Long-term outcomes of endoscopic papillary large-balloon dilation(12-15 mm) with or without limited sphincterotomy for removal of bile duct stones
Tao Li , Li-Xiao Hao , Chan Lv , Xing-JiLi , Xiao-Dan Ji , Meng Chen , Chang Liu ,Li-Ke Bie , Biao Gong , *
a Department of Gastroenterology, Shuguang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
b Department of Gastroenterology, Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai 20 0 025, China
Keywords:Endoscopic papillary large-balloon dilation Endoscopic sphincterotomy Bile duct stone
ABSTRACT Background: Limited endoscopic sphincterotomy with large balloon dilation (ES-LBD) and endoscopic papillary large-balloon dilation (EPLBD) have been proven safe and effective for removal of bile duct stones.However, the long-term outcomes are not clear.The aim of this study was to assess the longterm outcomes of EPLBD (12-15 mm) with or without limited sphincterotomy for removal of common bile duct (CBD) stones.Methods: Patients with EPLBD or ES-LBD referred for the removal of bile-duct stones between June 2008 and August 2020 were retrospectively reviewed.Complete stone clearance, endoscopic retrograde cholangiopancreatography (ERCP)-related adverse events, and late biliary complications during long-term follow-up were analyzed.Results: Basic patient characteristics were not significantly different between the groups that underwent EPLBD ( n = 168) and ES-LBD ( n = 57).EPLBD compared with ES-LBD resulted in similar outcomes in terms of overall successful stone removal (99.4% vs.100%, P = 1.00) and ERCP-related adverse events(7.7% vs.5.3%, P = 0.77).The mean duration of the follow-up were 113.6 months and 106.7 months for patients with EPLBD and ES-LBD, respectively ( P = 0.13).There was no significant difference between EPLBD and ES-LBD in the incidence of stone recurrence [20 (11.9%) vs.9 (15.8%); P = 0.49].Multivariate analysis showed that a diameter of CBD ≥15 mm (OR = 3.001; 95% CI: 1.357-6.640; P = 0.007) was an independent risk factor for stone recurrence.Conclusions: The application of a large balloon (12-15 mm) via EPLBD is an effective and safe alternative to ES-LBD for extraction of large CBD stones.Endoscopic sphincterotomy prior to EPLBD may be unnecessary.A diameter of CBD ≥15 mm is a risk factor of stone recurrence.
Introduction
Endoscopic papillary balloon dilation (EPBD) is an alternative to endoscopic sphincterotomy (EST) for the removal of common bile duct (CBD) stones [ 1 , 2 ], and it is associated with lower frequencies of hemorrhage and preserves the function of Oddi’s sphincter compared with EST.However, large stones appear to be more difficult to remove when using EPBD, because the biliary orifice is limited by the diameter of the balloon.To overcome this disadvantage, the technique of endoscopic papillary large balloon dilatation (EPLBD) using a balloon larger than 12 mm was introduced for the treatment of difficult CBD stones [3].Recent studies have shown that EPLBD alone produced satisfactory results with respect to the efficacy of stone clearance and has an acceptable complication rate [4-6].Several studies also demonstrated that EPLBD combined with simple EST (ES-LBD) is safe and effective for the removal of large or difficult CBD stones [7-9].However, there is no consensus yet on the long-term efficacy and safety of EPLBD (12-15 mm) with or without limited sphincterotomy for the treatment of CBD stones.The present study aimed to assess long-term outcomes of ES-LBD compared with EPLBD alone for the removal of bile duct stones.
