Hepatopancreatoduodenectomy for the treatment of extrahepatic cholangiocarcinoma ✩
Alerto Poru , Giuli Dein , Cludio F Feo , Chir Ninniri , Dvide Turilli ,Loren Tnd , Alessndro Fnellu ,
a Department of Clinical, Surgical and Experimental Sciences, Unit of General Surgery 2 - Clinica Chirurgica, University of Sassari, Sassari, Italy
b Unit of Radiological Sciences, AOU Sassari, Sassari, Italy
c Faculty of Medicine and Surgery, University of Sassari, Sassari, Italy
TotheEditor:
Extrahepatic cholangiocarcinoma (ECC) is an uncommon neoplasm associated with a poor prognosis [1-3].Surgical resection represents the only curative approach, since systemic treatments have scarce efficacy in achieving disease control.However, only 10%-40% of patients with ECC are resectable at diagnosis [1].Major hepatectomy and portal lymphadenectomy are usually required for hilar ECC, while pancreatoduodenectomy is the standard operation for distal ECC [3-5].However, ECC may spread horizontally along the biliary tree, causing tumor involvement of the entire extrahepatic biliary system.In these circumstances, hepatopancreatoduodenectomy (HPD) has been proposed as a procedure with curative intent [ 2 , 6 , 7 ].HPD is a complex operation which includes the combination of hepatic resection, pancreatoduodenectomy and extirpation of the extrahepatic biliary system.It has been generally considered a controversial operation, due to the high mortality and morbidity rates in front of uncertain oncological outcomes [ 5 , 7-9 ].However, in the last 5 years, encouraging survival outcomes, as well as acceptable mortality and morbidity rates, have been reported from surgical teams with high expertise in hepatobiliopancreatic (HBP) surgery [ 2, 10, 11].Most literature data focusing on HPD are from Asian institutions, where HPD has been gaining some popularity in the treatment of selected patients with ECC and gallbladder cancer.On the opposite, few reports came from Western countries, where HPD has not been considered a worthwhile, albeit feasible, procedure.
We herein describe a single-institution experience with HPD.In the period of 2010-2020, among 51 patients operated on for ECC(excluding gallbladder cancer), 6 received an HPD.One of the cases is depicted in Fig.1.Demographic and clinicopathological characteristics were resumed in Table 1.All patients were male, with a median age of 68 years.The median Charlson Comorbidity Index score was 4 score.Five patients received preoperative biliary drainage for obstructive jaundice.Portal vein embolization was applied in one patient having an estimated future remnant liver of less than 40% (evaluated at liver computed tomography volumetry).All patients had a preoperative diagnosis of ECC, based on clinical and radiological workup.In all cases, the planned operation was a hepatectomy associated to portal lymphadenectomy.The decision to perform an HPD was taken intraoperatively, due to the infiltration of distal common bile duct at frozen section.In all six patients, three or more hepatic segments were removed (major hepatic resection).Preoperative and postoperative liver function test were resumed in Table 2.

Table 1Demographic and clinicopathological characteristics of patients in this study( n = 6).

Table 2Preoperative and postoperative liver function test.

Fig.1.Extrahepatic cholangiocarcinoma in a 68-year-old man who presented with weight loss and obstructive jaundice.MRCP image showed a long stricture extended from the hepatic hilum to the distal common bile duct (yellow arrow), involving both right (green arrow) and left (green arrow) ducts, with secondary marked retrograde upstream dilation of the biliary tree.A small cystic lesion in the pancreatic head (red arrowhead) and a focal cystic dilatation of cystic duct (green arrowhead) were also present ( A ).Axial contrast-enhanced MRI demonstrated biliary ectasia (arrowhead) due to a hypovascular intraductal mass (arrow) located in extrahepatic biliary tract ( B ).Preoperative imaging was consistent with an extrahepatic cholangiocarcinoma of Bismuth-Corlette type IV.Preoperative biliary drainage was applied to relieve the obstruction.HPD comprising left hepatectomy enlarged to segment I was carried out in May 2018.Postoperative course was uneventful, and the patient was discharged at postoperative day 12.After 42 months, the patient is doing well, in stable health condition.MRCP: magnetic resonance cholangiopancreatography; HPD: hepatopancreatoduodenectomy; MRI:magnetic resonance imaging.
