COVID-19:Insights into long-term manifestations and lockdown impacts
Erik Hilbold,Christin Bär,b,c,Thoms Thum,b,c,*
a Institute of Molecular and Translational Therapeutic Strategies(IMTTS),Hannover Medical School,Hannover 30625,Germany
b Fraunhofer Cluster of Excellence Immune-Mediated Diseases(CIMD),Hannover 30625,Germany
c Fraunhofer Institute for Toxicology and Experimental Medicine(ITEM),Hannover 30625,Germany
Abstract Coronaviruses are pathogens thought to primarily affect the respiratory tracts of humans.The outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in 2019 was also marked mainly by its symptoms of respiratory illness,which were named coronavirus disease 2019(COVID-19).Since its initial discovery,many other symptoms have been linked to acute SARS-CoV-2 infections as well as to the long-term outcomes of COVID-19 patients.Among these symptoms are different categories of cardiovascular diseases(CVDs),which continue to be the main cause of death worldwide.The World Health Organization estimates that 17.9 million people die from CVDs each year,accounting for~32% of all deaths globally.Physical inactivity is one of the most important behavioral risk factors for CVDs.The COVID-19 pandemic has affected CVDs as well as the physical activity in different ways.Here,we provide an overview of the current status as well as future challenges and possible solutions.
Keywords: Cardiovascular disease;COVID-19;Long COVID;Physical activity;Return to play
1.Introduction
For almost 3 years now,the coronavirus disease 2019(COVID-19) pandemic has remained an acute global emergency.1The drastic measures that were temporarily implemented since the start of the pandemic have affected most aspects of human activity,including physical activity (PA),social interaction,and the ability to maintain regular health checks.
In addition,massive efforts were undertaken by the scientific community during the pandemic to gain new insights into the disease’s mechanisms.For example,angiotensinconverting enzyme 2 was identified as the primary severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)entry receptor,2,3and its common expression could explain the wide range of affected organs.3,4Nevertheless,COVID-19 is complex and still far from being completely understood.Many non-respiratory symptoms—a number of them related to cardiovascular diseases (CVDs)5,6—have been found to be associated with acute SARS-CoV-2 infections as well as with long-term manifestations of COVID-19 (Fig.1).Angiotensinconverting enzyme 2,for example,also plays an important role in the disease severity and long-term complications of heart failure(HF)patients.4,7
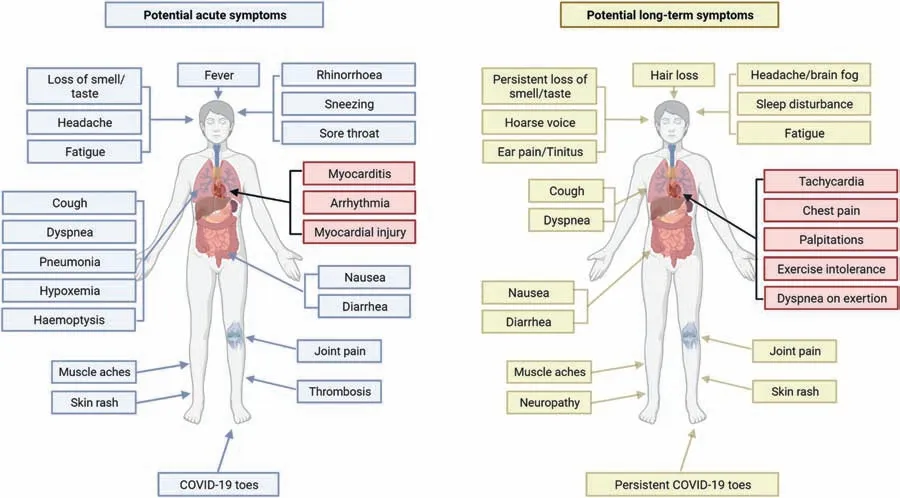
Fig.1.Potential symptoms of acute and post-acute coronavirus disease 2019(COVID-19).People suffering from COVID-19 show a diverse range of symptoms and signs affecting different organ systems.Potential cardiovascular symptoms of acute COVID-19 and long COVID are highlighted in red.
CVDs,a group of cardiac and vascular disorders,are the leading cause of death worldwide.8The World Health Organization (WHO) estimates that 17.9 million people die from CVDs each year (~32% of all deaths globally),primarily from heart attacks and strokes.8CVDs are considered to be age-related pathological conditions,and since the world’s elderly population is steadily increasing,they pose a growing health and socio-economic burden.9-12
Aside from an unhealthy diet,smoking,and harmful use of alcohol,physical inactivity (PI) is one of the most important behavioral risk factors for heart disease and stroke.8,13Individuals are classified as physically inactive if they do not follow PA guidelines.14-16There is a distinction,however,between PI and sedentary behavior (SB),which describes any waking behaviors characterized by an energy expenditure≤1.5 metabolic equivalents that is done while in a sitting,reclining,or lying position.15,16However,PA,which is defined as any bodily movement produced by skeletal muscles that results in energy expenditure,has been shown to be beneficial for cardiovascular health and to reduce the risk of CVDs.8,13,14,17-23
There are 5 types of PA: aerobic (e.g.,running,bicycling),muscle strengthening (weight lifting or resistance training),bone strengthening,balance activity,and multicomponent PA.24Depending on age,different types and amounts/intensities of PA are recommended for substantial health benefits(e.g.,for adults,at least 150-300 min of moderate-intensity aerobic PA per week,75-150 min of vigorous-intensity aerobic PA per week,or an equivalent combination of both is generally recommended).24Additionally,muscle-strengthening activities should be performed 2 or more days per week.24The 2nd edition of “Physical Activity Guidelines for Americans” provides detailed recommendations,25and additional specifications for staying physically active during selfquarantine were released by the WHO and the American College of Sports Medicine(Table 1).26,27Noteworthy,“green exercise” (PA in nature) positively affects mental health and quality of life,reduces mental health problems,and offsets the negative effects of unhealthy eating habits.28,29
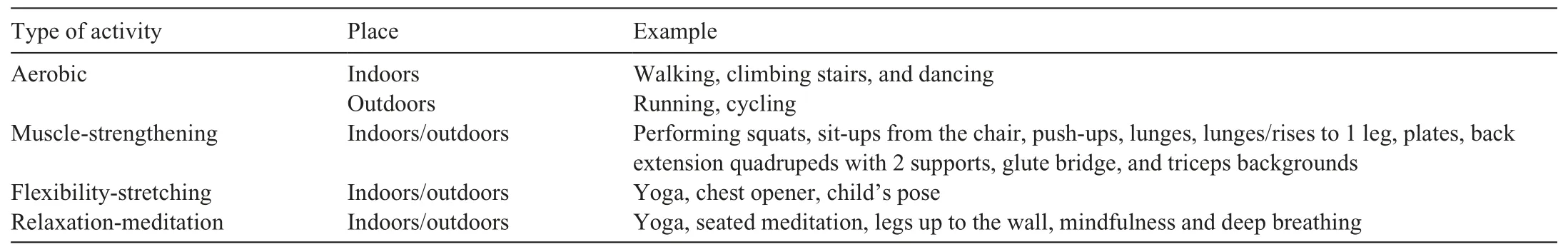
Table 1 Staying active during the COVID-19 pandemic(according to WHO and ACSM recommendations26,27).
In this review,we focus on cardiovascular complications from COVID-19 infections and the impact of the pandemic on PA and cardiovascular health.Additionally,we provide an outlook on future challenges and possible solutions in these areas.
For this purpose,original articles focusing on CVDs,COVID-19,and PA were researched in MEDLINE,PubMed,and PubMed Central.The search terms used were:“COVID-19”,“SARS-CoV-2”,“long COVID”,“cardiovascular disease”,“physical activity”,and“lockdown”,alone and in combination.