Methods
Patients
A longitudinal cohort study was implemented based on the medical data recorded in a prospectively maintained registry of patients who underwent EPLBD (12-15 mm) with or without limited sphincterotomy for the extraction of bile duct stones between June 2008 and August 2020 at two centers (Digestive Endoscopy Center of Ruijin Hospital and Shuguang Hospital, Shanghai, China).Patients were retrospectively selected based on the following criteria: (1) age ≥18 years, (2) CBD stones visualized during endoscopic retrograde cholangiopancreatography (ERCP), (3) difficult CBD stones ( ≥10 mm or ≥3 stones), (4) a naive major duodenal papilla status, and (5) the diameter of EPLBD of 12-15 mm.The exclusion criteria were: (1) prior history of EST, (2) concomitant intrahepatic stones or pancreaticobiliary malignancies, or (3)distal CBD with stricture.Patients were divided into two groups based on the methods of ampullary widening for the removal of bile duct stones: EPLBD group (n= 168) and ES-LBD group(n= 57).Patients’ baseline characteristics, laboratory and imaging results, ERCP operative details, and related adverse events after ERCP were collected and analyzed.The study was approved by the Ethics Committee of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine and Ruijin Hospital, Shanghai Jiao Tong University School of Medicine.
ERCP procedures
Written informed consent for the ERCP procedures was obtained from all patients.All ERCP procedures were carried out by experienced endoscopists with a standard side-viewing endoscope(TJF-240, JF-260, TJF-260, Olympus Optical, Tokyo, Japan).After selective bile duct cannulation, a diagnostic cholangiogram was performed to assess the diameter of the CBD, the size and number of stones.Either EPLBD alone or ES-LBD and the size of the balloon were chosen by the discretion of the endoscopists to facilitate difficult stone removal ( Fig.1 ).The choice of methods depended on the preference of the endoscopist in most cases.In addition, we preferred EPLBD to ES-LBD in the following cases: (1)patients with surgically altered anatomy (Billroth II or Roux-en-Y anatomy) and (2) anticoagulation therapy within 72 h.The stones were extracted by using a retrieval basket, balloon catheters, or even with mechanical lithotripsy.After complete stone removal,an occlusion cholangiogram was obtained at the end of the procedure.A naso-biliary drain (NBD) was routinely placed to prevent the postoperative infection and perform a repeat cholangiography to check the area if needed ( Fig.2 ).However, it can be difficult to extract in cases of very large stones ( ≥20 mm) or multiple stones where there is little space to manipulate.According to the guidelines [10]on the management of difficult CBD stones, endoscopic biliary stenting (EBS) was replaced at intervals of 3-6 months to prevent cholangitis.

Fig.1.A, B and C : Limited endoscopic sphincterotomy with endoscopic papillary large-balloon dilation was performed; D and E : stones were extracted using a retrieval basket; F : endoscopic papillary large-balloon dilation alone was performed.

Fig.2.A and B : Large balloon inflated across the guidewire within the bile duct; C : endoscopic naso-biliary drainage was inserted.
Evaluation of clinical and ERCP data
The CBD diameter, stone size and number were assessed using an initial diagnostic cholangiogram during ERCP.Complete stone clearance was defined as the absence of filling defects on the occlusion cholangiogram.Furthermore, for the patients with multiple CBD stones or using mechanical lithotripsy, we often performed repeated naso-biliary cholangiography to evaluate whether the stones were completely cleared before discharge.The overall success rate was defined as the rate of complete CBD stone retrieval irrespective of the use of mechanical lithotripsy or the number of ERCP sessions.Post-ERCP complications were sorted and graded according to the consensus guidelines [ 11 , 12 ].Late biliary complications occurring at least 90 days after complete stone removal were classified by clinical symptoms, related laboratory data and imaging findings.
Follow-up
All the patients were followed up after complete stone removal.Our follow-up was mainly based on telephone calls in combination with face-to-face interviews.During the follow-up, a blood sample for liver function tests were scheduled at every 6 months and the abdominal ultrasonography was checked at least once yearly after the removal of CBD stones.The last follow-up was done in May 2021.If clinical symptoms occurred indicative of biliary complications, such as stone recurrence and cholangitis, laboratory tests(blood routine, bilirubin, liver enzymes) and imaging modalities and/or ERCP were adopted to confirm them.Stone recurrence was defined as a newly detected CBD stone by cholangiography at least 90 days after complete stone removal [13].
