Prevalence and prognosis of acute pancreatitis in critically ill patients with COVID-19
Dongju Kang, Su Ho Park, Changkyo Oh, Yu Jin Kim, Jin Bae Kim, Sang Hoon Park,Myung Seok Lee, Jae Keun Park
Department of Internal Medicine, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul 07441, Korea
Keywords: Acute pancreatitis COVID-19 Coronavirus infections Intensive care unit
ABSTRACT Background: Coronavirus disease 2019 (COVID-19) is a global pandemic issue.In addition to the wellknown respiratory and fever symptoms, gastrointestinal symptoms have also been reported.This study aimed to evaluate the prevalence and prognosis of patients with COVID-19 infection complicated with acute pancreatitis in intensive care unit (ICU).Methods: This was a retrospective observational cohort study, and patients aged 18 years or older, admitted into the ICU in a single tertiary center from January 1, 2020, to April 30, 2022 were enrolled.Patients were identified by electronic medical records and reviewed manually.The primary outcome was the prevalence of acute pancreatitis among ICU patients with COVID-19.The secondary outcomes were the length of hospital stay, need for mechanical ventilation (MV), need for continuous renal replacement therapy (CRRT), and in-hospital mortality.Results: A total of 4133 patients, admitted into the ICU, were screened.Among these patients, 389 were infected by COVID-19, and 86 were diagnosed with acute pancreatitis.COVID-19 positive patients were more likely to present with acute pancreatitis than COVID-19 negative patients (odds ratio = 5.42, 95%confidence interval: 2.35-6.58, P < 0.01).However, the length of hospital stay, need for MV, need for CRRT, and in-hospital mortality were not significantly different between acute pancreatitis patients with and without COVID-19 infection.Conclusions: Severe COVID-19 infections may cause acute pancreas damage in critically ill patients.However, the prognosis may not differ between acute pancreatitis patients with and without COVID-19 infection.
Introduction
The global spread of coronavirus disease 2019 (COVID-19) has been mostly associated with respiratory symptoms.However, previous studies reported that up to 25% of COVID-19 patients also suffered from gastrointestinal symptoms [1-3].Abnormal gastrointestinal symptoms can be caused by multiple organ damage, including the pancreas, due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [4].The exact mechanism has not been elucidated, but one explanation is that SARS-CoV-2 may bind to pancreatic islet cells, which contain angiotensin-converting enzyme 2 (ACE2) receptor proteins, and cause damage.Several studies have reported that clinical cases support these possible explanations [5-7].A previous study reported the prevalence, risk factors, and outcomes of patients with COVID-19 infection presenting as acute pancreatitis [7].These findings support that acute pancreatitis could be included in the list of gastrointestinal manifestations of COVID-19 infection.However, the clinical course and outcome among patients with acute pancreatitis and COVID-19 have not yet been clearly determined due to the rarity of the disease.A study reported that patients presenting with acute pancreatitis and COVID-19 on admission had a more benign clinical course and overall better outcomes compared with COVID-19 patients who developed acute pancreatitis during hospitalization [8].Furthermore,the intensive care unit (ICU) admission rate was not significantly different between COVID-19 patients with and without acute pancreatitis in a previous meta-analysis study [9].
Previous reports have shown elevated levels of pancreatic enzymes in COVID-19 patients in ICU [10-12].However, those studies did not review the clinical data, including abdominal imaging of the enrolled patients, for assessing pancreatitis and treatment.This study aimed to evaluate the prevalence and prognosis of COVID-19 patients presenting with acute pancreatitis, especially in critically ill patients requiring ICU admission, by reviewing both clinical data and treatment protocols.
Materials and methods
Study population and data collection
A total of 4133 patients, admitted into the ICU from January 1, 2020 to April 30, 2022 at the Kangnam Sacred Heart Hospital(Seoul, Korea) were analyzed.All patients met two out of three of the following revised Atlanta classification criteria for acute pancreatitis [13]: i) a lipase rise greater than three times the upper limit of normal, ii) evidence of pancreatitis on computed tomography imaging, iii) characteristic upper abdominal pain.The quick sepsis-related organ failure assessment (qSOFA) was utilized to evaluate the severity of the patients [14].The qSOFA criteria were defined as follows: i) altered mental status, ii) a respiratory rate ≥22 per min, and iii) a systolic blood pressure ≤100 mmHg.
