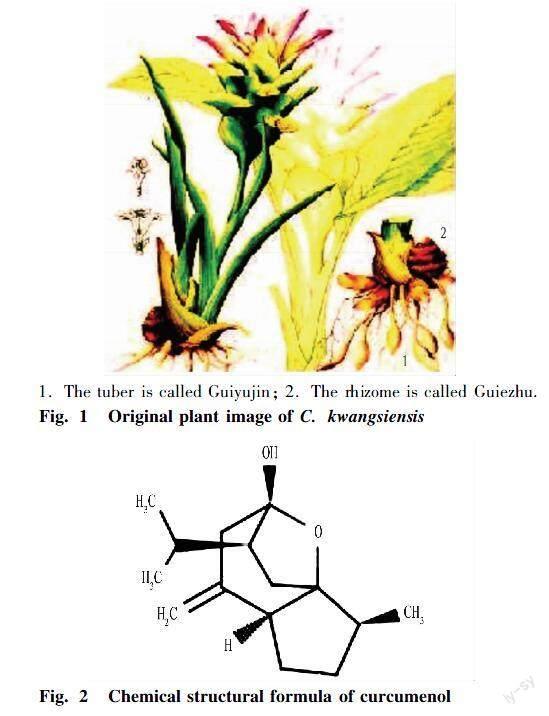
C. kwangsiensis S.G.Lee et C.F. Liang is a bulk genuine medicinal herb in Guangxi, with an annual output of approximately 1 200-1 500 t, accounting for about 60% of the total production in China. It is the main variety of Curcuma in the medicinal market. The dry rhizomes of C. kwangsiensis are called "Guiezhu", also known as "Maoezhu", and are traditional Chinese medicine for promoting blood circulation and resolving blood stasis (Fig. 1). It has a pungent, bitter and warm taste, and is attributed into the liver and spleen. It is strong and intense in drug property, and can break through the blood in the qi. It also has the ability to dissipate accumulation and relieve pain. Therefore, C. kwangsiensis can be used to treat diseases such as abdominal and hypochondriac distension and pain due to qi stagnation and blood stasis, abdominal lumps, amenorrhea due to blood stasis. The herb mainly contains volatile oil and curcumin; and the volatile oil (curcumol) is rich in content, accounting for about 1.0%-2.5% of its weight, mainly sesquiterpene lactones, and is the main active ingredient of curcumol in Guangxi[33] (Fig. 2). The 2010 edition of the Chinese Pharmacopoeia includes the volatile oil of Curcuma as an antiviral and anticancer drug, and uses the content of curcumol as a control indicator for the quality standard of Curcuma. According to literature reports, curcumol has various effects such as promoting blood circulation and resolving stasis, anti-tumor, lowering blood lipids, protecting the liver, anti-inflammatory, cholagogic, antioxidant, and antithrombotic[34]. Moreover, it has definite effects in treating hepatitis, reversing liver cirrhosis, protecting the liver, resisting inflammation and bacteria, regulating immunity, and controlling certain advanced malignant tumors[35]. Pharmacological research based on the rat model of blood stasis syndrome found that[36]: curcumol could significantly reduce the change rate of whole blood viscosity in rats with blood stasis syndrome and significantly prolong the blood coagulation time, and showed the effects of promoting blood circulation and resolving stasis on both blood stasis model and normal mice.