2.Cardiovascular injury—A symptom of COVID-19
2.1.Cardiovascular complications of acute COVID-19
Diverse abnormalities such as elevated cardiac biomarkers,electrocardiographic irregularities,and various cardiovascular complications (e.g.,myocarditis,myocardial injury,thrombosis,and arrhythmias) were reported among hospitalized COVID-19 patients(Table 2).30-36The underlying cause may be initially challenging to identify,as one or more of these abnormalities can coexist.30Myocardial injuries were additionally observed in both asymptomatic COVID-19 patients and COVID-19 mRNA vaccine recipients.30,37-39
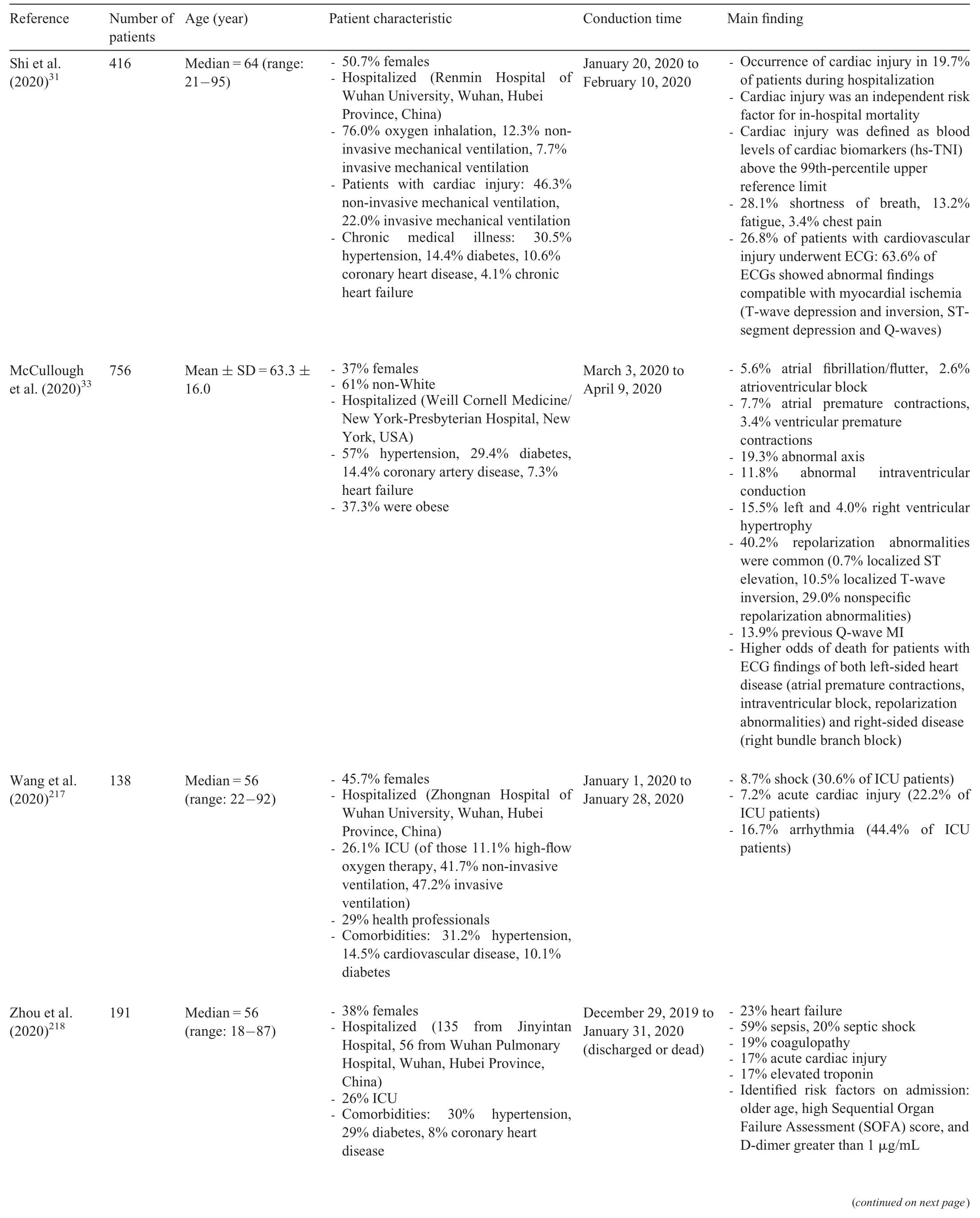
Table 2 Cardiovascular complications of acute COVID-19.
Remarkably,although rather infrequently,both fulminant myocarditis with cardiogenic shock or distributive shock resulting from sepsis and/or a hyperinflammatory state can occur with COVID-19.Importantly,case numbers seem to exceed the ones associated with viral myocarditis unrelated to COVID-19.30,40-44
Interestingly,in children (<18 years),most COVID-19 infections are asymptomatic or mild and hospitalizations are rare (though they did increase after the spread of the Delta variant).45-57However,multisystem inflammatory syndrome in children still occurred.45,58An assessment of multisystem inflammatory syndrome in children across the United States,most with no underlying conditions,revealed 80% with cardiovascular involvement,including elevated levels of B-type natriuretic peptide(73%)and troponin(50%),but with less severe or no respiratory problems.45,59However,a systematic review and meta-analysis reported a higher risk of severe COVID-19 and associated mortality for children with comorbidities,such as obese children,who had a 2.87 times higher risk of severe COVID-19.54
As most data were gathered from hospitalized patients,more studies of asymptomatic and mild cases are required to better assess the percentage of cardiac involvement,particularly with respect to post-acute and long-term cardiovascular consequences,which are reported with increasing frequency.5,60
2.2.Long-term cardiovascular outcomes of COVID-19
The term post-acute sequelae of SARS-CoV-2 infection(PASC) refers to a constellation of symptoms that emerge or persist after recovery from COVID-19,usually lasting for 4-12 weeks and beyond.30,61,62The terms: long COVID,post-acute COVID-19 syndrome,and long-haul COVID are also used to describe persisting symptoms after SARS-CoV-2 infection.61,63,64These patients suffer from diverse symptoms,such as fatigue,cognitive dysfunction,sleep disturbance,tachycardia,chest pain,and exercise intolerance.30Nearly all organ systems can be affected and,therefore,quality of life can be dramatically impacted.Importantly,even asymptomatic or minorly symptomatic individuals can experience long-term COVID-19 conditions.30,65
It is difficult to estimate the prevalence of long COVID as it is influenced by various factors,including differences in cohort characteristics,age,and sex of subjects enrolled,timing of assessment,sociodemographic factors,vaccines and variants,pre-existing health problems,sample size,study design,and variability in questionnaires or tools used.60Consequently,the reported prevalence is highly variable both across and within countries (e.g.,49%-76% in China,35%-77% in Germany,and 16%-53% in the United States60,66-71).However,risk factors (Fig.2) for developing long COVID appear to be relatively consistent.60In particular,female sex,increased age,obesity,asthma,poor general health,poor pre-pandemic mental health,poor sociodemographic factors,and type of work place (social/health care or teaching and education) represent important determinants across several studies.60,72-75Ironically,nationwide lockdowns and working remotely,which were measures meant to limit the spread of COVID-19,also restricted PA,increased obesity and poor dietary intake,and negatively affected mental health.60,76-78
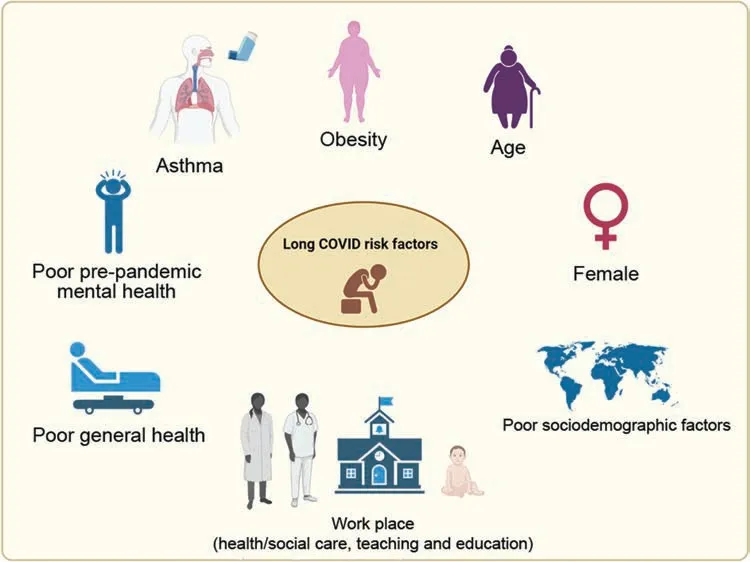
Fig.2.Long COVID risk factors.Important determinants for developing long-term symptoms after the acute illness across several studies include obesity,increasing age,female sex,poor sociodemographic factors,work place (social care,health care,teaching and education),poor general health,asthma,and poor pre-pandemic mental health.COVID=coronavirus disease.