The primary outcome was the prevalence of acute pancreatitis among critically ill patients presenting with COVID-19; the secondary outcomes were the length of hospital stay, need for mechanical ventilation (MV), need for continuous renal replacement therapy (CRRT), and in-hospital mortality.We compared the prognosis of acute pancreatitis patients with and without COVID-19 infection.This study was conducted in accordance with theDeclarationofHelsinkiand approved by the institutional review board of Kangnam Sacred Heart Hospital, Seoul, Korea (No.2022-06-008-001).
Statistical analysis
All statistical analyses were performed using the SPSS Statistics version 23 (IBM, Chicago, IL, USA).Categorical data are expressed as count and proportion, while continuous data are expressed as mean and standard deviation.Fisher’s exact test and Student’st-test were used to identify significant differences between clinical variables.The Kaplan-Meier survival curve was used to compare the survival probability.AP<0.05 was considered statistically significant.
Results
Baseline characteristics of the study population
A total of 4133 patients admitted into the ICU were included in this study, of which 389 (9.4%) were COVID-19 positive on admission.The mean age was 68.5 ± 15.5 years in the COVID-19 negative group, and 69.6 ± 15.4 years in the COVID-19 positive group(P= 0.172).Sex, underlying comorbidities, and qSOFA score did not show any significant difference between the two groups (allP>0.05) at the initial ICU admission.The basic clinical characteristics of the study population are listed in Table 1.Among the 389 patients with COVID-19 infection, 31 presented with acute pancreatitis.In the non-COVID-19-infected patients, 55 presented with acute pancreatitis ( Fig.1 ).
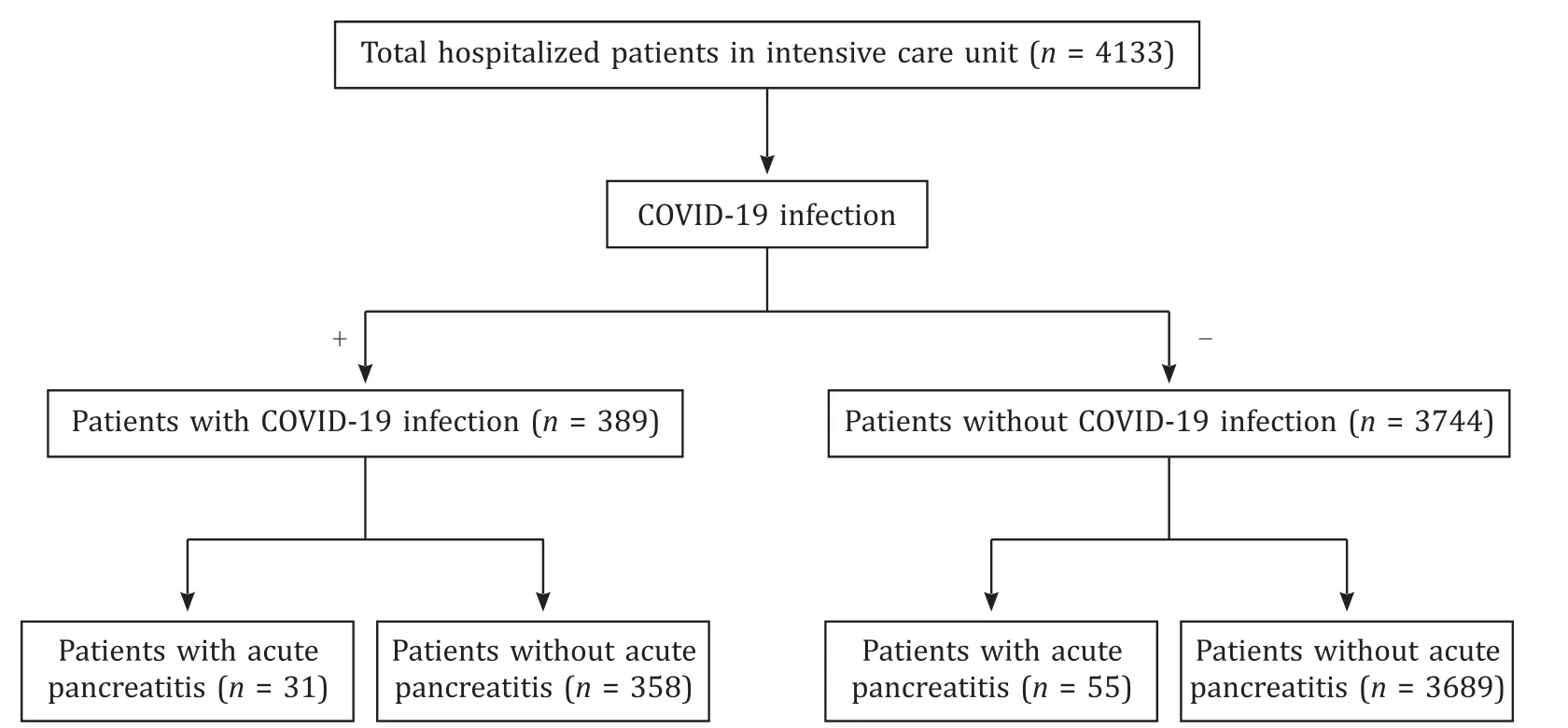
Fig.1.Flow chart of procedures in enrolled patients.COVID-19: coronavirus disease 2019.

