Effect of intubation in patients with functional epiphora after endoscopic dacryocystorhinostomy
Xue-Mei Han, Wen-Hao Jiang, Wen-Can Wu, Bo Yu
1Department of Ophthalmology, the First Affiliated Hospital of Zhejiang Chinese Medicine University, Hangzhou 310000,Zhejiang Province, China
2Department of Ophthalmology, the Fourth Affiliated Hospital of Zhejiang University School of Medicine, Yiwu 322000,Zhejiang Province, China
3Department of Orbital and Oculoplastic Surgery, National Clinical Research Center for Ocular Diseases, Eye Hospital,Wenzhou Medical University, Wenzhou 325027, Zhejiang Province, China
Abstract● AlM: To investigate the effect of bicanalicular silicone tube intubation (BSTI) in the treatment of functional epiphora after endoscopic dacryocystorhinostomy (En-DCR).
● KEYWORDS: bicanalicular silicone tube; endoscopic dacryocystorhinostomy; functional epiphora
INTRODUCTION
Dacryocystorhinostomy (DCR) is the procedure designed to create a direct drainage of the tears, in the case of nasolacrimal duct obstruction (NLDO), where the surgically created bypass goes directly into the nasal cavity.It can be performed either externally or intranasal endoscopy[1].Endoscopic dacryocystorhinostomy (En-DCR) was originally put forward by McDonogh and Meiring[2]in 1989.
It has gained popularity these years due to its advantages over external DCR (Ex-DCR), including less intraoperative bleeding, short hospital stay, and avoidance of scar formation.En-DCR reports success ratios changing from 80 to 90 percent,which is comparable to Ex-DCR[1,3-4].
Outcome success can be evaluated using anatomic and/or functional methods.Almost all the articles showed differences in anatomical and functional success rates, with functional success rates consistently slightly lower than anatomical success rates[5-6].This means that in certain situations, patients grumble of troublesome epiphora even though lacrimal duct is patent by lacrimal irrigation test and endoscopic examination,and the situation is named “functional epiphora”after En-DCR[6-8].
Functional epiphora therapy after Ex-DCR have been reported by a few articles[9-10].Silicone tube intubation, lid-tightening procedures, secondary DCR, punctate plasty as well as conjunctiva-DCR were the main methods[7].However, silicone tube intubation is known to be relatively simple, safe, and minimally invasive compared to other invasive procedures, and has been recommended by the authors[7,9-10].To our knowledge,there have been no reports on the functional epiphora therapy after En-DCR.In the paper, we studied the success ratio as well as complications of secondary bicanalicular silicone tube intubation (BSTI) surgery in patients with anatomically patent but functionally failed En-DCR.
SUBJECTS AND METHODS
Ethical ApprovalThe study was approved by the Institutional Ethics Committee and was consisted with the Declaration of Helsinki.We reviewed the medical records of 2559 patients(3256 eyes) who received En-DCRs by a surgical team from Sep.2012 to Dec.2019.The informed consent was obtained from the subjects.
En-DCRs were performed to patients with NLDO, chronic dacryocystitis, acute dacryocystitis, dacryocyst mucoceles or traumatic dacryocystitis.The surgeries were conducted with a standard process depicted in former reports[4-6,11].In many cases, silicone tubes were not implanted, except for punctual stenosis, canalicular stenosis, lacrimal sac scarring, or upper nasal cavity narrow.The tubes were removed about 1mo after surgeries.The therapeutic effect was evaluated >9mo after operation.The definition of functional epiphora after En-DCR was as follow: 1) postoperative recurrence or persistent epiphora, 2) slow dye disappearance on the fluorescein dye disappearance test (FDDT), 3) anatomically proved to be a patent for irrigation without obvious reflux; 4) evidence of ostial patency under the endoscopic visualization.Patients with facial nerve palsy, eyelid dislocation, previous eyelid surgeries,untreated conjunctivitis or blepharitis, and secondary lacrimal drainage obstruction were excluded.Details of the intubation procedure and post-operation complications were explained to the patients who had functional epiphora after En-DCR.If the patient agreed to next therapy, BSTI was conductedviarhinostomy under a zero-degree endoscope (Karl Storz,Tuttlingen, Germany) in an outpatient operating room.
All operations were conducted with local anesthesia(infraorbital nerve and anterior ethmoidal nerve) by the same surgeon.At the beginning of surgery, the nasal cavity was filled with cotton pad soaked in a 10:1 mixture of lidocaine (4%) as well as epinephrine (1 mg/mL) for 2min.Bicanalicular silicone tubes were inserted in the nasal ostium from the expanded upper and lower puncta, and the tube ends were tied together,leaving the knot in the nasal cavity.The time taken for the entire operation was recorded as well.