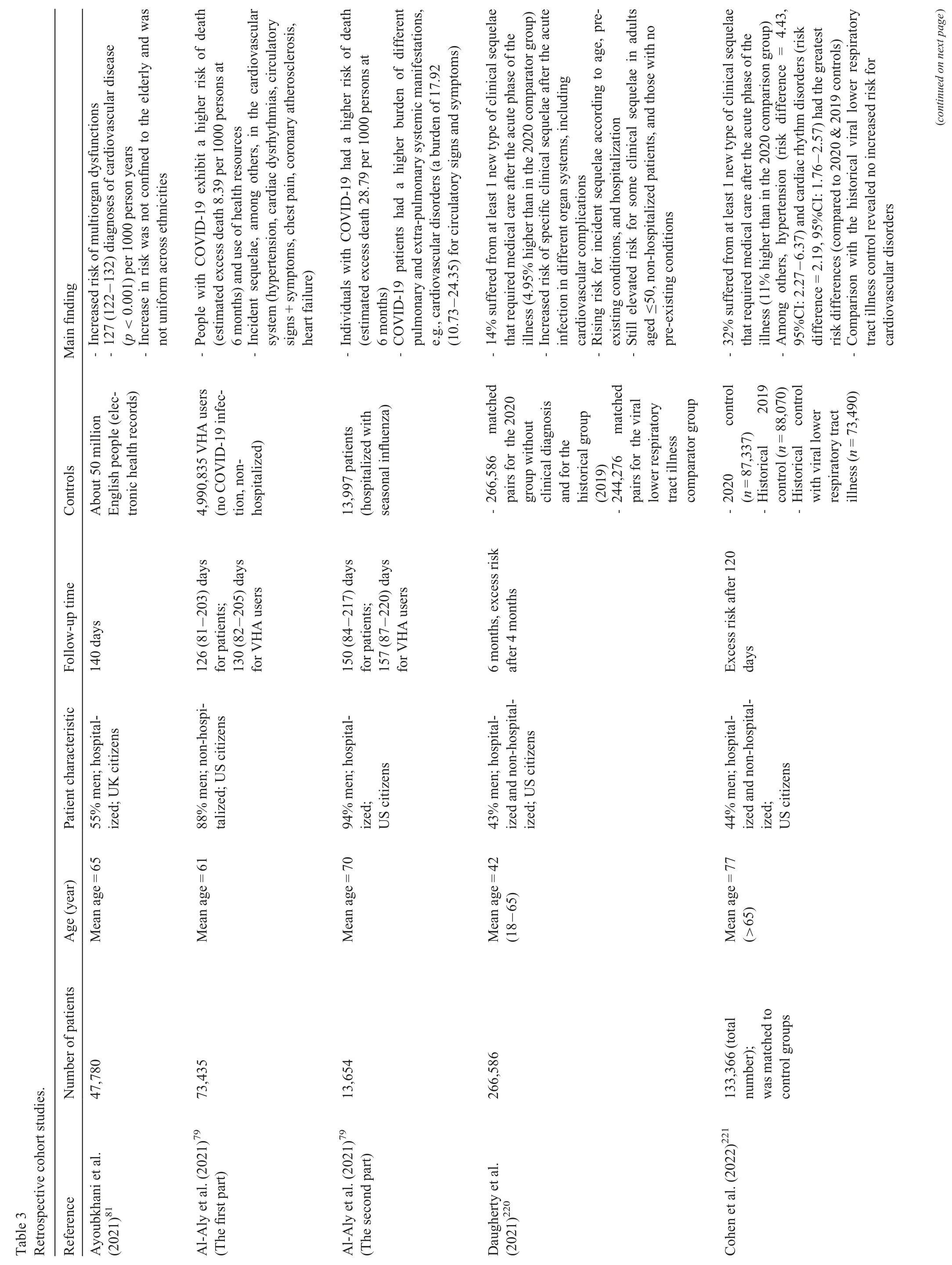
With respect to cardiovascular manifestations,recent articles were published reporting persistent cardiovascular symptoms after the acute phase of COVID-19 infections.These studies can be divided into 2 categories: retrospective(Table 3),those that rely on electronic medical health records and labeled datasets;or prospective (Table 4),those that use innovative technologies such as telemedicine,symptom apps,or face-face reviews.5,60,66,79-83
Within the scope of retrospective cohort studies,Xie and colleagues5analyzed the national healthcare databases from the U.S.Veterans Health Administration system to estimate the risks and 1-year burdens of a set of pre-specified incident cardiovascular outcomes.Therefore,they set up a cohort of 153,760 individuals who survived the first 30 days of COVID-19 and subdivided it according to the care setting during the acute infection phase (non-hospitalized (n=131,612),hospitalized(n=16,760),and admitted to an intensive care unit (ICU)(n=5388)).5Comparing this cohort with either control group (a contemporary (n=5,637,647) and a historical group from 2017(n=5,859,411),both without clinical evidence of COVID-19)revealed a higher risk of developing a pre-specified incident CVD(e.g.,myocarditis,HF,or dysrhythmia)for persons suffering from COVID-19 beyond the first 30 days after SARS-CoV-2 infection.5Interestingly,the risks and 1-year burdens of cardiovascular outcomes rose in accordance with severity of the acute illness.5Importantly,the available data were obtained between March 1,2020 and January 15,2021,5hence only the first variants(excluding Delta and Omicron) of SARS-CoV-2 were assessed and patients were almost exclusively unvaccinated.As variants differ in their characteristics (e.g.,severity or symptoms) and vaccinations can often affect the severity of an illness,the risk of developing CVDs that they found might not be representative for the current stage of the pandemic.Furthermore,most study members were White males and,therefore,the groups are not representative of the whole population.5Additionally,as the study is an electronic database analysis,misclassification bias and residual confounding cannot be excluded;and since the control group participants were not tested for SARS-CoV-2,it is possible that some of them were infected but asymptomatic.5As asymptomatic persons can also suffer unnoticeably from myocardial injury and involvement,30,37these individuals could have been incorrectly categorized into a control group while potentially developing long-term cardiovascular injuries over time.Apart from that,information on causes of death were not included in the datasets.5Nevertheless,a large sample size,the use of the U.S.Veterans Health Administration system,the evaluation across care settings,and multiple sensitivity analyses are strengths of this study.5
As a follow-up study,the same group investigated whether breakthrough SARS-CoV-2 infection (BTI) results in long COVID.82Therefore,they again used the U.S.Veterans Health Administration system to set up a cohort with BTI patients (n=33,940) and several controls of people without evidence of SARS-CoV-2 infection,including contemporary(n=4,983,491),historical (n=5,785,273),and vaccinated(n=2,566,369) controls.82The comparison to all control cohorts revealed a higher risk of death and incident PASC for people with BTIs 6 months after infection.82However,compared to persons suffering from COVID-19 who were not previously vaccinated,individuals with BTIs had a lower risk of death and incident PASC.82
Hence,the study has 2 key conclusions: (a) long COVID can also manifest in vaccinated individuals who experience a BTI,and (b) the range of organs affected by PASC,when it occurs,does not differ between BTIs and unvaccinated COVID-19 patients.82Finally,Al-Aly and colleagues82point out that vaccination prior to infection only provides partial protection in the post-acute phase of the disease and that measures to prevent BTIs are needed to reduce the risk of long-term health consequences from COVID-19.As the setup for this follow-up study mimics that of the first,the strengths and limitations are similar.