Table 1Baseline characteristics of enrolled ICU patients.
Prevalence and prognosis of the study population
The acute pancreatitis patients with and without COVID-19 infection are shown in Table 2.We classified the etiologies of acute pancreatitis into five categories: gallstone, alcohol, hypertriglyceridemia, post-endoscopic retrograde cholangiopancreatography (ERCP), and idiopathic.The incidence of etiology and qSOFA score were not significantly different between the two groups.The average length of hospital stay (20.6 vs.18.7 days), need for MV(10.9% vs.12.9%), need for CRRT (16.4% vs.16.1%), in-hospital mortality (9.1% vs.12.9%), and Kaplan-Meier survival curve for a 50-day follow-up period were also not significantly different between the two groups (allP>0.05) ( Table 2 and Fig.2 ).

Fig.2.Comparison of Kaplan-Meier survival curves for a 50-day follow-up period between critically ill patients with acute pancreatitis, with and without COVID-19 infection.COVID-19: coronavirus disease 2019.

Table 2Comparisons of acute pancreatitis with or without COVID-19 infection.
The prevalence of acute pancreatitis was significantly higher in the COVID-19-infected patients than in the non-COVID-19-infected patients (odds ratio = 5.42, 95% confidence interval: 2.35-6.58,P<0.01).
Discussion
In this study of critically ill patients admitted to the ICU, the prevalence of acute pancreatitis in COVID-19-infected patients was significantly higher than that in non-COVID-19-infected patients.However, there were no significant differences in the treatment outcomes, including the total hospital stay, and the need for MV and CRRT.Finally, there was no significant difference in the cumulative survival rate during a 50-day follow-up period.Our findings support that acute pancreatitis is one of the possible gastrointestinal manifestations of COVID-19 infection in critically ill patients requiring ICU admission.This was similar to findings reported by Inamdar et al.[7].However, the prognosis of these patients did not change significantly.
Previous studies reported acute pancreatitis as an initial clinical presentation of COVID-19 infection [ 5-7 , 15 ].However, acute pancreatitis caused by viral infection is very rare.A study revealed that hepatotropic virus, coxsackie virus, cytomegalovirus,human immunodeficiency virus, herpes simplex virus, mumps,varicella-zoster virus, and other viruses could be possible causes of infectious acute pancreatitis [16].Several explainable hypotheses were noted, including the virus binding to ACE2 receptor proteins [4]and diffuse micro ischemic damage to the pancreas [17].However, evidence to conclude the viral infection caused acute pancreatitis is lacking.Nevertheless, several case reports have revealed the relationship between COVID-19 infection and acute pancreatitis [ 11 , 18 ].Furthermore, SARS-CoV-2 has been isolated from pancreatic pseudocyst specimens from a patient with acute pancreatitis [19].