Statistical analysis
Statistical analyses were performed with the IBM SPSS Statistics(IBM Corp., Armonk, New York, USA).Continuous variables were analyzed by Student’st-test.Categorical variables were tested using Chi-square test or Fisher’s exact test.To evaluate the related risk factors, potential risk factors were initially assessed by univariate analysis.The predictive risk factors with aPvalue<0.1 in univariate analysis were then included in multivariate logistic regression analysis.Pvalues of<0.05 were defined as statistically significant.The cumulative incidence of stone recurrence during the follow-up was estimated by the Kaplan-Meier method.The log-rank test was used to assess the differences between the two groups.
Results
Patients
During the inclusion period a total of 225 patients referred to EPLBD alone (n= 168) and ES-LBD (n= 57) for CBD stone clearance in our center were reviewed.The baseline characteristics of these patients are summarized in Table 1.There was no statistically significant difference in basic characteristics between the EPLBD and ES-LBD groups.Seventy-one patients from the EPLBD group and 28 from the ES-LBD group had previous cholecystectomies (42.3% vs.49.1%,P= 0.44).Fourteen out of 49 patients with gallbladder stones in the EPLBD group had cholecystectomy within 1 month after EPLBD and 6 of 19 patients with gallbladder stone in the ES-LBD group had cholecystectomy after ES-LBD.No significant difference was found in the gallbladder status between the two groups.
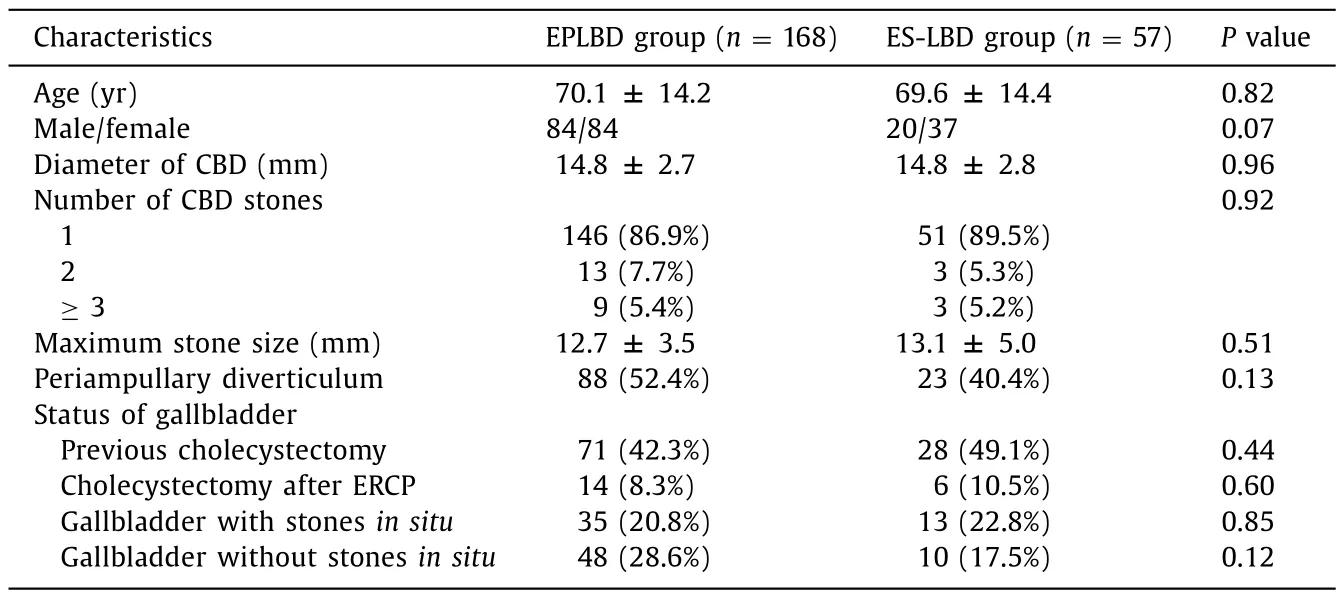
Table 1Baseline characteristics of the study patients who underwent EPLBD alone ( n = 168) and ES-LBD ( n = 57).