A retrospective cohort study of hospitalized COVID-19 patients quantified rates of organ specific dysfunction.81It compared 47,780 individuals(mean age=65 years;55% men)hospitalized with a primary COVID-19 diagnosis between January 1 and August 31,2020,to a matched control group of the general population(~50 million).81By doing so,this study revealed an increased risk of multiorgan dysfunction with a 3-fold higher chance of developing a major adverse cardiovascular event;this finding was not confined to the elderly and was more pronounced in ethnic minority groups.81Aside from its large sample size and completeness,the following limitations of this study need to be considered: data were only obtained from hospitalized patients (55% men) with a mean age of 65;hypertension and diabetes were not diagnosed,and individuals were considered to be “healthy” regarding these conditions;and,again,the data were acquired before the Delta and Omicron variants were circulating and when no vaccines were readily available.
Regarding prospective studies,cardiac involvement in the post-acute stage was reported in many studies(Table 4).Echocardiography,cardiac/cardiovascular magnetic resonance(CMR),cardiopulmonary exercise tests,and 12-lead electrocardiogram are often used investigative tools.60,84-88Dependent on these tools and the study design,the prevalence of abnormalities is highly variable and includes fewer cardiopulmonary symptoms(e.g.,5% chest pain)and no cardiac abnormalities in echocardiography,no cardiopulmonary symptoms but myocardial injury (e.g.,26% myocarditis) as determined by CMR,and cardiopulmonary symptoms (e.g.,76% chest pain) with myocardial injury (e.g.,19% myocarditis) as assessed by CMR.84,89,90
Recently,Hanneman and colleagues91investigated whether myocardial inflammation is present in patients who have currently recovered from COVID-19(85% at home,9% hospitalized,6% in ICU)and whether this is associated with abnormalities in tissue characterization and blood biomarkers.Using combined fluorodeoxyglucose-positron emission tomography/magnetic resonance imaging and blood biomarkers,they have demonstrated that myocardial inflammation is present in a small proportion of patients in association with cardiac magnetic resonance imaging abnormalities and systemic inflammation,and that all parameters improved after follow-up.91These findings contrast with the higher rates reported by Kotecha et al.84and the much higher rates found by Puntmann and colleagues.37The first group examined severely ill COVID-19 patients (all hospitalized,31% requiring ventilator support) with elevated troponin levels approximately 2 months after discharge by a standard CMR protocol.Although left ventricular function was found to be normal in 89% of patients,cardiac abnormalities were detected in 54%,including 26% with myocarditis-like scars,22% with ischemic injury patterns,and 6% with both pathologies.84However,inflammatory injury was found to a limited extent(3 or fewer myocardial segments)with minimal functional consequence,discounting 12 patients (8%) with findings consistent with active myocarditis at this late timepoint.84Puntmann et al.37reported that German patients (67% at home,33% hospitalized) had lower left ventricular ejection fraction and higher left ventricle volumes.Moreover,using CMR,cardiac involvement was found in 78% of patients,60% of whom suffered from ongoing myocardial inflammation.37These findings were independent of preexisting conditions,severity and overall course of the acute illness,and time from original diagnosis.37
Taken together,methodological and patient population variabilities (study size,severity characteristics,age,sex,varying definitions,co-morbidities,and medical history)make a direct comparison of these studies difficult.In this context,the different time periods of the studies should also be considered.Kotecha et al.84and Puntmann et al.37collected data during the first wave (until June 2020),whereas the data used by Hanneman et al.91were generated between November 2020 and June 2021,when SARS-CoV-2 variants were already circulating and vaccinations had begun.Still,cardiac tissue abnormalities (as identified by magnetic resonance imaging)appear to be common in recovering COVID-19 patients.Further investigation is required to determine whether patients with mild infections have less inflammatory injury than severely ill patients,as a comparison of the results reported by Hanneman et al.91and Kotecha et al.84could suggest.However,unlike the aforementioned retrospective studies,Puntmann and colleagues37did not find a relationship between these factors.In general,additional prospective studies with larger populations,defined parameters and controls,and mid-and long-term follow-up will be required to clearly identify cardiac long-term effects.
Regarding affected youth,fatigue (19%),headache (12%),insomnia (7.5%),muscle pain (6.9%),and confusion with concentration issues(6.8%)were the most common symptoms reported in a 12-month follow-up study.92Chest pain (3.8%)was also observed,but specific cardiovascular symptoms were not reported as this data was often not recorded.92-96Therefore,further studies are required to assess cardiovascular outcomes in youth,especially in severely ill pediatric patients(irrespective of multisystem inflammatory syndrome in children survivors,as those cardiovascular complications are known;see Section 2.1).Furthermore,the immune response to mild infections was similar in children and adults (reviewed by Chou et al.45);thus,similar cardiovascular outcomes for children could be expected.
2.3.Returning to sports after COVID-19
Possible cardiovascular sequelae following mild COVID-19 infection and observed myocardial injury in hospitalized patients5,30,37have raised concerns about how to proceed in terms of returning to play after acute illness,especially since myocarditis is known to be a common cause of sudden cardiac death in athletes.97
Several consensus recommendations were released,and they have changed over time according to increasing knowledge about the prevalence of cardiovascular events in collegiate and professional athletes,clinical manifestations,longterm complications,vaccine distributions,and features of new variants.98-101
Examinations,including CMR,in collegiate athletes from the United States showed myocardial and pericardial involvement in some individuals recovering from COVID-19.102-105However,large registries revealed a low prevalence of clinical myocarditis and have not found an increasing number of reported acute adverse cardiac events.106-108Additionally,a recent systemic cardiovascular screening in asymptomatic or mildly asymptomatic Olympic athletes before and after SARS-CoV-2 infections detected cardiac abnormalities (6% new ventricular arrhythmias,2% evidence for acute myocarditis (symptoms and elevated biomarkers)).109Thus,the initially strict precautions regarding post-COVID exercise(e.g.,resting for at least 7-14 days after being symptom free)were updated.30,101,110,111
The WHO has published guidelines for adults recovering from COVID-19 to support their rehabilitation and self-management.They recommend athletes follow a graduated 5-phase training to return to their baseline exercise regime(Table 5).112
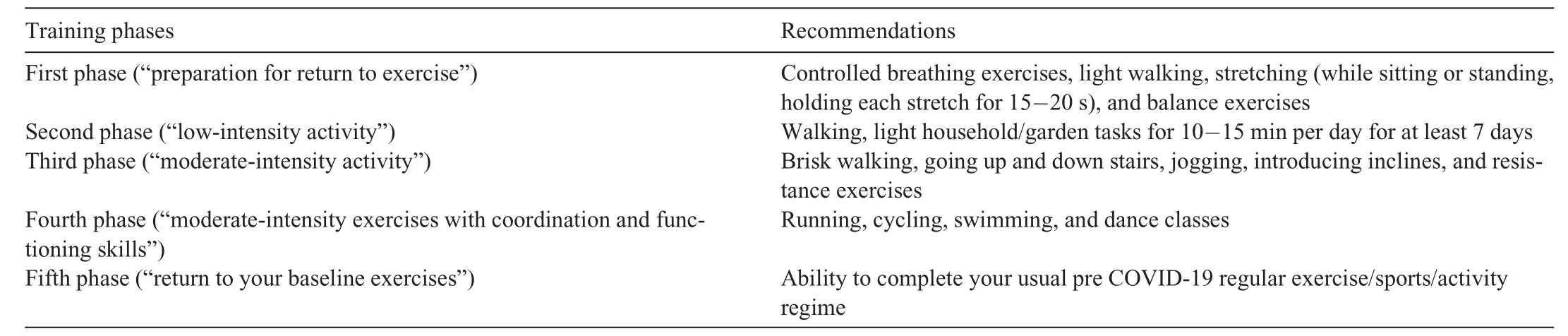
Table 5 Graduated 5-phase training for adults recovering from COVID-19(according to the WHO leaflet112).