In recent years, our research team has comprehensively carried out research on the active ingredient of the genuine medicinal herb in Guangxi, curcumol, in promoting blood circulation, resolving blood stasis, and resisting liver fibrosis. Here we will briefly introduce the preliminary research results of our research team. ① The decoction of C. kwangsiensis could obviously inhibit the acute liver damage of rats caused by CCl4, reduce the levels of ALT and AST and increase plasma albumin, and had the liver protection effects of reducing enzymes, inhibiting lipid peroxidation of liver tissue and improving liver protein synthesis[37]. Curcumol decoction could also reduce the content of HA, LN and PC III in plasma, and Masson staining observation confirmed the effect of reducing fibrosis in liver tissue[38]. ② Based on the study of human hepatic stellate cell line (HSC-LX2), which is the core cell of liver fibrosis, we focused on exploring the target sites and molecular mechanisms of curcumol action on this cell from several aspects such as cell proliferation rate, cell apoptosis, collagen synthesis and secretion, and expression of profibrotic cytokines[39-40]. The results showed that the drug could significantly inhibit the cell proliferation rate of HSC-LX2, block cells from entering the proliferation cycle, and induce cell apoptosis; this drug could reduce the synthesis and secretion of fibrotic components, α-SMA, type I and type III collagen of HSC-LX2 strain; it could reduce the expression level of fibrogenic factors such as TGF-β1 and VEGF; and it could also increase the expression of MMP1 and MMP13 enzymes that degrade fibrotic components. The above research results clarify the anti-liver fibrosis effect of curcumol by inhibiting the cell viability and secretion function of HSC-LX2. ③ In the study of human HSECs[41], it could be observed that curcumol could intervene in the phenomenon of hepatic sinusoidal capillarization by reopening the closed hepatic sinusoidal fenestrae of HSEC cells, resulting in a significant increase in the total area of fenestrae that allow materials to pass through; curcumol reduced the continuous basement membrane formed outside HSEC cells; and curcumol caused a decrease in the expression level of various cytokines that cause fibrosis and microcirculation disorders, such as ET-1 and TGF-β1, CTGF and Col IV. The above research results confirm that curcumol can significantly improve the pharmacological effects of promoting blood circulation and resolving blood stasis in liver microcirculation by inhibiting hepatic sinusoidal capillarization, and partially explain the action mechanism of curcumol on the structure and function of HSECs. Meanwhile, some valuable phenomena have also been found in the study: after using curcumol, the number of W-P bodies that appeared in HSECs could be significantly reduced; and the expression level of ET-1 protein in the cytoplasm of HSECs decreased (ET-1 is mainly stored in W-P bodies and released into the cytoplasm of HSEC after pathological stimulation). These have become considerations for further in-depth research. What is the relationship between the decrease in the level of ET-1 in the cytoplasm and the disappearance of W-P bodies? Are these two changes achieved by curcumol by altering the pathological changes of microvessels in the liver, improving the phenomenon of hepatic sinusoid capillarization, and improving microcirculation disorders in the liver? These issues need to be further addressed in subsequent research. In recent years, the hot spot of liver disease research suggests that the occurrence of liver microcirculation disorder is largely related to the formation of W-P bodies in HSEC cells during liver fibrosis, and the W-P bodies contain a large number of von Wiliebrand factor, P-selectin and ET-1; and these factors are excreted into the cytoplasm of HSECs by W-P bodies, and they can participate in the pathophysiological processes such as the hepatic sinusoid becoming smaller, the disappearance of the fenestrae, the chemotaxis and adhesion of platelets and white blood cells, thrombosis, and the acceleration of blood coagulation, resulting in the obvious disorder of liver microcirculation, the formation of blood stasis syndrome, and then leading to clinical cirrhosis of portal hypertension. It can be seen that research on the formation of W-P bodies, the cytokines stored in W-P bodies and the exocytosis function of W-P bodies is essential for intervening in liver microcirculation disorders and explaining the effect of anti-liver fibrosis drugs in promoting circulation and removing stasis, and is very valuable.
Conclusions and Prospects
Based on the above summary of the mechanism of liver fibrosis, the mechanism of promoting blood circulation and resolving stasis, the structural and functional characteristics of HSECs, and the pharmacological research progress of C. kwangsiensis, it has been clarified that the active ingredient of Guangxi specialty ethnic medicine, curcumol, has a definite anti-liver fibrosis effect. The inhibition of hepatic sinusoidal capillarization and the improvement of liver microcirculation by the drug were further observed, further indicating its blood-activating and stasis-resolving effects. Therefore, in-depth exploration can be conducted and further research hypothesis stating that the effects of C. kwangsiensis in promoting blood circulation, resolving blood stasis and resisting liver fibrosis are produced by affecting the formation of W-P bodies and the synthesis and storage of contents in W-P bodies and intervening in their exocytosis ability, can be proposed.