ERCP procedure
The details of EPLBD alone and ES-LBD for extraction of CBD stones were presented in Table 2.The CBD stone clearance was accomplished in 99.4% (167/168) of patients in the EPLBD group and 100% (57/57) in the ES-LBD group, and no significant difference was observed between the two groups (P= 1.00).Complete removal of CBD stones was achieved in one session for 98.2% (165/167) and 96.5% (55/57) of patients, two sessions for 1.2% (2/167) and 3.5% (2/57) of patients in the EPLBD and ES-LBD groups, respectively (P= 0.27).There was no significant difference between the EPLBD and ES-LBD groups in the mean size of the balloon (12.7 ± 1.2 vs.12.6 ± 1.2 mm,P= 0.79).Additional mechanical lithotripsy (ML) was required in 17.3% (29/168) of the EPLBDVariables EPLBD group (n= 168) ES-LBD group (n= 57)Pvaluegroup and 19.3% (11/57) in the ES-LBD group (P= 0.69).No significant difference was observed in the mean length of hospital stay between the two groups (7.7 ± 3.3 vs.7.8 ± 4.6 d,P= 0.83).
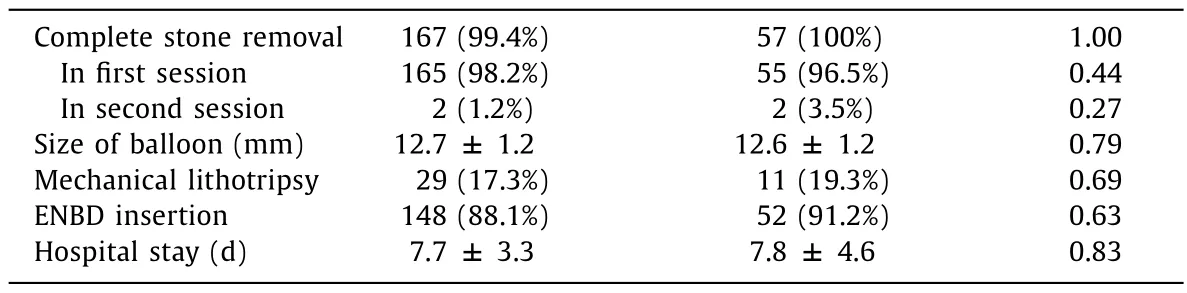
Table 2Comparison of procedural details between the EPLBD and ES-LBD groups.
ERCP-related complications
With respect to ERCP-related complications, the incidence of post-ERCP pancreatitis (4.8% vs.1.8%), hemorrhage (0.6% vs.0),and cholangitis (2.4% vs.3.5%) was not significantly different between the EPLBD and ES-LBD groups ( Table 3 ).All the patients with post-ERCP pancreatitis and cholangitis improved with conservative management.Post-ERCP bleeding was found in one patient in the EPLBD group, but no blood transfusion was required and bleeding was controlled with placement of a biliary covered metal stent.There were no severe complications or mortality related ERCP.The overall adverse events showed no significant difference between the EPLBD and ES-LBD groups.