Moreover,the American College of Cardiology (ACC) has published an expert consensus decision pathway,summarizing the current literature and providing recommendations related to cardiovascular sequelae of COVID-19 in adults.30
Here,it is important to evaluate cardiovascular symptoms suggestive of PASC and distinguish between a CVD (e.g.,myocarditis,arrhythmia) and a cardiovascular syndrome (“a heterogeneous disorder that includes widely ranging cardiovascular symptoms,without objective evidence of CVD using standard diagnostic tests”).30Therefore,a multidisciplinary approach should be used,as provided by the ACC.30If patients have persistent symptoms without a CVD,additional evaluation for PASC cardiovascular syndrome is recommended and should be determined by (a) “the most prominent symptom(s)”,(b)“the patient’s baseline characteristics”,and(c)“the pretest probability of CVD”.30
Recommendations made by the ACC with respect to 3 common cardiovascular symptoms are summarized in Fig.3.Regarding return to play (Fig.4),ACC recommendations include the following: (a) asymptomatic athletes may resume exercise training after 3 days of exercise abstinence during self-isolation;(b) exercise training may be resumed after resolving of symptoms only if they were mild or moderate non-cardiopulmonary ones;(c)resumption of exercise training without the need for additional testing if athletes suffer from remote infections (≥3 months) without ongoing cardiopulmonary symptoms;(d) triad testing (electrocardiogram,cardiac troponin,and echocardiogram)should be performed in athletes with ongoing cardiopulmonary symptoms (chest pain/tightness,palpitations,or syncope) and/or hospitalized athletes with increased suspicion for cardiac involvement as well as in those who develop new cardiopulmonary symptoms after resumption of exercise training;(e) in case of abnormal triad testing or persistent cardiopulmonary symptoms,CMR is recommended;(f) with myocarditis,exercise should be completely paused for 3-6 months;(g)if athletes have persistent cardiopulmonary symptoms and either normal CMR or a CMR that demonstrates other forms of myocardial(or pericardial) involvement,maximal-effort exercise testing (myocarditis has to be excluded with CMR before performing) and/or an ambulatory rhythm monitor may be helpful;(h) in athletes with recurrent COVID-19 in the absence of cardiopulmonary symptoms,repeat cardiac testing is not warranted;and (i)screening asymptomatic athletes or those with non-cardiopulmonary symptoms by CMR is probably low yielding.30Additionally,individuals with PASC who are not able to readily resume their previous level of activity should perform a structured and individualized graded exercise regimen during their recovery.30Precise exercise guidelines according to interventions used for postural orthostatic tachycardia syndrome will be useful for patients with tachycardia,exercise/orthostatic intolerance,and/or deconditioning to increase cardiac mass and blood volume as well as stroke volume,and improvemaximal oxygen uptake and functional capacity.30Detailed recommendations can be found in the ACC document.30
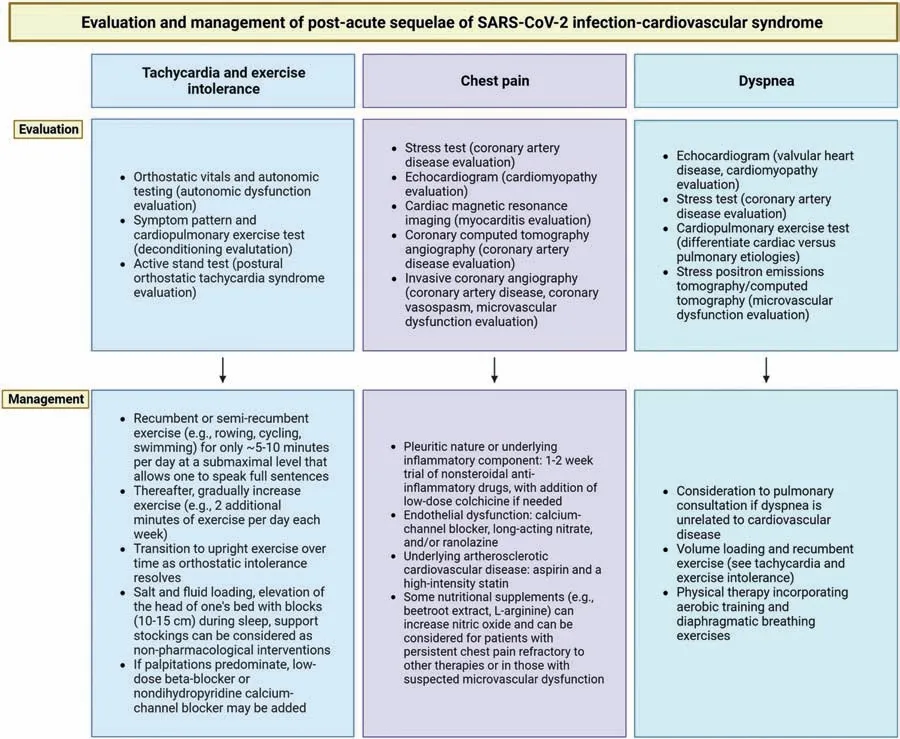
Fig.3.Evaluation and management of post-acute sequelae of SARS-CoV-2 infection-cardiovascular syndrome.Summary of evaluation and management recommendations for the common post-COVID-19 syndromes tachycardia and exercise intolerance,chest pain,and dyspnea,according to the American College of Cardiology.30 COVID-19=coronavirus disease 2019;SARS-CoV-2=severe acute respiratory syndrome coronavirus 2.
