老年冠心病患者行急诊PCI后心肌内出血风险因素预测模型的建立与验证
[摘要]目的建立并验证老年冠心病急诊患者行经皮冠状动脉介入治疗(PCI)后心肌内出血的风险因素预测模型。方法选择南京医科大学第一附属医院2022年收治的54例行PCI的急诊老年冠心病患者作为研究对象,同期选择50例行PCI的急诊老年冠心病患者作为验证组;以心脏磁共振成像作为诊断和评估心肌内出血的金标准,采用多因素logistic回归模型构建心肌内出血风险因素的预测模型,绘制ROC曲线分析预测模型的应用价值。结果心肌内无出血者29例(无出血组),出血者28例(出血组)。出血组心肌梗死部位、病变支数、开通时间、肾功能不全比较,差异均有统计学意义(P<0.05);多因素logistic分析,结果显示心肌梗死部位为前壁、病变支数为多支、开通时间>45 min、肾功能不全是影响患者术后心肌内出血的独立危险因素(P<0.05),其联合预测模型为logit(P)=0.695×心肌梗死部位+0.756×病变支数+0.678×开通时间+0.702×肾功能不全;该预测模型预测急诊老年冠心病患者PCI后心肌内出血的曲线下面积为0.870(95%CI:0.769~0.972,P<0.001);在验证组中采用预测模型的灵敏度为89.47%,特异度为90.32%,阳性预测值为85.00%,阴性预测值为93.33%,准确率为90.00%,具有较高的应用价值。结论通过心肌梗死部位、病变支数、开通时间、肾功能不全构建的预测急诊老年冠心病患者PCI后心肌内出血的模型具有较高的应用价值。
[关键词]老年冠心病;经皮冠状动脉介入治疗;心肌内出血;风险因素;预测模型
doi:10.3969/j.issn.1674-7593.2023.05.003
Establishment and Validation of a Risk Prediction Model for Myocardial Hemorrhageafter Emergency Percutaneous Coronary Intervention in Elderly Patientswith Coronary Heart Disease
Wei Qun,Meng Haoyu**,Zhang Min,Geng Yi
Department of Cardiovascular Medicine,the First Affiliated Hospital with Nanjing Medical University,Nanjing210029
**Corresponding author:Meng Haoyu,email:mhy7259@163.com
[Abstract]ObjectiveTo establish and validate a risk prediction model for myocardial hemorrhage after percutaneous coronary intervention(PCI) in elderly patients with acute coronary syndrome.Methods54 elderly patients with acute coronary syndrome(ACS) who received percutaneous coronary intervention(PCI) at the First Affiliated Hospital of Nanjing Medical University in 2022 were selected as the study group,and 50 elderly patients with ACS who received PCI during the same period were selected as the validation group.Cardiac magnetic resonance imaging was used as the gold standard for diagnosing and evaluating myocardial hemorrhage,and a multiple logistic regression model was used to construct a risk prediction model for myocardial hemorrhage.ROC curve analysis was performed to evaluate the predictive value of the model.ResultsA total of 29 patients(the non-hemorrhage group) had no myocardial bleeding,while 28 patients(the hemorrhage group) developed myocardial hemorrhage after PCI.The differences in infarct location,number of diseased vessels,time to revascularization,and renal dysfunction were statistically significant between the two groups(Plt;0.05).Multivariate logistic analysis demonstrated that infarct location in the anterior wall,multiple diseased vessels,time to revascularizationgt;45 min,and renal dysfunction were independent risk factors for postoperative myocardial hemorrhage(Plt;0.05).The combined prediction model determined by logistic regression analysis was logit(P)=0.695×infarct location+0.756×number of diseased vessels+0.678×time to revascularization+0.702×renal dysfunction.The AUC of the prediction model for elderly emergency patients with ACS after PCI-related myocardial hemorrhage was 0.870(95%CI:0.769-0.972,Plt;0.001).In the validation cohort,the sensitivity of the prediction model was 89.47%,the specificity was 90.32%,the positive predictive value was 85.00%,the negative predictive value was 93.33%,and the accuracy was 90.00%.The prediction model had high application value.ConclusionThe risk prediction model based on the location of myocardial infarction,number of diseased vessels,time to revascularization,and renal insufficiency has a high application value for predicting myocardial hemorrhage after PCI in elderly patients with acute coronary syndrome.