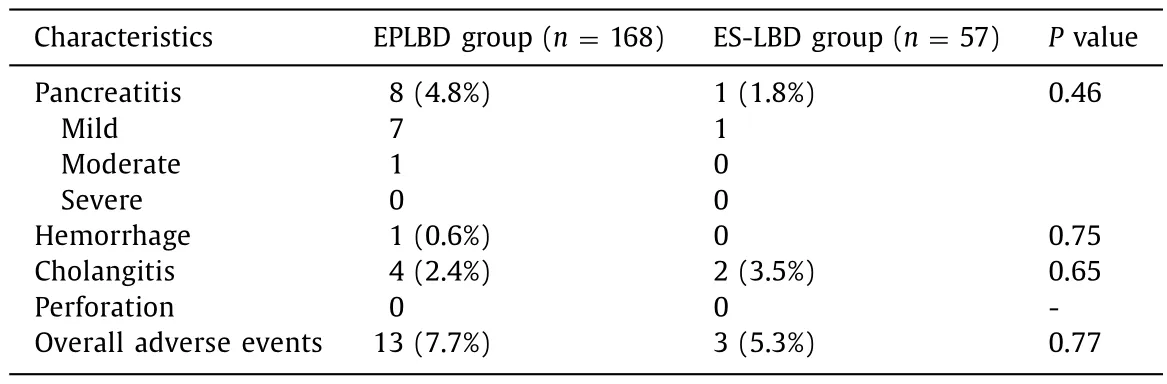
Table 3Comparison of the adverse events related to ERCP between the EPLBD and ES-LBD groups.
Long-term follow-up outcomes
Follow-up data were collected every year after complete stone clearance.There was no significant difference between the EPLBD and ES-LBD groups in the mean period of follow-up from the end of complete stone clearance to the last observation or death(113.6 ± 29.0 vs.106.7 ± 31.6 months,P= 0.13).Among these patients, 13 died of non-biliary diseases during a median follow-up of 38 months (range 27-101 months).There was no significant difference between the EPLBD and ES-LBD groups in the incidence of stone recurrence (11.9% vs.15.8%;P= 0.49) ( Table 4 ).ERCP procedures were successfully repeated in patients with recurrent bile duct stones.Each group had one cholangitis without stone recurrence, and they ultimately improved with conservative treatment.
Risk factors for stone recurrence
To examine predictive factors related to stone recurrence, we compared the stone recurrence group (n= 29) and no stone recurrence group (n= 196) and found that a diameter of CBD ≥15 mm was a risk factor for stone recurrence ( Table 5 ).Multivariate analysis also showed that diameter of CBD ≥15 mm (OR = 3.001;95% CI: 1.357-6.640;P= 0.007) was an independent risk factor for stone recurrence.Kaplan-Meier analysis revealed a significantly lower incidence of stone recurrence in the diameter of CBD<15 mm group than in the diameter of CBD ≥15 mm group (log-rank test,P= 0.001) ( Fig.3 ).
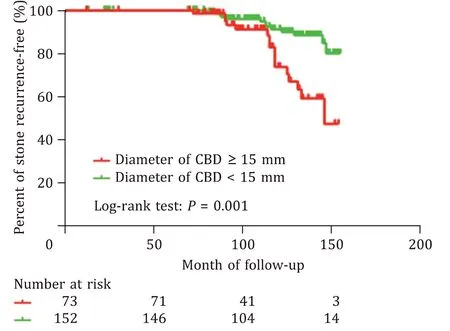
Fig.3.Cumulative incidence of bile duct stone recurrence.Kaplan-Meier estimated the proportion of patients with stone recurrence in the two groups.