The ideas for further research are as follows: we can establish a rat model of liver fibrosis of the blood stasis type and a human hepatic sinusoidal endothelial cell model activated by lipopolysaccharide, and the two models can be observed after being given C. kwangsiensis for intervention. ① The number of W-P bodies in HSECs will be observed and counted to jointly determine the number level of W-P bodies by combining with the detection of the expression level of intracellular vW factor (a specific protein of W-P bodies). ② The expression levels of vW factor, P-selectin, endothelin-1, histamine and NOS in HSEC cells will be detected to reflect the ability of W-P bodies to synthesize and store cytokines. ③ The driving force of exocytosis was measured through the binding level of Zyxin protein and Myosin IIa protein (the binding of which triggers the exocytosis of W-P bodies); and the final results of exocytosis of W-P bodies will be determined by the specific localization and distribution of vW factor, P-selectin, endothelin-1, histamine and NOS inside and outside the bodies. ④ After obtaining purified proteins of Zyxin and Myosin IIa using GST pull down technology, the pure binding relationship between the two proteins can be confirmed, and their binding level (binding amount) can be determined; at this point, C. kwangsiensis can be added to observe whether the drug directly blocks the binding of the two proteins, and explore whether the action target of the drug is based on interfering with the binding of Zyxin and Myosin IIa; and the blocking level (blocking amount) can be determined. Through the above observation, detection, analysis, and comparison, it is possible to comprehensively understand the specific interventions of C. kwangsiensis in the formation of W-P bodies, the ability to synthesize and store contents of W-P bodies, and the exocytosis capacity of W-P bodies in the occurrence of chronic liver disease from the organizational and cellular levels. The results can fully explore the action mechanism and target sites of the drug in promoting blood circulation and removing blood stasis and resisting hepatic fibrosis. This study can provide richer scientific basis for further development and utilization of the active ingredients of Guangxi specialty ethnic medicine, C. kwangsiensis, in the treatment of liver fibrosis diseases. It can provide new targets and new ideas for the treatment of liver cirrhosis and portal hypertension with traditional Chinese and Western medicine.
References
[1] THOMAS PEMBROKE, MARC DESCHENES, BERTRAND LEBOUCH, et al. Hepatic steatosis progresses faster in HIV mono-infected than HIV/HCV co-infected patients and is associated with liver fibrosis[J]. Journal of Hepatology, 2017, 24(9): 463-470.
[2] FAN HN, CHEN NW. Progress in epidemiological research on liver fibrosis[J]. International Journal of Digestive Diseases, 2014, 34(1): 29-31, 47. (in Chinese).
[3] SHI JJ, CHANG WX, LI YY, et al. Current state and challenges of clinical treatment of chronic hepatitis B[J]. Science & Technology Review, 2016, 34(20): 34-39. (in Chinese).
[4] FRIEDMAN SL. Mechanisms of hepatic fibrogenesis[J]. Gastroenterology, 2018, 134(6): 1655-1669.
[5] BATALLER R, BRENNER DA. Liver fibrosis[J]. J Clin Invest., 2005, 115(2): 209-218.
[6] GRIMM JB, ENGLISH BP, CHEN J, et al. A general method to improve fluorophores for live-cell and single-molecule microscopy[J]. Nat. Methods., 2017(12): 244-250.
[7] DU YQ, WU J, YANG DL. Role of liver sinusoidal endothelial cells in the development and progression of liver fibrosis and related therapeutic strategy[J]. Journal of Clinical Hepatol, 2017, 33(3): 438-444. (in Chinese).
[8] NOVO E, CCANNITO S, MORELLO E, et al. Hepatic myofibroblasts and fibrogenic progression of chronic liver diseases[J]. Histol Histopathol, 2019, 30(9): 1011-1032.
[9] MAJUMDER S, PIGUET AC, DUFOUR JF. Study of the cellular mechanism of sunitinib mediated inactivation of activated hepatic stellate cells and its implications in angiogenesis[J]. Eur J Pharmacol, 2018, 75(1-3): 86-95.