All subjects received nasal colt nasal spray (Astra Zeneca,Wilmington, USA) twice daily for 6wk.The bicanalicular silicone tubes were allowed to remain in the nasal ostium for 1mo before being taken out.Follow-up time was 1wk,1mo, 6mo, 1y as well as 2y post operation.At every followup, the presence of epiphora was was recorded, the slit-lamp examination, the lacrimal irrigation, endoscopic dyeing test and endoscopic ostium examination were also performed to evaluate the outcomes.
Functional success was with the definition as the lack of epiphora post operation, free flowing irrigation through the lacrimal system, disappearance dye tests and normal functional endoscopic dye tests were performed at 6mo, 1, and 2y of follow-up.
RESULTS
To sum up, 84 patients (95 eyes) with functional epiphora after En-DCR were included.Seven patients (9 eyes) refused the further interventions, 5 patients (6 eyes) failed to complete postoperative follow-up, and a bicanalicular silicone tube prolapse occurred within 1mo after surgery in a patient.In total, 71 patients (79 eyes) included at last.
Of the 71 surgical patients, 27 were male and 44 were female(79 eyes, 42 in the right eye and 37 in the left eye).The mean age of patients was 56.0y (from 27 to 73y; median age, 54y).Among them, 62 eyes had received En-DCRs, 17 eyes with En-DCRs and BSTIs.For specific reasons requiring En-DCR, there were 23 cases of NLDO, 44 cases of chronic dacryocystitis, 8 cases of acute dacryocystitis, and 4 cases of dacryocyst mucoceles.All secondly BSTI were successfully completed within 15min.
According to the definition of functional success, the success ratios at six months, one year as well as two years postoperation were 94.9% (75/79), 92.4% (73/79), and 91.1%(72/79), respectively (Figure 1).At the last follow-up, 3 eyes presented with punctal slitting (2 eyes without epiphora), 1 eye with canalicular slitting (Figure 2), 1 eye with canalicular stenosis and 4 eyes with still present functional epiphora without detectable abnormal.The change in the number of failures during postoperative follow-up is shown in Figure 3.Other associated complications, like ostium obstruction,canalicular obstruction, punctual granuloma or postoperative epistaxis were absentviathe 2y follow-up.
DISCUSSION
We use En-DCR to treat cases of functional epiphora with a chance of success in 91.1% of treated cases.In some large sample reports of En-DCRs, the possibility of functional epiphora has been reported in 2%-4% of cases[12-15].Although the probability is low, the total number of patients with functional epiphora is still quite large due to the large number of patients.The study reviewed the medical records of 3256 eyes receiving En-DCR and included 95 eyes with functional epiphora.According to the exclusion criteria, 71 cases (79 eyes) were included at last.For specific causes requiring En-DCR treatment, there were 23 cases of NLDO, 44 cases of chronic dacryocystitis, 8 cases of acute dacryocystitis, and 4 cases of dacryocystitis mucoceles.
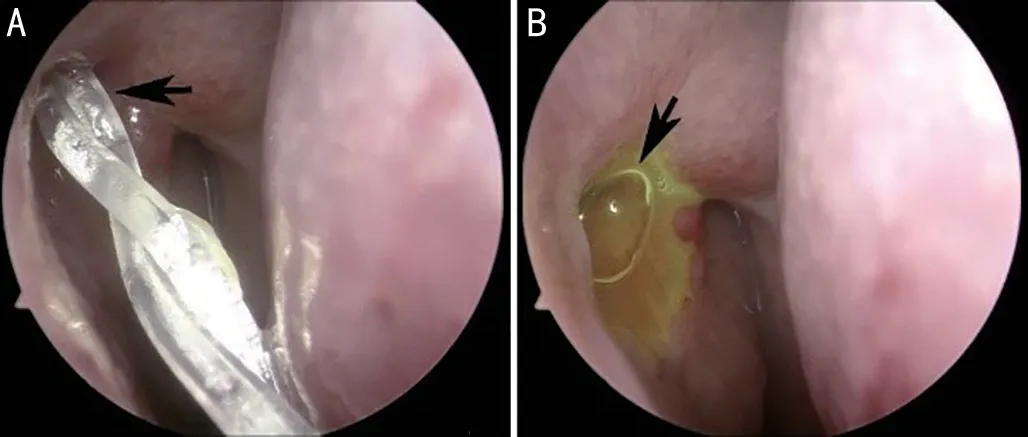
Figure 1 A successful case with BSTI A: Silicone tube placement in the ostium (arrow); B: Normal FDDT results (arrow) 2y after tube removing.BSTI: Bicanalicular silicone tube intubation; FDDT:Fluorescein dye disappearance test.