In 2 cases, a vascular resection/reconstruction was necessary:in one case a portal resection with direct end-to-end reconstruction; in the other case a resection of the right hepatic artery was made, that was anastomosed with the left hepatic artery.The median surgery duration was 412 minutes.Four patients (4/6) developed postoperative complication, and one required re-laparotomy for treatment of postoperative hemorrhage ( Table 3 ).Perioperative mortality occurred in 2 patients.One patient died of sepsis at postoperative day 19; the second patient died at postoperative day 28 for liver failure, after a reoperation for hemorrhage.Excluding 30-day mortality, median follow-up duration was 21 months, with a median survival of 24 months.Two patients died of disease progression after 19 and 24 months from the operation, respectively.Two patients were alive and in good shape after 24 months and 42 months from the operation, respectively ( Table 3 ).
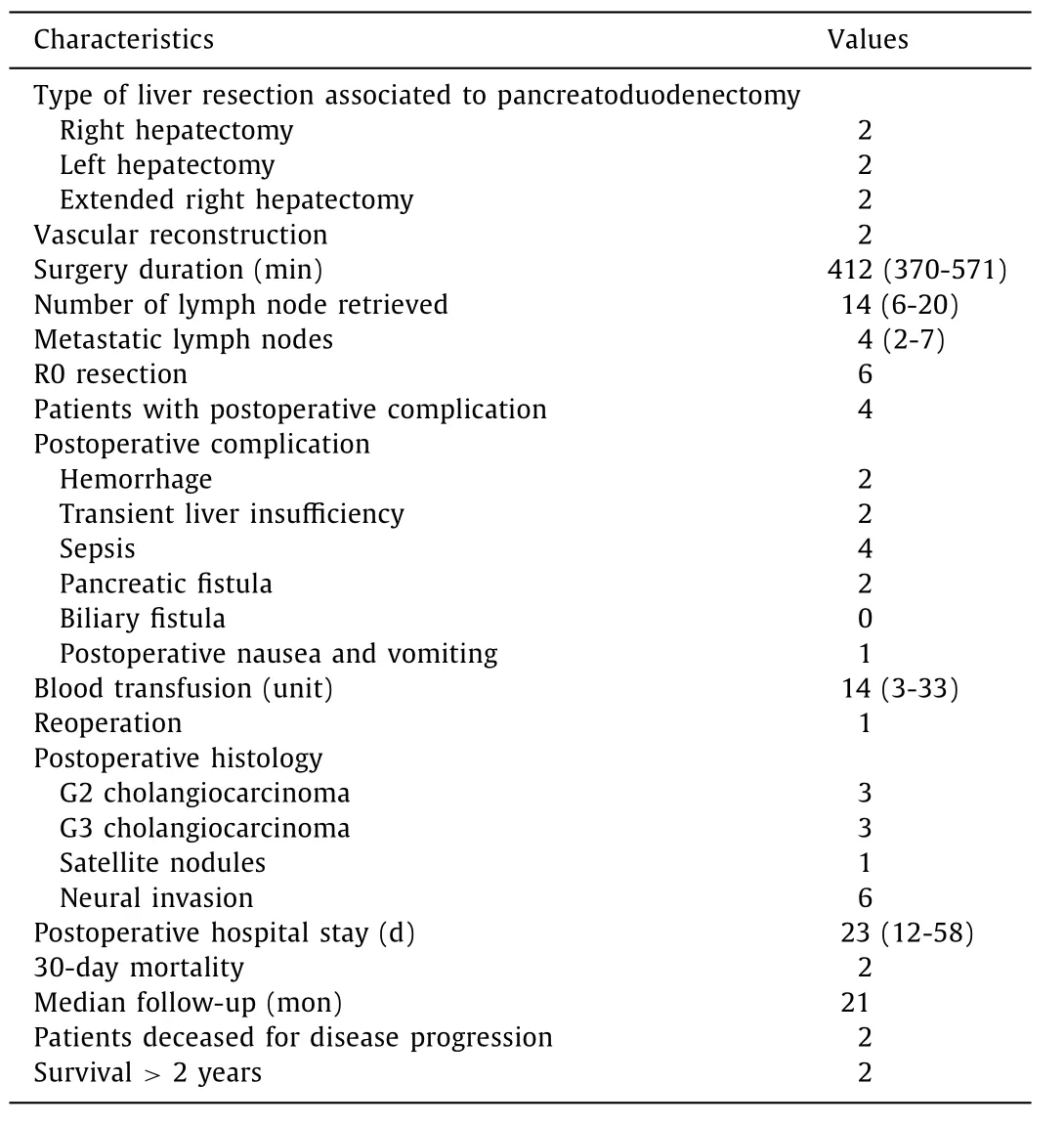
Table 3Operative and postoperative data and outcomes ( n = 6).