[10] ZHANG S, MA Q, LIANG S, et al. Annual economic burden of hepatitis B virus-related diseases among hospitalized patients in twelve cities in China[J]. J Viral Hepat., 2016, 23(3): 202-210.
[11] FALLOWFIELD J. Macrophage-derived vascular endothelial growth factor and angiogenesis within the hepatic scar-new pathways unmasked in the resolution of fibrosis[J]. Hepatology, 2018, 61(6): 1790-1792.
[12] KISSELEVA T. The origin of fibrogenic myofibroblasts in fibrotic liver[J]. Hepatology. 2017, 65(3): 1039-1043.
[13] VALENTIJN KM, SADLER JE, VALENTIJN JA. Functional architecture of Weibel-Palade bodies[J]. Blood, 2019(117): 5033-5043.
[14] NIGHTINGALE TD. Actomyosin II contractility expels von Willebrand factor from Weibel-Palade bodies during exocytosis[J]. Cell Biol., 2018(194): 613-629.
[15] LI SB, JIA YJ. The interaction between extracellular matrix and stellate cells in liver fibrosis[J]. Progress in Physiological Sciences, 2014, 45(6): 462-464. (in Chinese).
[16] VERHENNE S, DENORME F, LIBBRECHT S, et al. Platelet-derived VWF is not essential for normal thrombosis and hemostasis but fosters ischemic stroke injury in mice[J]. Blood, 2018(126): 1715-1722.
[17] TORISU T. Autophagy regulates endothelial cell processing, maturation and secretion of von Willebrand factor[J]. Nat Med., 2018(19): 1281-1287.
[18] KONG D, ZHANG F, ZHANG Z, et al. Clearance of activated stellate cells for hepatic fibrosis regression: Molecular basis and translational potential[J]. Biomed Pharmacother, 2019, 67(3): 246-250.
[19] URSULA E LEE, SCOTT L. Friedman, mechanisms of hepatic fibrogenesis[J]. Best Practice & Research Clinical Gastroenterology, 2011, 25(2):195-206.
[20] LAI L, CHEN Y, TIAN X, et al. Artesunate alleviates hepatic fibrosis induced by multiple pathogenic factors and inflammation through the inhibition of LPS/TLR4/NF-κB signaling pathway in rats[J]. Eur J Pharmacol, 2018(765): 234-241.
[21] WATANABE A, SOHAIL MA, GOMES DA, et al. Inflammasome-mediated regulation of hepatic stellate cells[J]. Am J Physiol Gastrointest Liver Physiol., 2019, 296(6): G1248-G1257.
[22] ERENT M. Rate, extent and concentration dependence of histamine-evoked Weibel-Palade body exocytosis determined from individual fusion events in human endothelial cells[J]. J Physiol. 2019(583): 195-212.
[23] SCHRODER K, TSCHOPP J. The inflflammasomes[J]. Cell, 2010(140): 821-832.
[24] HAN XF, LI P, YANG ZH, et al. Zyxin regulates endothelial von Willebrand factor secretion by reorganizing actin filaments around exocytic granules[J]. Nature Communication, 2017, 17(7): 1-11.
[25] LI P, WEI G, CAO Y, et al. Myosin IIa is critical for cAMP-mediated endothelial secretion of von Willebrand factor[J]. Blood, 2018, 12(5): 42-51.
[26] LIU M, ZHANG B. Treating liver fibrosis from the perspective of blood stasis[J]. Chinese Journal of Integrated Traditional and Western Medicine on Digestion, 2018, 5(3): 310-314. (in Chinese).
[27] WU Y, JIN X. The research on the relevance between different syndromes of compensatory phase cirrhosis and liver fibrosis target[J]. Journal of Practical Traditional Chinese Internal Medicine, 2017, 31(3): 8-11. (in Chinese).
[28] HE SQ, ZHANG XF, CAI HB. Introduction to professor Lv Zhipings experience in the diagnosis and treatment of chronic hepatitis and liver fibrosis[J]. Journal of New Chinese Medicine, 2005, 37(3): 16-19. (in Chinese).