[Key words]Elderly coronary heart disease;Percutaneous coronary intervention;Myocardial hemorrhage;Risk factors;Prediction model
冠心病是指冠状动脉狭窄或阻塞引起的心肌缺血性疾病,可能导致心肌梗死、心力衰竭等严重后果[1-3]。急诊经皮冠状动脉介入治疗(Percutaneous coronary intervention,PCI)是目前常见的用于急性冠状动脉综合征患者的治疗方法,有助于加速恢复冠状动脉血流,缓解心肌缺血和心绞痛,而术后心肌内出血是一种严重的并发症,可能导致心功能衰竭和死亡[4-5]。有学者指出,出血的原因通常是手术时损伤了冠状动脉或其他血管的壁层,导致血液渗漏到周围组织中[6]。但也有研究显示,一些因素可能增加心肌内出血的风险,如患者的年龄、女性、肾功能不全、体质量过轻等[7]。特别是在使用抗凝药物和抗血小板药物的情况下,心肌内出血临床发病率居高不下,可能导致心包填塞、心脏功能障碍等严重后果。如何准确有效地构建预测老年冠心病患者急诊PCI后心肌内出血的模式,对临床指导救治具有十分重要的意义。
1对象与方法
1.1研究对象
经本院伦理委员会审议并批准,选择南京医科大学第一附属医院2022年收治的54例行PCI的急诊老年冠心病患者作为研究对象,其中男37例,女17例,年龄(72.72±5.48)岁。同期选择50例行PCI的急诊老年冠心病患者作为验证组,其中男35例,女15例,年龄(71.93±6.03)岁。纳入标准:①患者符合冠心病诊断标准[8];②年龄≥60岁;③临床资料完整;④并存严重心绞痛症状,出现心电图异常改变且心肌酶谱升高,符合急诊PCI治疗的相关标准;⑤对本研究知情并签署知情同意书。排除标准:①入组前半年接受过外科手术治疗;②合并肝肾等脏器功能不全;③合并存在恶性肿瘤;④合并存在自身免疫系统、血液系统或感染性疾病;⑤临床或随访资料缺失。