Figure 2 A case with complication associated with BSTI A: Tubeassociated proximal canaliculus slitting (arrow); B: Proximal canaliculus slitting (arrow); C: Slow dye disappearance on the FDDT(5min after dye instillation), note that fluorescein dye remained in right eye (arrow).BSTI: Bicanalicular silicone tube intubation; FDDT:Fluorescein dye disappearance test.
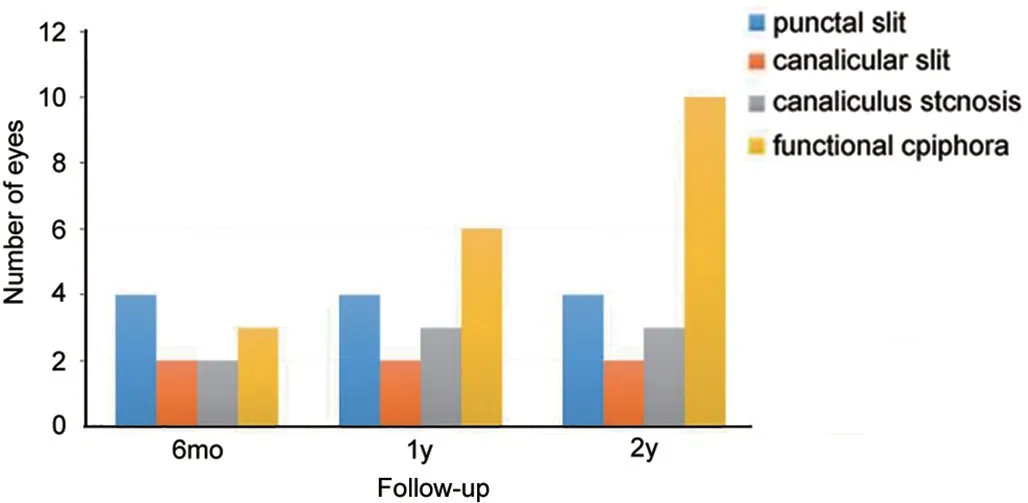
Figure 3 The change in the number of failures during postoperative follow-up.
Nasal ostium closure has been reported to be the primary cause of failure after En-DCR treatment[2,6,12-13].However,in cases of functional epiphora with patent rhinostomy, no obvious larimal puncta or eyelid abnormalities were observed as well, the pathophysiological reasons of functional epiphora are unclear.Aminet al[16]using dacryocystography after DCR,found no anatomic or physiologic abnormality in 58% of patients that experienced postoperative epiphora recurrence.Some scholars have remarked that defects in the function of the lacrimal pump may be the major reason of functional epiphora[10,17-18].Another possible explanation is the presence of mild stenosis of canalicular or common canalicular, which may affect the ability of drainage[19].Whereas, in spite of the hypotheses, the precise mechanisms of the functional epiphora remain unknown.
Secondly En-DCR with or without intubation has been proved to be a feasible method for failed Ex-DCR because of the closure of nasal ostium[6,20].However, functional epiphora therapy after anatomically patent DCR is challenging.There have been no reports on the treatment of functional epiphora after En-DCR.Secondary silicone tube intubation, lidtightening procedures, punctoplasty, as well as conjunctival-DCR using Jones tube are available treatment options for functional epiphora after Ex-DCR[7].Because the latter three methods are more invasive, have more complications and may require multiple surgeries, the authors recommended silicone tube intubation as a better method[7-9].In a study of 13 cases with functional epiphora after Ex-DCR, BSTI has achieved good results[9], due to the small sample size as well as shortterm follow-up, impeding inferences about specific summaries.In addition, it has been reported that permanent BSTI has a good effect on 34 functional epiphora patients after Ex-DCR[10].However, authors also figure out that the long time advantages of permanent intubation was restricted by probable requirement for tube replacement (26.9%) as well as tubeassociated canaliculitis (15.4%).
In this study, the success rate of BSTI for treatment of functional epiphora after En-DCR was >90% after two years of follow-up.BSTI is a commonly used approach to supporting the lacrimal sac ostium to improve this success ratio of En-DCR[2-3,12].However, the reasons of functional epiphora resolved after BSTI are unclear.One possible explanation is BSTI can enhance lacrimal pump function[8-9].The slow disappearance of FDDT was observed in all cases in the paper before secondary BSTI, which may indicate lacrimal pump dysfunction.Therefore, influenced patients would benefit from surgery to enhance lacrimal pump function, as normal FDDTs were observed in many cases after secondary BUTIs.Thus, we believe that the silicone intubation performed in the paper has influenced the lacrimal pump.Some scholars have found out that maintenance tube can enhance the function of lacrimal pump by helping the apposition of upper and lower puncta, and increasing the capillarity function of the lacrimal duct[9].However, in this study, functional epiphora was completely eliminated in most cases after a long period of time of tube removing, and there was no significant change in the apposition of upper and lower puncta by slit lamp examination during the follow-up.The diameter of the lacrimal punctum,lacrimal canalicular and nasal ostium opening may be slightly enlarged after the silicone intubation.The function of lacrimal pump may be increased by slightly enlarged lacrimal punctum and canalicular after the secondary BSTI.In addition, the presence of mild stenosis of canalicular or common canalicular maybe a reason for functional epiphora just as mentioned above[19].There may be mild lacrimal duct stenosis that affects the function of lacrimal pump, which can be treated with BSTI but cannot be detected by the surgeon with lacrimal duct irrigation.However, these hypothetical causes, the exact mechanism of epiphora resolution remains unclear.