[29] LIU CH, LIU P, HU YY, et al. Progress of clinical and basic research on liver fibrosis with traditional Chinese medicine[J]. World Science and Technology—Modernization of Traditional Chinese Medicine and Materia Medica, 2007, 9(7): 112-119. (in Chinese).
[30] SONG F, DING XS. The study of the changes of biological superficial signs of blood stasis and hemorheology of hepatic fibrosis rats[J]. Journal of Nanjing University of Traditional Chinese Medicine, 2014, 10(4): 271-274. (in Chinese).
[31] CRESPO YANGUAS S, COGLIATI B, WILLEBRORDS J, et al. Experimental models of liver fibrosis[J]. Arch Toxicol, 2019, 9(5): 1025-1048.
[32] PENG Y, DUAN XL, ZHAO TJ, et al. Constrution of rat model of hepatic fiborsis with blood stasis snydrome integrated with traditional Chinese medicine (TCM) snydrome and western medicine diseases[J]. Animal Husbandry and Feed Science, 2017, 9(2): 101-107.
[33] ZHAO TJ, FU PY, ZHENG Y, et al. Effects of several active ingredients of Rhizoma Curcumae on liver diseases[J]. World Chinese Journal of Digestology, 2017, 25(27): 2433-2440. (in Chinese).
[34] LI J, SHAN CM, ZHAO YD. Exploring the mechanism of action of Sparganium stoloniferum and Curcuma phaeocaulis on liver fibrosis in rats[J]. Shandong Medical Journal, 2012, 37(8): 25-27. (in Chinese).
[35] QIN HZ, LI B, SHI B. Effect of Guangxi Curcuma kwangsiensis on hepatic histopathology of hepatic fibrosis in rat[J]. Chinese Journal of Experimental Traditional Medical Formulae, 2010, 16(7): 130-133. (in Chinese).
[36] TANG ZY, ZONG CG, LIN Y. Experimental study on the activity of curcumenol for promoting blood circulation and resolving blood stasis of zedoary turmeric alcohol[J]. Pharmacology and Clinics of Chinese Materia Medica, 2013, 19(6): 15-18. (in Chinese).
[37] PENG Y, DUAN XL, ZHAO TJ, et al. Effects of aqueous extract of Plumbago zeylanica L. in the revesal of DMN-induce hepatic fiborsis in rat[J]. Agricultural Biotechnology, 2017, 6(5): 64-70.
[38] PENG Y, MIAO WN, ZHAO TJ, et al. Effects of volatile oils of Radix Curcumae on the activity and secretion of hepatic stellate cells[J]. Medicinal Plant, 2015, 6(5-6): 48-54.
[39] LIU XM, LI GY, DENG Y, et al. The effects of Guangxi Curcuma extract to the function of secretory collagen protein and MMPs of human hepatic stellate cell[J]. Lishizhen Medicine and Materia Medica Research, 2013, 34(4): 35-39. (in Chinese).
[40] PENG Y, WU G, ZHAO TJ, et al. Study on the effects of alcohol extract from rhizomes of Curcuma kwangsiensis on proliferation, cell cycle and apoptosis of human hepatic stellate cells[J]. Lishizhen Medicine and Materia Medica Research, 2012, 23(5): 1076-1078. (in Chinese).
[41] DUAN XL, PENG Y, ZHAO TJ, et al. Effect of curcumin against capillarization of hepatic sinusoids and its mechanism[J]. Chinese Journal of Tissue Engineering Research, 2018, 22(8): 1247-1254.
Editor: Yingzhi GUANGProofreader: Xinxiu ZHU
- 农业生物技术(英文版)的其它文章
- Optimization of Extraction Conditions for Total Flavonoids from Fructus Aurantii Immaturus and Its Anti-UVB Radiation Activity
- Research on Maize Seed Classification Method Based on Convolutional Neural Network
- Common Species Distribution Models in Biodiversity Analysis and Their Challenges and Prospects in Application
- Vegetable Tunnel House Technology in Tropical Island Countries
- Purification and Characterization of Hyaluronate Lyases Produced by Two Types of Bacteria
- Renewable Energy Seawater Desalination Technology and Application Analysis