1.2方法
本组研究中以心脏磁共振成像作为诊断和评估心肌内出血的金标准,利用T1、T2及T2加权等多种序列扫描检查均可用于对心肌内出血的诊断。
本研究详细记录性别、吸烟史、糖尿病、高血压、高脂血症、饮酒史、病变支数、心肌梗死部位、白细胞计数、闭塞冠状动脉开通时间、中性粒细胞计数、肾功能不全比例、血红蛋白水平、红细胞计数。
1.3统计学方法
采用SPSS20.0统计学软件进行数据分析。正态分布计量资料采用±s表示,组间比较采用t检验;计数资料采用χ2检验;采用logistic回归模型构建心肌内出血风险因素的预测模型;出血风险预测模型与金标准诊断结果比较采用kappa一致性检验;绘制ROC曲线分析预测模型的应用价值,P<0.05为差异有统计学意义。
2结果
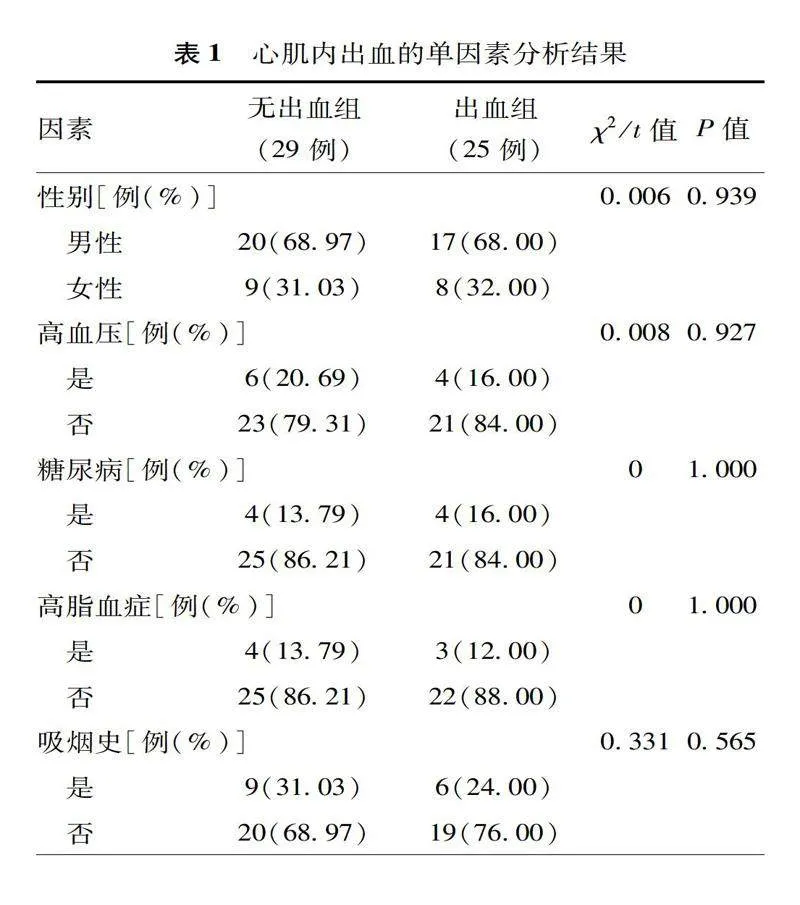
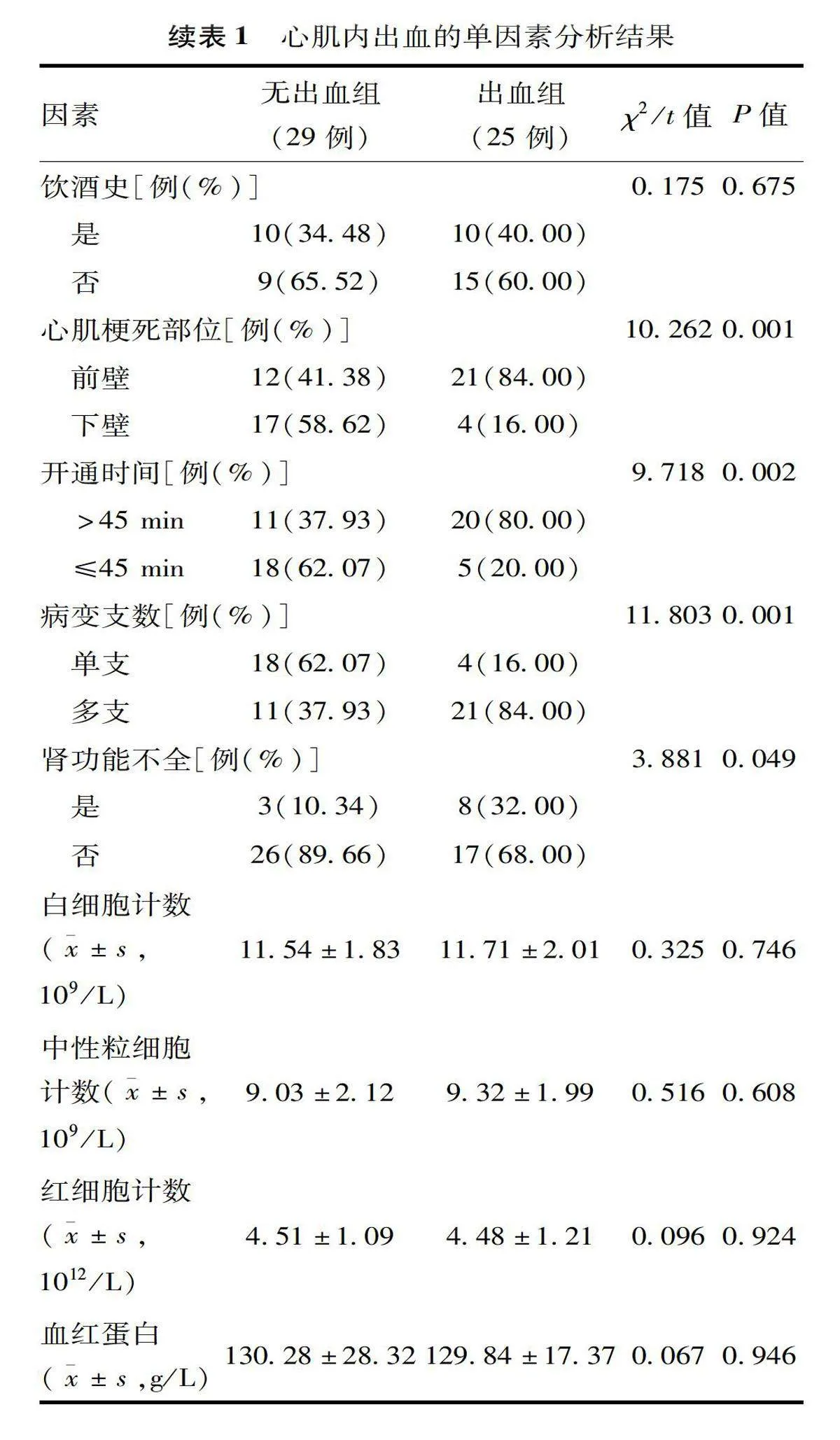
2.1心肌内出血的单因素分析
心肌内无出血者29例(无出血组),出血者28例(出血组)。出血组心肌梗死部位、病变支数、开通时间、肾功能不全比较,差异均有统计学意义(P<0.05),见表1。
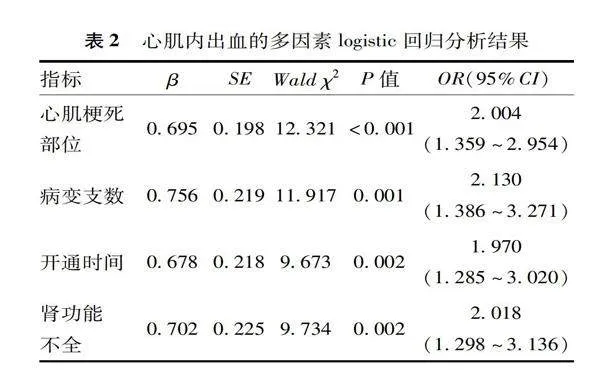
2.2心肌内出血的多因素分析
将单因素分析中的心肌梗死部位(下壁=0,前壁=1)、病变支数(单支=0;多支=1)、开通时间(≤45 min=0,>45 min=1)及肾功能不全(否=0,是=1)作为自变量,将是否心肌内出血作为因变量(未发生=0,发生=1)进行多因素logistic分析,结果显示心肌梗死部位为前壁、病变支数为多支、开通时间>45 min、肾功能不全是影响患者术后心肌内出血的独立危险因素(P<0.05),其联合预测模型为logit(P)=0.695×心肌梗死部位+0.756×病变支数+0.678×开通时间+0.702×肾功能不全,见表2。