Discussion
EST is currently a standard procedure for the treatment of CBD stones [11].However, it carries some serious short-term risks,especially bleeding and perforation.Moreover, EST also causes a permanent reduction in Oddi’s sphincter function, and perhaps an increased incidence of ascending cholangitis and formation of bile duct stones [ 14 , 15 ].EPBD has been introduced as a less traumatizing method compared to EST for clearance of CBD stones [ 2 , 8 , 16-18 ].However, it is more difficult to remove larger stones, because the biliary opening is enlarged to a lesser extent compared with EST.To overcome this disadvantage,Ersoz et al.[3]first described the EPLBD using a balloon larger than 12 mm for the removal of larger bile duct stones that were difficult to retrieve by conventional procedures after EST.Since then, EPLBD with limited or large EST has become rapidly and widely adopted [19-22].As an alternative method, EPLBD without a preceding EST was introduced as a simplified technique in 2009 [23].However, debate regarding the safety of EPLBD for the treatment of CBD stones has continued, because EPLBD shares a similar method of ballooning to that of EPBD, and there are still some concerns about the risk of post-ERCP pancreatitis.However,recent studies indicated that EPLBD for the removal of large bile duct stones does not increase the risk of post-ERCP pancreatitis, and that post-EPLBD pancreatitis was not associated with a larger balloon size [ 5 , 6 ].The present study shows that there was no statistically significant difference in the EPLBD (12-15 mm)with or without limited sphincterotomy groups with respect to complete stone clearance, application of ML, and overall adverse events rates.We demonstrated that ES-LBD and EPLBD alone were equally effective for CBD stone extraction.Another retrospective comparison study of EPLBD with or without EST for the management of large CBD stones by Okuno et al.[24]reported no significant difference in terms of overall successful stone removal, balloon size, procedure time, application of ML, or adverse events.Hwang et al.[25]also retrospectively compared the clinical outcomes of EPLBD with EST to those without EST and found that EPLBD alone may be a simple, safe, and effective alternative to ESLBD for the extraction of large CBD stones, and it can simplify the procedure compared with ES-LBD.All these studies indicate that EST prior to EPLBD may be unnecessary and can be omitted to simplify the procedure.A previous study [26]reported that an increase in balloon size may lead to tearing of the sphincter muscles and result in serious bleeding.We also found that EPLBD with a relatively large balloon ( ≥15 mm) was an independent risk factor for stone recurrence.According to our experience, extensive dilation may cause bleeding due to the damage of blood vessels.It is difficult to find the bleeding point and perform endoscopic hemostasis.In such cases, angiographic embolization may be the only effective therapeutic approach.In conclusion, the application of a larger balloon (12-15 mm) in size by EPLBD is an effective and safe procedure with respect to difficult stone clearance, and EST prior to EPLBD may be unnecessary and can be omitted to simplify the procedure.
The data on the long-term outcomes of ES-LBD compared with EPLBD alone for the removal of CBD stones are limited.In our study, the mean duration of the follow-up from the end of the complete stone clearance to the last observation or death were 113.6 and 106.7 months in the EPLBD and ES-LBD groups, respectively which we believe was sufficient to determine the incidence of stone recurrence.There was no significant difference between the EPLBD and ES-LBD groups in the incidence of stone recurrence.Kogure et al.[27]followed their patients for 22 months and found that stone recurrence was 14% after EPLBD with or without sphincterotomy, with a significant correlation to dilated CBD,which is similar to our study.The stone recurrence in the first 50 months was lower in our study than in other studies [27-29].This difference may be due to the follow-up method.Our telephone calls may miss some cases of stone recurrence.In addition, ursodeoxycholic acid (10 mg/kg) was recommended to use for these patients after bile duct stone removal which may be an effective treatment strategy to delay the recurrence of CBD stones.Yasuda et al.[30]also reported that EST was a predictive risk factor for the recurrence of bile duct stones.These results suggest that biliary sphincter dysfunction after EST results in additional late complications.In theory, the cause of long-term biliary adverse events after EST is thought to be duodenobiliary reflux caused by the permanent loss of the barrier of antireflux.The intestinal contents which may change the environment of biliary tract and bring about bacterial colonization.The bacteria produceβ-glucuronidase,which is associated with the formation of calcium bilirubinate gallstones [31].Thus, subsequent duodenobiliary reflux and bacterial contamination may cause late biliary complications such ascholangitis and stone formation.However, little is known about the long-term effects of biliary-sphincter function loss after EPLBD with or without EST.Recently, Cheon et al.[32]in a prospective randomized study have revealed that both EPLBD alone and EST + EPLBD resulted in persistent and comparable loss of sphincter of Oddi function.Hakuta et al.[33]also reported that EPLBD without EST increased late biliary complications compared with EPBD,suggesting the impairment of Oddi function.It appears that EPLBD with a relatively large balloon ( ≥12 mm) could permanently disrupt sphincter function and cause long-term adverse events in the same manner as EST which is similar to our present study.Based on these studies, we speculate that EPLBD with or without limited sphincterotomy provides sufficient orifice dilatation for stone removal and jeopardizes sphincter function permanently.