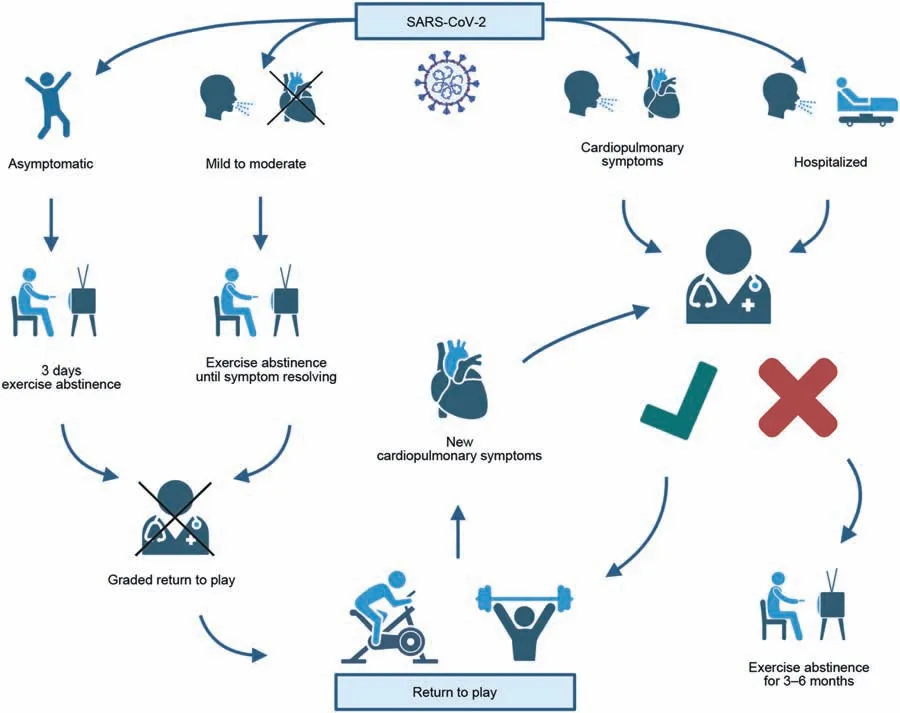
Fig.4.Return to play.Simplified graphical summary of return to play guidance according to recommendations made by the American College of Cardiology.30 SARS-CoV-2=severe acute respiratory syndrome coronavirus 2.
3.PA and COVID-19
3.1.PA—A severity predictor of COVID-19?
Since the beginning of the COVID-19 pandemic,the question has been,why are some patients asymptomatic or have only mild symptoms while others become severely ill,require hospitalization/intensive care,or die?As far as non-communicable disease outcomes are concerned,it is known that lifestyle risk factors are correlated to morbidity,mortality,and loss of disease-free years of life.113-116Moreover,low PA is a major risk factor for CVDs including coronary heart disease,stroke,peripheral artery disease,and HF.13,117,118Regardless of age,increased PA and reduced SB were found to be beneficial for health outcomes.13,20,21,119-139For example,higher selfreported moderate-to-vigorous PA and less screen time were associated with lower cardio-metabolic risk in adolescents(12-17 years).121In inactive healthy adults,the beneficial effects (p≤0.05) of walking improved 7 cardiovascular risk factors (body mass,body mass index,body fat,systolic and diastolic blood pressure,fasting glucose,and maximal cardiorespiratory fitness).124Moreover,a 12-week aerobic exercise program significantly reduced ambulatory and office bloodpressure in patients with resistant hypertension.119Furthermore,the effects of PA on mortality and CVDs in 130,000 people from 17 high-,middle-,and low-income countries were assessed.130Compared to low PA (<150 min/week of moderate intensity PA),moderate PA (150-750 min/week)and high PA (>750 min/week) were associated with a graded reduction of major cardiovascular events(hazard ratio for highvs.low,0.75 (95% confidence interval (95% CI): 0.69-0.82);moderatevs.low,0.86 (95% CI: 0.78-0.93);highvs.moderate,0.88 (95% CI: 0.82-0.94) during a mean 6.9 years of follow-up.130Also for mobility-limited older adults (mean age=78.9 years),higher levels of accelerometer-measured PA and increased step numbers were significantly associated with lower cardiovascular event rates.139
In addition,PI was associated with a higher risk for systemic infections and pneumonia.140-144In contrast,daily PA positively impacts the immune system.145-147Several studies reported positive effects,such as higher levels of natural killer cells,neutrophils,lymphocytes,monocytes,and plasma interleukin-6,as well as an increased function of natural killer cells and a decrease in inflammation.28,148-151Thus,several studies additionally focused on investigating whether PA is related to COVID-19 outcomes and severity.152-161
Among the general population,there is a 32% higher relative risk for physically inactive persons and a 105% increased relative risk for obese people to experience a COVID-19-associated hospital admission.156This is in line with a crosssectional study showing an association between low PA levels and more severe disease forms.162In contrast,a UK Biobank study observed “suggestive evidence for lower odds (up to 20%) of severe COVID-19 per 30 min of daily moderate-tovigorous PA (p=0.06)”.154,163Another UK Biobank study found a significantly lower risk of dying from COVID-19 for persons with moderate (adjusted relative risk (aRR)=0.43,95% CI: 0.25-0.75) and high fitness (aRR=0.37,95% CI:0.16-0.85).164Significantly reduced odds for hospital admission in physically active individuals were also reported using an online questionnaire.165Additionally,at least 150 min a week of moderate-intensity PA or 75 min a week of vigorousintensity PA reduced the prevalence of hospital admission by 34.3%.157Furthermore,consistent PI was associated with a greater risk for severe COVID-19 outcomes requiring hospitalization (odds ratio (OR)=2.26;95% CI: 1.81-2.83),admission to the ICU (OR 1.73;95% CI: 1.18-2.55),or leading to death (OR=2.49;95% CI: 1.33-4.67).161Compared to physically inactive individuals,adults who followed the 2018 PA guidelines for both aerobic and muscle strengthening activities had a lower risk of SARS-CoV-2 infection (2.6%vs.3.1%;aRR=0.85;95% CI: 0.72-0.96),severe COVID-19 illness (0.35%vs.0.66%;aRR=0.42;95%CI: 0.19-0.91),and COVID-19-related death (0.02%vs.0.08%;aRR=0.24;95% CI: 0.05-0.99).153One analysis of U.S.counties showed a negative association between PA rates and COVID-19 cases and deaths.166
An accelerometer-based study supports these results by demonstrating that 30 min of daily moderate-to-vigorous PA reduced odds of severe COVID-19 by 37% in women and 16% in men.154Reinforcing these findings is a recent South African study,for which the PA of 65,361 adults was directly assessed by smart devices,clocked gym attendance,and mass participation using a healthy lifestyle behavioral change program called Vitality.159PA was found to be positively associated with protection against adverse outcomes from COVID-19.159Highly physically active adults had a 34% lower relative risk for hospitalization,41% less relative risk of admission to the ICU,and a relative risk of death reduced by 42% compared to low activity participants.159Even moderate PA showed significantly better outcomes.159Regarding long-term symptoms,a negative association between PA and neurocognitive impairment and fatigue symptoms was detected in healthcare workers with initially asymptomatic,mild,and moderate infections.158
Moreover,autonomic dysfunction,which can cause alterations in the cardiovascular and immune systems,was associated with an increased severity of COVID-19.160,167,168Even in mild-to-moderate COVID-19 infections,autonomic dysfunction(greater sympathetic activity,less parasympathetic activity,global heart rate variability) appeared in young adults.160As obesity and PI were correlated with worse indices of cardiac autonomic modulation,160this indicates a beneficial effect of PA.