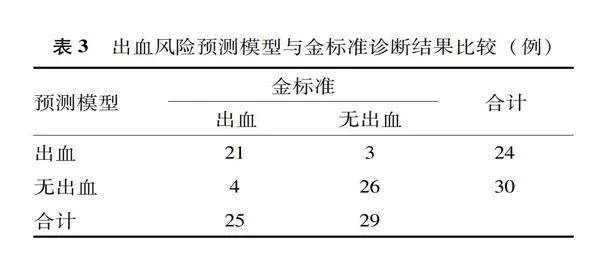
2.3心肌内出血风险预测模型与金标准诊断结果比较
心肌内出血风险预测模型预测急诊PCI术后患者出现心肌内出血共24例,无心肌出血30例,与金标准的一致性较好(Kappa=0.739,P<0.001),见表3。
2.4心肌内出血预测模型应用价值
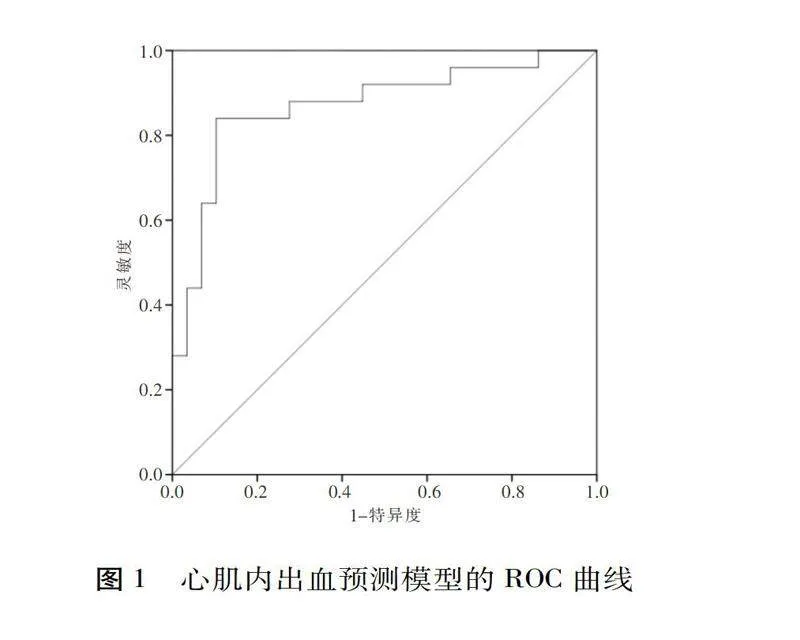
该预测模型预测急诊老年冠心病患者PCI后心肌内出血的曲线下面积为0.870(95%CI:0.769~0.972,P<0.001),见图1。
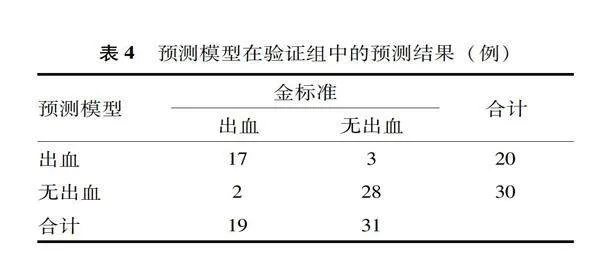
2.5预测模型在验证组中的预测结果
在验证组中采用预测模型的灵敏度为89.47%,特异度为90.32%,阳性预测值为85.00%,阴性预测值为93.33%,准确率为90.00%,具有较高的应用价值,见表4。
3讨论
急诊PCI在冠状动脉患者治疗中的应用非常广泛,可以有效地缓解症状、减轻心肌损伤、改善预后和挽救患者的生命,可用于对急性心肌梗死、不稳定性心绞痛、ST段抬高型心肌梗死、冠状动脉狭窄等患者的临床救治[9-10]。但有研究显示,急诊PCI过程中可能导致患者出现包括出血、心律失常、血管损伤等多种并发症[11]。心肌内出血多在PCI过程中或术后,冠状动脉插管和球囊扩张等操作导致冠状动脉壁和心肌组织损伤,从而引起心肌内血管破裂和血液外渗[12]。