The etiologies of acute pancreatitis are difficult to distinguish clearly and sometimes it is difficult or impossible to explain with one factor.Inamdar et al.[7]and Kumar et al.[8]have also noted the difficult nature of etiology studies.In this study, the most common etiology of acute pancreatitis was alcohol consumption, and the second was gallstones.If gallstones were present without a history of smoking and alcohol, it was diagnosed as pancreatitis caused by gallstones.Interestingly, there were no patients with post-ERCP pancreatitis in our study since the ERCP facility could not be performed during the COVID-19 outbreak.In gallstone pancreatitis with cholangitis cases, a percutaneous cholecystostomy was initially performed with percutaneous transhepatic gallbladder drainage.Only one (3.2%) and two (3.6%) patients were classified as having an idiopathic etiology of acute pancreatitis, in COVID-19-infected and non-COVID-19-infected groups, respectively.
Although our data show no significant difference in the cumulative survival rate, there are several trends worth noting.Firstly,there was a tendency towards a shorter hospital stay in acute pancreatitis patients with COVID-19 infection than without COVID-19 infection.Kumar et al.[8]reported that COVID-19 patients with acute pancreatitis on admission had a better clinical outcome when compared to COVID-19 patients who developed acute pancreatitis during hospitalization.Our study focused on COVID-19 patients with acute pancreatitis on admission.Secondly, the number of patients who required MV showed an increasing trend in the acute pancreatitis with COVID-19-infected patients comparedto those without COVID-19-infected patients.It is speculated that the occurrence of acute pancreatitis in COVID-19-infected patients may be associated with the worsening of respiratory symptoms,but evidence is lacking.Thirdly, in-hospital mortality also showed an increasing trend in acute pancreatitis with COVID-19-infected patients compared to those without COVID-19-infected patients.
Our study has several limitations, including only a single-center retrospective cohort study.Also, the number of patients with acute pancreatitis and COVID-19 was relatively small.Since the study population was critically ill patients admitted to the ICU, results cannot be generalized to acute pancreatitis and COVID-19 patients with mild symptoms.For excluding the five causes of acute pancreatitis (gallstones, alcohol, hypertriglyceride, post-ERCP, and idiopathic), and taking into account other causes such as drug-induced,inherited and autoimmune related causes, the review of the clinical data was limited due to the special situation in the ICU.Finally, we used the qSOFA as a predicting value of the severity in the enrolled patients.Although qSOFA has been validated for patient evaluation in critically ill patients, as recommended in the sepsis-3 guidelines [ 14 , 20 , 21 ], qSOFA has not been universally applied in patients with acute pancreatitis to evaluate the severity.Future studies are required to evaluate the adequacy of the patient severity scoring system.
This study has important implications.Firstly, to our knowledge,this is the first report to observe the disease progress of critically ill patients with acute pancreatitis and COVID-19 infection.Secondly, this is also the largest report to follow up on critically ill patients admitted to the ICU.
In conclusion, severe SARS-CoV-2 infection may cause acute pancreas damage, especially in critically ill patients.However, patient prognosis may not differ between acute pancreatitis patients with and without COVID-19 infection.Future worldwide large-scale studies are required to strengthen our findings and determine whether the treatment of acute pancreatitis should vary depending on whether patients have a COVID-19 infection.
Acknowledgments
None.
CRediTauthorshipcontributionstatement
Dongju Kang:Conceptualization, Data curation, Writing - original draft.Su Ho Park:Data curation.Changkyo Oh:Investigation, Methodology, Validation.Yu Jin Kim:Investigation, Methodology, Validation.Jin Bae Kim:Investigation, Methodology, Validation.Sang Hoon Park:Investigation, Methodology, Validation.Myung Seok Lee:Investigation, Methodology, Validation.Jae Keun Park:Conceptualization, Supervision, Writing - review & editing.
Funding
None.
Ethical approval
This study was conducted in accordance with theDeclarationof Helsinkiand approved by the institutional review board of Kangnam Sacred Heart Hospital, Seoul, Korea (No.2022-06-0 08-0 01).
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2023年4期
Hepatobiliary & Pancreatic Diseases International2023年4期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Novel re-intervention device for occluded multiple uncovered self-expandable metal stent (with video)
- Hepatopancreatoduodenectomy for the treatment of extrahepatic cholangiocarcinoma ✩
- Microbiological cultures and antimicrobial prophylaxis in patients undergoing total pancreatectomy with islet cell autotransplantation
- Risk factors for posttransplant diabetes in patients with hepatocellular carcinoma
- The role of targeting protein for Xklp2 in tumorigenesis of hepatocellular carcinoma
- Isolated IgG4-associated autoimmune hepatitis or the first manifestation of IgG4-related disease?