HPD is a complex surgical procedure that can be used with curative intent in patients with ECC extending from the hilar bile duct down to distal common bile duct.However, its development has been hindered by high morbidity and mortality rates, since that procedure bears risk for complications of concurrent pancreatoduodenectomy and hepatic resection.In addition, skepticism in the acceptance of HPD has resulted from uncertain oncological benefits [ 2 , 7 ].Nonetheless, recent reports on the use of HPD underscored that acceptable morbidity rates can be obtained in centers with high expertise in HBP surgery, and also that encouraging survival outcomes are achievable in selected patients [ 2 , 11 ].
HPD has been introduced in the 1980s in Japan, where the operation is currently deemed as a curative option for widespreading bile duct cancer [12].However, HPD have been rarely
reported from outside Asian countries.In particular, some reports
form American and European institutions showed discouraging re
sults [ 5 , 8 , 13 ].Nonetheless, it should be recognized that the liter
ature on this topic is sometimes difficult to interpret, due to het
erogeneity of indications and procedures, since HPD has been performed also for conditions different from ECC, including metastases and benign diseases.Moreover, HPD in some instances consisted of pancreatoduodenectomy associated to limited liver resection involving one Coineaud segment or less [ 8 , 13 , 14 ], rather than a genuine HPD.We are reporting our experience exclusively on the use of HPD for ECC (excluding gallbladder cancer), where pancreatoduodenectomy and complete removal of the entire extrahepatic biliary system were associated with an hepatectomy comprising at least three to six hepatic segments in all cases.To note, major complications occurred in 4 out of 6 patients of the present series.This finding is in line with previous reports.In a review including the most recent experiences on HPD (2015-2020), morbidity rates after HPD ranged between 37.0% and 87.5% [2].These figures can beexplained by the fact that HPD bears the potential risks and complications of both hepatectomy and pancreatoduodenectomy.A primary concern after pancreatic surgery is the occurrence of pancreatic fistula [5].Postoperative pancreatic fistulas can result in intraabdominal hemorrhage and formation of abscesses, and are associated with increased mortality rates in patients undergoing pancreatoduodenectomy [ 15 , 16 ].In our experience, in two cases we observed a pancreatic fistula that was resolved with conservative treatment.We observed hepatic failure in three cases, although in two cases it was a transient condition that was resolved at postoperative day 15.It is likely that indications and patient selection for extended liver resection should be more restrictive than usual in patient candidates to HPD.In this regard, it should be noted that in all the cases described herein, the decision to perform an HPD was taken intraoperatively in patients originally candidates to hepatectomy alone, due to the infiltration of the distal margin of the common bile duct at frozen section examination.This fact might partially explain the high rates of morbidity and mortality observed.However, the precise extent of bile duct involvement is not always possible with preoperative radiologic workup, due to the particular infiltration pattern of ECC.