研究显示,当急诊PCI后出现心肌内出血极易导致心肌组织缺血,严重者可以导致心肌梗死,使患者心肌功能受损,甚至导致心力衰竭等严重后果[13]。此外,心肌内出血可以导致心肌组织的血液灌注不足,心脏收缩力下降,导致心力衰竭,部分患者病情严重时还会进一步刺激心肌组织,导致心律失常的发生,甚至导致心脏骤停[14-15]。
本研究分析认为:首先,冠状动脉病变支数是指冠状动脉狭窄的数量,狭窄越多,心肌缺血的程度越重,术后心肌内出血的风险也就越高;其次,心肌梗死部位是指心肌受损的具体位置,不同位置的心肌梗死可能会导致心肌组织的不同反应,从而影响术后心肌内出血的发生率;再次,肾功能不全是指肾脏的滤过功能下降,可能导致身体内的毒素和废物无法有效排出,这种情况可能会导致血液中的血小板聚集和凝血能力增强,进而增加心肌内出血的风险;最后,冠状动脉开通时间是指PCI的时间,如果治疗时间过长,可能会导致术后心肌内出血的风险增加。临床中可通过联合分析上述指标制定更为有效的治疗方案和预防措施。本组研究表明,在应用过程中通过该预测模型,可以提前识别高危患者,针对性地进行干预和治疗,从而减少心肌内出血的发生率,提高患者的安全性。此外,临床可以根据该预测模型有针对性地分配医疗资源,优化医疗资源的利用。
综上所述,该模型具有较高应用价值,但本研究为单中心小样本临床研究,有待后续深入研究和分析。
参考文献
[1]Wang L,Liu T,Wang C,et al.Development and validation of a predictive model for adverse left ventricular remodeling in NSTEMI patients after primary percutaneous coronary intervention[J].BMC Cardiovasc Disord,2022,22(1):386.