Our multivariate analysis found that a diameter of CBD ≥ 15 mm was the key factor for the increased incidence of stone recurrence.Kaplan-Meier analysis revealed a significantly lower incidence of stone recurrence in the diameter of CBD<15 mm group than in the diameter of CBD ≥ 15 mm group.A dilated CBD likely leads to bile stasis and bacterial infection, which play central roles in the stone formation.We usually insert self-expandable metal stent to ensure bile drainage and prevent stone recurrence caused by cholestasis for patients with bile duct dilatation>20 mm.According to our experience,this treatment strategy is effective in preventing the recurrence of bile duct stones.However, future randomized controlled trials and multicenter studies are expected in order to define the optimal endoscopic therapy.
The major limitation of this study is its retrospective design,which may cause the selection bias.Another limitation is the small sample size, and further multicenter prospective cohort studies are required to verify our findings.
In summary, EPLBD alone was simple, effective and safe compared with ES-LBD for the removal of CBD stones.EST preceding EPLBD may not be necessary.Our long-term follow-up showed no significant difference between EPLBD and ES-LBD in the incidence of stone recurrence.A diameter of CBD ≥15 mm may be a significant risk factor for stone recurrence.
Acknowledgments
We thank all the staff from the Digestive Endoscopy Center, Ruijin Hospital Affiliated to Shanghai Jiao Tong University School of Medicine and Department of Gastroenterology, Shuguang Hospital Affiliated to Shanghai University of Traditional Chinese Medicine for their help in this study.
CRediT authorship contribution statement
Tao Li :Funding acquisition, Writing - original draft.Li-Xiao Hao :Data curation.Chan Lv :Formal analysis.Xing-Jia Li :Data curation.Xiao-Dan Ji :Formal analysis.Meng Chen :Methodology.Chang Liu :Methodology.Li-Ke Bie :Supervision.Biao Gong :Conceptualization, Supervision, Writing - review & editing.
Funding
The study was supported by a grant from the Shuguang Hospital, Shanghai University of Traditional Chinese Medicine ( SGKJ-202010 ).
Ethical approval
This study was approved by the Ethics Committee of Shuguang Hospital, Shanghai University of Traditional Chinese Medicine and Ruijin Hospital, Shanghai Jiao Tong University School of Medicine.Written informed consent was obtained from all participants.
Competing interest
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
 Hepatobiliary & Pancreatic Diseases International2023年4期
Hepatobiliary & Pancreatic Diseases International2023年4期
- Hepatobiliary & Pancreatic Diseases International的其它文章
- Novel re-intervention device for occluded multiple uncovered self-expandable metal stent (with video)
- Hepatopancreatoduodenectomy for the treatment of extrahepatic cholangiocarcinoma ✩
- Microbiological cultures and antimicrobial prophylaxis in patients undergoing total pancreatectomy with islet cell autotransplantation
- Risk factors for posttransplant diabetes in patients with hepatocellular carcinoma
- The role of targeting protein for Xklp2 in tumorigenesis of hepatocellular carcinoma
- Isolated IgG4-associated autoimmune hepatitis or the first manifestation of IgG4-related disease?