In a study of hospitalized COVID-19 patients,sedentary lifestyle increased mortality risk by almost 6-fold.152On the contrary,a separate study showed that PA was not independently associated with length of stay or any other clinically relevant outcomes of hospitalized patients with moderate-tosevere COVID-19.155Both studies had relatively small sample sizes and assessed PA levels using a questionnaire.Additionally,in the first study,the questionnaire was answered by relatives for patients who died.Thus,bias cannot be ruled out as self-reporting PA can lead to under-or overestimation.159It is likely that different underlying factors influenced the outcomes of hospitalized patients and that the benefit of PA may decrease with increasing severity of the disease.Further research with larger sample numbers and more defined methods will be required to determine whether PA levels are related to a better prognosis in already-hospitalized patients.However,these studies clearly emphasized the importance of regular PA for reducing the risk of severe COVID-19 outcomes in the general population.Hence,PA interventions are a valuable and cheap preventive tool to improve body composition along with cardiorespiratory,metabolic,and mental health,and to enhance antibody responses after vaccination.28,169
3.2.Lockdown impact on PA and CVD
The COVID-19 pandemic has lasted almost 3 years and so,along with it,have the drastically restrictive measures that are temporarily affecting peoples’ daily lives.Occasionally,a complete or incomplete lockdown mandates remote school/work and orders all non-essential facilities closed,causing social isolation and loneliness as well as a relative decrease in PA and increase in SB for most of the global population.170-174
Social isolation(an objective state of absent social connections or interactions)and loneliness(the subjective experience of social isolation and feeling alone) are problems that cooccur in all ages,but they are particularly present in older adults.174-177Both were associated with mental health problems,cognitive decline,CVDs,and a higher risk of mortality.175-184Loneliness is a predictor of elevated systolic blood pressure and an independent risk factor for PI.185-187Furthermore,unhealthy eating habits,such as overeating and snacking,might be developed as a consequence of social isolation and may lead to weight gain and nutritional imbalances that impair immune function.28,188
Regarding PA,surveys of healthy adults in Spain compared a normal pre-pandemic week to the first 2 weeks of lockdown in 2020 and showed a reduction in vigorous PA and walking time of 16.8% and 58.2%,respectively,whereas sedentary time increased 23.8%.189Supporting this,an international online survey from April 2020 revealed a 24% reduction in the number of days/week for all PA and a decrease in the number of min/day of 33.5%,whereas the number of sitting hours per day increased by 28.6% in adults from Asia (36%),Africa(40%),Europe (21%),and others (3%) during home confinement.190Also,in young Chinese adults,a significant decrease in PA,along with an increase in SB and sleeping time,was reported during the COVID-19 pandemic.191On the contrary,a recent study from the Republic of Korea has found no general decline of vigorous (adjusted OR (aOR)=0.96,95% CI: 0.79-1.18,p=0.696) and moderate (aOR=1.12,95% CI:0.94-1.32,p=0.201)PA between the years 2019 and 2020.192In fact,an increased moderate PA (aOR=1.29,95% CI:1.01-1.65,p=0.042)was seen in females in 2020 as compared to 2019.192Moreover,the study found a lower sedentary time(aOR=0.35,95% CI:0.17-0.72,p=0.005)for adults from the Republic of Korea during the pandemic.192Weekly PA (mean difference (MD)=-159.87;95% CI:-100.44 to -219.31) and weekly sitting time (MD=-106.76;95% CI: -71.85 to -141.67) both increased in Spanish college students (age=20.50±4.56 years,mean ±SD).193Note that the weekly time of specific parameters was compared before and during the lockdown;hence,negative numbers indicate an increase in those behaviors during the lockdown.Interestingly,the female students increased their PA by 185.24 min/week during lockdown,whereas the rise was only 53.46 min/week in the male group.193In contrast,a Bavarian online survey based on step-count data from smartphones or wearables showed a 25% reduction in step counts/day during the lockdown.194Of the Bavarian students(age=23.3±4.0 years,mean ± SD),44.5% decreased their amount of training and 32.8% increased their amount of PA.194
Observed discrepancies in PA levels between the aforementioned studies might be caused by a number of factors,including the variety of lockdown regulations between countries.For example,during the first lockdown in Italy and Spain,people were only allowed to leave their houses for reasons related to work or health or to purchase food and drugstore items,whereas people could still perform outdoor activities in Germany.Moreover,personal characteristics could play a crucial role.It is conceivable that some people who,prior to the pandemic,would have liked to increase their PA but did not have enough time during the course of their normal working day would,as a result of the switch to remote or short-time work,suddenly have time to join an online sports class or go jogging.In contrast,people who used to cycle to work would likely see a decrease in PA if forced to work remotely due to the restrictions.Furthermore,among the Spanish university students,group-related alterations of PA levels and SB were found for groups “first year of study”,“overweight or obese”,and “smokers”.These individuals did not experience differences,which points toward a high baseline SB regardless of pandemic-related restrictions.193
A Greek online survey showed an increase in sleep duration and screen time along with a decrease in PA,leading to an increase in bodyweight in children and adolescents.195Several studies have reported similar findings.196-198Since lower levels of PA are associated with increased bodyweight and mental health problems (which can alter eating behavior),obesity is a clear potential risk factor for severe COVID-19 and for developing CVDs.13,28,54,188,195,199The long-term consequences of safety/lockdown guidelines for today’s youth strongly underline the importance of staying active.The elderly did not fare well in the lockdowns either,with decreased PA levels and a 5.8% increased prevalence of locomotive syndromes,according to one Japanese study.200
In another recently published Italian survey comparing preand post-lockdown time periods,sedentary time was still increased,especially during weekends,several months after the lockdown,with an overall 7% increase in PI.201Moreover,locations and types of activities have changed over time in the Italian population: PA at home increased by 13% but decreased by 17% indoors (e.g.,gyms and swimming pools)and by 3% outdoors (e.g.,outdoor playground and parks).201Fitness sports,jogging,and cycling increased,and participation in excursions,water sports,dance,and volleyball declined.201
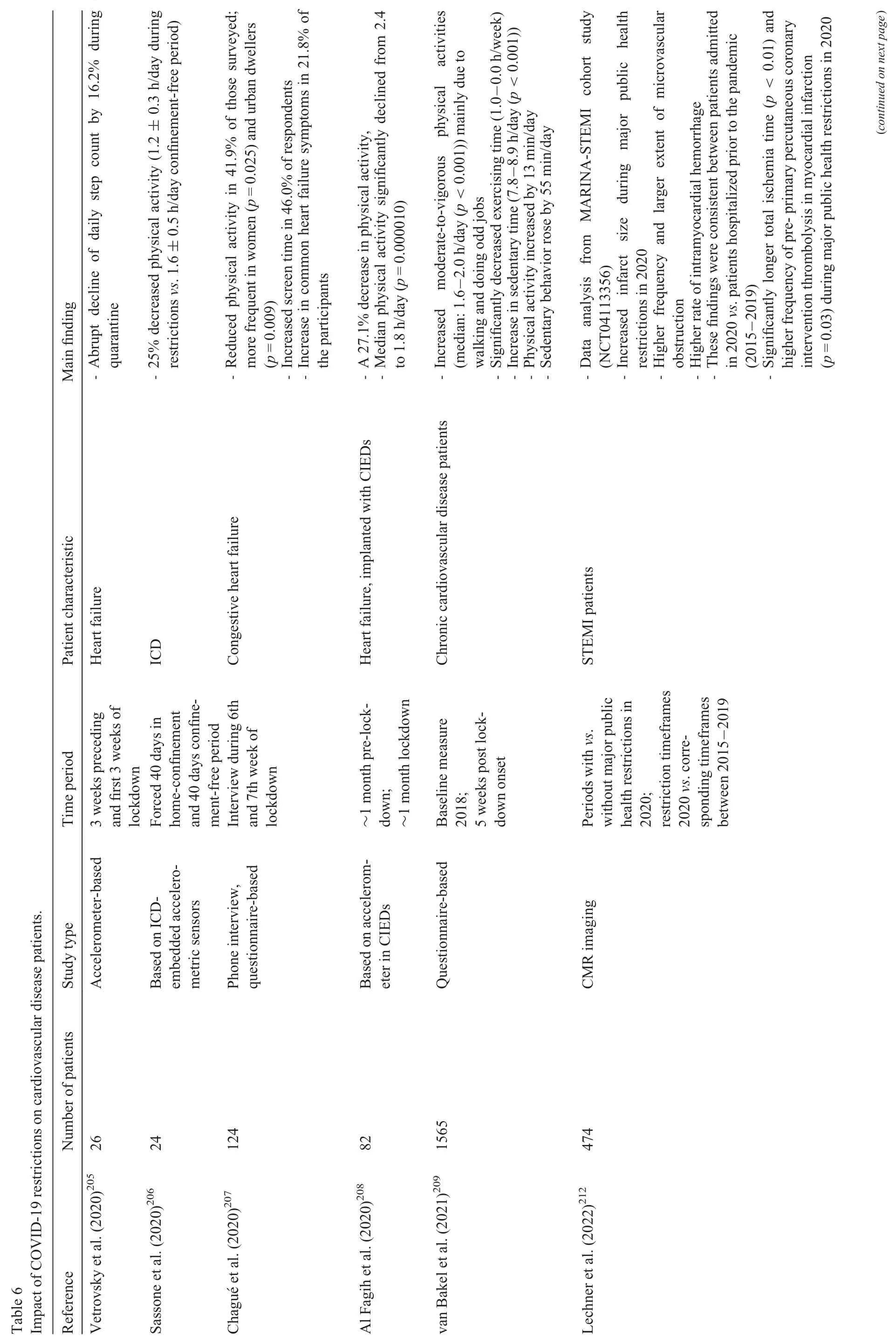