[2]Padro T,Manfrini O,Bugiardini R,et al.ESC working group on coronary pathophysiology and microcirculation position paper on 'coronary microvascular dysfunction in cardiovascular disease'[J].Cardiovasc Res,2020,116(4):741-755.
[3]Xu Z,Li Y,Zhang R,et al.Risk factors for cardiac rupture after acute ST-segment elevation myocardial infarction during the percutaneous coronary intervention era: a retrospective case-control study[J].J Thorac Dis,2022,14(4):1256-1266.
[4]Liu T,Howarth AG,Chen Y,et al.Intramyocardial hemorrhage and the “wave front” of reperfusion injury compromising myocardial salvage[J].J Am Coll Cardiol,2022,79(1):35-48.
[5]van der Bijl P,Abou R,Goedemans L,et al.Left ventricular post-infarct remodeling:implications for systolic function improvement and outcomes in the modern era[J].JACC Heart Fail,2020,8(2):131-140.
[6]Shoji K,Yanishi K,Kawamata H,et al.New risk factors for early- and late-onset cardiac rupture in ST-elevation myocardial infarction patients after primary percutaneous coronary intervention[J].J Cardiol,2022,79(3):400-407.
[7]Ylmaz S,Coansu K.Prognostic factors and outcomes in young patients with presented of different types acute coronary syndrome[J].Angiology,2020,71(10):894-902.
[8]颜红兵,柯元南.美国冠心病诊断与治疗指南[M].北京:中国环境科学出版社,2004:187.
[9]Tehrani BN,Truesdell AG,Psotka MA,et al.Astandardized and comprehensive approach to the management of cardiogenic shock[J].JACC Heart Fail,2020,8(11):879-891.
[10]Tiller C,Reindl M,Holzknecht M,et al.Association of plasma interleukin-6 with infarct size,reperfusion injury, and adverse remodelling after ST-elevation myocardial infarction[J].Eur Heart J Acute Cardiovasc Care,2022,11(2):113-123.
[11]李静林,王贵松.非心脏外科手术围术期心肌梗死的危险评估与处理[J].临床内科杂志,2022,39(1):1-3.
[12]Mohamed MO,Hirji S,Mohamed W,et al.Incidence and predictors of postoperative ischemic stroke after coronary artery bypass grafting[J].Int J Clin Pract,2021,75(5):e14067.
[13]Powell-Wiley TM,Poirier P,Burke LE,et al.Obesity and cardiovascular disease:a scientific statement from the american heart association[J].Circulation,2021,143(21):e984-e1010.
[14]Molek P,Zmudzki P,Wlodarczyk A,et al.The shifted balance of arginine metabolites in acute myocardial infarction patients and its clinical relevance[J].Sci Rep,2021,11(1):83.
[15]Cokic I,Chan SF,Guan X,et al.Intramyocardial hemorrhage drives fatty degeneration of infarcted myocardium[J].Nat Commun,2022,13(1):6394.
(2023-04-12收稿)