Possible complications associated with BSTI include intranasal granulation tissue, peripunctate granulation, canaliculitis,postoperative infection, punctal and canalicular slitting, and punctual adhesions[3,6,8-9,12,14-15].Three eyes with punctal slitting and 1 eye with proximal canalicular slitting were observed in the study after BSTI.Complications may be associated with intraoperative damage of peripheral tissues around the puncta by punctum dilator, and with the continuous pull towards the inner canthus by the implanted tube.For 3 eyes presented with punctal slitting, however, 2 eyes with punctal slitting did not show any epiphora during the follow-up, and this phenomenon has also been reported in other literatures[8,19,21].One eye with proximal canaliculus slitting, and symptoms of epiphora were present during the follow-up.Canalicular stenosis occurred in 1 eye who complain of epiphora at the follow-up of 6mo and did not show any symptoms of epiphora within the time of tubes retention.It may be related to the damage of mucous membrane lining the canalicular by BSTI, resulting in canalicular stenosis after repair.Moreverover, recurrent functional epiphora is an occasional postoperative condition in the study.At 6mo of follow-up, only 1 eye had functional epiphora, at 12mo of follow-up, 3 eyes had functional epiphora, and the number increase to 4 eyes at the 24mo follow-up.As it can be seen, with the extension of followup time, the number of patients with functional epiphora increased.A second BUTI may be useful for patients having recurrent functional epiphora[10].However, a second BUTI was not performed among patients having recurrent functional epiphora in the study.
Granulation tissue hyperplasia of DCR ostium caused by stimulation of silicone tube is considered as a common complication.However, no granulation tissue of DCR ostium was found in this study, which may be due to the fact that all functional epiphora patients received BSTI more than 9mo after the first En-DCR, when the ostomy mucosa was stable.Meanwhile, BSTI was performed under endoscope to minimize the damage to the ostomy mucosa.In addition, routine use of hormonal nasal sprays to inhibit granulation tissue proliferation may also be responsible[6,12].Tube-associated canaliculitis was another common complication of BSTI[8].However, no patient was found to have a canaliculitis in this study.This may be because the silicone tubes in this study were removed 1mo after surgery, and long-term retention of the silicone tubes may cause tube-associated canaliculitis[8].
There are several restrictions to this study.First, anatomically patent confirmed with patent irrigation without significant reflux, and the lacrimal irrigation is somewhat subjective because the effect of irrigation varies with the intensity and speed of irrigation.In addition, mild canalicular stenosis may be included in this study.This problem may be addressed by lacrimal microendoscopy examination, which could be used to view the mucuos membranes of canalicular directly[22].
Second, the 2-year follow-up in this study was insufficient to fully evaluate the long-term results.As described above, the number of functional epiphora increased with the extension of follow-up.Finally, silicone tube retention time may be a factor affecting the success of postoperative function.Although the retention time of silicone tube for 1mo in this study achieved a good effect, the optimal retention time was not obtained in this study.
Nevertheless, in view of the above limitations, this study shows that BSTI can lead to the resolution of epiphora in cases of anatomically patent but functionally failed En-DCR.The operation of this approach was simple, and most patients have completely eliminated the epiphora without any obvious complications.
ACKNOWLEDGEMENTS
Conflicts of Interest: Han XM,None;Jiang WH,None;Wu WC,None;Yu B,None.
 International Journal of Ophthalmology2023年7期
International Journal of Ophthalmology2023年7期
- International Journal of Ophthalmology的其它文章
- Research on classification method of high myopic maculopathy based on retinal fundus images and optimized ALFA-Mix active learning algorithm
- Predicting visual acuity with machine learning in treated ocular trauma patients
- ldentification of hub genes for glaucoma: a study based on bioinformatics analysis and experimental verification
- Protective effect of ginsenoside Rg1 on 661W cells exposed to oxygen-glucose deprivation/reperfusion via keap1/nrf2 pathway
- Effects of endogenous dopamine induced by low concentration atropine eye drops on choroidal neovascularization in high myopia mice
- Differential analysis of aqueous humor cytokine levels in patients with macular edema secondary to diabetic retinopathy or retinal vein occlusion