Although the lymph node metastasis classification differs across guidelines and staging systems, lymphadenectomy plays a fundamental role in patients with ECC, since lymph node metastasis is present in 30%-60% of resectable ECC [ 1 , 10 , 17 ].Lymph node status is one of the most important factors affecting the prognosis, and guiding adjuvant treatments after R0 liver resection.In a study including 146 patients who underwent curative-intent resection of hilar cholangiocarcinoma with regional lymphadenectomy, the 5-year survival rate of N0 patients with lymph node micrometastasis was significantly lower than those without micrometastasis (P= 0.01), and not significantly different to N1 patients(P= 0.54) [18].
Vascular resection/reconstruction was performed in two patients of the series reported herein, in order to achieve an R0 resection.Reconstruction of the portal vein, or hepatic artery, or both is required in 20%-30% of cases during HPD [ 19 , 20 ].Mortality rates of HPD historically has remained high when compared to other major gastrointestinal surgeries, and range between 14% and 50% [14].However, mortality of HPD has remarkably reduced in the last decade, especially in Japanese institutions, where mortality rates were below 5%.It is worthy to mention that Aoki et al.observed no mortality in the first 90 days among 52 patients who underwent HPD for biliary cancer [11].To note, two patients of our case series are alive and disease-free after more than two years after HPD.Although we registered high mortality and morbidity rates in this short case series, we believe that those survival outcomes are worthy of attention.In this regard, we would like to point out that survival of patients with ECC who underwent HPD should be compared to the survival of patients who did not undergo surgery, who experience a survival of few months.We acknowledge that this study has limitations, such as retrospective nature and the small sample size.However, it should be noted that articles reporting on HPD specifically for ECC are scarce in recent literature, reflecting the controversial use of this extended surgical approach.For example, a recent multicenter study from Europe included only 66 patients from 19 countries in a long-time frame(2003-2018) [5].Despite these important limitations, to the best of our knowledge, our experience represents the first single-center report on the use of HPD for ECC from an Italian institution, and one of the few from Europe.
Evidence is emerging that HPD, albeit its complexity and invasive essence, may provide acceptable oncological outcomes in selected patients with wide-spread ECC [ 2 , 21 ].Data from our experience, although based on a small sample size, support this trend.We believe that this case-series accumulated the cases on the application of HPD in surgical practice.Standardization of both surgical technique and selection criteria, national-based databases, and centralization of cases in centers with high experience, are the keys to identify patients with ECC who may benefit from HPD.
Acknowledgments
None.
CRediT authorship contribution statement
Alberto Porcu:Conceptualization, Data curation, Writing - review & editing.Giulia Deiana:Data curation, Resources.Claudio F Feo:Investigation, Methodology.Chiara Ninniri:Investigation,Methodology.Davide Turilli:Data curation, Methodology.Lorena Tanda:Investigation, Methodology, Visualization.Alessandro Fancellu:Conceptualization, Funding acquisition, Methodology, Writing - original draft.
Funding
This work was supported by the FAR19 grant of the University of Sassari, Italy.
Ethical approval
This retrospective study was approved by the Institutional Review Board of the Department of Clinical, Surgical and Experimental Sciences of University of Sassari.All patients signed an informed consent for all diagnostic and surgical procedures.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2023年4期
Hepatobiliary & Pancreatic Diseases International2023年4期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Novel re-intervention device for occluded multiple uncovered self-expandable metal stent (with video)
- Microbiological cultures and antimicrobial prophylaxis in patients undergoing total pancreatectomy with islet cell autotransplantation
- Risk factors for posttransplant diabetes in patients with hepatocellular carcinoma
- The role of targeting protein for Xklp2 in tumorigenesis of hepatocellular carcinoma
- Isolated IgG4-associated autoimmune hepatitis or the first manifestation of IgG4-related disease?
- Left abdominal mass with carcinosis: Unusual presentation of pancreatic acinar cell carcinoma