As exercise and PA are economic and successful methods for improving cardiovascular health and reducing CVDs,202-204it is of special interest how the lockdown influenced patients suffering from CVDs.Similar to the majority of the findings in healthy individuals,a significant decline in PA and an increase in SB were reported in CVD patients during the lockdown (Table 6).172,205-211A large,accelerometerbased observational study was done on patients in New York City and Minneapolis/Saint Paul who had pacemakers and implantable cardioverter-defibrillators;it showed a 26% reduction in PA in New York City and a 15% reduction in Minneapolis/Saint Paul during the lockdown.210The decrease in PA was most pronounced within the first 2 weeks of the regional lockdown;it increased slowly but did not return to pre-restriction levels 5 months after the lockdown ended.210Additionally,a large registry has investigated the impact of the lockdown on PA and arrhythmia burden in patients who received cardiac resynchronization therapy (CRT) devices with daily,automatic remote monitoring functions.172In these patients,PA abruptly decreased in the first 2 weeks of lockdown,then returned to pre-lockdown levels 3-7 weeks later,and surpassed these levels after 8-10 weeks.172Thus,when PA was relatively decreased,by 6.5%,during the initial lockdown,172the atrial high rate episode burden was increased by 17%,with no changes observed in ventricular arrhytmia.172Moreover,a small single-center study in HF patients with CRT and implantable cardioverter-defibrillators analyzed the 3-month period immediately preceding the lockdown,the 69 days of lockdown,and the 3-month period following the first lockdown.211It showed a decline in daily PA of 16.6%during the lockdown,with mean daily PA decreasing from 3.4±1.9 to 2.9±1.8 h per day(p<0.001).211No significant difference in the average daily PA was ascertained between the pre-and post-lockdown period (-0.0007 h/day;p=0.99)or between the post-lockdown period and the same time period from the previous year (3.4±2.0 h/dayvs.3.5±2.0 h/day;p=0.40).211In contrast to the large registry,172no significant difference was identified regarding the burden of atrial arrhythmias.211However,lower PA during the lockdown correlated with more alarm episodes detected in HF patients,assuming a generally negative effect from reduced PA211and a potentially underestimated arrhythmia burden due to the small study size.
Importantly,Lechner and colleagues212explored how the major public health restrictions of the COVID-19 pandemic affected ST-elevation myocardial infarction with respect to severity and myocardial tissue damage.Using CMR,they found an increased infarct size (22% (interquartile range(IQR):12%-29%)vs.14%(IQR:6%-23%),p<0.01),more extensive micro-vascular obstruction (1.5% (IQR:0.1%-11.4%)vs.0.2% (IQR: 0.0%-2.6%),p<0.01),and a higher rate of intramyocardial hemorrhage (56%vs.34%,p=0.02) in COVID-19 negative ST-elevation myocardial infarction patients during the lockdown period of 2020 as compared to phases without major COVID-19 restrictions.212Different underlying causes are conceivable.For example,patients might have been afraid of getting infected with SARS-CoV-2 after visiting their physician or following a hospital admission and,therefore,might have delayed medical consultation.In support of this hypothesis,a reduction in hospital admissions was seen in Austria,Italy,and England during March 2020.213-215Besides a decrease in hospital admissions,a significantly longer ischemia time and a door-toballoon time beyond 30 min were observed by De Luca and colleagues,216which might be explained by organizational delay due to specific COVID-19 protocols (e.g.,screening patients and preparing equipment).216Apart from that,an unhealthy lifestyle (PI,obesity) can also contribute to worsened ST-elevation myocardial infarction outcomes.Further research is required to investigate the impact of lockdown restrictions on CVDs and their underlying causes.
4.Conclusions and future perspectives
Almost 3 years in the COVID-19 pandemic has revealed that cardiovascular complications are common in severely ill patients,but also appear in mild and asymptomatic cases.PASC of COVID-19 evolved to become a major public health issue,in part due to the high burden of cardiovascular symptoms.The underlying pathomechanisms remain relatively illunderstood and could change to some degree with emerging variants.Hence,current priorities are,among others,(a) to establish the prevalence of long-term cardiovascular outcomes according to different circulating variants,vaccination status,and disease severity,(b)to further investigate underlying pathomechanisms,and (c) to ascertain the role of possible causal mechanisms,such as PA,obesity,social isolation,loneliness,immune function,and genetic predispositions.Adjusting vaccines to emerging variants and developing new therapies for acute and long COVID-19 are also high priority projects.With respect to long COVID,a wide range of clinical trials is listed on the WHO’s International Clinical Trials Registry Platform,and Raman and colleagues have reviewed a selection of them.60
Furthermore,maintaining sufficient levels of PA and staying active during the COVID-19 pandemic,despite potential quarantine restrictions,is crucial for health conditions.26,27,170There are new techniques and tools,such as fitness tracking apps and wearables,online sports classes,telerehabilitations or simple at-home training according to special exercise plans,that show promise for helping to achieve regular PA in difficult situations like in lockdowns.Further development and integration of these methods into daily life may be beneficial in case of another pandemic,as these things may be more easily implemented if patients are already familiar with them.
Acknowledgments
This work was supported by the MWK Lower Saxony,Germany and the COVID-19 Forschungsnetzwerk Niedersachsen (COFONI).Figures were created with BioRender.com.We thank Sarah Cushman for English language editing of the manuscript.
Author’s contributions
EH wrote the manuscript and prepared the figures;CB and TT guided the manuscript preparation and critically revised it.All authors have read and approved the final version of the manuscript,and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests(with regard to this article).
 Journal of Sport and Health Science2023年4期
Journal of Sport and Health Science2023年4期
- Journal of Sport and Health Science的其它文章
- Beyond cardiomyocytes:Cellular diversity in the heart’s response to exercise
- Exercise training attenuates angiotensin II-induced cardiac fibrosis by reducing POU2F1 expression
- Specific alterations of regional myocardial work in strength-trained athletes using anabolic androgenic steroids compared to athletes with genetic hypertrophic cardiomyopathy
- Effects of exercise by type and duration on quality of life in patients with digestive system cancers:A systematic review and network meta-analysis
- Recovery shape of physical activity after COVID-19 pandemic
- Sports compression garments improve resting markers of venous return and muscle blood flow in male basketball players
